Abstract
Oral estrogens reduce GH-induced IGF-1 production and preliminary studies have shown that adjuvant estroprogestin (EP) therapy with octreotide LAR may control disease activity in some female patients who are partially responsive to octreotide LAR. Our aim was to verify if EP alone or in combination with octreotide LAR can achieve remission of acromegaly in selected cases of patients uncontrolled by surgery. Eleven women with persistent active acromegaly following surgery participated in this unblinded open label pilot study. Their mean age was 49.8 ± 4.3 years. Two patients were drug naïve, two patients had stopped octreotide LAR because of intolerance and seven were treated with octreotide LAR. The patients received either EP (EP pill, 20 μg ethinylestradiol, 100 μg levonorgestrel) alone (4 patients) or added to octreotide LAR (7 patients). Fasting GH, IGF-1, glucose, HDL- and LDL-cholesterol, and triglycerides were measured at baseline and at last visit. MRI was controlled at baseline and at last visit. Duration of estrogen treatment was 3.1 ± 0.5 years. Serum IGF-1 levels were normalized in 8/11 patients (73%). Serum GH concentrations did not change significantly during treatment (11.6 ± 5.6 μg/L prior to EP vs 5.5 ± 1.2 μg/L following EP). In patients treated with EP alone, remission was achieved in 2/4 patients (IGF-1 percentages of the upper limit of normal age-matched range (%ULN): 211 ± 40% before EP compared to 95 ± 15% after EP, P = 0.028). In the seven patients treated by EP added to octreotide LAR, remission was achieved in 6 patients (IGF-1%ULN: 158 ± 9% before EP compared to 86 ± 4% after EP, P = 0.0003). Glucose and cholesterol levels were unchanged by EP treatment (data not shown). MRI did not show any evidence of tumour progression with EP in patients who had a tumour remnant. In conclusion, oral estrogen treatment appears to normalize serum IGF-1 concentrations in over 70% of women with acromegaly uncured by surgery irrespective of their sensitivity to octreotide LAR. We suggest that estrogens may be a temporary cost-effective and safe treatment for women with postoperative persistent acromegaly.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Morbidity and mortality of acromegaly are associated with elevated serum levels of growth hormone (GH) and Insulin-like Growth Factor-1 (IGF-1) [1]. The aim of treatment is to reduce mortality, relieve symptoms, control tumour growth and ensure biochemical control or cure [2]. Neurosurgical resection of GH-secreting adenomas is the first-line treatment of acromegaly. The best reported cure rates for micro- and macroadenomas are 80–90 and 50–60%, respectively [3]. Because macroadenomas represent approximately 75% of GH-secreting adenomas, the surgical overall cure rate rarely exceeds 50%. Medical treatment of acromegaly, with somatostatin analogues (SSA), often used in surgical failures, can lead to normalized GH and IGF-1 levels, relief of symptoms and tumour shrinkage [4]. However, SSA provide biochemical control in approximately 50% of patients [5, 6]. Other available pharmacological drugs for treatment of acromegaly include dopamine agonists and GH receptor antagonists. The dopamine receptor agonist, cabergoline, may be useful alone or combined with somatostatin agonists in a minority of patients [7, 8]. The GH receptor antagonist, pegvisomant, has a greater efficacy [9], but its use is limited by its elevated cost.
Over 30 years ago, administration of high doses of estrogens to patients with acromegaly has been shown to improve the symptoms of acromegaly, glucose tolerance and to reduce the serum concentration of bioassayable somatomedin [10–12]. This treatment was later disregarded because of the high incidence of side effects from high-dose estrogen treatment. The doses of ethinylestradiol of 0.5–1 mg used are 30–50 times those currently used in oral contraceptives preparations. There has been only one report in the literature on the beneficial effects of low dose estrogens in eight women with acromegaly [13].
We report additional longer follow-up experience on the evaluation of the effects of estroprogestins (EP) alone or added to octreotide LAR on clinical and biochemical control of acromegaly in selected cases of female patients uncured by surgery.
Patients and methods
Patients
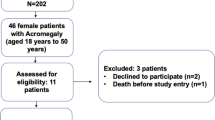
Between September 2004 and February 2008, female patients with acromegaly uncured by surgery and followed at our pituitary clinic were invited to participate in this open pilot study. Inclusion criteria were: (1) active acromegaly with GH nadir >1 μg/L during a standard 75 g 2 h oral glucose tolerance test (OGTT) and elevated age-adjusted IGF-1 level, at least 6 months after surgery or 3 years following radiation therapy. Exclusion criteria were: (1) residual pituitary tumours with suprasellar expansion, (2) any labelled contraindications to estrogens such as past or present thrombophlebitis, cerebro- or cardiovascular disease, breast cancer and uncontrolled arterial hypertension. Eleven consecutive patients participated in this study and were followed until January 2010. Their mean age was 49.8 ± 4.3 years (range 33–78). All patients had been previously treated by neurosurgical resection of GH-secreting adenomas (at least 1 year prior to the study) and two had received subsequent radiotherapy (at least 3 years prior to the study). Four had regular menstruations, one patient had hypogonadotropic hypogonadism without estrogen replacement at study entry and the remaining patients were post-menopausal. All patients had breast and gynaecologic examination prior to study. In addition, post-menopausal women had normal mammograms. Two patients were drug naïve because they were unwilling to be treated with SSA and nine were treated with octreotide LAR (Sandostatin LAR®, Novartis Pharmaceutical Canada Inc.). Of these, two patients had stopped octreotide LAR at least 3 months before the study because of abdominal discomfort, whereas seven patients who had sub-optimal IGF-1 reduction maintained octreotide LAR at the maximally effective or tolerated dose (20 mg every 4 weeks in four patients and 30 mg/4 weeks in five) throughout the study (Table 1). No patient had been taking estrogens in the 5 years preceding study entry.
Protocol
Written informed consent was obtained from each patient before inclusion. The study was approved by the Ethics committee of our institution. All patients received daily EP pill (20 μg ethinylestradiol, 100 μg levonorgestrel: Alesse®, Wyeth-Ayerst, Montreal, Canada). In four patients (#1–4, Table 1) EP was the only treatment for acromegaly; seven patients (#5–11, Table 1) had EP added to octreotide LAR treatment.
Methods
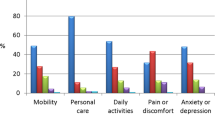
Symptom scores for headaches, sweating, arthralgia, fatigue and paresthesia were graded 0 (absent), 1 (mild), 2 (moderate) and 3 (severe) by the same observer at baseline and at 6 months.
Fasting GH and IGF-1 were determined at baseline and at last visit by immunoradiometric assays (IRMA) using commercial kits from Cis-Bio. Fasting serum glucose, HDL- and LDL-cholesterol, and triglycerides were measured at baseline and at last visit, by using commercial enzymatic kits. Pituitary MRI was controlled at baseline and at last visit.
Statistical analysis
Data were expressed as mean ± SEM. IGF-1 values were expressed as absolute values and as percentages of the upper limit of the normal age-matched (IGF-1%ULN) values. Data were analyzed using parametric (paired t-test) and non-parametric (Mann–Whitney) tests and Spearman correlation test.
Results
Individual clinical scores and biochemical data of eleven women with persistent acromegaly after surgery, before and following treatment with EP, are shown in Table 1. Mean duration of EP treatment was 3.1 ± 0.5 years (range, 0.5–5 years). Mean symptom score decreased significantly from 7.4 to 4 at the last visit. Overall mean absolute serum levels of IGF-1 (%ULN) were significantly reduced from 569 ± 42 μg/L (199 ± 15%) to 246 ± 17 μg/L (89 ± 5%) (P < 0.0001). Serum IGF-1 levels were normalized in 8/11 patients (73%) (Fig. 1). In the three remaining patients, IGF-1 levels decreased from 230 ± 50% to 112 ± 6%. Two of these patients had IGF-1 within 110% ULN (#1 and 10, Fig. 1). The third patient was not controlled with EP and was unwilling to receive SSA (#2, Fig. 1). Serum GH concentrations did not change significantly during treatment (11.6 ± 5.6 μg/L prior to EP in comparison with 5.5 ± 1.2 μg/L following EP). In patients treated with EP alone, remission was achieved in 2/4 patients (IGF-1%ULN: 211 ± 40% before EP compared to 95 ± 15% after EP, P = 0.028). In the seven patients treated by EP added to octreotide LAR, remission was achieved in 6 patients (IGF-1%ULN: 158 ± 9% before EP compared to 86 ± 4% after EP, P = 0.0003). IGF-1 normalization was not correlated with initial levels of GH (between 0.85 and 55 μg/L) and IGF-1 (between 165% ULN- 327% ULN). Glucose and cholesterol levels were unchanged by EP treatment (data not shown). Gynaecologic examinations and mammograms of postmenopausal women performed yearly during this study were normal.
Pituitary MRI showed residual intrasellar microadenomas in nine patients of whom 4 had cavernous sinus invasion; and no evidence of remnant tumour in one patient. One patient had no MRI, however, a postoperative pituitary CT-scan showed no residual tumour. MRI did not show any evidence of tumour progression with EP in patients who had a tumour remnant.
Discussion
Our study showed that long-term oral estroprogestin given as monotherapy or in addition to monthly octreotide LAR was effective in disease control in 91% of women with postoperative persistent acromegaly. Clinical control of the disease was significantly improved in all patients. Serum IGF-1 levels were normalized in 73% of the patients. These results confirm and extend previous findings by Cozzi et al. [13] who reported the effects of a triphasic pill (ethynil-estradiol 30–40–30 μg/day and desogestrel 50–70–100 μg/day) treatment for 13 ± 7 months on GH/IGF-1 control in 8 women with acromegaly; three of them resistant to medical treatment. In that study, IGF-1 decreased in six patients (75%) and normal values were reached in four (50%) without any change in GH levels. In our study, chronic EP administration for a mean period of over 3 years showed sustained reduction of IGF-1 without evidence of tachyphylaxis, GH change or remnant pituitary tumour progression. In our study population, the observed IGF-1 reduction was similar in pre- and postmenopausal women, thus independently of the gonadal status. Moreover, the normalization of IGF-1 levels appeared to be independent of initial levels of GH and IGF-1. It is well known that high levels of endogenous (during pregnancy) or exogenous estrogens can improve symptoms of acromegaly and reduce serum levels of IGF-1. The mechanism of IGF-1 suppressive action by estrogens remains elusive. It is clearly not mediated by GH decrease as shown by the study of Cozzi et al. [13] and ours. There is some evidence that estrogens modulate GH action, through effects exerted on the liver, based on the observations that oral but not transdermally administered estrogens impair metabolic actions of GH. It is also known that estrogens influence responsiveness to GH replacement therapy in adults. The liver is a sex-responsive organ, as well as the major site of GH-regulated metabolism and the principle source of IGF-1. Some studies showed that high estrogen concentrations impair hepatic IGF-1 synthesis, as well as the acid labile subunit (ALS) that colocalized with IGF-1 in hepatocytes. The effects of estrogens on IGFBP3 synthesized in Kuppfer cells are less consistent. In our study, IGFBPs and ALS were not measured. In addition, estrogens increase the secretion of GHBP in humans by an unknown mechanism and contribute to IGF-1 decrease. Finally, estrogens attenuate GH action by suppressing GHR function, through the JAK/STAT pathway via the upregulation of SOCS proteins (see for review Leung [14]). In our study, IGF-1 decrease with unchanged GH levels was accompanied by a significant improvement in acromegaly symptoms. Although GH may still exert direct actions on various tissues, we did not observe any GH-mediated deleterious effects of EP on serum glucose and lipid levels with the dosage and duration of treatment used in this study. Other parameters, such as bone markers, were not assessed in our study. Although the effect of estrogens is at the periphery level, we did not observe any radiological evidence of tumor remnant progression in our series. One of the main concerns with estroprogestins use in postmenopausal women rests in the associated long-term risks. There was an increased risk of coronary events in the first years of use in the over-seventies age group. In the younger age groups (50–59 years), there was a trend towards reduction of risk and a significant reduction in all-cause mortality. The dose of estrogen was postulated to be a contributing factor [15, 16]. Moreover, the use of estroprogestin therapy is also associated with an increased risk for breast cancer after 3 years of use [17].
The overall remission rate of acromegaly is approximately 75% of patients after surgery and/or SSA. Therefore, a significant proportion of patients remains uncontrolled and need further therapy, such as cabergoline, pegvisomant and radiotherapy. Our results suggest that EP may be an alternative cost-effective therapy for women with persistent acromegaly after surgery. In light of safety considerations, women for whom this therapy could be considered should be aged less than 60 years and the EP treatment duration should be determined on an individual benefit-risk assessment.
References
Holdaway IM, Bolland MJ, Gamble GD (2008) A meta-analysis of the effect of lowering serum levels of GH and IGF-I on mortality in acromegaly. Eur J Endocrinol 159(2):89–95
Melmed S, Colao A, Barkan A et al (2009) Guidelines for acromegaly management: an update. J Clin Endocrinol Metab 94(5):1509–1517
Nomikos P, Buchfelder M, Fahlbusch R (2005) The outcome of surgery in 668 patients with acromegaly using current criteria of biochemical ‘cure’. Eur J Endocrinol 152(3):379–387
Melmed S, Sternberg R, Cook D et al (2005) A critical analysis of pituitary tumor shrinkage during primary medical therapy in acromegaly. J Clin Endocrinol Metab 90(7):4405–4410
Melmed S (2006) Medical progress: acromegaly. N Engl J Med 355(24):2558–2573
Vallette S, Serri O (2008) Octreotide LAR for the treatment of acromegaly. Expert Opin Drug Metab Toxicol 4(6):783–793
Abs R, Verhelst J, Maiter D et al (1998) Cabergoline in the treatment of acromegaly: a study in 64 patients. J Clin Endocrinol Metab 83(2):374–378
Cozzi R, Attanasio R, Lodrini S, Lasio G (2004) Cabergoline addition to depot somatostatin analogues in resistant acromegalic patients: efficacy and lack of predictive value of prolactin status. Clin Endocrinol (Oxf) 61(2):209–215
Trainer PJ, Drake WM, Katznelson L et al (2000) Treatment of acromegaly with the growth hormone-receptor antagonist pegvisomant. N Engl J Med 342(16):1171–1177
Mccullagh EP, Beck JC, Schaffenburg CA (1955) Control of diabetes and other features of acromegaly following treatment with estrogens. Diabetes 4(1):13–23
Hamwi GJ, Skillman TG, Tufts KC Jr (1960) Acromegaly. Am J Med 29:690–699
Clemmons DR, Underwood LE, Ridgway EC, Kliman B, Kjellberg RN, Van Wyk JJ (1980) Estradiol treatment of acromegaly. Reduction of immunoreactive somatomedin-C and improvement in metabolic status. Am J Med 69(4):571–575
Cozzi R, Barausse M, Lodrini S, Lasio G, Attanasio R (2003) Estroprogestinic pill normalizes IGF-I levels in acromegalic women. J Endocrinol Invest 26(4):347–352
Leung KC, Johannsson G, Leong GM, Ho KK (2004) Estrogen regulation of growth hormone action. Endocr Rev 25(5):693–721
Panay N (2009) Estrogen dose: the cardiovascular impact. Climacteric 12(Suppl 1):91–95
Stevenson JC, Hodis HN, Pickar JH, Lobo RA (2009) Coronary heart disease and menopause management: the swinging pendulum of HRT. Atherosclerosis 207(2):336–340
Lyytinen H, Pukkala E, Ylikorkala O (2009) Breast cancer risk in postmenopausal women using estradiol-progestogen therapy. Obstet Gynecol 113(1):65–73
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vallette, S., Serri, O. Oral estroprogestin: an alternative low cost therapy for women with postoperative persistent acromegaly?. Pituitary 13, 311–314 (2010). https://doi.org/10.1007/s11102-010-0236-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-010-0236-5