Abstract
Background Concurrent opioid and benzodiazepine use (“double-threat”) and opioid, benzodiazepine, and muscle relaxant use (“triple-threat”) are linked to increased adverse events compared to opioid use alone. Objectives To assess prevalence of double-threat and triple-threat in the US and to measure association between double- and triple-threat and emergency department visits. Setting Nationally representative, 2-year health database of the United States. Method A retrospective cohort study was conducted using the national medical expenditure panel survey. Two-year prevalence of combination use was measured. Association between 2013–2014 double- and triple-threat exposure and emergency department visit compared to non-users, opioid-users, and all other exposure combinations assessed using logistic regression. Main outcome measures Survey-weighted prevalence of triple-threat and double-threat in 2013 and 2014 was measured. The outcome variable of at least one emergency department visit in a study year was utilized for the logistic regression. Results Opioids, benzodiazepines, and muscle relaxants were used in 11.9% (38.4 million lives), 4.2% (13.5 million), and 3.4% (10.9 million) individuals respectively in 2013, and 12.2% (39.3 million), 4.6% (14.8 million), and 3.6% (11.6 million), respectively in 2014. Prevalence of individuals on double-threat rose from 1.6 to 1.9% from 2013 to 2014. Triple-threat prevalence was unchanged at 0.53% in that interval. Triple-threat patients had increased emergency department visit probability with ORs of 9.19 (95% CI 9.17–9.22) in 2013, 9.82 (95% CI 9.79–9.85) in 2014, and 5.90 (95% CI 5.89–5.92) for longitudinal 2013–2014 analysis compared to non-users. Double-threat patients had increased emergency department visit probability with ORs of 4.57 (95% CI 4.56–4.58) in 2013, 6.66 (95% CI 6.65–6.68) in 2014, and 4.49 (95% CI 4.48–4.50) for 2013–2014 analysis compared to non-users. Conclusions Concurrent opioid and benzodiazepine use and opioid, benzodiazepine, and muscle relaxant use increased probability of emergency department visit. Amplified efforts in surveillance, prescribing, and default follow-up for concurrent opioid, benzodiazepine, muscle relaxant use are needed to reduce this public health concern.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impacts on practice
-
Patients on double-threat and triple-threat are significantly more likely to experience an emergency department visit than those not taking opioids or taking an opioid, benzodiazepine, or muscle relaxant, individually.
-
Review of patients’ medication records should always be performed before adding these medications and a longitudinal plan to attempt deprescribing must be defined if care necessitates concurrent usage of these agents.
Introduction
The Centers for Disease Control and Prevention (CDC) reported that more than 400,000 opioid-related overdose deaths occurred between 1999 and 2017 in the US [1]. To put that number in perspective, it is roughly the number of American fatal casualties in world war II and is more than six times the number of American fatalities in the Vietnam war [2, 3]. The rate of overdoses continues to grow each year reaching 70,237 deaths in 2017 alone [1]. While it is well understood that opioids increase risk of death due to respiratory depression, concurrent consumption of other types of depressants of the central nervous system (CNS) synergize dampening of the respiratory system and the associated lethality of opioids [4]. Benzodiazepines are a known health concern with abuse potential due to sedating properties, associated dependency, and withdrawal symptoms upon rapid discontinuation [5]. While the risks of benzodiazepines have become clearer, the number of benzodiazepine prescriptions has continued to increase unabated with the number of adults who filled a benzodiazepine prescription growing 67% between 1996 and 2013 [6]. In a large study of more than 300,000 subjects prescribed opioids with continuous coverage between 2001 and 2013, the percentage of persons also prescribed benzodiazepines rose to 17% in 2013 from 9% in 2001 [7]. These trends continue despite the most recent CDC guideline for prescribing opioids for chronic pain that explicitly recommended against co-prescribing of opioids and benzodiazepines [8]. Similar to benzodiazepines, muscle relaxants such as carisoprodol, cyclobenzaprine, and metaxalone pose a risk when co-administered with opioids due to CNS depression and synergistic respiratory depressive pharmacodynamics [9]. While muscle relaxants have been documented to increase risk for central nervous system-related morbidity and mortality, a recent payer-perspective utilization analysis found that more than 32% of injured workers prescribed an opioid were also taking a muscle relaxant. In this analysis, the percentage simultaneously taking an opioid with a muscle relaxant exceeded the proportion taking both an opioid and a benzodiazepine (10.5%) [10].
The federal National Institute on Drug Abuse of the National Institutes of Health reported that greater than thirty percent of opioid induced overdoses involved concurrent use of a benzodiazepine [1]. The concurrent use of opioids, benzodiazepines, and muscle relaxants for the treatment of chronic conditions has been associated with increased adverse events compared to opioids alone [11, 12]. Analysis that examined the additive risk of opioids for benzodiazepine users found a 24–55% increased risk of serious adverse events for those consuming both types of medications compared to those using benzodiazepines alone [13]. Due to the synergistic deleterious effect when opioids and benzodiazepines are prescribed simultaneously, both the Food and Drug Administration (FDA) and CDC have issued boxed warnings for concurrent prescribing of opioids and benzodiazepines [8, 11]. However, quantification of the increased likelihood of emergency department visit for those taking concurrent opioid and benzodiazepine use (commonly called “double-threat”) and opioid, benzodiazepine, and muscle relaxant use (“triple-threat”) in a nationally representative longitudinal database has not been completed [14].
Study aims
The goals of this study were to utilize US. Department of Health & Human Services (HHS) medical expenditure panel survey (MEPS) data to quantify the national prevalence of concurrent opioid and benzodiazepine use (commonly called “double-threat”) and opioid, benzodiazepine, and muscle relaxant use (“triple-threat”) [14, 15]. MEPS is drawn from a nationally representative subsample of households that completed the National Health Interview Survey (conducted by the National Center for Health Statistics) in the prior year. Conducting interviews in the household, MEPS collects information for each person in the household on use of medical services including prescription drug usage [16].
Secondary study objectives were to assess longitudinal association of double-threat and triple-threat with emergency department (ED) visits. The incremental relationship on ED visit likelihood in patients on “triple-threat” and “double-threat” compared to those on opioids, benzodiazepines, and muscle relaxants was also assessed in the US population.
Ethics approval
This retrospective database study project #160343XX was issued exempt status by the UC San Diego Human Research Patient Protections Program Institutional Review Board.
Method
Data assembly
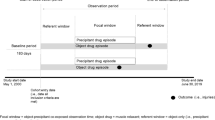
The 2013 and 2014 MEPS-Panel 18 longitudinal data from HHS and the affiliated 2013 and 2014 prescribed medicines file were utilized for this analysis [15]. The cohort surveyed in MEPS has been weighted to be reflective of the US population. The demographic and healthcare utilization data were obtained from a MEPS combined file consisting of healthcare utilization data for the study years. The pooled file was analyzed for longitudinal trends in benzodiazepine, opioid, and muscle relaxant usage and utilized to quantify the association between double and triple-threat usage with the outcome of ED visit.
Longitudinal analysis of benzodiazepine, opioids, and muscle relaxant usage
The medication files were combined with longitudinal MEPS-Panel 18 by matching subject numbers. The panel-based approach of MEPS involves survey completion for reach respondent at three standardized intervals per year. Each of these intervals is referred to as a “round”. Multiple prescriptions of the same drug prescribed per patient within a designated round were summed together to obtain total day supply per round based on average daily dose. Medications without dose or medication quantity were excluded from this analysis.
Prevalence estimation of “double-threat” and “triple-threat”
Using the final pooled analysis data set, concurrent use of muscle relaxants, benzodiazepines, and/or opioids were categorized as either “double-threat” and/or “triple-threat.” Thus, those on triple-threat included those on double-threat for the purpose of the prevalence estimations. Final national prevalence estimations of muscle relaxant, benzodiazepine, opioid, double-threat and triple-threat usage were calculated using affiliated population survey weights.
Association of high risk medication exposure with emergency department visits
Analyses were performed to quantify the association between double and triple-threat to ED within the same year (2013) and the following year of medication exposure. We measured the likelihood with the normalized outcome of odds ratio (OR) of ED visit due to exposure of any single study medication or combinations of study medications using a designated reference group.
Statistical analysis plan
Multiple logistic regression was performed to measure association quantified as ORs of medication exposures with the outcome of ED visit. Study subjects were categorized into exposure groups as non-users (non-use of opioids, benzodiazepines, or muscle relaxants), opioid users, benzodiazepine users, muscle relaxant users, “double-threat” users, and “triple-threat” users. For the purposes of regression analysis estimations, all exposure groups were mutually exclusive. In separate regression models, the reference groups were varied to determine the incremental increase in odds of ED visit for each exposure group compared to a specified control category. Chi-squared tests were applied for changes in proportions of medication use. Analyses were conducted using RStudio® 1.1.5 (Boston, MA) with α-level < 0.05 for all comparisons.
Results
Prevalence analysis
A total of 16,715 respondents in MEPS survey-weighted to represent 321 million people living in the US. A total of 49 (0.5%) medication records were dropped from the analysis due to absence of quantity. Opioids, benzodiazepines, and muscle relaxants were prescribed in 11.9% (38.4 million lives), 4.2% (13.5 million), and 3.4% (10.9 million), respectively, of the individuals in 2013, and 12.2% (39.3 million), 4.6% (14.8 million), and 3.6% (11.6 million), respectively in 2014. In 2013, 1.6% of the population were on double-threat and 0.53% of the population were on triple-threat. In 2014, 1.9% of the population were on double-threat while the population on triple-threat remained at 0.53%.
Of the total 9961 medication records for study medications, 62.3% were opioids, 21.9% were benzodiazepines, and 15.8% were muscle relaxants. From 2013 to 2014, the average days’ supply per patient in 2013 for opioids was 18.9 days and in 2014 was 19.2 days. From 2013 to 2014, the average days’ supply per patient was 39.9 days in 2013 and 41.7 days in 2014 for benzodiazepines. Muscle relaxants average days’ supply in 2013 was 27.8 days and 2014 was 31.8 days.
Triple-threat and double-threat comparison to non-opioid users
Patients on either double-threat or triple-threat were at increased probability of emergency department visits compared to non-users. Analysis revealed patients on triple-threat had an increased probability for ED visits with ORs of 9.19 (95% CI 9.17–9.22) for the 2013 analysis, 9.82 (95% CI 9.79–9.85) for the 2014 analysis, and 5.90 (95% CI 5.89–5.92) for longitudinal 2013–2014 analysis compared to non-users. Patients on double-threat had an increased probability for ED visits with ORs of 4.57 (95% CI 4.56–4.58) for 2013 analysis, 6.66 (95% CI 6.65–6.68) for 2014 analysis, and 4.49 (95% CI 4.48–4.50) for longitudinal 2013–2014 analysis compared to non-users (Table 1).
Triple-threat and double-threat comparison to opioid alone users
Patients on triple-threat had increased odds for ED visits compared to those taking opioids alone with OR of 2.20 (95% CI 2.19–2.20), 1.73 (95% CI 1.72–1.73), and 3.02 (95% CI 3.01–3.03) for years 2013, 2014, and 2013–2014 longitudinal analysis. Patients on double-threat had increased odds for ED visits compared to those taking opioids alone with OR of 1.09 (95% CI1.09–1.10), 1.17 (95% CI 1.17–1.17), and 2.30 (95% CI 2.29–2.30) for years 2013, 2014, and 2013–2014 longitudinal analysis (Table 1).
Triple-threat to double-threat comparison
Compared to patients on double-threat, patients on triple-threat had statistically significant increased odds of ED visits of 2.01 (95% CI 2.00–2.02), 1.47 (95% CI 1.47–1.48), and 1.31 (95% CI 1.31–1.32) for years 2013, 2014, and 2013–2014 longitudinal analysis respectively (Table 1).
Discussion
This is the first comprehensive analysis using a longitudinal US nationally-representative database of the additive likelihood of an ED visit outcome for patients with concurrent use of opioids, benzodiazepines, and muscle relaxants. While a limited number of studies have attempted to describe the pharmacology behind the increased toxicity with combined use of opioids, benzodiazepines and muscle relaxants, no comprehensive clinical utilization studies have been conducted [6, 17, 18]. Results using this validated 2013–2014 longitudinal survey showed that patients on triple-threat are at enhanced probability for ED visits compared to non-users and to those on double-threat.
This study demonstrated a year upon year increase in patients concurrently using opioids and benzodiazepines. The proportion using all three study medications of opioids, benzodiazepines, and muscle relaxants was consistent from 2013 to 2014. This analysis demonstrated patients on triple-threat had a minimum 9.19-fold increased odds for experiencing a same year ED visit compared to non-users. Double-threat patients had a minimum 4.57-fold increased odds for experiencing a same year ED visit compared to non-users. Users of triple-threat and double-threat were more likely to have an ED visit compared to users of opioids alone. Triple-threat and double-threat patients were at elevated probability of ED visit compared to opioid users. This study showed users of triple-threat and double-threat were statistically more likely to experience an ED visit than users of any one of the study medications of opioids, benzodiazepines, or muscle relaxants. As would be expected, triple-threat patients had an increased probability of ED visit compared to double-threat patients.
Given the increased association of a catastrophic outcome with concurrent use of these medications, it is important to amplify processes to reduce unnecessary use. Several state-wide protocols and regulations have been established to reduce the potential misuse of these medications. For example, The state of California has established a mandatory system to document and survey patients’ dispensed controlled substances. The controlled substance utilization review and evaluation system (CURES) is a prescription drug monitoring program in California that documents patients’ prior dispensed controlled medication to give healthcare providers a resource to monitor for potential medication abuse. Since the implementation of this system, CURES has been integrated in both hospital and outpatient pharmacies [19]. Although CURES documents the patterns of patients’ prescribed medications, it does not alert the provider nor pharmacy of any concurrent use of high-risk medications [20]. Thus, medication reconciliation involving these medications relies on prescriber awareness and discretion. With the demonstrated association now defined, prescription drug monitoring programs should be bolstered to alert prescribers and pharmacists automatically when double-threat and triple-threat prescribing has occurred.
Manifold other approaches are now being initiated to reduce high-risk medication use. Some states in the US have developed approaches to minimize opioid and benzodiazepine associated risks applying other types of monitoring systems [21,22,23]. Several managed care organizations have implemented medical electronic alerts as surveillance strategies to improve medication safety [24,25,26]. Other experts have suggested that extending monitoring to at-risk special populations, such as older adults, would greatly aid in individualizing the medication regimen to prevent additive toxicity. The Centers for Medicare & Medicaid Services (CMS) has planned on finalizing new policies for 2019 to prevent opioid overuse [27]. Expansion and coordination of surveillance efforts at the state and national level in the US would likely harmonize healthcare systems and decrease gaps in care coordination.
Review and identification of past or existing double-threat and triple-threat medication therapy should be completed prior to the initiation of any new opioid, benzodiazepine, or muscle relaxant for all patients. This may involve usage of prescription drug monitoring programs if present or review of available administrative claims data to detect potentially offending medications. Ideally, an automated prompt in the electronic health record itself would inform the prescriber of the synergistic risk of adding the agent to the current regimen. For patients that are candidates for double-threat or triple-threat therapy based on the evidence, the clinician care plan should entail automatic follow-up on at least a monthly basis to ensure validated, longitudinal measurement of symptom outcomes and attempts at gradual dose reduction or de-prescribing. Pharmacist-to-patient consultation to ensure patient understanding of treatment goals, potential risks, adverse events, including availability of opioid overdose reversal agents such as naloxone, must also be completed. While this analysis focused on the US population, the enhanced probability of an emergent outcome is pertinent in any global region where these medications exist. The US is currently beleaguered by a fragmented health care system that disrupts prescription data coordination. However, the presence of regional and national prescription data in many countries offer the prospect of enhanced monitoring of concurrent use of high-risk medications that could benefit for prevalence and trend measurement.
Limitations
This is a survey-based analysis and thus potentially subject to study respondent error or recall bias. For this analysis, the 2-year panel-design of the MEPS longitudinal database allows assessment of association between exposure and outcome rather than a causal linkage between them. While the longitudinal analysis from 2013 exposure of double-threat and triple-threat to 2014 ED visit outcome provides firmer correlation between possible cause-and-effect, the relationship cannot be fully characterized in this database. That given, MEPS is a validated database sponsored by the Agency for Healthcare Research and Quality of HHS and routinely used for national estimation by researchers and the federal government [28].
Conclusions
Double-threat and triple-threat exposure are associated with increased probability for an emergency department visit compared to non-users. Improved monitoring to preclude unnecessary use and planned longitudinal follow-up to attempt deprescribing of combination use of opioids, benzodiazepines, and muscle relaxants for each patient is critical to reduce consumption of these agents and the translational harm these medications produce.
References
Abuse NI on D. Overdose death rates. 2019 [cited 2019 Sep 12]. Available from: https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates.
Research starters: worldwide deaths in world war II. Natl. WWII Mus. New Orleans. [cited 2019 Sep 12]. Available from: https://www.nationalww2museum.org/students-teachers/student-resources/research-starters/research-starters-worldwide-deaths-world-war.
Vietnam war US. Military fatal casualty statistics. Natl. Arch. 2016 [cited 2019 Sep 12]. Available from: https://www.archives.gov/research/military/vietnam-war/casualty-statistics.
Chou R, Fanciullo GJ, Fine PG, Adler JA, Ballantyne JC, Davies P, et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(113–130):e22.
Schmitz A. Benzodiazepine use, misuse, and abuse: a review. Ment Health Clin. 2016;6:120–6.
Bachhuber MA, Hennessy S, Cunningham CO, Starrels JL. Increasing benzodiazepine prescriptions and overdose mortality in the United States, 1996–2013. Am J Public Health. 2016;106:686–8.
Sun EC, Dixit A, Humphreys K, Darnall BD, Baker LC, Mackey S. Association between concurrent use of prescription opioids and benzodiazepines and overdose: retrospective analysis. BMJ. 2017;356:j760.
CDC guideline for prescribing opioids for chronic pain-United States, 2016. MMWR Recomm Rep. 2016 [cited 2019 Sep 16];65. Available from: https://www.cdc.gov/mmwr/volumes/65/rr/rr6501e1.htm..
van Tulder MW, Touray T, Furlan AD, Solway S, Bouter LM, Cochrane Back Review Group. Muscle relaxants for nonspecific low back pain: a systematic review within the framework of the cochrane collaboration. Spine. 2003;28:1978–92.
Concerns with concurrent therapy | Express scripts. [cited 2019 Apr 17]. Available from: https://lab.express-scripts.com/lab/insights/workers-compensation/concerns-with-concurrent-therapy.
Horsfall JT, Sprague JE. The pharmacology and toxicology of the ‘holy trinity’. Basic Clin Pharmacol Toxicol. 2017;120:115–9.
Relationship between concomitant benzodiazepine-opioid use and adverse outcomes among US veterans.. [cited 2019 Sep 16]. Available from: https://reference.medscape.com/medline/abstract/29189516.
Day C. Benzodiazepines in combination with opioid pain relievers or alcohol: Greater risk of more serious ED visit outcomes. CBHSQ Rep. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2013 [cited 2019 Sep 16]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK384672/.
State of Missouri Department of Social Services. Authorization Form for Anti-Anxiety Benzodiazepine usage. https://dss.mo.gov/mhd/cs/pharmacy/pdf/AntianxietyBenzodiazepines.pdf.
Medical expenditure panel survey home. [cited 2018 Oct 3]. Available from: https://meps.ahrq.gov/mepsweb/index.jsp.
Medical expenditure panel survey background. [cited 2019 Sep 22]. Available from: https://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp.
Research C for DE and. New safety measures announced for opioid analgesics, prescription opioid cough products, and benzodiazepines. FDA. 2019 [cited 2019 Sep 20]; Available from: https://www.fda.gov/drugs/information-drug-class/new-safety-measures-announced-opioid-analgesics-prescription-opioid-cough-products-and.
McDonald DC, Carlson K, Izrael D. Geographic variation in opioid prescribing in the US. J Pain. 2012;13:988–96.
Controlled substance utilization review and evaluation system. State Calif.-Dep. Justice-Off. Atty. Gen. 2016 [cited 2019 Sep 18]. Available from: https://oag.ca.gov/cures.
Munzing T. Physician guide to appropriate opioid prescribing for noncancer pain. Perm J. 2017 [cited 2019 Sep 18];21. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5424587/.
2017pdmpannualreport.pdf. [cited 2019 Sep 19]. Available from: https://www.floridahealth.gov/statistics-and-data/e-forcse/funding/2017pdmpannualreport.pdf.
Illinois-opioid-action-plan-Sept-6-2017-FINAL.pdf. [cited 2019 Sep 19]. Available from: https://dph.illinois.gov/sites/default/files/publications/Illinois-Opioid-Action-Plan-Sept-6-2017-FINAL.pdf.
Model-prescription-monitoring-program-PMP-Act.pdf. [cited 2019 Sep 18]. Available from: https://namsdl.org/wp-content/uploads/Model-Prescription-Monitoring-Program-PMP-Act.pdf.
United States Department of Health and Human Services. Center for Medicaid and CHIP Services Informational Bulletin. Best Practices for Addressing Opioid Overdoses, Misuse, and Addiction. https://www.medicaid.gov/sites/default/files/Federal-Policy-Guidance/Downloads/cib-02-02-16.pdf.
Theriault BM, Burger CF, Schlesinger JJ. EMR implementation of default opioid prescription quantities. J Gen Intern Med. 2018;33:1827.
Malte CA, Berger D, Saxon AJ, Hagedorn HJ, Achtmeyer CE, Mariano AJ, et al. Electronic medical record alert associated with reduced opioid and benzodiazepine coprescribing in high-risk veteran patients. 2018 [cited 2019 Sep 19]. Available from: https://www.ingentaconnect.com/content/wk/mcar/2018/00000056/00000002/art00010.
2019 Medicare advantage and part D rate announcement and call letter | CMS. [cited 2019 Sep 20]. Available from: https://www.cms.gov/newsroom/fact-sheets/2019-medicare-advantage-and-part-d-rate-announcement-and-call-letter.
Cohen SB, Cohen JW. The capacity of the medical expenditure panel survey to inform the affordable care act. Inq J Health Care Organ Provis Financing. 2013;50:124–34.
Acknowledgements
Dr. Watanabe receives support from the Health Resources and Services Administration (HRSA) of the US. Department of Health and Human Services (HHS) under Grant U1WQHP28726, “Geriatrics Workforce Enhancement Program.” Dr. Watanabe receives research support from the State of California Tobacco-Related Disease Research Program Award No. 588100 and from the National Academy of Medicine Anniversary Pharmacy Fellowship Program. He also receives support from the National Academy of Medicine Emerging Leaders in Health and Medicine Scholars program. This information, content, and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS, or the US. government, the state of California, or the National Academies of Sciences, Engineering, and Medicine.
Funding
This study received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Watanabe, J.H., Yang, J. Association of combination opioid, benzodiazepine, and muscle relaxant usage with emergency department visits in a nationwide cohort in the United States. Int J Clin Pharm 43, 358–364 (2021). https://doi.org/10.1007/s11096-020-01012-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-020-01012-5