Abstract
Objective The aim of this study is to describe recommendations made by clinical pharmacists when co-managing hypertension with physicians. Setting Two family medicine clinics at a major teaching hospital in the mid-western United States. Method This report details the specific recommendations made by pharmacists during a prospective randomized controlled clinical trial. Patients with uncontrolled hypertension were enrolled in a 9-month intensive pharmacist–physician co-management study. Clinical pharmacists saw patients at baseline, 2, 4, 6, and 8 month visits. Optional visits were allowed between required visits. Main outcome measure For this analysis, pharmacist recommendations were grouped. Physician acceptance of the pharmacists’ recommendations was also evaluated. Results Data from 101 patients were included and analyzed in this study. Changes in drug therapy were recommended 267 times for these 101 patients. Most recommendations for a change in treatment involved adding a new antihypertensive medication (46.4%) or increasing a dose (33.3%). The majority of pharmacist recommendations to modify drug therapy were made at the baseline visit (41.6%), with 76.8% of recommendations made by the 2 month visit. Physicians accepted and implemented 95.9% of the 267 pharmacist recommendations to modify drug therapy. Pharmacists recommended no change in the treatment plan 361 times, most often because the patient’s blood pressure (BP) had achieved the goal. Average BP decreased from 153.1 ± 10.0/84.9 ± 12.0 mmHg (average ± SD) at baseline to 124.2 ± 9.7/74.7 ± 9.6 mmHg (P < 0.001) at the end of 9 months, with 89.1% (P < 0.001) of patients reaching their BP goal. Conclusion Pharmacist recommendations for alterations in drug therapy generally occurred early in the course of the study and were largely to intensify therapy through higher dosages or additional medications. Pharmacist–physician co-management of BP is effective at reducing BP and improving BP control rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impact of findings on practice
-
Pharmacist recommendations are effective in improving patient outcomes in hypertension.
-
Widespread physician–pharmacist co-management of hypertension may be one way to improve BP control rates and reduce negative cardiovascular outcomes.
Introduction
Hypertension is an increasingly common health problem throughout the world [1, 2]. It is estimated that hypertension currently affects more than 1 billion people worldwide [2]. Hypertension is known to increase the risk of heart attack, heart failure, stroke, and kidney disease [3]. In fact, uncontrolled blood pressure (BP) accounts for 7.1 million deaths worldwide each year [2]. Controlling BP with antihypertensive agents can reduce strokes by 35–40%, myocardial infarctions by 20–25%, and heart failure by more than 50% [3].
Despite the clear benefits of adequate treatment, hypertension remains prevalent and BP control rates remain unacceptably low. The Canadian Heart Health Surveys determined that hypertension was undetected in almost half of all hypertensive Canadians and only 13% of hypertensive people surveyed were treated and controlled [4]. The British Heart Foundation Statistics Database reports that over 70% of hypertensive patients in England are not receiving treatment and of the 30% that are being treated, only 40% are controlled [5]. In the United States, it is estimated that 37% of hypertensive patients are at their BP goal [6]. Control rates were reported to be less than 40% in Spain [7]. Although poor hypertension recognition and control appears universal, better control rates are possible. Numerous controlled clinical trials have achieved BP control rates as high as 70–80% with close follow-up and forced drug titration [8–12]. However, clinical trials are highly structured (efficacy studies) and control rates of 70–80% are not reflective of real life (effectiveness).
Limited access to care and poor patient adherence are two common reasons cited for poor BP control [3, 13]. However, Hyman and Pavlik recently found that most cases of uncontrolled hypertension occur in patients over 65 years of age who have access to health care and who have frequent contact with physicians [14]. Two other studies have confirmed that BP remained poorly controlled despite up to six physician visits per year [15, 16]. Oliveria et al. found that patient factors (adherence, patient acceptance, regimen complexity) were uncommon barriers to BP control cited by physicians or patients [16]. The primary barrier (91% of patient visits) was related to physicians who were satisfied with BP values that were not at recommended goals. It is becoming clear that practitioner acceptance of uncontrolled BP is a significant factor in poor control rates.
One approach to improving BP control is to involve clinical pharmacists in the care of patients with hypertension [9, 12, 17–32]. Numerous studies have shown that involving clinical pharmacists in the care of patients with a variety of conditions is widely accepted by physicians and improves patient outcomes [33–36]. In addition, several studies have found that the involvement of clinical pharmacists in treating patients with hypertension leads to better BP results in clinics as well as community pharmacies [9, 12, 17–32]. However, the specific therapy changes made during pharmacist interventions and the types of strategies used by clinical pharmacists to improve BP control are not well described.
Aim of the study
The aim of this study is to describe the types of recommendations made by pharmacists to co-manage BP in a group of patients with uncontrolled hypertension in two Family Medicine Clinics.
Methods
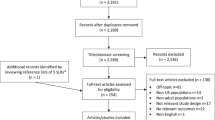
This study was part of a larger study designed to test whether BP could be better controlled with physician/pharmacist collaborative teams compared to usual care [37]. This report details the specific recommendations made by pharmacists during a prospective randomized controlled clinical trial. Patients in the control group did not have interactions with clinical pharmacists, so the present report only included patients from the two family medicine clinics that served as intervention sites for the larger study. For these analyses all intervention patients were included.
Patients included in the main study were recruited from the current patient population seen at the clinics. Patients had to have seen their primary physician on at least two previous visits thus having an established relationship. All patients were seen in these two family medicine clinics. Patient inclusion and exclusion criteria are provided in Table 1. Potential study patients were recruited in one of three ways. Research nurses screened medical records of hypertensive patients and contacted those who met study criteria. Additionally, research nurses screened daily appointment lists for patients with hypertension. Finally, physicians could refer patients to the study. Only patients under the care of physicians on the family medicine faculty were included.
Five clinical pharmacists participated in the study. All pharmacists were appointed as faculty or residents in the two family medicine clinics. Each pharmacist had at a minimum of a Doctor of Pharmacy degree and one year of a primary care residency in Family Medicine. The study protocol specified that the clinical pharmacist conduct a baseline visit with each patient to include hypertension staging, risk stratification, determination of a goal BP, and treatment recommendations to the patient’s physician. All study visits with the research nurse and the pharmacist were conducted in one of the two family medicine physician offices. At all study visits, patients met with the research nurse prior to seeing the pharmacist. The research nurses measured each patient’s BP at least three times using a mercury sphygmomanometer using standardized techniques from BP clinical trials [38, 39]. Research nurses were certified every 3 months on their ability to accurately position the patient and measure the BP. The second and third BP values were averaged as per previous clinical trials [38] and used as the BP for the visit. The goal BP was <130/80 mmHg for patients with diabetes mellitus and <140/90 for all other patients, consistent with current US guidelines [3]. After the 1 h baseline visit with the research nurse and pharmacist, follow-up visits lasting approximately 30 min were conducted with each intervention patient at 2, 4, 6, and 8 months. These time points were chosen as BP collection times to remain consistent with other short-term randomized clinical trials testing the efficacy of hypertension therapies. The patient was already coming to clinic to see the research nurse for BP measurement, so it was logical that the pharmacist see the patient at those time points. Clinical pharmacists could also schedule additional optional visits between scheduled visits at their discretion. At each visit, the clinical pharmacist conducted a thorough interview of the patient, identified problems leading to poor BP control, provided patient education, developed a new treatment plan, and presented recommendations to the physician regarding changes in drug therapy and appropriate medication monitoring. Recommendations were most commonly made face-to-face with the physician in the family medicine clinic immediately after the study visit, although they could also be made via telephone or written communication. All study visits and recommendations were documented in patient medical records. Patients saw their physician at baseline and 9 month visits and as needed during the study period. Physicians could make changes in drug therapy independent of the pharmacist, although this was virtually never done because BP care was usually delegated to the pharmacist and decisions about therapy changes were decided upon collaboratively.
To describe clinical pharmacist recommendations, we divided the recommendations into those that involved drug therapy recommendations, non-drug recommendations or no specific recommendation at a given patient encounter. We looked at specific drug therapy recommendations made at each visit and then grouped each recommendation into one of eight categories: added thiazide diuretic, added other drug, drug dose increased or decreased, changed dose frequency, switch within same class, drug discontinued, and regimen not changed.
The frequency of occurrence of each recommendation type was calculated at each time period, and these values were summed to yield an overall frequency of occurrence. The rate at which physicians accepted pharmacist recommendations to change drug therapy was also calculated. Paired t-tests were used for BP comparisons at baseline and the end of 9 months, using intention-to-treat analyses. For all descriptive statistics, means, standard deviations, and ranges were calculated.
Recommendations that did not include drug therapy were usually made to the patient. We tabulated these non-drug recommendations separately since they did not involve a recommendation to the physician. The study was approved by the Institutional Review Board of the University of Iowa.
Results
Patient recruitment began in January 2004 and the last patient completed the study in October 2006. A total of 101 patients with uncontrolled BP participated in this evaluation and all patients signed informed consent. Nine patients withdrew from the study. Of these, one attended the baseline visit only, four attended two visits, two attended three visits, and two attended four visits. Patient demographic information is provided in Table 2. Patients averaged 6.8 ± 1.6 total visits (including the final study visit at which they did not see the pharmacist and only had BP measurement by the research nurse).
Clinical pharmacists made a total of 628 recommendations. Pharmacists made 267 recommendations to change drug therapy (Table 3). The majority of these recommendations for a change in treatment involved adding a new antihypertensive drug (46.4%) or increasing a dose (33.3%). The largest numbers of pharmacist recommendations (41.6%) were made at the baseline visit, and 76.8% of all recommendations were made by the 2-month visit. The average number (±SD) of recommendations for a change in drug therapy was 2.64 ± 1.45 per patient with a range of 1–6. A summary of antihypertensive medications at baseline and end of study, in addition to the percent of patients requiring 1, 2, 3, etc. drug therapy recommendations are given in Table 4.
Pharmacists made 45 recommendations to add a thiazide diuretic. These recommendations occurred early in the study, with 40 (88.9%) of the 45 recommendations occurring at the baseline visit. In fact, no recommendations to add a thiazide diuretic were made after the 2-month visit. Recommendations to add other antihypertensive medications or to increase a drug dose also occurred most frequently at the baseline visit and then declined throughout the study. Of the 267 pharmacist recommendations to modify drug therapy, 256 were implemented, yielding a 95.9% physician acceptance rate.
Of the 628 total drug therapy recommendations made by pharmacists, 361 recommendations were to make no changes in the treatment plan. These cases in which no recommendation was made typically occurred later in the course of the study and were because the patient had already achieved BP control with previous recommendations by the pharmacist. Recommendations made earlier in the study for no change in drug therapy were usually due to poor medication adherence or that a previous medication change may not yet have achieved a full therapeutic effect. The average number (±SD) of recommendations for no change in drug therapy is 3.57 ± 1.40 per patient with a range of 0–7. Physicians agreed with 359/361 (99.4%) of pharmacist recommendations when they suggested that no changes be made.
Clinical pharmacists made numerous recommendations for non-pharmacologic therapies generally directly to the patient. A total of 441 documented recommendations were to modify lifestyle, roughly 4.4 recommendations per patient. An additional 17 recommendations encouraged medication adherence. The lifestyle modification recommendations included increasing activity (44.9%), reducing weight (27.0%), initiating the DASH diet (14.3%), discussing diet without specific mention of DASH (7.9%), restricting sodium (5.4%), and decreasing alcohol consumption (0.5%). We did not determine how many of these recommendations were successfully implemented by the patients.
Average BP (average ± SD) at baseline as measured by the research nurse was 153.1 ± 10.0/84.9 ± 12.0 mmHg and was significantly reduced to 124.2 ± 9.7/74.7 ± 9.6 mmHg (P < 0.001) after 9 months of the clinical pharmacy intervention. By definition, none of the patients had controlled BP at baseline. At the end of 9 months, 89.1% (P < 0.001) of patients had achieved their BP goal (Table 3).
Discussion
The vast majority of the pharmacists’ recommendations occurred within the first 2 months of the study. This finding suggests that the pharmacists were making recommendations early in order to quickly achieve BP control. Early control of BP is important because studies have found that controlling BP within the first 6 months can significantly reduce cardiovascular events [40]. The frequent recommendations by the pharmacist led to a marked improvement in BP control (89%) and mean BP. We have previously reported that 53% of the control group from this study achieved BP control [37].
Our results differ substantially from those reported by Chrischilles et al. in their evaluation of the Iowa Medicaid Pharmaceutical Case Management (PCM) program. Although Chrischilles et al. also found that the most common type of recommendations were starting a medication (24.5%) and changing dose (16.2%), these types of recommendations constituted a substantially lower percentage of total recommendations than was found in the current study [35]. This difference in outcomes might have resulted because the PCM program was conducted by community pharmacists making recommendations concerning numerous disease states via facsimile to private physicians. Chrischilles et al. also found that physicians accepted only 49% of community pharmacists’ recommendations, similar to the acceptance rate found by Park et al. (53%), which was a hypertension intervention in community pharmacy [28]. These acceptance rates are markedly lower than the 95.9% found in the current study. The lower physician acceptance rates found in these two previous studies might be due to differences in the study settings. Chrischilles et al. studied community pharmacies, while Park et al. studied recommendations made by pharmacists working in chain community pharmacies. In contrast, our study involved clinical pharmacists who practice in the same office as the physician.
The most common recommendations for a change in drug therapy made by pharmacists in these studies involved adding medications or increasing doses because hypertension or other conditions were not being controlled adequately. In the Zillich et al. HOME study, which only looked at pharmacist recommendations for a change in drug therapy for patients with hypertension, nearly 60% of the pharmacist recommendations involved adding an antihypertensive medication or increasing the dose of an existing medication [31].
The 95.9% acceptance rate for clinical pharmacists’ recommendations found in the current study is almost identical to the acceptance rates found by Brown et al. (96%) and by Haxby et al. (98%) [34, 36]. These two studies involved recommendations for numerous disease states. All of these studies were conducted in family medicine offices where the clinical pharmacist worked directly with the physician as a colleague. The discrepancies in acceptance rates between settings might lead one to hypothesize that acceptance rates could be dependent on the relationship between the physician and pharmacist. In areas where they work together, acceptance rates are high. However, acceptance rates are lower for recommendations made by pharmacists in community pharmacies, perhaps because communication is more difficult and the physicians and pharmacists do not know each other as well.
The 89.1% BP control rate found in this study is appreciably greater than those reported in other studies using pharmacists in a similar capacity. Carter et al. achieved a control rate of 68% using community pharmacists that practiced in the same building as the prescribing physician [32]. Park et al. achieved a control rate of 52.2% when using community pharmacists in the chain community pharmacy setting [28]. It is possible that BP control rates, like physician acceptance rates, are linked to the relationship between the pharmacist and the physician. That is, BP control rates are highest when physicians and pharmacists work together in the same office. In contrast, control rates are lowest when recommendations are made by pharmacists working in the chain setting where they have no working relationship with the physician.
This report has some limitations. First, the study was designed as an efficacy study to maintain high internal validity and simulate clinical trials in hypertension. The results only apply to the use of this physician–pharmacist collaborative model where pharmacists practice directly in the physician’s office. The investigators are performing an ongoing effectiveness study of physician–pharmacist collaborative management of hypertension in community-based family medicine clinics. Second, the intervention was short, lasting only 9 months. Future research should be of a longer duration to determine if the effect of physician–pharmacist co-management of hypertension is sustainable. Finally, the sample population is small and largely Caucasian, which may lead to difficulty in generalizability of the results. However, the study did include patients of all socioeconomic strata. Future research should be done with larger patient populations with a greater diversity of geographic locations and including a greater number of patients from racial and ethnic minority groups.
Conclusion
Pharmacist–physician co-management of BP is effective at reducing BP and improving BP control rates. The frequent recommendation to start thiazide diuretics in this study is interesting as it is consistent with US guidelines for BP therapy. Additionally, most recommendations to modify drug therapy were made early in each patient’s enrollment period, suggesting that pharmacists understood the importance of aggressive management of hypertension to quickly achieve BP control. Physician acceptance of pharmacist recommendations and BP control rates were high, probably because both providers worked in the same setting. This study suggests one effective method of improving BP control is for pharmacists to recognize inadequate drug therapy, decide upon an appropriate course of action, and make a specific recommendation to the patient’s physician to change therapy. Active and direct interventions by pharmacists, therefore, hold potential for widespread improvements in BP control.
References
2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens 2003;21(6):1011–53.
World Health Report 2002. Reducing risks, promoting healthy life. Geneva, Switzerland: World Health Organization; 2002. http://www.who.int/whr/2002/.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 2003;42(6):1206–52.
Petrella RJ, Campbell NR. Awareness and misconception of hypertension in Canada: results of a national survey. Can J Cardiol 2005;21(7):589–93.
CHD 2006. Blood pressure. Chapter 9, BHF Coronary heart disease statistics. Published May 2006. http://www.heartstats.org/temp/Chaptersp9.pdf.
Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension 2007;49(1):69–75.
Coca A, Aranda P, Bertomeu V, Bonet A, Esmatjes E, Guillen F, et al. Strategies for effective control of arterial hypertension in Spain. Consensus document. Rev Clin Esp 2006;206(10):510–4.
Black HR, Elliott WJ, Neaton JD, Grandits G, Grambsch P, Grimm RH Jr, et al. Baseline characteristics and early blood pressure control in the CONVINCE trial. Hypertension 2001;37(1):12–8.
Bond CA, Monson R. Sustained improvement in drug documentation, compliance, and disease control. A four-year analysis of an ambulatory care model. Arch Intern Med 1984;144(6):1159–62.
Hansson L, Zanchetti A, Carruthers SG, Dahlof B, Elmfeldt D, Julius S, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet 1998;351(9118):1755–62.
Grimm RH Jr, Margolis KL, Papademetriou VV, Cushman WC, Ford CE, Bettencourt J, et al. Baseline characteristics of participants in the antihypertensive and lipid lowering treatment to prevent heart attack trial (ALLHAT). Hypertension 2001;37(1):19–27.
Carter BL, Zillich AJ, Elliott WJ. How pharmacists can assist physicians with controlling blood pressure. J Clin Hypertens 2003;5(1):31–7.
Miller NH, Hill M, Kottke T, Ockene IS. The multilevel compliance challenge: recommendations for a call to action. A statement for healthcare professionals. Circulation 1997;95(4):1085–90.
Hyman DJ, Pavlik VN. Characteristics of patients with uncontrolled hypertension in the United States. N Engl J Med 2001;345(7):479–86.
Berlowitz DR, Ash AS, Hickey EC, Friedman RH, Glickman M, Kader B, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med 1998;339(27):1957–63.
Oliveria SA, Lapuerta P, McCarthy BD, L’Italien GJ, Berlowitz DR, Asch SM. Physician-related barriers to the effective management of uncontrolled hypertension. Arch Intern Med 2002;162(4):413–20.
Monson R, Bond CA, Schuna A. Role of the clinical pharmacist in improving drug therapy. Clinical pharmacists in outpatient therapy. Arch Intern Med 1981;141(11):1441–4.
Bogden PE, Abbott RD, Williamson P, Onopa JK, Koontz LM. Comparing standard care with a physician and pharmacist team approach for uncontrolled hypertension. J Gen Intern Med 1998;13(11):740–5.
Borenstein JE, Graber G, Saltiel E, Wallace J, Ryu S, Archi J, et al. Physician–pharmacist comanagement of hypertension: a randomized, comparative trial. Pharmacotherapy 2003;23(2):209–16.
Erickson SR, Slaughter R, Halapy H. Pharmacists’ ability to influence outcomes of hypertension therapy. Pharmacotherapy 1997;17(1):140–7.
Forstrom MJ, Ried LD, Stergachis AS, Corliss DA. Effect of a clinical pharmacist program on the cost of hypertension treatment in an HMO family practice clinic. DICP 1990;24(3):304–9.
Hawkins DW, Fiedler FP, Douglas HL, Eschbach RC. Evaluation of a clinical pharmacist in caring for hypertensive and diabetic patients. Am J Hosp Pharm 1979;36(10):1321–5.
Lee JK, Grace KA, Taylor AJ. Effect of a pharmacy care program on medication adherence and persistence, blood pressure, and low-density lipoprotein cholesterol: a randomized controlled trial. JAMA 2006.
McGhan WF, Stimmel GL, Hall TG, Gilman TM. A comparison of pharmacists and physicians on the quality of prescribing for ambulatory hypertensive patients. Med Care 1983;21(4):435–44.
McKenney JM. Pharmacy management of hypertensive patients. J Am Pharm Assoc 1974;14(4):190–5.
McKenney JM, Slining JM, Henderson HR, Devins D, Barr M. The effect of clinical pharmacy services on patients with essential hypertension. Circulation 1973;48(5):1104–11.
Mehos BM, Saseen JJ, MacLaughlin EJ. Effect of pharmacist intervention and initiation of home blood pressure monitoring in patients with uncontrolled hypertension. Pharmacotherapy 2000;20(11):1384–9.
Park JJ, Kelly P, Carter BL, Burgess PP. Comprehensive pharmaceutical care in the chain (pharmacy) setting. J Am Pharm Assoc 1996;NS36(7):443–51.
Vivian EM. Improving blood pressure control in a pharmacist-managed hypertension clinic. Pharmacotherapy 2002;22(12):1533–40.
Walsh JM, McDonald KM, Shojania KG, Sundaram V, Nayak S, Lewis R, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care 2006;44(7):646–57.
Zillich AJ, Sutherland JM, Kumbera PA, Carter BL. Hypertension outcomes through blood pressure monitoring and evaluation by pharmacists (HOME study). J Gen Intern Med 2005;20(12):1091–6.
Carter BL, Barnette DJ, Chrischilles E, Mazzotti GJ, Asali ZJ. Evaluation of hypertensive patients after care provided by community pharmacists in a rural setting. Pharmacotherapy 1997;17(6):1274–85.
Carter BL, Helling DK. Ambulatory care pharmacy services: has the agenda changed? Ann Pharmacother 2000;34(6):772–87.
Brown DJ, Helling DK, Jones ME. Evaluation of clinical pharmacist consultations in a family practice office. Am J Hosp Pharm 1979;36(7):912–5.
Chrischilles EA, Carter BL, Lund BC, Rubenstein LM, Chen-Hardee SS, Voelker MD, et al. Evaluation of the Iowa Medicaid pharmaceutical case management program. J Am Pharm Assoc (Wash DC) 2004;44(3):337–49.
Haxby DG, Weart CW, Goodman BW Jr. Family practice physicians’ perceptions of the usefulness of drug therapy recommendations from clinical pharmacists. Am J Hosp Pharm 1988;45(4):824–7.
Carter BL, Bergus GR, Dawson JD, Farris KB, Doucette WR, Chrischilles EA, et al. A cluster-randomized trial to evaluate physician/pharmacist collaboration to improve blood pressure control. J Clin Hypertens (Submitted June 2007).
Wright JT Jr, Bakris G, Greene T, Agodoa LY, Appel LJ, Charleston J, et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: results from the AASK trial. JAMA 2002;288(19):2421–31.
Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension 2005;2005(45):142–61.
Julius S, Kjeldsen SE, Weber M, Brunner HR, Ekman S, Hansson L, et al. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet 2004;363(9426):2022–31.
Acknowledgements
The authors would like to acknowledge the assistance of Janyce Stewart, RN and Gail Ardery, PhD (project managers); George Bergus, MD, Jeffrey Dawson, ScD, Karen Farris, PhD, William Doucette, PhD, Elizabeth Chrischilles, PhD, and Arthur Hartz, MD, PhD, (study steering committee); Karen Kluesner, RN and Sheryl Eastin, RN (research nurses); Paul James, MD, Christopher Goerdt, MD, and David Katz, MD (data and safety monitoring board).
Funding
This project was supported by the National Heart, Lung, and Blood Institute, 1 R01 HL069801-01A1. Dr. Carter is also supported by the CRIISP Center, Iowa City Department of Veterans Affairs.
Conflicts of Interest
Dr. Carter is also supported by the Center for Research in Implementation in Innovative Strategies in Practice (CRIISP), Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service (HFP 04-149). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs. Dr. Carter receives funding from NHLBI for another study and he is a paid investigator/educator for the dissemination program: “A Joint Project of the National High Blood Pressure Education Program and the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) Collaborative Research Group.” The other authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Von Muenster, S.J., Carter, B.L., Weber, C.A. et al. Description of pharmacist interventions during physician–pharmacist co-management of hypertension. Pharm World Sci 30, 128–135 (2008). https://doi.org/10.1007/s11096-007-9155-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-007-9155-6