Abstract
Maternal depression is a well-established risk factor for the development of depression in offspring. As such, reducing maternal depression may be key to effective prevention efforts to reduce offspring’s depression. Based on the broad risk represented by maternal depression, examining cross-over effects of parent-focused interventions on maternal depression is important. The present study examined improvements in maternal depression as a mediator of the long-term effects of the Family Check-Up (FCU) prevention program on youth depression across three randomized controlled trials. The FCU is a family-focused intervention originally designed to reduce youth problem behaviors, particularly conduct problems and substance use, but has also been found to have cross-over effects on other youth problem behaviors, including internalizing symptoms. We utilized integrative data analysis that allows for powerful tests of prevention effects across trials, specifically moderated nonlinear factor analysis, to integrate data across three trials: one trial initiated in early childhood and two in early adolescence. Using a latent growth modeling approach, we first examined direct effects of the FCU on changes in maternal depression. Then we examined the mediating effect of maternal depression on changes in both parent and youth reports of youth depression. A significant intervention effect on maternal depression was observed across the three trials, with the FCU predicting improvements in maternal depression. In turn, such improvements predicted a reduction in the growth in both parent and youth reports of youth depressive symptoms across 10 years post baseline. These results demonstrate the utility in addressing cross-over effects of family-focused interventions in reducing the long-term development of depression in youth through mediating pathways.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Depression in adulthood is highly prevalent and associated with substantial suffering. Indeed, depression is one of the leading causes of worldwide disability as well as death (see Kessler, 2012). It is also associated with tremendous social and occupational disruption, and diminished quality of life (see Richards, 2011). For instance, depression is associated with lower educational and occupational attainment (Ueno & Krause, 2020), greater marital instability (Whisman & Uebelacker, 2009), and diminished life expectancy (Pratt et al., 2016). Therefore, identifying prevention and intervention opportunities to reduce the burden of depression represents a critical public health goal.
Depression in parents, more narrowly, includes additional challenges. Maternal depression, in particular, is a well-established risk factor for the development of emotional and behavioral problems in youth (Goodman et al., 2011). Mechanisms of transmission are complex, for instance, Goodman and Gotlib’s model (1999) highlights several critical pathways for the intergenerational transmission of depression risk including genetic risk, neuroregulatory dysfunctions, heightened contextual stress, and altered parenting styles. This last pathway is of particular importance for prevention efforts, as it highlights the potential benefits of parenting interventions for disrupting depression risk in offspring. Indeed, maternal depression is related to disruption in a variety of facets of typical parent–child functioning, putting youth an increased risk for psychopathology (Goodman et al., 2011). For example, parental depression has been associated with harsher parenting and greater negative emotionality in parent–child interactions (e.g. Shaw et al., 2006). These familial factors in turn have been identified as risk factors for the development of anxiety, depression, and suicidal ideation in youth (Kingsbury et al., 2019).
Prevention of Depression
In light of the substantial public health ramifications of depression in adulthood, and the specific risks associated with maternal depression, identifying opportunities to alleviate depression in mothers represents a critical goal. Moreover, successful reduction of depression in mothers may yield benefits for youth. Indeed, two lines of research suggest that parental depression has important implications for the prevention of depression in youth. First, parental depression has been associated with diminished responsiveness to youth-focused interventions for depression. For instance, Brent and colleagues (1998) found that the efficacy of a child-focused CBT intervention was significantly reduced in the presence of maternal depressive symptoms. Several other trials with youth in middle to late childhood have reported similar reduced effectiveness of interventions in the face of elevated maternal depression (e.g., Eckshtain et al., 2018, 2019). This pattern of results suggests the importance of attending to parental depression in the context of prevention and intervention programs for youth.
Second, parenting interventions may lead to reductions in parental depression, though literature has demonstrated mixed findings on this issue (Easterbrooks et al., 2016). For instance, parent training programs, designed to reduce youth behavior problems, may give parents hope and a sense of mastery (e.g., Wittkowski et al., 2016), and skills to manage child behavior more effectively and positively. These skills may reduce parent’s stress and depressed mood. Indeed, Hutchings and colleagues (2012) found that improvements in parental depression partially mediated the effects of the Incredible Years parent-training intervention on youth behavior problems in a sample of parents of 3- and 4-year-old children. Identification and study of such secondary effects (in other words, on outcomes not originally the target of the intervention, referred to as cross-over effects) may hold important implications for youth depression treatments. However, few other studies have directly examined parental depression as a mediator of prevention or intervention effects on improvements in youth emotional or behavior problems.
Family Check-Up
One such parenting program with established cross-over effects on both youth and maternal depression is the Family Check-Up (FCU). The present study extends the work of Connell and colleagues (2021), which demonstrated the main effect of the FCU on youth depression, by examining the indirect effect of maternal depression. The FCU is a prevention program originally designed to reduce conduct problems, substance use, and other externalizing symptoms in youth by targeting parent and family mechanisms (Dishion & Stormshak, 2007). The FCU employs motivational interviewing techniques to motivate parents to enhance effective parenting skills utilizing an adaptive intervention framework with intervention targets and techniques adapted to the goals of individual families. Prior trials have demonstrated that the FCU is effective at reducing externalizing problems and substance use when delivered in early childhood (Dishion et al., 2008, 2014) and adolescence (Van Ryzin et al., 2012). The FCU has also previously demonstrated cross-over effects. For example, the FCU delivered in adolescence predicted reduced symptoms of depression across adolescence (Connell et al., 2018) and into early adulthood (Connell et al., 2016). Indeed, intervention effects on depression have been observed regardless of age administered in and have been shown to endure for several years after delivery (Connell et al., 2021). Similarly, FCU delivery in early childhood was associated with reductions in co-occurring internalizing and externalizing problems mediated by family environment (Wang et al., 2019). Further, Connell and colleagues (2016) found that the FCU delivered in adolescence was associated with reduced suicidal thoughts and behaviors in young adulthood. Conceptually, similar results were observed in an early childhood trial of the FCU, with reductions in suicidal ideation in early adolescence mediated by improvements in youth self-regulatory abilities (Connell et al., 2019).
Several parent- and family-level mechanisms of intervention effects on youth emotional and behavior problems have been documented, including reductions in family conflict (Fosco et al., 2016; Smith et al., 2014) and improvements in positive parenting (e.g., Brennan et al., 2013; Dishion et al., 2008; Gardner et al., 2007). Of relevance to the present study, improvements in maternal depression have also been shown to mediate the effects of the FCU in early childhood on reductions in youth emotional and behavior problems (e.g., Shaw et al., 2009). For example, Reuben et al. (2015) found that reducing maternal depression in early childhood was associated with lower levels of parent-reported, youth depressive symptoms in late childhood. Similarly, Wang and colleagues (2019) found that reductions in maternal depression mediated risk for co-occurring internalizing and externalizing symptoms in youth at later follow-ups (age 14 years).
However, analyses of maternal depression as a mediator of intervention effects on youth depression, particularly in other FCU trials, have been hampered by the limited measurement of depression, and changes in measures of depression that were employed over time within trials. For instance, in the first trial of the FCU program in early adolescence (the Project Alliance 1 study), measures of depression in parents and youth were initially only administered to a subset of youth identified by teachers as being at high-risk for conduct problems. Although these measures were later administered to the entire sample, the complex early measurement plan limited statistical power for tests of mediation (see Connell & Dishion, 2008). Similarly, changes in measurement approaches in the individual trials have limited longitudinal analyses. For instance, in both the Project Alliance 1 and 2 studies, different measures of youth depression were used in early adolescence versus later assessments.
Present Study
To date, the mediating role of maternal depression has only been examined in one trial of the FCU initiated in early childhood, and there is scant evidence of broader mediating effects of maternal depression in other prevention programs beyond childhood. The present study seeks to extend this work by incorporating evidence across three trials of the FCU, one initiated in early childhood and two in early adolescence, to provide a comprehensive test of improvements in maternal depression as a mediator of intervention effects on youth depression over time and across trials. We employed integrative data analysis (IDA) techniques to synthesize data across three trials of the FCU. IDA allows researchers to synthesize results across multiple trials, providing a powerful test of general prevention effects. Such techniques also provide opportunities to address the previously described measurement challenges that may limit the examination of mediation in individual trials. Therefore, IDA approaches allow researchers to leverage existing prevention trial datasets to address novel questions, including the examination of mediating pathways of intervention effects across multiple trials.
In particular, we employed moderated nonlinear factors analysis (MNLFA; Bauer & Hussong, 2009), which allows for item-level harmonization analyses of multiple measures of the same construct across trials. MNLFA provides a method of accounting for possible differential item functioning (DIF) across covariates and creating scores for the construct of interest based on all available items. With this technique, we can provide an overarching test of the mediating effects of the FCU on reductions in youth depression via improvements in maternal depression, across three randomized trials covering a broad developmental span.
Methods
The present study employs harmonization analyses drawing data from three separate intervention trials of the FCUFootnote 1. The methods section includes description of the original studies as well as the IDA methods employed in the present study. First, we discuss the samples collected for each study, the protocol section reviews how the FCU was implemented, and measures section details the assessment methods from the different trials that were used for the harmonization. Next, we describe the analytic plan for both the harmonization analyses and the structural equation modeling employed using the new, harmonized variables.
Samples
Early Steps
This trial included 731 low-income families recruited from three different locations: Pittsburgh, Pennsylvania, Eugene, Oregon, and Charlottesville, Virginia. The youth sample was 49.5% female and were racially/ethnically diverse: 54.4% White, 28.2% African American, 10.7% Latinx, and 6.7% multiracial or other. Families were recruited when youth were between the ages of 2 years and 0 months and 2 years 11 months from Women, Infants, and Children Nutritional Supplement (WIC) centers. Families were screened to ensure they met study criteria.
Families were randomized to two conditions, intervention (50.2%) or control conditions (49.8%) at baseline. Control families completed yearly assessments and intervention families completed assessments and the FCU as well as follow-up services as warranted which typically included annual visits on eight occasions when youth were ages 2 to 10.5 years old. Of the 367 families randomized to the intervention condition, 343 (93.5%) took part in the initial FCU assessment (interview, assessment, feedback) at least once between ages 2 and 10.5. Families who elected to receive follow-up sessions focused on parenting, child development, and behavior management. The percentage of families in the intervention condition receiving additional sessions ranged from a low of 65% (age 7.5) to the high of 74% (age 4), and average number of sessions at each wave ranged from 2.3 (age 10.5) to 3.5 (age 5) across waves.
Project Alliance 1
This trial included 998 families recruited in sixth grade from three middle schools in low-income neighborhoods in a metropolitan area in the northwestern United States. The sample included 50.6% female youth, and was racially/ethnically diverse: 49.2% White, 29.2% African American, 6.8% Latinx, and 14.8% multiracial or other. Families were recruited when youth were 11 years old and followed through ages 28–30 years old. Families were randomized to two conditions, intervention (50.1%) or control conditions (49.8%) at baseline. Control families completed yearly assessments. Intervention families completed assessments and the FCU as well as follow-up services as warranted. Retention remained above 80% for most assessment points, with 75.6% retention at the final assessment point. In the intervention condition, 224 families (45%) received the FCU at least once between grades 7–11.
Project Alliance 2
This trial included 593 families recruited in sixth grade from three middle schools in low-income neighborhoods in a metropolitan area in the northwestern United States. The youth sample was 48.5% female and was racially/ethnically diverse: 36% White, 15.2% African American, 18% Latinx, and 30.8% multiracial or other. Families were recruited when youth were 11 years old and followed through age 23 years old. Families were screened to ensure they met study criteria.
Families were randomized to two conditions, intervention (65%) or a school-as-usual control condition (35%) at baseline. This trial used an unbalanced randomization in order to increase power to detect heterogeneous patterns of intervention effects. Control families completed yearly assessments, and intervention families completed assessments and the FCU as well as follow-up services as warranted which typically included annual visits at seven assessment waves when youth were age 11 years to age 23 years. For the full sample, retention was above 80% for most assessment points, with 78% of participants completing at least one of the early-adult assessments. Within the intervention condition, 42% (n = 163) of families received the FCU between grades 7–9, 80% of whom received follow-up intervention services. Average duration of intervention services was 337 min (approximately 6 h). The FCU was offered to families again in early adulthood (age 20), at which 34.7% (n = 134) of those in the intervention condition families received the FCU, with an average of 1.92 h of intervention time.
Protocol
The FCU is an ecological, family-centered intervention program which utilizes motivational interviewing techniques to enhance parent application of skills and maintenance of benefits (Dishion & Stormshak, 2007). The ecological framework includes an in-depth assessment of the youth’s environment including socioemotional, peer relational, and familial and parenting factors. Interventions are then tailored to address the individual needs of the child, making them developmentally sensitive and individualized to the level of care required by the child and family. The intervention is conducted in several parts, including an initial get-to-know-you session that in clinical practice is followed by the assessment sessions noted aboveFootnote 2. Following the assessment, a consultation and feedback session are conducted to highlight the interventionists’ observations from both the get-to-know-you interview and assessment, highlighting both strengths and challenges of the child and family. Whereas previous work across trials indicates the benefits of participating in these 3 sessions (get-to-know-you, assessment, and feedback), families have the option of engaging in follow-up treatment sessions tailored to parent’s goals identified in the feedback session. These options often include in-person/remote family management sessions, phone check-ups, and specific community referrals. Therefore, the FCU is a relatively brief, ecologically valid, individualized intervention program designed to support family and youth adjustment. The present study examined three randomized-control trials of the FCU in three separate samples, including long-term follow-ups. First, Early Steps was initiated to families beginning when children were age 2, with developmentally appropriate targets chosen for intervention (e.g., parenting practices, child self-regulation). Project Alliance 1 and Project Alliance 2 were school-based prevention trials initiated when children were in 6th grade and included a multilevel prevention framework.
Measures
Supplemental Table 1 lists the measures administered at each assessment point. Of note, the Center for Epidemiological Studies–Depression scale (CES-D; Radloff, 1977) was administered to parents across all three trials of the FCU: Early Steps, PAL1, and PAL2. The CES-D is a 20-item self-report measure assessing past week symptoms of depression on a scale from 0 to 3.
Early Steps
The CES-D was administered to parents at the following youth ages: 2, 3, 4, 5, 7.5, 8.5, 9.5, 10.5, 14, and 16 years old. Children completed diagnostic interviews using the computerized Diagnostic Interview Schedule for Children IV (Shaffer et al., 2000) at age 10.5. Current analyses focused on symptoms from the depression module. At ages 14 and 16, youth completed the Child Depression Inventory (CDI; Kovacs, 1992), a 27-item self-report measure of depressive symptoms in youth over the past 2 weeks. Parents completed the Child Behavior Checklist for Ages 1.5–5 (CBCL; Achenbach, 1991), at ages 2, 3, 4, and 5, and the CBCL for Ages 6–18 (Achenbach, 1991) during the age 7.5, 8.5, 9.5, 10.5, 14, and 16 assessments, which includes depression-symptoms rated on a 3-point scale (0 = not true, 1 = somewhat/sometimes true, 2 = very true/often true), with a 6-month time-frame.
PAL1
A stratified assessment approach was used at the age 11, 12, and 13 assessments, such that depression data was only collected for an elevated-risk subset of youth and parents, based upon teacher reports of behaviors related to the risk for conduct problems (see Connell & Dishion, 2008). Parents completed the CES-D when youth were ages 11, 12, 13, 16, and 18 years old. At ages 11, 12, 13, and 18, parents and youth completed the CBCL-ages 6–18 (Achenbach, 1991). Youth also completed the CDI (Kovacs, 1992) at ages 11, 12, and 13, and the Brief Symptom Inventory (Derogatis & Spencer, 1982) at ages 16, 22, and 23, which includes items assessing depression symptom severity in the prior week. At four time-points (age 11, 12, 13, and 16), youth completed a self-report health measure that included items regarding past-year occurrence of suicide attempts. Youth completed the Life Events Coping Inventory (Dise-Lewis, 1988) at ages 11, 12, 13, 16, 18, 22, and 23, which includes two items reflecting suicidal ideation and self-harm in response to stress. Participants also completed the Composite International Diagnostic Interview (World Health Organization, 1997), administered by trained research staff blinded to intervention status at age 18. Participants completed a range of diagnostic modules, and current analyses focused on symptoms from the depression module.
PAL2
Parents completed the CES-D at youth ages 11, 12, 13, 20, 21, and 22 years old. Youth completed a depression symptom checklist at ages 11–14 that includes 14 items reflecting past-month severity of symptoms associated with depression diagnoses (Klostermann et al., 2016). Youth also completed the CDI (Kovacs, 1992) at ages 11, 12, and 13, as part of the FCU assessment. At ages 20, 21, and 22, parents and youth completed the CBCL (Achenbach, 1991), measuring symptoms of depression in the past 6 months.
Analytic Plan
Overview of Data Harmonization
Data harmonization analyses employed MNLFA (Hussong et al., 2013), which facilitates item-level analyses across datasets when items from different measures have been used across trials. MNLFA permits the estimation of a final latent-variable reflecting the construct of interest, adjusting for Differential Item Functioning. Parent and youth reports of depression were analyzed separately using the R-based MNLFA package (Gottfredson et al., 2019) to draw calibration samples and iteratively format Mplus command files. MNLFA analyses were conducted in Mplus 8.4 (Muthen & Muthen, 2020). Following Gottfredson and colleagues (2019), a single time-point of data for each participant was randomly selected to generate a calibration sample for establishing measurement properties. Using the calibration sample, an iterative series of analyses was conducted to examine invariance across covariates for factor means, variances, and item intercepts/factor loadings to obtain valid item parameter estimates adjusting for DIF. Covariates were included as follows: youth gender (0 = male, 1 = female), ethnic minority status (0 = European American, 1 = racial/ethnic minority), age at assessment, intervention assignment (0 = Control condition, 1 = Intervention condition), and study (with two orthogonal contrasts, comparing PAL1 with PAL2, and PAL1 with Early steps).
First, in a series of separate analyses, we examined potential covariate differences in overall mean and variance in depression severity to assess the extent to which individual items reflected depression severity (i.e., factor loadings) and the likelihood of item endorsement across levels of the covariate for individuals at the same level of depression severity (i.e., item intercepts). Second, results from these analyses were then included in a full model, simultaneously testing invariance across these model parameters for all covariates with significant effects in the first-step analyses. Third, to protect against type I errors, a Benjamini-Hochberg (1995) family-wise error correction was applied to results from the second-stage analysis, to generate a final scoring model including only significant effects that survive correction. Finally, MNLFA estimates were fixed to the parameter estimates from this final model using the calibration sample results to generate a scoring model. This final scoring model was then used to generate depression estimates using the full longitudinal data set, which were used in subsequent analyses.
We conducted separate MNLFA analyses for parental depression, and for parent and youth reports of youth depression. For parental depression, as all studies employed the CES-D to assess depressive symptoms, harmonization analyses included all 20 items on this measure, with responses ranging from 0 (“Rarely or none of the time”) to 3 (“Most or all of the time”). For youth depressive symptoms, based on the array of measures employed over time across studies, a more complex approach to data harmonization was employed to capture the range of depressive symptoms while also prioritizing feasibility in the face of data complexity (for example, harmonizing meaningfully similar constructs like low mood assessed in slightly different ways). Following a comprehensive examination of available items for youth depression and consideration of diagnostic criteria, we mapped items from all available measures onto 17 depression symptoms. Symptoms were as follows: (1) sad/blue, (2) irritable/moody, (3) anhedonia, (4) appetite disturbance, (5) sleep disturbance, (6) restless/agitated, (7) low energy, (8) overtired, (9) feeling worthless/inferior, (10) feelings of guilt, (11) concentration problems, (12) suicidal ideation, (13) self-harm/suicide attempt, (14) thoughts of death/dying, (15) hopelessness, (16) loneliness, (17) cries a lot. For complete details, see Connell and colleagues (2021). Given the different response scales used across measures, item responses for youth depression were dichotomized to represent the endorsement of a given symptom across available measures at a given age (0 = no, 1 = yes). The latent parent and youth depression variables were scaled to have mean = 0 and variance = 1 in all MNLFA models.
Longitudinal Models
Longitudinal analyses were conducted in several steps. First, separate growth models were examined for parental depression and youth depression to establish the necessary growth parameters in separate analyses. Once a good-fitting model was achieved, covariates (gender, ethnic minority status, intervention assignment, and orthogonal contrasts comparing PAL1 with PAL2, and with Early Steps) were added to the models for parent and youth depression. Trajectories of parental depression were estimated using an Autoregressive Latent Trajectory Model (ALT; Bollen & Curran, 2004), due to poor fit of a model without autoregressive paths. Therefore, the time-score of zero (i.e., the latent intercept) was used to reflect 1 year post baseline in the ALT model. Baseline depression was not included in the estimation of the latent intercept or slope parameters. However, baseline depression was allowed to predict subsequent depression through both an autoregressive path predicting 1-year post-baseline, and a path predicting the intercept (Bollen & Curran, 2004). The autoregressive paths captured time-specific variability around the underlying latent trajectory. Intervention assignment was not allowed to predict the pre-treatment baseline assessment but was allowed to predict latent intercept of parent depression (reflecting depression at 1-year post-baseline) and the linear slope in depression over time. All other covariates were allowed to predict both the latent intercept and slope parameters, as well as depression at the pre-treatment baseline.
For youth depression trajectories, a latent growth model that included latent intercept, linear slope, and quadratic slope provided good fit to the data, and so the ALT modeling approach was not employed. Therefore, in these youth depression LGMs (both parent and youth report), time was modeled as “Years Post-Baseline,” with a time-score of “0” representing the pre-treatment baseline, and intervention assignment was allowed to predict the linear and quadratic slope parameters. Next, the mediating effect of improvements in parental depression was examined using parallel process growth models that included both parental and youth depression trajectories in the same analysis, with separate analyses for parent and youth reports of youth depression. In these final two models, we examined the indirect effect of intervention on changes in youth depression via the effect of intervention on the intercept of parental depression (parameterized as 1 year post-baseline as described previously). Standard errors for indirect effects were calculated using the delta method (MacKinnon et al., 2002). Acceptable model fit is indicated by non-significant chi-square value, CFI values above 0.90, and RMSEA/SRMR values less than 0.08 (e.g., Hu & Bentler, 1999).
Results
Descriptive Statistics
The aggregated sample included data from 2322 families. The number of parents and youth providing depression-related data at each study wave is shown in Table 1. The sample included 49.7% female youth, and was racially/ethnically diverse (47.5% White, 25.4% African American, 10.9% Latinx, and 16.3% multiracial/other). The CES-D mean scores were M = 14.43 (SD = 10.9) at baseline, with 37% of the sample above the clinical cutoff score of 16 at baseline.
Data Harmonization Results
Due to space constraints, we present full results for harmonization analyses for parental depression, only. Complete details regarding harmonization analyses for youth depression are presented in the Connell and colleagues (2021) study. Full results for the parental depression model are shown in Supplemental Table 2. The factor mean was significantly negatively associated with youth age at assessment. The factor variance was positively associated with youth age at assessment, and was more positive in the Early Steps sample versus the PAL1 sample. While no significant covariate effects on item discrimination were observed, several significant covariate effects on item difficulty were. Difficulty estimates for items 1 (“I was bothered by things that usually don’t bother me”) and 2 (“I did not feel like eating; My appetite was poor”) were negatively associated with youth age. Difficulty estimates for items 5 (“I had trouble keeping my mind on what I was doing”) and 20 (“I could not get going”) were positively associated with youth racial/ethnic minority status. Item 5 difficulty was higher in PAL2 versus PAL1.
Latent Growth Model for Parental Depression
The unconditional ALT model for maternal depressive symptoms provided good fit to the data (χ2 = 54.95, df = 36, p = 0.02, CFI = 0.99, TLI = 0.99, RMSEA = 0.02, SRMR = 0.06). The intercept (estimate = − 0.18, SE = 0.02) and slope parameters (estimate = -0.02, SE = 0.004) were both significant, and the intercept (representing depression at one year post-baseline) was significantly predicted by baseline depression (estimate = 0.31, SE = 0.02). Significant and positive autoregressive effects were observed across all adjacent assessment waves from 1 year post baseline to 8 years post baseline (estimates ranging from 0.16 to 0.26), although the autoregressive effects from 8 to 9 years (estimate = 0.14, SE = 0.09) and from 9 to 10 (estimate = 0.11, SE = 0.07) years were both nonsignificant.
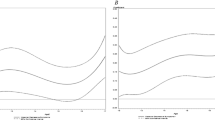
With covariates added to the ALT model for maternal depression, model fit remained strong (χ2 = 57.73, df = 70, p = 0.85, CFI = 1.00, TLI = 1.00, RMSEA = 0.00, SRMR = 0.07). Random assignment to the FCU versus control condition was significantly negatively associated with the intercept (estimate = − 0.10, SE = 0.04), showing that the FCU predicted early reductions in maternal depressive symptoms (Fig. 1a). Intervention was also positively associated with the latent slope (estimate = 0.02, SE = 0.01), indicating that FCU effects waned over time.
Mediation Models for Youth Depression
Two final models were examined that incorporated a latent growth model for youth depressive symptoms from baseline to 10 years post baseline, including latent intercept, linear slope, and quadratic slope parameters. Separate models were conducted for parent and youth reports of youth depression. Parameters for youth depression trajectories were regressed on all covariates (although the intercept was not regressed on intervention), and on the latent intercept and slope parameters for maternal depression. Strong model fit was observed for the youth report model (χ2 = 234.18, df = 156, p < 0.001, CFI = 0.98, TLI = 0.97, RMSEA = 0.02, SRMR = 0.09). Intervention assignment was not significantly related to the linear slope (estimate = 0.02, SE = 0.02) or quadratic slope (estimate = − 0.002, SE = 0.002; Fig. 1b). However, the linear rate of change in youth depression was significantly positively associated with the latent intercept of maternal depression (estimate = − 0.02, SE = 0.008). The indirect effect of the FCU intervention on the linear slope of youth-reported depression outcomes via intervention effects on the maternal depression intercept was significant (estimate = − 0.002, SE = 0.001).
Acceptable model fit was also observed for the parent-report model (χ2 = 387.50, df = 74, p < 0.001, CFI = 0.94, TLI = 0.93, RMSEA = 0.03, SRMR = 0.09). Intervention assignment was significantly related to the linear slope (estimate = − 0.05, SE = 0.02) and quadratic slope (estimate = 0.005, SE = 0.002) of youth depression (Fig. 1c), showing a significant direct effect of intervention on parent reports of youth depression that waned over time. Further, the linear rate of change in youth depression was significantly positively associated with the latent intercept of maternal depression (estimate = − 0.02, SE = 0.008). The indirect effect of the FCU intervention on the linear slope of parent reports of youth depression via intervention effects on the maternal depression intercept was significant (estimate = − 0.005, SE = 0.002).
A separate supplement results section (Supplemental Results 3) presents the same analyses but examines potential differences in intervention effects between the Early Steps sample and the PAL1 and PAL2 samples, given differences in ages across these studies. Of note, significant differences in intervention effects across trials were not observed.
Discussion
The present study examined the effects of three separate trials of the Family Check-Up on reductions in maternal depression, and further examined whether such improvements led to improvements in youth depression across early childhood and adolescence. Utilizing integrative data analysis, effects across three randomized trials of the FCU were examined, providing a powerful test of mediation across multiple samples. This work builds on the emerging literature showing the utility of IDA for leveraging existing trial data to address novel questions regarding intervention effects (Leijten et al., 2018). In the following sections, we first discuss our harmonization efforts and results, and then discuss findings of mediation analyses using harmonized estimates of parent and youth depression.
Data Harmonization
IDA presents a number of methodological novel strengths, challenges, and choices for researchers. First, prior to harmonization analyses, decisions are required at the level of front-end data aggregation. As an example, for developing the youth depression construct, we decided to focus on 17 common symptoms of depression, which was guided by diagnostic criteria and a comprehensive review of available measures and items across the trials. Subsequently, we aggregated responses to each item administered at a specific assessment point that asked about a specific symptom. This process required meticulous care reviewing each measure item by item, discussions among researchers on conceptual overlaps, and developing a comprehensive data-map connecting items to symptoms (see Connell et al., 2021).
Next, we addressed challenges involving the heterogeneity of response scales across measures (e.g., with measures using 2, 3, or 4 point scales), coupled with sometimes-sparse endorsement of responses indicating more severe symptoms. Ultimately, we addressed such issues by dichotomizing responses for youth symptoms across measures, which allowed for a streamlined process for aggregating responses across measures (a choice also employed by Curran and colleagues, 2014). Such decisions may have implications for subsequent analyses. Dichotomizing scores may result in a loss of construct variability, washing out differences related to symptom severity. These decisions are also variable-specific, and researchers engaged in complex IDA projects with multiple outcomes will need to weigh such decisions for every variable examined. For instance, these decisions were less complex in the current study for maternal depression because the same measure (i.e., CES-D) was used across trials and waves. Because the same measure was used, harmonization analyses simply included all 20 items on the measure and employed the full response scale, rather than dichotomizing scores. As IDA becomes more common, researchers might facilitate future harmonization efforts by planfully employing common measures across trials.
Once these decisions were made, harmonization analyses were conducted using MNLFA, which facilitates the examination of several aspects of differential item functioning, and ultimately provides a means to estimate constructs of interest across independent samples while accounting for DIF across covariates. Although a full discussion of these effects is beyond the scope of this paper, several illustrative results are worth highlighting. For instance, for maternal depression, several effects of youth age were observed, including age effects on the factor mean and variance, with average levels of maternal depressed mood highest for mothers of younger children, but more variable for parents of older children. Although not the primary goal of the current project, these kinds of MNLFA results may inform our understanding of the measurement of important traits of interest (such as depression) over time and across studies.
Intervention Effects
Our primary goal was to employ MNLFA to provide an overarching test of maternal depression as a mediator of the effects of the FCU on youth depression across trials. Indeed, across the three samples, we found that random assignment to the FCU was associated with reductions in maternal depressive symptoms over time. This finding for maternal depression is consistent with previous work which has shown that interventions focusing on developing parenting skills in parents of young children and adolescence have effects on parents’ sense of self-efficacy (Glatz & Koning, 2016; Wittkowski et al., 2016). Similarly, family-focused interventions aimed at improving parent–child interactions (e.g., increasing warmth, praise, positivity) may also lead to improvements in family climate and reductions in parenting stress. Improvements in parental self-efficacy and reductions in parenting stress may help to explain FCU effects on parental depression across the current studies.
However, the strongest benefits for improvements in maternal depression were observed in the early years of these trials, and declined thereafter, suggesting that improvements in maternal mood were somewhat transient across studies. It is possible that we may see an early benefit for maternal depression as parents learn new skills and feel more hopeful, which may lead to early reductions in depressive symptoms. It is also worth noting that families were offered the FCU on multiple occasions over time in each of the trials (between 6 and 9 years post baseline). It is possible that more sustained “booster sessions” of the FCU may help to maintain effects across a longer time-span.
Of note, early improvements in maternal depression still appeared to have long-lasting benefits for improvements in youth symptoms, assessed by either youth or parent report, underscoring the benefits of even shorter-term reductions in maternal symptoms. Although the direct effect of the FCU intervention differed by rater (with a significant direct effect on youth depression observed only for parental reports), a significant indirect effect of the FCU on youth depression via treatment effects on maternal depression was observed for both parent and youth reports of youth depression. These results are consistent with literature documenting maternal depression as a long-term risk for youth (Goodman et al., 2011). Moreover, the current findings highlight that prevention-related improvements in maternal depression can have long-term benefits for youth even when maternal depression was not directly targeted. Augmenting the FCU program to include booster sessions and/or more directly target maternal depression (e.g., adding mood regulation modules) may enhance these effects on parents and youth. Clinically, the effect sizes for reductions in maternal depression are generally small to moderate. However, they were achieved with a relatively brief prevention program not directly targeting parental depression, but rather targeted parental motivation and provided support for effective parenting skills. Because the parenting intervention is relatively brief, it may be widely disseminated to achieve public health benefits with respect to improvements in parental depression, even with relatively modest effect sizes.
Summary and Future Directions
The present study contains several limitations that are important to acknowledge. First, the FCU was not designed specifically to reduce depression in either parents or youth, but rather was originally designed to prevent conduct problems and substance use. The current results showed that prevention effects on maternal depression and on parent reports of youth depression waned over time. Future work may be warranted to adapt the FCU program to incorporate elements focused directly on depression (e.g., incorporating CBT elements). Second, there was substantial variability in in recruitment setting (school-based vs. WIC-recruited), in youth ages at baseline across trials, and the consistency of youth report. Although age effects and study membership were controlled for in harmonization analyses, the heterogeneity across studies may decrease the precision of intervention estimates in the current analyses. Third, all trials recruited either lower-income families (Early Steps) or from schools in lower-income neighborhoods (PAL1 and PAL2), and results may not generalize to middle and upper SES families. Fourth, a challenge exists in cleanly interpreting standard tests of mediation in randomized trials because the mediator is not generally randomly assigned (and so the mediated path may be biased due to the possible presence of unmeasured confounders; Imai et al., 2010). Future research employing newer developments in causal mediation modeling may further enhance our understanding of maternal depression as a common mediating factor across trials of the FCU. Finally, our examination of mediation was limited to parental depression, although there are likely numerous important mechanisms through which the FCU may lead to improvements youth depression, including improvements in parental support, reductions in family conflict, or improved peer relational functioning. Future research is needed to examine a broader range of mediating pathways of FCU effects on youth depression. Despite such limitations, our results provide evidence across multiple trials that improvements in maternal depression resulting from the FCU can have long-term effect on reducing youth depression.
Data Availability
Data will be made available by request, please contact Arin M. Connell.
Notes
Data will be made available by request, please contact Arin M. Connell.
In clinical trials of the FCU, the assessments are often conducted by trained research assistants, while the get-to-know-you sessions are conducted by FCU interventionists. Therefore, contrary to clinical practice, in clinical trials, the assessment precedes the get-to-know-you session in order to maintain blindness of intervention group assignment during the assessment.
References
Achenbach, T. M. (1991). Manual for the Child Behavior Checklist/4-18 and 1991 profile. University of Vermont.
Bauer, D. J., & Hussong, A. M. (2009). Psychometric approaches for developing commensurate measures across independent studies: Traditional and new models. Psychological Methods, 14, 101–125.
Benjamini, Y., & Hochberg, Y. (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, 57, 289–300.
Bollen, K. A., & Curran, P. J. (2004). Autoregressive latent trajectory (ALT) models a synthesis of two traditions. Sociological Methods & Research, 32(3), 336–383.
Brennan, L., Shelleby, E., Shaw, D., Gardner, F., Dishion, T., & Wilson, M. (2013). Indirect effects of the family check-up on school-age academic achievement through improvements in parenting in early childhood. Journal of Educational Psychology, 105(3), 762–773.
Brent, D., Kolko, D., Birhmaher, B., Bridge, J., Roth, C., & Holder, D. (1998). Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. Journal of the American Academy of Child & Adolescent Psychiatry, 37, 906–914.
Connell, A., Magee, K., Stormshak, E., Ha, T., Westling, E., Wilson, M., & Shaw, D. (2021). Long-term cross-over effects of the Family Check-Up prevention program on child and adolescent depression: Integrative data analysis of three randomized trials. Journal of Consulting and Clinical Psychology, 89, 773–782.
Connell, A., Shaw, D., Wilson, M., Danzo, S., Weaver-Krug, C., Lemery-Chalfant, K., & Dishion, T. (2019). Indirect effects of the early childhood family check-up on adolescent suicide risk: The mediating role of inhibitory control. Development and Psychopathology, 31, 1901–1910.
Connell, A., Stormshak, E., Dishion, T., Fosco, G., & Van Ryzin, M. (2018). The family check-up and adolescent depression: An examination of treatment responders and non-responders. Prevention Science, 19-(Suppl. 1), 16–26.
Connell, A. M., & Dishion, T. J. (2008). Reducing depression among at-risk early adolescents: Three-year effects of a family-centered intervention embedded within schools. Journal of Family Psychology, 22(4), 574–585.
Connell, A. M., McKillop, H. N., & Dishion, T. J. (2016). Long-term effects of the family check-up in early adolescence on risk of suicide in early adulthood. Suicide & Life-Threatening Behavior, 46(Suppl. 1), S15–S22.
Curran, P. J., McGinley, J. S., Bauer, D. J., Hussong, A. M., Burns, A., Chassin, L., Sher, K. & Zucker, R. (2014). A moderated nonlinear factor model for the development of commensurate measures in integrative data analysis. Multivariate Behavioral Research, 49(3), 214–231.
Derogatis, L. R. & Spencer, P. M. (1982). The Brief Symptom Inventory (BSI): Administration and procedures manual-1. Baltimore, MD: Johns Hopkins University School of Medicine, Clinical Psychometric Research Unit.
Dise-Lewis, J. E. (1988). The life events and coping inventory: An assessment of stress in children. Psychosomatic Medicine, 50(5), 484–499.
Dishion, T., Brennan, L., Shaw, D., McEachern, A., Wilson, M., & Jo, B. (2014). Prevention of problem behavior through annual family check-ups in early childhood: Intervention effects from home to early elementary school. Journal of Abnormal Child Psychology, 42, 343–354.
Dishion, T., & Stormshak, E. (2007). Intervening in children’s lives: An ecological, family centered approach to mental health care. American Psychological Association.
Dishion, T. J., Shaw, D., Connell, A., Gardner, F., Weaver, C., & Wilson, M. (2008). The family check-up with high-risk indigent families: Outcomes of positive parenting and problem behavior from ages 2 through 4 years. Child Development, 79(5), 1395–1414.
Easterbrooks, M. A., Kotake, C., Raskin, M., & Bumgarner, E. (2016). Patterns of depression among adolescent mothers: Resilience related to father support and home visiting program. American Journal of Orthopsychiatry, 86(1), 61–68.
Eckshtain, D., Marchette, L. K., Schleider, J., & Weisz, J. R. (2018). Parental depressive symptoms as a predictor of outcome in the treatment of child depression. Journal of Abnormal Child Psychology, 46(4), 825–837.
Eckshtain, D., Marchette, L. K., Schleider, J., Evans, S., & Weisz, J. R. (2019). Parental depressive symptoms as a predictor of outcome in the treatment of child internalizing and externalizing problems. Journal of Abnormal Child Psychology, 47(3), 459–474.
Fosco, G. M., Van Ryzin, M. J., Connell, A. M., & Stormshak, E. A. (2016). Preventing adolescent depression with the family check-up: Examining family conflict as a mechanism of change. Journal of Family Psychology, 30(1), 82–92.
Gardner, F., Shaw, D., Dishion, T., Supplee, L., & Burton, J. (2007). Randomized prevention trial for early conduct problems: Effects on proactive parenting and links to toddler disruptive behavior. Journal of Family Psychology, 21, 398–406.
Glatz, T., & Koning, I. M. (2016). The outcomes of an alcohol prevention program on parents’ rule setting and self-efficacy: A bidirectional model. Prevention Science, 17(3), 377–385.
Goodman, S. H., & Gotlib, I. H. (1999). Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review, 106(3), 458–490.
Goodman, S. H., Rouse, M. H., Connell, A. M., Broth, M. R., Hall, C. M., & Heyward, D. (2011). Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review, 14, 1–27.
Gottfredson, N., Cole, V., Giordano, M., Bauer, D., Hussong, A., & Ennett, S. (2019). Simplifying the implementation of modern scale scoring methods with an automated R package: Automated moderated nonlinear factor analysis (aMNLFA). Addictive Behaviors, 94, 65–73.
Hu, L., & Bentler, P. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55.
Hussong, A. M., Curran, P. J., & Bauer, D. J. (2013). Integrative data analysis in clinical psychology research. Annual Review of Clinical Psychology, 9(1), 61–89.
Hutchings, J., Bywater, T., Williams, M. E., Lane, E., & Whitaker, C. J. (2012). Improvements in maternal depression as a mediator of child behavior change. Psychology, 3, 795–801.
Imai, K., Keele, L., & Tingley, D. (2010). A general approach to causal mediation analysis. Psychological Methods, 15(4), 309–334. https://doi.org/10.1037/a0020761
Kessler, R. C. (2012). The costs of depression. Psychiatric. Clinics, 35(1), 1–14.
Kingsbury, M., Sucha, E., Manion, I., Gilman, S. E., & Colman, I. (2019). Adolescent mental health following exposure to positive and harsh parenting in childhood. The Canadian Journal of Psychiatry, 65(6), 392–400.
Klostermann, S., Connell, A., & Stormshak, E. A. (2016). Gender differences in the developmental links between conduct problems and depression across early adolescence. Journal of Research on Adolescence, 26(1), 76–89.
Kovacs, M. (1992). Children’s depression inventory. Multi-Health Systems.
Leijten, P., Raaijmakers, M., Wijngaards, L., Matthys, W., Menting, A., Hemink-van Putten, M., & Orobio de Castro, B. (2018). Understanding Who Benefits from Parenting Interventions for Children’s Conduct Problems: an Integrative Data Analysis. Prevention Science, 19, 579–588.
MacKinnon, D., Lockwood, C., Hoffman, J., West, S., & Sheets, V. (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7, 83–104.
Muthén, L., & Muthén, B. (2020). Mplus: The comprehensive modelling program for applied researchers: User’s guide (Version 8.4).
Pratt, L., Druss, B., Manderscheid, R., & Walker, E. (2016). Excess mortality due to depression and anxiety in the United States: Results from a nationally representative survey. General Hospital Psychiatry, 39, 39–45.
Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401.
Reuben, J., Shaw, D., Brennan, L., Dishion, T., & Wilson, M. (2015). A family-based intervention for improving children’s emotional problems through effects on maternal depressive symptoms. Journal of Consulting and Clinical Psychology, 83, 1142–1148.
Richards, D. (2011). Prevalence and clinical course of depression: A review. Clinical Psychology Review, 31(7), 1117–1125.
Shaffer, D., Fisher, P., Lucas, C. P., Dulcan, M. K., & Schwab-Stone, M. E. (2000). NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry, 39(1), 28–38.
Shaw, D. S., Dishion, T. J., Connell, A., Wilson, M. N., & Gardner, F. (2009). Improvements in maternal depression as a mediator of intervention effects on early child problem behavior. Development and Psychopathology, 21, 417–439.
Shaw, D. S., Schonberg, M., Sherrill, J., Huffman, D., Lukon, J., Obrosky, D., & Kovacs, M. (2006). Responsivity to offspring’s expression of emotion among childhood-onset depressed mothers. Journal of Clinical Child and Adolescent Psychology, 35, 540–552.
Smith, J. D., Knoble, N., Zerr, A., Dishion, T., & Stormshak, E. (2014). Family check-up effects across diverse ethnic groups: Reducing early-adolescence antisocial behavior by reducing family conflict. Journal of Clinical Child and Adolescent Psychology, 43, 400–414.
Ueno, K., & Krause, A. (2020). Occupational attainment and depressive symptoms in young adulthood. Stress and Health, 36(2), 107–118.
Van Ryzin, M. J., Fosco, G. M., & Dishion, T. J. (2012). Family and peer predictors of substance use from early adolescence to early adulthood: An 11-year prospective analysis. Addictive Behaviors, 37(12), 1314–1324.
Wang, F. L., Feldman, J. S., Lemery-Chalfant, K., Wilson, M. N., & Shaw, D. S. (2019). Family-based prevention of adolescents’ co-occurring internalizing/externalizing problems through early childhood parent factors. Journal of Consulting and Clinical Psychology, 87(11), 1056–1067.
Whisman, M., & Uebelacker, L. (2009). Prospective associations between marital discord and depressive symptoms in middle-aged and older adults. Psychology and Aging, 24, 184–189.
Wittkowski, A., Dowling, H., & Smith, D. M. (2016). Does engaging in a group-based intervention increase parental self-efficacy in parents of preschool children? A systematic review of the current literature. Journal of Child and Family Studies, 25, 3173–3191.
World Health Organization. (1997). Composite International Diagnostic Interview – Version 2.1. Geneva: World Health Organization.
Funding
This research was supported by grants from NIMH (MH122213 to Connell, Shaw, Wilson, Stormshak, Westling, & Ha), NIDA (DA25630 and DA26222 to Shaw, Dishion, and Wilson; DA07031 to Ha; and DA018374 to Stormshak), NIAAA (AA022071 to Ha), and NICHD (HD075150 to Stormshak).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
Approved by Case Western Reserve University IRB, STUDY20191414. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent to Participate
Not applicable (secondary data analysis).
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Seidman, S., Connell, A., Stormshak, E. et al. Disrupting Maternal Transmission of Depression: Using Integrative Data Analysis (IDA) to Examine Indirect Effects of the Family Check-Up (FCU) Across Three Randomized Trials. Prev Sci 24, 1523–1534 (2023). https://doi.org/10.1007/s11121-022-01471-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11121-022-01471-4