Abstract
Purpose
To assess the long-term impact of postoperative two-field-conventional radiotherapy (RT) on neurocognitive functions of adult patients with operated pituitary adenomas (PA).
Methods
We selected 124 adult patients with operated PA—56 of whom had also received RT—recorded their main clinical data and performed a neuropsychological assessment in all of them that included 15 standardized tests, and a cerebral SPECT in eight patients. Comparative analyses were carried out on major clinical and neurocognitive domains between irradiated and not irradiated patients, and on cerebral SPECT source.
Results
Compared with non-irradiated patients, irradiated patients performed significantly worse on Barcelona’s story recall test (P < 0.001) and arithmetic problems (P < 0.03) and on five categories of the Wisconsin card sorting test, especially on perseverative answers and errors (P < 0.001) without differences in other examined functional domains. RT was the only factor associated with worse results in these tests regardless other clinical and treatment-related variables. Kaplan–Meier analysis suggested that the probability of achieving poorer results with time was related to RT total dose and field-size, type of PA and age at the time of RT. Four of the five SPECTS performed in irradiated patients revealed a similar altered perfusion in the left temporal lobe cortical region.
Conclusions
In adult patients with operated PA, RT was independently associated with an impairment on verbal memory and executive function, when compared to non-irradiated patients. Our data suggest that diagnosis of acromegaly or Cushing’s disease, and age at the time of RT were able to modulate this long-term radioinduced neurocognitive sequelae.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It’s been more that 80 years since the first case of radionecrosis was reported by Fischer and Holfelder in 1930 [1], 4 years before the death of Marie Curie. During these eight decades radioinduced neurocognitive effects have been widely described in children [2, 3] but less studied in adults [4, 5], mainly due to the usually poor prognosis associated with the intracranial malignancies for which radiotherapy is required. However, there is recent evidence that limiting the volume of temporal lobe that receives high radiation doses and avoiding the hippocampus reduce the risk of radioinduced neurocognitive sequelae both in children [6] and in adults [7], and studies in mice have confirmed that radiation harmful effects are aging-dependent [8] and include microvascular and hippocampal neuronal precursor cell damage leading to neurogenic dysfunction [9, 10]. This impairment on hippocampal neurogenesis is potentially reversible [11] and restorable by specific treatments [12] that also may prevent its related neurocognitive defects [13].
Theoretically, thanks to their usually good prognosis, patients with pituitary adenomas (PA) constitute a good model to investigate long-term radioinduced neurocognitive decline in adults, but neurocognitive problems that are frequently found in these patients have not always been unequivocally attributed to the effects of radiation itself. In 1974 Luria described an amnesic syndrome in a patient with a huge pituitary tumor [14] and later Lishman suggested that cognitive defects appeared in patients with extensive suprasellar PA extension due to the compressive effect of the tumor [15]. Additionally, hormonal hypersecretion from some PA may produce cognitive and psychiatric alterations, as it was soon observed in untreated naive patients with Cushing’s disease (CD) [16, 17] and more recently in those with acromegaly (AC) [18].
It was not until late nineties when it was confirmed that patients with PA still suffered mood disturbances [19, 20] and cognitive impairments [21–26] mainly difficulties in memory and executive functions even after having been successfully treated for their tumors. Furthermore, in 2010 it was revealed that subtle memory and executive function impairments were present in patients with long-term cure of CD [27], but not of AC [28], and that psycholopathology and maladaptive personality traits were increased after long-term cure of both CD and AC [28].
Surprisingly, the results obtained during these last two decades are still contradictory with regards to a causal relationship between pituitary radiotherapy and neuropsychological changes in adult patients. Noad et al. [26] reported a greater neurocognitive impairment mainly on executive function in irradiated patients with PA when compared to those non-irradiated, but other authors were not able to prove any neurocognitive impact of pituitary radiotherapy [29, 30]. This lack of concordance could be explained by differences in the type of neuropsychological assessment used and irradiation techniques employed, and in the number and characteristics of the recruited patients, including all the variables that might influence cerebral tissue responses to radiation (like hormonal status and age at the time of radiotherapy), acting simultaneously or asynchronously as confounding factors. The main aims of the present study were to evaluate the long-term effects of postoperative two-dimensional-conventional radiotherapy (RT) on neurocognitive functions of adult patients operated for PA and explore the factors that could modulate them.
Methods
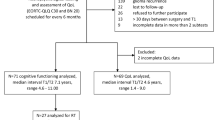
Patients
From September 2003 to January 2005 all patients with operated PA that attended their routine checkup with their endocrinologists in Puerta de Hierro University Hospital (PHUH), a tertiary referral center located in Madrid, were informed about the study and offered to participate. From the 132 who agreed, 8 met some exclusion criteria, so 124 were included in the final analysis. All patients had been operated in PHUH by the same neurosurgeon (Dr. José García-Uría) between January 1971 and January 2004 through a sublabial-rinoseptal-transsphenoidal approach. Using the microscope, a thorough and careful pituitary gland exploration was carried out, performing a total and selective adenomectomy whenever it was possible. Intraoperative findings and anatomopathologic results were recorded.
In those patients with tumoral remnant or regrowth and/or persistence of hormonal hypersecretion after transsphenoidal surgery (TS), two-dimensional conventional external beam radiotherapy using a two-parallel-lateral-opposed field technique was delivered in PHUH according to the protocol followed by the Radiation Oncology Department, using a linear accelerator that generated 18MV photons. The radiation target was defined by tumoral volume including a safety margin of 1–2 cm, with very little variations among individuals in the final total dose—that ranged from 48 to 52 Gy—and fractionation schemes. During treatment planning, no attempt was made to conformally avoid the hippocampus, that was within the radiation fields and received no <50 % of the total radiation dose. The indications of radiotherapy and irradiation techniques used changed over time, depending on the availability of medical therapies to control hormonal hypersecretion, and on the development of new neuroimaging and irradiation techniques. In the seventies and early eighties, radiotherapy was systematically indicated after TS in patients with persistence of hormonal hypersecretion, or tumor remnants, including non-functioning adenomas (NF). More individualized indications were applied afterwards, based on tumor stabilization/regrowth and response to medical treatments. Cobalt-60 radiotherapy was employed in the seventies and three dimensional conformal planning and stereotactic radiotherapy techniques were started to be used in selected patients in the late nineties in PHUH, but none of the patients included in this study were treated with these techniques. Total and fractionated radiation doses and field sizes, endocrinological evaluation results and pharmacological treatments used at diagnosis, during the follow-up and at the time of the neurocognitive assessment were registered.
Although TS was the initial treatment in most cases, dopamine agonists were first used in some patients with prolactinomas. Diabetes insipidus was diagnosed based on typical clinical symptoms and electrolyte measurements in blood and urine. Combined triple-stimulation test (LHRH, TRH, insulin) was performed until mid nineties to evaluate anterior pituitary function. Insulin-induced hypoglycemia test alone was used afterwards to examine ACTH and GH axis. In the absence of dynamic studies, GH was considered deficient if thyroid, adrenal and gonadal deficiency were present (all three) and IGF-1 levels were low for age and sex; gonadotropine deficiency was diagnosed based on low FSH/LH levels for age and sex, low estradiol/testosterone levels and hypogonadal symptoms; and persistently low TSH and free levothyroxine levels were considered indicative of TSH deficiency. All operated patients (except those with persistent CD) were discharged after TS with oral glucocorticoid coverage, that was progressively adjusted in the cases that were possible. Circadian rhythm and stress response were routinely checked in patients with CD to assess corticotroph function. Hormonal replacement therapies were systematically indicated in all patients with ADH, ACTH and TSH deficiencies, and in males and premenopausal women with gonadotropin deficiency but were not recommended for those postmenopausal women with gonadotropin deficiency and for patients with GH deficiency that previously had AC.
Inclusion criteria were age between 18 and 80 years, having been diagnosed and treated with TS for a PA, and a time interval from either RT or TS to the cognitive assessment of at least 6 months. Exclusion criteria were age under 18 or over 80 years, having been diagnosed with epilepsy, depression or any other psychiatric disorder, and having been treated with other types of radiotherapy techniques different from two-dimensional conventional radiotherapy.
Cognitive evaluation
All study participants were individually examined in the morning of their visit to PHUH with a battery of 15 standardized cognitive tests that were administered in a fixed sequence by the same specialist that was blinded to the patient’s RT status. The selection of tests was done by experts from the Neuropsychology Unit of PHUH to objectively evaluate in <60 min patients’ main cognitive functions, focusing on those most likely affected by RT, and define their clinical profile (preserved and affected capacities) and the distribution (focal or diffuse) of potential cognitive defects. It covered a wide array of cognitive functional domains, including verbal, visual and spatial memory functions, frontal lobe and executive functions, and was composed of the following tests, all of them validated for Spanish population: Mini-mental state examination (MMSE), Benton visual retention test (BVRT), Wisconsin card sorting test (WCST) and 12 subtests from “Barcelona Test” (BT). All the neuropsychological test used provided age- and education-adjusted normative data, that permitted to transform raw scores into mean centiles based on the age- and education level of each individual. Lower mean centiles implied a higher rate of errors and poorer performance in all tests.
The MMSE is a 30-point questionnaire designed by Folstein et al. in 1975 [31] that was started to be used in Spain in 1977 by Lobo et al. It objectively evaluates global cognitive functioning and abstract reasoning and also includes a first subjective question regarding the presence and severity of loss of memory as evaluated by the patient which results are recorded as raw scores (higher rate of positive answers meaning more memory problems). The BVRT assess perception, visual memory and visuoconstructive abilities. It provides a delayed recognition component and scores total correct reproductions and errors, as well as the type of errors [32]. The WCST examines executive functions and the ability to switch mental set. The presence of mainly perseverative errors/answers indicates difficulties in the ability to display flexibility in the face of changing schedules of reinforcement (set-shifting) [33]. Finally, the BT is an integrated program for global neuropsychological examination designed by Peña-Casanova [34], that contains 42 subtests, from which 12 were selected. This selection included, among others, digit span forwards and backwards, a word list learning test, verbal and reading comprehension tests, a story recall test (SRT) with immediate and delayed free and cued recalls, an arithmetic problem test (AP) and an information test.
Neuroimaging studies
Preoperative morphologic PA evaluation was usually performed using computerized tomography scan or magnetic resonance (MR), and classified PA in microdenomas (intrasellar tumors of <1 cm) and macroadenomas (tumors >1 cm). Type of expansions were also recorded, either suprasellar lateral and/or inferior. Postsurgical PA status was usually examined by postoperative MR, and classified in normal sella/postsurgical changes, intrasellar remnants, big remnants or empty sella.
Additionally, cerebral Single Photon Emission Computerized Tomography (SPECT) was done in 8 selected patients. 15 mCi (550 MBq) of 99mTc-ECD (Neurolite®) were injected intravenously. After 20–30 min of sensory rest the radioactive emission was registered in a gamma camera with a high-resolution collimator, following the protocol of the Department of Nuclear Medicine of PHUH. The images obtained after the injection of the radioisotope, representing the brain regional perfusion rate, were all informed by the same expert, that was not aware of the patients’s RT status.
Hormone assays
Serum growth hormone was measured by radioimmunoassay (RIA) after acid–ethanol extraction (Nichols Institute of Diagnostics, San-Juan Capistrano, CA) until 1988 and by immunoradiometric assay (Immunotech International) thereafter. Plasma insulin-like growth factor-1 measurement was not available before 1988. From 1989 onward it was measured by radioimmunoassay (Bioclone) and age-adjusted Z scores were calculated using values obtained in healthy subjects. Plasma corticotropin was measured by radioimmunoassay before 1989 (with kits obtaimed from Immuno Nuclear Corporation, Stillwater, Minn.) and thereafter by immunoradiometric assay (Nichols Institute D, San Juan Capistrano, Calif.). Plasma cortisol was measured by radioimmunoassay until 1992 (ICN Biomedicals, Costa Mesa, Calif., and Immunotech International, Marseille, France) and thereafter by time-resolved fluorescence immunoassay (Delfia System, Wallac, Oy, Turku, Finland). Cortisol was measured in unextracted urine at low pH by radioimmunoassay (Diagnostic Systems Laboratories, Los Angeles, and ICN Biomedicals). Serum thyrotropin was measured by immunoradiometric assay (Kodak Amerlite TSH-30 Ultrasensitive assay; Amersham International, Buckinghamshire, United Kingdom). Plasma estradiol, serum luteinizing hormone, follicle-stimulating hormone and prolactin, were measured with fluoroimmunoassays (Delfia System, Pharmacia). Radioimmunoassay was used to determine total and free levothyroxine, (LIA-mat, ByK-Sangtec), total testosterone (Radioassays System Laboratories) and free testosterone levels (Diagnostic Systems Laboratories, Texas, USA).
Statistical analysis
Data were analysed using SPSS for Windows version 14.0 (SPSS Inc., Chicago, IL). All demographic, clinical, biochemical, imaging and neurocognitive variables recorded were compared among the irradiated and non-irradiated groups. Qualitative and quantitative clinical data are usually expressed as raw values (mean ± SD) or percentages, and neurocognitive scores are reported also as age- and level of education-adjusted centiles, according to normative data scales given for each test. Hypothesis of normality for each continuous variable was tested using Kolmogorov–Smirnov and Shapiro–Wilk tests and was rejected in most laboratory measurements, in which nonparametric tests such as Mann–Whitney U test and Kruskall–Wallis one-way analysis of variance were applied. To compare quantitative data with normal distribution among two or more than two groups, t test and ANOVA test were used, respectively. Two-by-two comparisons of qualitative parameters were done applying Pearson’s Chi square test, Yates’ Chi squared test and Fisher’s exact test. Internal consistency was tested for all the 20 neuropsychological items evaluated, to select which of them summarize better the total variability of neurocognitive scores. A stepwise multiple regression analysis using the logistic model was employed and all clinical and treatment-related factors were independently evaluated by linear univariate regression analysis to assess their effect on neurocognitive performance (NP). The absolute effect of RT on NP was estimated adjusting for the type of PA and initial tumoral size. To study the effect on NP of the age at the time of RT and of time from RT to neurocognitive assessment, dispersion diagrams and regression lines were created through the lineal regression method with a 95 % prediction interval. The probability of remaining free of cognitive impairment was calculated by the Kaplan–Meier method, with a 95 % confidence interval. Cognitive impairment-free time was defined as the interval from RT to scoring equal or under the 50th centile in the cued delayed recall (CDR) item of the SRT of BT or to the date of neuropsychological evaluation for patients who achieved better results. Differences between groups were tested using the log-rank nonparametric test. The level of significance was set at P ≤ 0.05.
Ethical permission
The study maintained all data confidential, guaranteed ethical standards for this project and was approved by the Clinical Research Ethics Committee of PHUH. The aims of the study were carefully explained to the patients and written informed consent was obtained from those who agreed to participate.
Results
Demographic and clinical variables
Demographic and clinical data of the total group are summarized in Tables 1 and 2. Table 3 separately presents basic demographic and clinical characteristics of patients with AC and CD. Globally, there were 124 patients, 45 men and 79 women, aged 50.3 ± 12.8 years (20–78 years), 66 diagnosed with AC (42 non-irradiated and 24 irradiated), 33 with CD (17 non irradiated and 16 irradiated), 8 prolactinomas (PRL; 4 irradiated and 4 non-irradiated), 15 non-functioning (NF; 4 non-irradiated and 11 irradiated), 1 irradiated TSHoma, and 1 non irradiated gonadotropinoma. All patients had been treated with TS, and 56 (45 %) also with additional RT after surgery. Irradiated patients had received a mean total dose of 4964 ± 186 cGy (48–52 cGy), distributed in 25–30 fractions, with a mean dose per session of 188 cGy (1.5–2 Gy), 5 days per week.
No differences in any demographic variable were found between both groups. Only seven patients in the whole group were older than 70 years, four in the non irradiated group (ages 71, 72, 74 and 78) and three in the irradiated group (ages 72, 73 and 74). No differences were also detected in the prevalence of comorbidities, mean duration of symptoms before diagnosis, types of PA other than AC, presurgical tumoral size, type and localization of tumoral expansions at diagnosis, tumoral invasion found at surgery and disease activity at the time of the neuropsycholgical exam between both groups. However, the proportion of patients with macroadenomas described by the surgeon at surgery, postsurgical tumoral remnants, anterior pituitary deficiencies (PD), and patients operated more than once, was higher in the irradiated group. Conversely, the proportion of patients with AC, of total and selective adenomectomies reported by the surgeon, and the incidence of transient and permanent insipidus diabetes and of spinal fluid leak was higher in the non-irradiated group.
At the time of the neuropsychological assessment all patients with active disease were using at least one pharmacological treatment for controlling their hormonal hypersecretion, with no differences in the distribution of each of these drugs in both groups. Patients with active AC (Table 3) were treated with somatostatin analogues (only one irradiated patient was on pegvisomant), those with active CD (Table 3) were treated with ketoconazol, and patients with uncured PRL were on cabergoline. All of them achieved disease control at the time of the neuropsychological assessment. Although the prevalence of PD was globally higher in the irradiated group, in patients with CD, those irradiated showed a significantly lower ACTH deficiency rate when compared to non irradiated patients (20 vs. 50 %, respectively; Table 3). Even though the global prevalence of patients with at least one substituted pituitary deficiency was higher in the RT group, the percentages of treated patients for each type of deficiency were similar in both groups.
Neuropsychological results
Table 4 summarizes global neuropsychological results. Separate neuropsychological results in patients with AC and CD are detailed in Table 3. Both irradiated and non irradiated patients in the total group performed similar in BVRT, ten subtests from BT and MMSE objective evaluation. However, irradiated patients performed significantly worse than those non-irradiated in two subtests from BT (SRT and AP) and in five categories of the WCST, especially in perseverative errors (PE) and perseverative answers (PeA) and referred more frequently memory problems scoring them as more severe when they were asked to subjectively grade them during MMSE.
Internal consistency analyses revealed that the three items that summarized better the total variability of all neurocognitive scores were BT SRT CDR, WCST PE, and the subjective evaluation of loss of memory, as reported by the patients in the MMSE. Multivariate regression analysis and one-by-one separate univariate comparisons by subgroups using these items, confirmed that the deleterious effect of RT on NP persisted independently of other clinical and treatment-dependent variables. RT was the only factor that remained significantly associated with worse results in both items. Significant correlations were found between tumoral size at diagnosis, postoperative remnants and the presence of PD, so these variables could not be included in the multivariate regression analysis. One-by-one separate univariate comparisons of BT SRT CDR centile scores by subgroups according to type of PA, disease status, presence of each type of PD at the time of the study and size of postoperative remnants, are presented in Fig. 1a, b, c and d, respectively. All the analysis by subgroups demonstrated lower neuropsychological scores in irradiated patients when compared to non-irradiated and the same profile of impairments found in the whole irradiated group (specific defects in verbal memory and executive function with preservation of other neurocognitive capacities). Patients with CD showed the greatest differences in both items among RT and non-RT groups, followed by patients with AC and NF PA. On the other hand, irradiated patients operated more than once obtained better scores than those operated only in one occasion, but still significantly worse than non-irradiated treated with more than one surgery. Average decrements of −32 points in BT STR CDR, and of −18 points in WCST PE centile scores, respectively, were estimated for irradiated patients when compared to non-irradiated, regardless the subgroup evaluated.
Box plot comparisons of mean cued delayed recall centiles obtained in the story recall test of the Barcelona test between irradiated and non irradiated groups according to: a type of PA, b disease status (cured vs. not cured), c presence or absence of pituitary deficiencies (any axis vs. no deficiency) and d neuroimaging tumoral evaluation after surgery. SRT, story recall test; RT, radiotherapy; AC, acromegaly; CD, Cushing’s disease; PRL, prolactinoma; NF, non-functioning pituitary adenoma; MR, magnetic resonance; NS, normal sella/postsurgical changes; IR, intrasellar tumoral remnants, BR; big tumoral remnants; ES, empty sella
In the irradiated group, box plot comparisons and Kaplan–Meier survival curves revealed that patients treated with higher radiation doses and larger RT field sizes (defined by size of postoperative remnants) developed poorer results and earlier in time (Fig. 2a, b). Data regarding age at the time of RT and time intervals from diagnosis and RT to neurocognitive assessment, and from TS to RT are presented in Table 5. No linear correlation was found between any of these variables and NP in the whole irradiated group. Nevertheless, separate analysis in irradiated patients with AC and CD to examine the influence on NP of time interval from RT to neurocognitive assessment, and of age at RT, revealed the presence of opposed correlations in these subgroups. More time since RT and younger age at RT correlated with poorer NP in CD patients and better NP in patients with AC, respectively. Survival curves in patients with AC and CD confirmed different patterns of NP decline depending on the type of PA and age at RT (Fig. 2c, d). Patients with AC showed a differential speed of NP deterioration depending on the age at RT, with a slower and milder NP worsening in those irradiated before 40 years of age when compared to those irradiated afterwards. On the contrary, younger patients with CD showed sooner and sharper NP deterioration. These differential cognitive decline profiles present in irradiated patients were not found in non-irradiated patients, and RT was proved to be their differentiating factor.
Kaplan–Meier estimates of the cumulative probability of scoring above 50th percentile on cued delayed recall of the SRT of the Barcelona test in the irradiated group after RT according to: a total radiation dose, b neuroimaging tumoral evaluation after surgery, c age at the time of RT in patients with AC, and d age at the time of RT in patients with CD
Spects
Cerebral SPECT results are presented in Table 6. They revealed a higher rate of perfusion defects in the irradiated patients (4/5, 80 vs. 1/3, 30 %). Nonetheless, due to the small sample size statistical analysis was not applicable. Curiously, cortical involvement was present in all the four SPECTs informed as abnormal among irradiated patients, whereas it was absent in the abnormal SPECT found among non-irradiated patients.
Discussion
To our knowledge, this study is the largest of its kind reported to date, the only one in which conventional radiotherapy was delivered using two-parallel-lateral-opposed fields, a feature that enhanced its ability to correlate neurocognitive results with specific disrupted neural networks, and the first conducted in Spanish population. The distinctive cognitive profile demonstrated in irradiated patients—an RT-related impairment on verbal memory and executive function with preservation of other examined functional domains—pointed at a specific damage of the neural pathways located in the temporal lobes, hippocampus and prefrontal cortex (involving the limbic system), the areas crossed by RT beams.
Interestingly, Kaplan–Meier curves in irradiated patients with AC suggested the possibility of a progressive recovery of radioinduced cerebral damage with time and/or a more efficient response to this injury in adult younger patients with AC, that is in accordance with previous experimental studies. A differential age-related response to radiation [8] and a protective effect of GH/IGF-1 on cerebral microcirculation and hippocampal neurogenesis that enhances functional brain recovery after radiotherapy and progressively disappears with age have already been demonstrated in young adult mice [35]. In contrast to patients with AC, those with CD showed poorer NP, and their age at RT had less impact on it. The effects of hypercortisolism on hippocampus [36] with proinflammatory and atherosclerotic processes affecting microvasculature impede neurogenesis even in younger brains, so a poorer recovery capacity in irradiated patients with CD may be expected regardless their age. Taken together, the results found in our analyses support firmly the suspected causal link between RT and an specific dysfunction on hippocampus and temporal lobes, but also suggest the presence of a dynamic process in which several damage/reparative mechanisms of different nature and efficacy depending on individual variables—like hormonal status and age at the time of RT—are activated after RT and interact simultaneously modulating its final effect on NP in each patient. Moreover, these individual differences could in part explain the lack of concordance among previous studies regarding long-term cognitive effects of pituitary radiotherapy in patients with PA.
Adrenal insufficiency has been linked with attention impairments [37] and high levels of corticosteroids have been demonstrated to have a differential impact on memory performance depending on the balanced activation of different types of corticosteroid receptors [38]. However, the specific cognitive profile we found in the global irradiated group (including the 32 irradiated patients with ACTH deficiency) has not been described as a result of either adrenal insufficiency or hydrocortisone replacement regimens. Besides, the low rate of ACTH deficient irradiated patients with CD (only three patients) ruled out a potential influence of glucocorticoid overdosage and/or ACTH deficiency on the NP of irradiated patients with CD. On the other hand, the main aim of our study was to unmask and eventually describe the cognitive long-term impact of conventional RT in the whole RT group. The influence of the type of adenoma became evident only after detailed statistical subanalysis, so further larger prospective studies specifically designed to define the exact differences among acromegalic and Cushing’s patients responses to pituitary irradiation over time, and the impact of each PD—especially of ACTH deficiency—on NP are required.
Pituitary radiotherapy has been used for more than a century [39] and it can effectively achieve tumor control in 70–90 % of patients at 20 years [40, 41]. However, it has been linked with a number of long-term significant complications including hypopituitarism, cerebrovascular disease, malignant brain tumors [42, 43], damage to the optic chiasm [44], radionecrosis [45] and mortality [46, 47]. Neuropsychological radioinduced changes have also been suggested in several studies, but rarely firmly proved [21–26]. Apart from ours, the only study that has objectively assessed neurocognitive function in a large group of patients with different types of operated PA and compared the results obtained from irradiated to those from non-irradiated patients was the one by Noad et al. [26]. In accordance to our results, it described a greater cognitive impairment in the irradiated group, in this case mainly on executive function, but six main differences exist between Noad’s and our work. First, total group size was smaller than ours (71 patients vs. 124 in our study) which limited its statistical power; second, it excluded patients with CD whereas we enrolled patients with all types of PA, including CD; third, a three-field irradiation technique with two beams projected laterally and one frontally (superior oblique) instead of a two-parallel-lateral-field method was used; fourth, the mean total dose was lower (45 Gy instead of 49.6 Gy); fifth, it included a shorter follow-up period since primary TS (10 vs. 33 years in our study); and sixth, it did not evaluate any effect of the age at radiotherapy and of time since radiation on NP.
A similar design was employed by Van Beek et al. [29] in 2007 but, in contrast to Noad’s and to our study, they only included patients with NF PA and neurocognitive results were obtained from questionnaires sent by postal mail to all patients. Although the differences weren’t statistically significant they also found lower memory scores in irradiated patients. Five years later, Brummelman et al. [30] in 75 patients with NF PA showed that there were no significant differences on NP between the three-, four-, and five-field irradiated groups and the non-irradiated patient group. It is noteworthy that no significant associations between pituitary radiotherapy and incidence of second tumors [48], mortality [48], and stroke [49] were found by other groups of the same medical center, unlike the results of many works performed in different centers [42, 43, 46, 47].
Despite their usually good prognosis, long-term care of patients with PA, that commonly remains in the hands of their endocrinologists, requires a fine understanding and early recognition of cognitive impairments. Radioinduced cognitive sequelae are still easily undervalued and even misdiagnosed by clinicians, but they may have a major negative impact on dailylife, as it was subjectively reported by our patients in the MMSE. According to our results, past history of two-field irradiation, might be taken into account as a potential cause of progressive cognitive impairments when evaluating patients with PA in the long-term. The identification of those features that confer a higher risk for developing radioinduced neurocognitive dysfunction may help in individualizing clinical management. In irradiated high-risk patients, an early control of hypercortisolism should be encouraged together with an intensification of preventive measures to delay cerebral atherosclerosis progression [12, 50], including optimization of hypertension, diabetes, hyperlipidemia and obesity treatments, and promotion of a healthy lifestyle [51]. Cognitive rehabilitation exercises should also be recommended to enhance cerebral neuroplasticity [52–56], but the use of specific medications [12, 13] still needs more research to be indicated. Our study also establishes the accuracy of BT SRT, proving it to be a highly sensitive and fast screening test to detect radioinduced cognitive problems in our population. WCST could be used as second line, since its PeA and PE scores correlated well with BT SRT results. The distinctive pattern observed in the cerebral SPECT performed in irradiated patients suggests its potential utility as a screening tool to rule out other causes of cognitive decline like depression or dementia, and avoid inappropriate treatments. In addition, our findings reinforce the current recommendation to select modern conformal stereotactic radiation techniques and to conformally avoid the hippocampus [5–7, 50].
The main limitations of the present study are its retrospective cross-sectional design, the use of a group of non-irradiated patients as control group, and the lack of premorbid information on cognitive function and of longitudinal prospective neuropsychological assessments. Nonetheless, these limitations do not diminish the value of our results. While the use of two-field-conventional radiotherapy is now almost completely abandoned (in PHUH more than a decade ago), many patients that are still followed in endocrinology clinics were treated in the past with this radiotherapeutic technique. Therefore, in this clinical setting, a retrospective design is the only possible approach to examine its long-term cognitive impact. The large size and diverse composition of the total group (with all types of PA), patients selection method, homogeneity of treatment protocols employed always by the same teams in the same Hospital, and the absence of differences in all demographic and many major clinical variables among non-irradiated and irradiated patients made our series especially suitable for the study, and facilitated case and control groups direct comparisons. Those clinical and treatment-related variables that differed among irradiated and non-irradiated groups, other than cognitive scores, were separately and carefully analyzed, to evaluate their potential impact on NP as confounding factors, overcoming this limitation. The detailed statistical analysis was able to demonstrate that the specific deleterious effect of RT on NP persisted independently of the influence of all the examined factors. Furthermore, the large period of time covered by the study (33 years) enables it to examine potential effects of time on NP through the creation of survival curves. This aspect had not been analyzed before and could be considered another strength of our study, together with the scarcity of long-term cognitive data from adults patients treated with cranial radiotherapy for other primary or metastatic conditions. During the almost one decade that was required for data recovery and categorization, and extensive sequential statistical analysis, the evolvement of treatments for patients with PA, especially with acromegaly, has definitely changed their management in the majority of centers. But some of the lessons extracted from the past by our study might well be used to anticipate the future of our current patients and of those to come worldwide.
Conclusions
Postoperative pituitary RT in adult patients operated for a PA was associated with a dose and field-size related impairment on verbal memory and executive function when compared to non-irradiated patients, that was not detectable by general cognitive tests and couldn’t be explained by differences in any variable other than RT. However, age at the time of RT and pre-existing hormonal status (type of PA) were able to modulate it. Early prevention-using stereotactic radiation techniques and avoiding hippocampus-, detection- with BSRT and WCST- and individualized management of this specific neurocognitive decline will be essential to improve the long-term quality of life of patients with PA in the future.
References
Fischer AW, Holfelder H (1930) Lokales amyloid im gehirn. Dtsch Z Chir 227:475–483
Meadows AT, Gordon J, Massari DJ, Littman P, Fergusson J, Moss K (1981) Declines in IQ scores and cognitive dysfunctions in children with acute lymphocytic leukaemia treated with cranial irradiation. Lancet 2:1015–1018
Moore IM, Kramer JH, Wara W, Halberg F, Ablin AR (1991) Cognitive function in children with leukemia. Effect of radiation dose and time since irradiation. Cancer 68:1913–1917
Glosser G, McManus P, Munzenrider J, Austin-Seymour M, Fullerton B, Adams J, Urie MM (1997) Neuropsychological function in adults after high dose fractionated radiation therapy of skull base tumors. Int J Radiat Oncol Biol Phys 38:231–239
Abayomi OK (2002) Pathogenesis of cognitive decline following therapeutic irradiation for head and neck tumors. Acta Oncol 41:346–351
Redmond KJ, Mahone EM, Terezakis S, Ishaq O, Ford E, McNutt T, Kleinberg L, Cohen KJ, Wharam M, Horska A (2013) Association between radiation dose to neuronal progenitor cell niches and temporal lobes and performance on neuropsychological testing in children: a prospective study. Neuro-oncology 15:360–369
Gondi V, Hermann BP, Mehta MP, Tomé WA (2013) Hippocampal dosimetry predicts neurocognitive function impairment after fractionated stereotactic radiotherapy for benign or low-grade adult brain tumors. Int J Radiat Oncol Biol Phys 85:348–354
Schindler MK, Forbes ME, Robbins ME, Riddle DR (2008) Aging-dependent changes in the radiation response of the adult rat brain. Int J Radiat Oncol Biol Phys 70:826–834
Coderre JA, Morris GM, Micca PL, Hopewell JW, Verhagen I, Kleiboer BJ, van der Kogel AJ (2006) Late effects of radiation on the central nervous system: role of vascular endothelial damage and glial stem cell survival. Radiat Res 166:495–503
Monje ML, Mizumatsu S, Fike JR, Palmer TD (2002) Irradiation induces neural precursor-cell dysfunction. Nat Med 8:955–962
Ben Abdallah NM, Slomianka L, Lipp HP (2007) Reversible effect of X-irradiation on proliferation, neurogenesis, and cell death in the dentate gyrus of adult mice. Hippocampus 17:1230–1240
Monje ML, Toda H, Palmer TD (2003) Inflammatory blockade restores adult hippocampal neurogenesis. Science 302:1760–1765
Yazlovitskaya EM, Edwards E, Thotala D, Fu A, Osusky KL, Whetsell WO Jr, Boone B, Shinohara ET, Hallahan DE (2006) Lithium treatment prevents neurocognitive deficit resulting from cranial irradiation. Cancer Res 66:11179–11186
Luria AR (1976) The neuropsycology of memory. John Wiley, New York
Lishman WA (1987) Organic psychiatry: the psychological consecuences of cerebral disorders. Blackwell, Oxford
Starkman MN, Schteingart DE (1981) Neuropsychiatric manifestifications of patients with Cushing’s syndrome. Arch Intern Med 141:215–219
Dorn LD, Burgess ES, Dubbert B, Simpson SE, Friedman T, Kling M, Gold PW, Chrousos GP (1995) Psychopathology in patients with endogenous Cushing’s syndrome: atypical or melancholic features. Clin Endocrinol 43:433–442
Leon-Carrion J, Martin-Rodriguez JF, Madrazo-Atutxa A, Soto-Moreno A, Venegas-Moreno E, Torres-Vela E, Benito-López P, Gálvez MA, Tinahones FJ, Leal-Cerro A (2010) Evidence of cognitive and neurophysiological impairment in patients with untreated naive acromegaly. J Clin Endocrinol Metab 95:4367–4379
Peace KA, Orme SM, Sebastian JP, Thompson AR, Barnes S, Ellis A, Belchetz PE (1997) The effect of treatment variables on mood and social adjustment in adult patients with pituitary disease. Clin Endocrinol 46:445–450
Page RC, Hammersley MS, Burke CW, Wass JA (1997) An account of the quality of life of patients after treatment for non-functioning pituitary tumours. Clin Endocrinol 46:401–406
Grattan-Smith PJ, Morris JG, Shores EA, Batchelor J, Sparks RS (1992) Neuropsychological abnormalities in patients with pituitary tumours. Acta Neurol Scand 86:626–631
McCord MW, Buatti JM, Fennell EM, Mendenhall WM, Marcus RB Jr, Rhoton AL, Grant MB, Friedman WA (1997) Radiotherapy for pituitary adenoma: long-term outcome and sequelae. Int J Radiat Oncol Biol Phys 39:437–444
Peace KA, Orme SM, Padayatty SJ, Godfrey HP, Belchetz PE (1998) Cognitive dysfunction in patients with pituitary tumour who have been treated with transfrontal or transsphenoidal surgery or medication. Clin Endocrinol 49:391–396
Peace KA, Orme SM, Thompson AR, Padayatty S, Ellis AW, Belchetz PE (1997) Cognitive dysfunction in patients treated for pituitary tumours. J Clin Exp Neuropsychol 19:1–6
Guinan EM, Lowy C, Stanhope N, Lewis PD, Kopelman MD (1998) Cognitive effects of pituitary tumours and their treatments: two case studies and an investigation of 90 patients. J Neurol Neurosurg Psychiatry 65:870–876
Noad R, Narayanan KR, Howlett T, Lincoln NB, Page RC (2004) Evaluation of the effect of radiotherapy for pituitary tumours on cognitive function and quality of life. Clin Oncol 16:233–237
Tiemensma J, Kokshoorn NE, Biermasz NR, Keijser BJ, Wassenaar MJ, Middelkoop HA, Pereira AM, Romijn JA (2010) Subtle cognitive impairments in patients with long-term cure of Cushing’s disease. J Clin Endocrinol Metab 95:2699–2714
Tiemensma J, Biermasz NR, van der Mast RC, Wassenaar MJ, Middelkoop HA, Pereira AM, Romijn JA (2010) Increased psychopathology and maladaptive personality traits, but normal cognitive functioning, in patients after long-term cure of acromegaly. J Clin Endocrinol Metab 95:E392–E402
van Beek AP, van den Bergh AC, van den Berg LM, van den Berg G, Keers JC, Langendijk JA, Wolffenbuttel BH (2007) Radiotherapy is not associated with reduced quality of life and cognitive function in patients treated for nonfunctioning pituitary adenoma. Int J Radiat Oncol Biol Phys 68:986–991
Brummelman P, Sattler MG, Meiners LC, Elderson MF, Dullaart RP, van den Berg G, Koerts J, Tucha O, Wolffenbuttel BH, van den Bergh AC, van Beek AP (2012) Cognitive performance after postoperative pituitary radiotherapy: a dosimetric study of the hippocampus and the prefrontal cortex. Eur J Endocrinol 166:171–179
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Benton AL (1945) A visual retention test for clinical use. Arch Neurol Psychiatry 54:212–216
Nelson HE (1976) A modified card sorting test sensitive to frontal lobe defects. Cortex 12:313–324
Peña-Casanova J, Guardia J, Bertran-Serra I, Manero RM, Jarne A (1997) Shortened version of the Barcelona test (I): subtests and normal profiles. Neurologia 12:99–111
Aberg ND, Brywe KG, Isgaard J (2006) Aspects of growth hormone and insulin-like growth factor-I related to neuroprotection, regeneration, and functional plasticity in the adult brain. Sci World J 6:53–80
Pruessner M, Pruessner JC, Hellhammer DH, Bruce Pike G, Lupien SJ (2007) The associations among hippocampal volume, cortisol reactivity, and memory performance in healthy young men. Psychiatry Res 155:1–10
Klement J, Hubold C, Hallschmid M, Loeck C, Oltmanns KM, Lehnert H, Born J, Peters A (2009) Effects of glucose infusion on neuroendocrine and cognitive parameters in Addison disease. Metabolism 58:1825–1831
Tytherleigh MY, Vedhara K, Lightman SL (2004) Mineralocorticoid and glucocorticoid receptors and their differential effects on memory performance in people with Addison’s disease. Psychoneuroendocrinology 29:712–723
Beclere J (1909) The radiotherapeutic treatment of tumours of the hypophysis, gigantism and acromegaly. Arch Roentgen Ray 3:114
Brada M, Rajan B, Traish D, Ashley S, Holmes-Sellors PJ, Nussey S, Uttley D (1993) The long-term efficacy of conservative surgery and radiotherapy in the control of pituitary adenomas. Clin Endocrinol 38:571–578
Estrada J, Boronat M, Mielgo M, Magallón R, Millan I, Díez S, Lucas T, Barceló B (1997) The long-term outcome of pituitary irradiation after unsuccessful transsphenoidal surgery in Cushing’s disease. N Engl J Med 336:172–177
Erfurth EM, Bülow B, Mikoczy Z, Svahn-Tapper G, Hagmar L (2001) Is there an increase in second brain tumours after surgery and irradiation for a pituitary tumour? Clin Endocrinol 55:613–616
Brada M, Ford D, Ashley S, Bliss JM, Crowley S, Mason M, Rajan B, Traish D (1992) Risk of second brain tumour after conservative surgery and radiotherapy for pituitary adenoma. BMJ 304:1343–1346
Millar JL, Spry NA, Lamb DS, Delahunt J (1991) Blindness in patients after external beam irradiation for pituitary adenomas: two cases ocurring after small daily fractional doses. Clin Oncol 3:291–294
al-Mefty O, Kersh JE, Routh A, Smith RR (1990) The long-term side effects of radiation therapy for benign brain tumours in adults. J Neurosurg 73:502–512
Ayuk J, Stewart PM (2009) Mortality following pituitary radiotherapy. Pituitary 12:35–39
Burman P, Mattsson AF, Johannsson G, Höybye C, Holmer H, Dahlqvist P, Berinder K, Engström BE, Ekman B, Erfurth EM, Svensson J, Wahlberg J, Karlsson FA (2013) Deaths among adult patients with hypopituitarism: hypocortisolism during acute stress, and de novo malignant brain tumors contribute to an increased mortality. J Clin Endocrinol Metab 98:1466–1475
Sattler MG, van Beek AP, Wolffenbuttel BH, van den Berg G, Sluiter WJ, Langendijk JA, van den Bergh AC (2012) The incidence of second tumours and mortality in pituitary adenoma patients treated with postoperative radiotherapy versus surgery alone. Radiother Oncol 104:125–130
Sattler MG, Vroomen PC, Sluiter WJ, Schers HJ, van den Berg G, Langendijk JA, Wolffenbuttel BH, van den Bergh AC, van Beek AP (2013) Incidence, causative mechanisms, and anatomic localization of stroke in pituitary adenoma patients treated with postoperative radiation therapy versus surgery alone. Int J Radiat Oncol Biol Phys 87:53–59
Armstrong CL, Gyato K, Awadalla AW, Lustig R, Tochner ZA (2004) A critical review of the clinical effects of therapeutic irradiation damage to the brain: the roots of controversy. Neuropsychol Rev 14:65–86
Naylor AS, Bull C, Nilsson MK, Zhu C, Björk-Eriksson T, Eriksson PS, Blomgren K, Kuhn HG (2008) Voluntary running rescues adult hippocampal neurogenesis after irradiation of the young mouse brain. Proc Natl Acad Sci USA 105:14632–14637
Ramón YCS (1952) Structure and connections of neurons. Bull Los Angel Neuro Soc 17:5–46
Morris RG, Anderson E, Lynch GS, Baudry M (1986) Selective impairment of learning and blockade of long-term potentiation by an N-methyl-d-aspartate receptor antagonist, AP5. Nature 319:774–776
Bliss TV, Collingridge GL (1993) A synaptic model of memory: long-term potentiation in the hippocampus. Nature 361:31–39
Hallbergson AF, Gnatenco C, Peterson DA (2003) Neurogenesis and brain injury: managing a renewable resource for repair. J Clin Investig 112:1128–1133
Ma DK, Jang MH, Guo JU, Kitabatake Y, Chang ML, Pow-Anpongkul N, Flavell RA, Lu B, Ming GL, Song H (2009) Neuronal activity-induced Gadd45b promotes epigenetic DNA demethylation and adult neurogenesis. Science 323:1074–1077
Acknowledgments
We thank all patients for their collaborative participation in this study and Ana Ruiz, José Ortiz Berrocal, and Rosa Magallón for their help in selecting the battery of neurocognitive tests, SPECT performance and interpretation, and radiotherapy data collection, respectively.
Conflict of interest
The authors have nothing to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lecumberri, B., Estrada, J., García-Uría, J. et al. Neurocognitive long-term impact of two-field conventional radiotherapy in adult patients with operated pituitary adenomas. Pituitary 18, 782–795 (2015). https://doi.org/10.1007/s11102-015-0653-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-015-0653-6