Abstract
Purpose
Oxidative stress is a hallmark of Alzheimer’s Disease (AD) and promotes tau phosphorylation. Since Thioredoxin Interacting protein (TXNIP), the inhibitor of the anti-oxidant system of Thioredoxin, is up regulated in the hippocampus of AD patients, we investigated whether TXNIP plays a role in promoting tau phosphorylation and whether Verapamil, an inhibitor of TXNIP expression, prevents TXNIP downstream effects.
Methods
We analyzed TXNIP expression and tau phosphorylation in the hippocampus of the 5xFAD mice in the absence and presence of a pharmacological treatment with Verapamil. Using SH-SY5Y cells, we verified the causative role of TXNIP in promoting tau phosphorylation at Ser202/Thr205, by inducing TXNIP silencing.
Results
The amyloid beta peptide (Aβ1–42) leads to TXNIP over-expression in SH-SY5Y cells, which in turns induces oxidative stress and the activation of p38 MAPK, promoting tau phosphorylation at Ser202/Thr205. Silencing of TXNIP abolishes Aβ1–42-induced tau phosphorylation, p38 MAPK phosphorylation and subsequent tau phosphorylation. Verapamil prevents TXNIP expression as well as p38 MAPK and tau phosphorylation at Ser202/Thr205 in the hippocampus of the 5xFAD mice.
Conclusions
Our study unveil a novel pathway involved in AD progression that is inhibited by Verapamil, shedding new light on the understanding of the therapeutic potential of Verapamil in AD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is a age-related neurodegenerative disorder, which leads to dementia (1 #96). AD is characterized by the accumulation of the amyloid beta (Aβ) peptides, producing the amyloid plaques, and the formation of aggregates of the microtubule-associated protein tau, producing the neurofibrillary tangles (NTFs) (1 #96). NTFs are manly constituted by hyper phosphorylated tau. Tau is implicated in the microtubule assembly, which is essential for maintaining the function of neuronal cells (2 #908). Aβ promotes tau phosphorylation, leading to impaired synaptic function as well as altered cytoskeletal assembly (3 #687). The understanding of the molecular mechanisms involved in aberrant tau phosphorylation is of high relevance in order to set up therapeutic strategies.
Oxidative stress is a hallmark of AD and participates in the pathophysiology of AD by promoting the oxidative damage of proteins as well by activating specific signaling pathways that alters the neuronal activity, both mechanisms affects tau function (4 #909). Indeed, the oxidative damage alters tau capability to promote the microtubule assembly (5 #903). On the other hands, oxidative stress-induced signaling pathways promote aberrant tau phosphorylation (6 #906; 7 #899). Interestingly, the anti-oxidant system of Thioredoxin (Trx) plays a key function in preventing tau oxidative damage and preserving is capability in promoting the microtubule assembly (5 #903; 6 #906). Thioredoxin Interacting protein (TXNIP) is the inhibitor of Trx and its expression leads to oxidative stress (8 #35; 9 #160). A previous study reports that oxidative stress promoted tau phosphorylation by inducing that activation of p38 MAPK (6 #906). In addition, it has been shown that p38 MAPK signaling pathway is responsible for tau phosphorylation at Ser202/thr205 site (10 #907). Several studies including our own clearly demonstrate that TXNIP plays a key role in oxidative-stress induced p38 MAPK activation (11 #914; 12 #644; 13 #913; 14 #89; 15 #122). Although it has been shown that TXNIP is one of the mRNA most over-expressed in the hippocampus of AD patients and 3Tg transgenic mice (16 #363), there is no any study investigating the role of TXNIP in altering tau phosphorylation. At the light of the key role of TXNIP in the activation of p38 MAPK (11 #914; 12 #644; 13 #913; 14 #89; 15 #122), which is responsible of Ser202/Thr205 tau phosphorylation (10 #907), we investigated whether TXNIP mediates p38 MAPK-induced Ser202/Thr205 tau phosphorylation.
Verapamil has been shown to have beneficial effects in animal models of cardiovascular diseases and diabetes by suppressing TXNIP expression (17 #185; 18 #304). Verapamil has been also proposed as a therapeutic agent for AD (19 #192). We investigated whether oral treatment of Verapamil reduces TXNIP expression into the brain of the 5xFAD mice and inhibits Ser202/Thr205 tau phosphorylation.
Herein, we show that in differentiated SH-SY5Y neuronal cells, TXNIP mediates Aβ-induced alterations of tau capability to assemble the microtubules. Silencing of TXNIP restores tau interaction with the microtubules. In addition, we report that TXNIP plays a pivotal role in p38 MAPK-induced Ser202/Thr205 tau phosphorylation, which is abolished by TXNIP silencing.
Previously we demonstrated that TXNIP is early over-expressed in the hippocampus of the 5xFAD transgenic mice (20 #283). We show that TXNIP over expression parallels tau hyper phosphorylation and p38 MAPK phosphorylation in the hippocampus of the 5xFAD mice. Our data show that inhibition of TXNIP expression by Verapamil prevents p38 MAPK phosphorylation, and ameliorates Ser202/Thr205 tau phosphorylation in the 5xFAD mice.
Materials and methods
Animals
Animal treatment and maintenance were performed in accordance with the Ethics Committee of the public institutions involved in this project and with the guidelines published by European Communities Council Directive of November 24, 1986 (86/609/EEC). All efforts were made to minimize animal suffering and to reduce the number of mice used. The generation of 5XFAD mice has been described previously (21 #179). These transgenic mice overexpress both mutant human APP (695) with the Swedish (K670 N, M671 L), Florida (I716V), and London (V717I) familial Alzheimer’s Disease (FAD) mutations and human PS1 harboring two FAD mutations, M146 L and L286 V. Expression of both transgenes is regulated by neural-specific elements of the mouse Thy1 promoter to drive overexpression in neurons.
The 5XFAD strain (B6/SJL genetic background) was maintained by crossing hemizygote transgenic mice with B6/SJL F1 breeders (Jackson Laboratories, Bar Harbor, Maine, USA). 5XFAD heterozygote transgenic mice were used for the experiments with non-transgenic wild-type (WT) littermate mice as controls. Before experimentation, genomic DNA was extracted from the tail tips of all mice to assess their genotype by PCR. All transgenic and WT mice were bred in our animal facility, had access to food and water ad libitum, and were housed under a 12 h light-dark cycle at 22–24°C.
Treatment with Verapamil: Verapamil (1 mg/kg/day) was added in the drinking water of 5xFAD mice of 2 months age (first formation of intracellular amyloid A deposition) for 3 months (18 #304). Previous studies demonstrated that a long-term treatment of Verapamil in the drinking water at this concentration has no any toxic effect on the mice (17 #185; 18 #304; 22 #915). Indeed, we did not observe any alteration of the weight and the activity in Verapamil treated 5xFAD mice (data not shown). Control wild type mice, untreated 5xFAD and Verapamil treated 5xFAD mice were sacrificed (animals will received anesthesia, then sacrificed by cervical dislocation).
Immunohistochemistry for Aβ plaques using BSB
Mice were deeply anesthetized (sodium pentobarbital, ip) and transcardially perfused (4% paraformaldehyde). Brains were extracted and postfixed overnight in cold paraformaldehyde. Coronal brain sections (30 m thick) were serially generated using a vibratome (Thermo Scientific HM650V, Illkirch, France) and stored at −20°C in 6-wellplates containing 30% glycerol, 30% ethylene glycol in 0.05 M PBS until processed. After washing in PBS, floating sections were incubated 1 h at room temperature with blocking buffer (3% BSA, 0.1% Triton X-100 in PBS) and overnight at 4°C with a rabbit polyclonal anti-GFAP (1:400, Dako, Trappes, France). Slices were rinsed 5 min in PBS and incubated for 90 min at rt. with cross-adsorbed Alexafluor 594-conjugated anti-rabbit secondary antibodies (1:500, Jackson Immunoresearch, West Grove, PA, USA). The detection of amyloid aggregates-plaque were performed by the Congo red derivative (trans,trans)-1-bromo-2,5-bis(3-hydroxycarbonyl-4-hydroxy) styrylbenzene (BSB). (23 #189) After 3 washes in PBS, slides were counter-stained with 0.5 ng/ml Hoechst blue (#33342, Sigma-Aldrich) for 30 min at rt. and mounted with ProLong Gold Antifade reagent. Confocal image acquisition was performed as previously described (23 #189). Quantification of BSB staining was performed on 30 μm thick brain coronal sections stained with BSB at the frontal level using the ImageJ software. The pictures were binarized to 16-bit black and white images and a fixed intensity threshold was applied defining the BSB staining. Percentage of covered area by the fluorescent staining was calculated. Five animals were used in this analysis with two frontal sections per mice. Statistical T test was used to compare age-dependent changes.
Analysis of human brain samples
We examined 4 brains autopsy. The study was approved by the Ethics Committee and Review boards of the University of Turin, Italy, according to the Declaration of Helsinki issued by the World Medical Association (24 #683). Written informed consensus for all subjects was obtained from their families. Two patients were neuropathologically diagnosed as “high likelihood” AD, according to the general consensus for the postmortem AD diagnosis: NIA-Reagan Institute criteria (25 #659) (F:M, 1:1; age at death 61 years and 81 years respectively).The autopsy-proven control group consisted of 2 individuals with no history of dementia, died with or without a history of neurological disease (encephalitis; myocardial infarction, respectively) and in whom the brain either was considered normal or showed abnormalities other than neurodegenerative lesions upon histological examination. The presence of a few neurofibrillary tangles in the hippocampus and parahippocampal gyrus and of neuritic senile plaques (<5/mm2 in these regions and the neocortex) was considered within normal limits (F:M, 1:1; age at death 79 years and 89 years respectively). For the immunohistochemistry (IHC), 10-μm-thick sections cut from formalin-fixed blocks of the cerebral hemispheres (hippocampus) were deparaffinized with 2 washes in xylene for 5 min. Sections were rehydrated with 2 washes in 100% ethanol for 3 min, followed by washes in 95% and 80% ethanol for 1 min. Then the slides were rinsed in distilled water. We performed the antigen retrieval in citrate buffer (pH 6) at 95°C for 20 min. Then the sections were rinsed twice in Phosphate buffered saline (PBS) for 5 min. Unspecific binding was blocked in blocking buffer (3% BSA, 0.1% Triton X-100 in PBS) for 1 h at room temperature. Slides were then incubated over night at 4°C with a mouse monoclonal anti-TXNIP antibody (1:100, MBL, clone JY2) and an anti human tau (1:100, DAKO) in blocking buffer. Then, slices were rinsed (3–5 min) in PBS and incubated for 90 min a room temperature (rt) with cross-adsorbed Alexafluor 488- or 594-conjugated anti-rabbit or anti-mouse secondary antibodies (1:500, Jackson Immunoresearch, West Grove, PA, USA) in dark conditions. After several washes in PBS, slides were counter-stained with 0.5 ng/ml Hoechst blue (#33342, Sigma-Aldrich) for 30 min at room temperature and mounted with ProLong Gold Antifade reagent (Life Technologies, Saint Aubin, France). Confocal image acquisition was performed on a Zeiss 510 laser-scanning microscope with 63× oil immersion objectives.
Aβ preparation
Aβ1–42 was prepared as previously described (23 #189): Aβ peptides were dissolved in 1,1,1,3,3,3-Hexafluoro-2-propanol (HFIP) in order to obtain 100 μM concentration. Aβ dissolved in HFIP was dried and dissolved in 100 μl NaOH 50 mM, then 0.9 ml of PBS was added. The solutions of Aβ1–42 was maintained 2 h on ice. Following a centrifugation for 30 s, the peptides were subjected to a chromatographic separation using Fluorescent Dye Removal Columns (Thermo Scientific) according to the protocol provided by the manufacturer. Then, Aβ1–42 solution was filtered using a 0.2 μm filter and added to the cells.
The incubation of the peptides for 2 h on ice results in the isolation of Aβ1–42 dimers and trimers (23 #189) (supplementary figure 1). The formation of Aβ1–42 dimers and trimers was verified by western blotting, after separation on a 15% SDS PAGE. The Aβ1–42 dimers and trimers were detected using the mouse monoclonal Bam-10 antibody against Aβ (Sigma).
In vitro culture of SH-SY5Y neuroblastoma cell line
SH-SY5Y cells were grown in Dulbecco’s modified eagle medium (DMEM)/F12 (1:1 ratio) supplemented with 10% (vol/vol) FBS. For the Aβ treatment (3 μM), cells were differentiated for 5 days in DMEM/F12 supplemented with 2% FCS, 1 μM retinoic acid (RA) and 50 ng/mL BDNF, as previously described (26 #916). Cells were treated with Aβ (3 μM) in the differentiation medium for 24 h. TXNIP expression was inhibited by transfecting the cells with a plasmid encoding an shRNA targeting TXNIP RNA (Super Array Bioscience Corporation, Frederik, MD, USA), or a contro shRNA scramble (Super Array Bioscience Corporation, Frederik, MD, USA), as previously described (14 #89; 15 #122). We obtained clones of SH-SY5Y cells stably expressing either the shRNA targeting TXNIP or the scramble shRNA as previously described (14 #89). Cells were treated with Aβ dimers and trimers for 24 h. We inhibited TXNIP expression by adding Verapamil (a voltage gated Ca2+ channel inhibitor) 1 μM (17 #185; 18 #304) 24 h before and during Aβ addition. The p38 MAPK inhibitor SB203580 (10 μM, Sigma-Aldrich) was added 30 min before and during Aβ1–42 treatment (14 #89). N-acetylcysteine (NAC, 5 mM, Sigma) was added 30 min before and during Aβ1–42 treatment (27 #377).
Western blot
After NaCl transcardial perfusion, the hippocampi were microdissected and snap-frozen for biochemical assays. For western blots (WB), each sample was homogenized in 25% w/v of 50 mM Tris-HCl pH 7.5 buffer containing 150 mM NaCl, 2 mM EDTA, 1% Triton X-100, 1% SDS and proteinase inhibitor cocktail (Millipore, Molsheim, France) and centrifuged at 10,000×g for 20 min. Protein concentrations were determined using the Lowry method (Bio-Rad, Hercules CA, USA).
Proteins extracts from SH-SY5Y cells were obtained using RIPA buffer as previously described (23 #189; 28 #67). After boiling, aliquots containing equal amounts of protein (30 μg) were loaded in Laemmli buffer and separated by 8% sodium dodecyl sulphate (SDS) polyacrylamide (Bio-Rad) gel electrophoresis (PAGE) using a MiniBlot system (Bio-Rad). Western blotting was performed as previously described (14 #89; 15 #122; 29 #86). Proteins were transferred onto nitrocellulose membranes (Amersham Biosciences, Buckinghamshire, UK) in transfer buffer (25 mM Tris, 192 mM glycine, 20% ethanol). Membranes were incubated overnight in blocking buffer at RT and then probed with a primary antibody, diluted in blocking buffer: (i) anti-TXNIP (MBL, clone JY2) 1:1000 dilution in PBS 1% fat free milk; (ii) anti-total tau (Tau 1, Sigma Aldrich), anti-tau phosphorylated at Ser202/Thr 205 (AT8 Thermo Scientific), anti-p38 MAPK and anti-phosphorylated p38 MAPK (Cell Signaling), and anti-tubulin (DM1A, Sigma) 1:1000 dilution in PBS 5% fat free milk; (iii) anti-actin (Sigma) 1:3000 dilution in PBS 5% fat free milk. After incubation with primary antibodies, membranes were incubated with a horseradish-peroxidase conjugated secondary antibody (Jackson Immunoresearch, West Grove PA, USA). Finally, proteins were detected using a chemiluminescence kit (Roche Diagnostics). When necessary, autoradigraphic films were digitized using GeneTools software (Syngen) and ODs of the bands were assessed using scion image software (Scion Corporation MA, USA). The T-test was used to calculate the significance of protein expression variations.
Determination of intracellular ROS levels
Cells were plated on 96-wells plates and intracellular ROS level was determined as previously described (23 #189; 30,31 #120; 32 #85). The day before experiments, SH-SY5Y cells were cultured in medium containing 2% FCS (Gibco) and maintained in low serum condition for 16 h. The day of the experiments, cells were washed with PBS and incubated in 5% CO2/95% air at 37°C for 6 h in DMEM without FCS. Cells were washed twice with DMEM. Aβ1–42 peptide (10 μΜ) was preincubated 5 min at room temperature in DMEM containing copper (10 μM) and ascorbate (300 mM), in a final volume of 50 μL, as previously described (30,31 #120). The cells were treated with Aβ1–42 for 60 min at 37°C as previously described (23 #189). Intracellular ROS levels were monitored by using the fluorescent dye 2′,7′-dichlorodihydrofluorescein diacetate (H2DCFDA; Molecular-Probes, Invitrogen) as previously described (32 #85). After treatment, cells were washed twice and incubated in DMEM containing H2DCFDA (20 μM). After 30 min incubation at 37°C, cells were washed with PBS and fluorescence intensity was measured in a Fluoro plate reader (FLX800 Biotek Instruments, software KL4) with the excitation and emission wavelengths at (485 ± 20 nm 525 ± 20 nm) respectively. The cell-permeant H2DCFDA is converted into a no fluorescent polar derivative (H2DCF) by cellular esterases after incorporation into cells. H2DCF is oxidized rapidly to the highly fluorescent 2′,7′-dichlorofluorescein (DCF) in the presence of intracellular ROS. The results obtained are the average of three independent experiments each of them performed with 4 replicates for each point analyzed (n = 12 and three independent experiments).
Assay of microtubule-binding activity of tau
Microtubule-binding activity of tau was measured by the method described previously (33 #898). Briefly, cells were harvested in a high- salt reassembly buffer (100 mM Tris, 0.5 mM MgSO4, 1 mM EGTA, 2 mM dithiothreitol, and 750 mM NaCl, pH 6.8) supplemented with 0.1% Triton X-100, 20 lM taxol, 2 mM GTP, and a mixture of prote- ase inhibitors (2 mM phenylmethylsulfonyl fluoride, L-1-chloro-3-(4- tosylamido)-4-phenyl-2-butanon, L − 1-chloro-3-(4-tosylamido)-7-ami- no-2-heptanone-hydrochloride, leupeptin, pepstatin A, and soy bean trypsin inhibitor; 1 lg/ml each) at 37°C. Cell lysates were homogenized with 15 strokes in a warm Dounce homogenizer and then centrifuged at 50000 · g for 20 min (25°C). We removed the supernatant (S) containing unbound tau and we dissolved the remaining pellet (P) in sample buffer. We measurement the protein concentration and analyzed the samples by Western blot analysis. The ratio of tau and Ser202/Thr205 phosphorylated tau bound to microtubules (P) versus unbound (S) was analyzed by comparing the immunoreactivity of tau in these two fractions.
ELISA analysis of phosphorylated p38 MAPK
We analyzed the amount of phosphorylated p38 MAPK using the p38 MAPK (Total/Phospho) Multispecies InstantOne™ ELISA Kit (ThermoFisher) according tot he manufacturer instructions. The T-test was used to calculate the significance of protein expression variations.
Cell viability assay (MTT)
Cell viability was measured by using the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) dye reduction assay. Basically, MTT (25 μl of 5 mg/ml−1 solution in PBS) was added to each cell sample Subsequently, DMSO (1 ml) was added and the reduced MTT was measured by absorption at 570 nm, as previously described (23 #189; 30,31 #120). Results are the average of three independent experiments following normalization (n = 3). The T-test was used to calculate the significance of cell viability variations.
Results
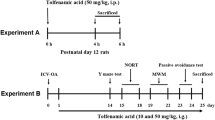
Verapamil blocks TXNIP over expression and Tau phosphorylation in the hippocampus of the 5xFAD mice
TXNIP is one of the mRNA more over expressed in the hippocampus of AD patients as well as in the hippocampus of the 3Tg AD mice (16 #363). We demonstrated that TXNIP is early over expressed in the hippocampus of 4 months old 5xFAD mice (20 #283). Several studies including our own demonstrated that TXNIP induces oxidative stress (8 #35; 9 #160; 14 #89). Recent reports underline the role of oxidative stress in promoting the phosphorylation of tau at ser202/Thr205 (7 #899). We first analyzed whether TXNIP over expression correlates with enhanced ser202/Thr205 tau phosphorylation in the hippocampus of 5 months old 5xFAD mice. We observed that enhanced TXNIP expression paralleled to increased ser202/Thr205 tau phosphorylation compared to age matched littermates (Fig. 1a-c). Verapamil, a L-type voltage gated calcium channel blocker, inhibits TXNIP expression and is proposed as therapeutic agents for TXNIP-driven pathologies such as cardiovascular diseases, diabetes and retinal inflammation (17 #185; 18 #304; 34 #658).Verapamil is also proposed as pharmacological therapeutic strategy for AD (19 #192; 35 #905). We treated 2 months old 5xFAD mice with oral Verapamil (1 mg/kg/day) for 3 months. It has been shown that oral treatment with oral Verapamil at this concentration efficiently inhibited TXNIP expression n vivo mice models (17 #185; 18 #304). In addition, previous studies demonstrated that a long-term treatment of Verapamil in the drinking water at this concentration has no any toxic effect on the mice (17 #185;18 #304; 22 #915). Indeed, we did not observe any alteration of the weight and the activity in Verapamil treated 5xFAD mice (data not shown). We observed that Verapamil treatments resulted in a significant decrement of TXNIP expression in the hippocampus of 5xFAD mice (Fig. 1a,b), as well as a significant decrement of tau phosphorylation at Ser202/Thr205 (Fig. 1a,c).
Verapamil inhibits TXNIP expression and tau phosphorylation at Ser202/Thr205 in the hippocampus of the 5xFAD mice. (a). Western blot analysis of TXNIP, Ser202/Thr205 phosphorylated tau, total tau, and actin (normalization) of protein extracts derived from the hippocampus of: age matched control mice, 5 months old 5xFAD mice, and 5 months old 5xFAD mice treated 3 months with oral administration of Verapamil. This is a representative of 2 different experiments. (b) Quantification of TXNIP protein level in the hippocampus of control and 5xFAD mice treated as in A. Actin has been used for normalization (n = 8, * = p < 0,05 versus control wild type mice; # = p < 0,05 versus 5xFAD mice). (c) Quantification of Ser202/Thr205 phosphorylated tau protein level in the hippocampus of control and 5xFAD mice treated as in A. Total tau and actin have been used for normalization (n = 8, * = p < 0,05 versus control wild type mice; # = p < 0,05 versus 5xFAD mice).
Verapamil ameliorates Aβ plaques formation in the 5xFAD mice
The 5xFAD mice are an early onset mice model of AD, characterized by a robust production of amyloid beta peptides and the formation of amyloid plaques is detectable in 2 months old mice (21 #179; 36 #917).
In the 5xFAD mice the hippocampus-dependent impairment of learning and memory starts in 4 months old mice and increases in older mice (36 #917). Such hippocampus-dependent cognitive deficit occurs in correlation with an enhanced amyloid plaques formation (36 #917). For this reason, we investigated whether Verapamil ameliorates he amyloid plaques formation in the 5xFAD mice. Images were acquired by confical microscopy (see material and methods). The focal plane for the detection of the BSB staining is different compared to the focal plane for the detection of GFAP staining, demonstrating that BSB is detecting extracellular aggregates. We observed a significant reduction of amyloid plaques in 5 months old 5xFAD mice treated with Verapamil compared to the age-matched untreated 5xFAD mice (Fig. 2a-c).
Verapamil ameliorates the amyloid plaques formation in the 5xFAD mice. (a) Histological analysis of GAFP (red) and amyloid beta aggregates (green) in the hippocampus of 5 moths old untreated 5xFAD mice (left) and 5xFAD mice treated with Verapamil (right). Amyloid beta aggregates were detected using BSB (a derivative of Congo Red). Images were acquired by confocal microscopy as described in the Material and Methods section. The focal plane for the detection of the BSB staining is different compared to the focal plane for th detection of GFAP staining, demonstrating that BSB is detecting extracellular amyloid aggregates. This experiments is representative of 5 independent experiments (number of animal analyzed for each group = 5). (b) Quantification of BSB staining in in the hippocampus of 5 moths old untreated 5xFAD mice and 5xFAD mice treated with Verapamil (N = 5; p < 0,05, using the T-test).
Aβ1–42 induces TXNIP expression and oxidative stress in differentiated SH-SY5Y cells, which are inhibited by Verapamil
At the light of the data we obtained in vivo (Fig. 1a-c), we investigated whether TXNIP expression in neuronal cells plays a causative role in altering Ser202/Thr205 tau phosphorylation. First, we analyzed whether treatment with Aβ1–42 induces TXNIP expression of TXNIP in differentiated SH-SY5Y cells. We treated the cells with a mixture of Aβ1–42 dimers and trimers (supplementary Fig. 1), which are considered the Aβ species providing the highest neuronal dysfunction (37 #142). We employed 3 μM concentration of Aβ1–42 dimers and trimers, which is inferior compared the Aβ1–42 used in previous studies (38 #910; 39 #912), in order to reduce the Aβ1–42-dependent cell death. We observed a significant increment of TXNIP expression after 24 h of Aβ1–42 (3 μM) addition (Fig. 3a,b). Addition of Verapamil (1 μM) inhibited Aβ1–42-dependent TXNIP over expression, as well as silencing of TXNIP by a shRNA (Fig. 3a,b), while a scramble shRNA had no any effect on Aβ1–42’dependent TXNIP over expression (Fig. 3a,b). The reactive oxygen species inhibitor N-acetyl-cysteine (NAC) reduced Aβ1–42-induced TXNIP expression (Fig. 3a,b) as previously reported (27 #377).
Verapamil and NAC inhibit Aβ 1–42- induced TXNIP expression and ROS production in differentiated SH-SY5Y cells. (a) Western blot analysis of TXNIP and actin protein level in differentiated SH-SY5Y cells treated as indicated in the figure. This experiment is representative of 4 independent experiments. (b) Quantification of TXNIP protein level in differentiated SH-SY5Y cells treated as indicated in the figure. Actin has been used for normalization (N = 4, * = p < 0,01 versus control untreated cells, # = p < 0,01 versus Aβ1–42 treated cells). (c) Analysis of ROS production in differentiated SH-SY5Y cells treated as indicated in the figure (N = 4, * = p < 0,01 versus control untreated cells, # = p < 0,01 versus Aβ1–42 treated cells).
We next investigated whether TXNIP expression mediates Aβ1–42-induced ROS formation. We observed an increase of ROS due to Aβ1–42 treatment, which was inhibited by the silencing of TXNIP, while scramble shRNA has no any effect on Aβ1–42-induced ROS production (Fig. 3c). The addition of Verapamil as well as of NAC totally prevented Aβ1–42-induced ROS formation (Fig. 3c), suggesting that Verapamil prevents Aβ1–42-induced ROS formation by inhibiting TXNIP expression.
We observed a reduction of the cell viability in cells treated with Aβ1–42 dimers and trimers (3 μM) (Fig. 4c). We verified that a lower concentration of Aβ1–42 dimers and trimers (0,5 μM), which showed the cell viability comparable to untreated cells (Fig. 4c), still induced TXNIP expression (Fig. 4a,b). The addition of Verapamil on untreated cells did not reveal any significant reduction of the cell viability (Fig. 4c) and ameliorated the viability of the cells treated with 3 μM Aβ1–42 dimers and trimers (Fig. 4c).
0,5 μM Aβ 1–42 induces TXNIP expression, p38 MAPK phosphorylation, and Ser202/Thr205 tau phosphorylation. (a) Western blot analysis of TXNIP, phosphorylated p38 MAPK, total p38 MAPK, Ser202/Thr205 tau phosphorylation, total tau, and actin protein level in differentiated SH-SY5Y cells treated with 0,5 μM Aβ1–42. This experiment is representative of 4 independent experiments. (b) Quantification of TXNIP, relative phosphorylated p38 MAPK, and relative Ser202/Thr205 phosphorylated tau protein level in differentiated SH-SY5Y cells treated as indicated in the figure. Actin has been used for normalization (N = 4, * = p < 0,01 versus control untreated cells). (c) Cell viability assay using the MTT test (see material and methods) in differentiated SH-SY5Y cells treated as indicated in the figure (N = 4, * = p < 0,05 versus untreated control cells, # = p < 0,05 versus cells treated with 3 μM Aβ1–42).
Aβ1–42 impairs microtubule binding activity of tau, which is restored by either TXNIP silencing or Verapamil
TXNIP is the inhibitor of Thioredoxin (Trx) (8 #35; 9 #160), which plays a pivotal role in blocking the cysteine oxidation of tau and subsequent ROS-induced reduction of microtubule polymerization capability of tau (5 #903). For this reason, we analyzed whether Aβ1–42 affected the capability of tau to bind the microtubule using a tau microtubule-binding activity assay (33 #898). Treatment with Aβ1–42 (3 μM) for 24 h reduced the level of tau associated to the taxol-stabilized microtubules (pellet fraction), while enhanced unbound tau (soluble fraction) (Fig. 5a,c,d, data normalized for tubulin expression). We also extrapolated the ratio between tau present in the soluble and pellet fraction, normalized for the analysis of tubulin expression obtaining similar results (Fig. 5b). Silencing of TXNIP as well as treatment with either NAC or Verapamil restored the capability of tau to bind the microtubules (Fig. 5a-d).
Verapamil, NAC and silencing of TXNIP inhibit Aβ 1–42- induced reduction of tau capability to interact with the microtubule. (a) Western blot analysis of total tau, Ser202/Thr205 phosphorylated tau, and tubulin in the soluble (S) and pellet (P) fraction protein level in differentiated SH-SY5Y cells treated as indicated in the figure. This experiment is representative of 4 independent experiments. (b) Quantification of the ratio of total tau in the S and P fraction (N = 4, * = p < 0,05 versus control untreated cells, # = p < 0,05 versus Aβ1–42 treated cells). (c) Quantification of the relative total tau in the soluble fraction (N = 4, * = p < 0,05 versus control untreated cells, # = p < 0,05 versus Aβ1–42 treated cells). (d) Quantification of the relative total tau in the pellet fraction (N = 4, * = p < 0,05 versus control untreated cells, # = p < 0,05 versus Aβ1–42 treated cells). (e) Quantification of the ratio of Ser202/Thr205 phosphorylated tau in the S and P fraction (N = 4, * = p < 0,05 versus control untreated cells, # = p < 0,05 versus Aβ1–42 treated cells).
We also found that Aβ1–42-induced impairment of tau association to the microtubules correlated with an enhanced Ser202/Thr205 tau phosphorylation in the soluble fraction (Fig. 5a,e). Silencing of TXNIP as well as treatment with either NAC or Verapamil resulted in a significant decrement of Ser202/Thr205 tau phosphorylation in the soluble fraction, which correlated with an enhanced binding of tau to the microtubules (Fig. 5a,e).
Verapamil inhibits tau phosphorylation at Ser202/Thr205 by blocking ROS-TXNIP-p38 MAPK pathway
Several studies indicate that p38 MAPK is implicated in tau phosphorylation (6 #906; 7 #899; 10 #907). Notably, it has clearly shown that p38 MAPK is essential for tau phosphorylation in the Ser202/Thr205 site (10 #907). Since TXNIP plays a key role in the activation of p38 MAPK (11 #914; 12 #644; 13 #913; 14 #89; 15 #122), we analyzed whether TXNIP is necessary for Aβ1–42-induced Ser202/Thr205 tau phosphorylation. We first investigated whether phosphorylated p38 MAPK is enhanced in the hippocampus of 5 months old 5xFAD mice by an ELISA assay. We demonstrated that phosphorylated p38 MAPK is enhanced in the hippocampus of 5xFAD mice compared to the age matched control littermates and that the treatment of Verapamil restores the basal level of p38 MAPK phosphorylation (Fig. 6a). We next analyzed whether treatment with 3 μM Aβ1–42 enhanced p38 MAPK phosphorylation in differentiated SH-SY5Y cells and whether TXNIP mediates the effect induced by Aβ1–42. Addition for 24 h of Aβ1–42 (3 μM) resulted in enhanced p38 MAPK phosphorylation (Fig. 6b). We observed similar results by treating the cells with 0,5 μM of Aβ1–42 (Fig. 4a,b) Silencing of TXNIP, as well treatment with either NAC or Verapamil inhibited Aβ1–42-induced p38 MAPK phosphorylation (Fig. 6b). We verified that the p38 MAPK-specific inhibitor SB203580 blocked Aβ1–42-induced p38 MAPK phosphorylation (Fig. 6b). Finally, we assessed whether the TXNIP-ROS-p38 MAPK pathway was implicated in tau phosphorylation at Ser202/Thr205. Treatment with Aβ1–42 (3 μM) for 24 h produced a significant increase of tau phosphorylation (Fig. 6c,d). We observed similar results by treating the cells with 0,5 μM of Aβ1–42 (Fig. 4a,b) Silencing of TXNIP, as well treatment with either NAC or Verapamil inhibited Aβ1–42-induced p38 MAPK phosphorylation (Fig. 6b). Silencing of TXNIP, treatment with either NAC or Verapamil, as well addition of SB203580 blocked Aβ1–42-induced tau phosphorylation (Fig. 6c,d). We used as control of these experiments SH-SY5Y stably expressing a scramble shRNA. We verified that siScramble SH-SY5Y cells did not show any alteration in tau and p38 MAPK phosphorylation both at basal conditions and after treatment with Aβ1–42 (3 μM) compared to wild type SH-SY5Y (Supplementary Fig. 2 A-C).
Verapamil inhibits tau Sr202/Thr205 phosphorylation by blocking the TXNIP/ROS/p38 MAPK pathway. (a) ELISA analysis of phosphorylated p38 MAPK normalized for total p38 MAPK from the protein extract derived from the hippocampus of: age matched control mice, 5 months old 5xFAD mice, and 5 months old 5xFAD mice treated 3 months with oral administration of Verapamil (N = 6, * = p < 0,05 versus control mice, # = p < 0,05 versus 5xFAD mice). (b) ELISA analysis of phosphorylated p38 MAPK normalized for total p38 MAPK from the protein extract derived from differentiated SH-SY5Y cells treated as described in the figure (N = 4, * = p < 0,01 versus control untreated cells, # = p < 0,01 versus Aβ1–42 treated cells). (c) Western blot analysis of Ser202/Thr205 phosphorylated tau, total tau, and actin (normalization) of protein extracts derived from differentiated SH-SY5Y cells treated as described in the figure. This experiment is representative of 4 independent experiments. (d) Quantification of Ser202/Thr205 phosphorylated tau protein level in differentiated SH-SY5Y cells treated as described in the figure (normalized for total tau and actin protein level, N = 4, * = p < 0,01 versus control untreated cells, # = p < 0,05 versus Aβ1–42 treated cells).
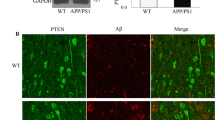
TXNIP is over-expressed in neuronal cells of human AD patients and colocalizes with tau
We analyzed 4 human brain samples: 2 controls without dementia and 2 AD. TXNIP was over-expressed exclusively in the brain of AD patients, while not demented controls showed lower TXNIP expression (Fig. 7a,b). Tau completely co-localized with TXNIP (Fig. 7c). Although we analyzed a very limited number of human samples, these data supported the role of TXNIP in modulating tau function.
TXNIP is over expressed in the hippocampus of AD patients. (a) representative IHC analysis of TXNIP expression in hippocampal section of control and AD patients. Bars: 9 μm. Magnification of some areas is shown in the insets. (b) quantification of TXNIP staining in different areas of the hippocampus of control and AD patients. Quantification is performed on four brains, N > 80 cells. Error bars, ± SD, p < 0,01. (c) Representative IHC analysis of TXNIP and tau in hippocampal section of AD patients.
Discussion
Although TXNIP is one of the most over expressed mRNA in the hippocampus of the AD patients and of the 3Tg AD mice (16 #363), there is not any study that investigate whether TXNIP is implicated in the pathophysiology of AD. TXNIP is the inhibitor of Trx and induces oxidative stress (8 #35; 9 #160). Oxidative stress induces tau phosphorylation at Ser202/Thr205 (7 #899). It has been clearly shown that p38 MAPK is essential for Ser202/Thr205 tau phosphorylation (10 #907). Since TXNIP plays a key role in the activation of p38 MAPK (11 #914; 12 #644; 13 #913; 14 #89; 15 #122), we focused our attention to analyze whether TXNIP mediates p38 MAPK induced tau phosphorylation at Ser202/Thr205. Herein we demonstrate that enhanced TXNIP expression in the hippocampus of the 5xFAD mice parallels enhanced phosphorylation of tau at Ser202/Thr205 and increased phosphorylation of p38 MAPK, reinforcing the hypothesis that TXNIP mediated p38 MAPK-dependent tau phosphorylation at Ser202/Thr205.
Verapamil, an inhibitor of L-type voltage gated calcium channels, inhibits TXNIP expression and ameliorates several pathologies, in which TXNIP plays a key role (34 #658; 17 #185; 18 #304). Aβ treatment activates L-type voltage sensitive calcium channels in neuronal cells (40 #897). Interestingly, Verapamil has been proposed as therapeutic agent for AD (19 #192; 41 #676). The oral administration of Verapamil in the drinking water efficiently inhibits TXNIP in mice and ameliorates the pathologic effect of TXNIP in animal models of diabetes and cardiovascular diseases (17 #185; 18 #304). For this reason, we analyzed whether the oral treatment with Verapamil inhibited TXNIP expression in the hippocampus of the 5xFAD mice. We did not investigate the uptake of Verapamil into the brain of the 5xFAD mice. Herein we report that 5xFAD mice treated with oral administration of Verapamil show a significant decrement of TXNIP expression. Although, we cannot exclude that the reduction of hippocampal expression of TXNIP is due to a peripheral effect of Verapamil, we show that the hippocampal reduction of TXNIP correlated with a decreased tau phosphorylation at Ser202/Thr205 and p38 MAPK phosphorylation, further reinforcing the hypothesis that TXNIP is necessary to mediate p38 MAPK-dependent Ser202/Thr205 tau phosphorylation. In agreement with this hypothesis, a peptide blocking TXNIP activity completely inhibits p38 MAPK phosphorylation in mice brain (12 #644).
The 5xFAD mice show a cerebrovascular and inflammatory pathology (42 #832). We have unpublished data showing that TXNIP is also early over expressed in the brain micro-vessels and in the glial cells in the cortex and hippocampus of the 5xFAD mice. These data are the subject of another manuscript in preparation. Indeed, TXNIP plays a key role in inflammation and vascular dysfunction (20 #283). Thus, we cannot exclude that the Verapamil-dependent reduction of the phosphorylation of p38 MAPK and tau at Ser202/Thr205 in the hippocampus of the 5xFAD mice are the consequence of a decreased expression of TXNIP in glial and endothelial cells of the 5xFAD mice brains. However, in support to a role of TXNIP in neuronal cells, Verapamil suppresses TXNIP-mediated neurotoxicity in the retina, by inhibiting TXNIP expression and blocking p38 MAPK activation (34 #658).
To confirm that neuronal expression of TXNIP plays a causative role in promoting Ser202/Thr205 tau phosphorylation, we analyzed in detail the TXNIP-dependent signaling pathways in differentiated SH-SY5Y neuronal cells. We treated the cells with Aβ1–42 dimers and trimers, which has been reported to produce neuronal dysfunction (37 #142; 43 #124). In addition, we previously reported that the addition of Aβ1–42 dimers and trimers to differentiated SH-SY5Y cells leads also to the formation of intracellular toxic oligomers (23 #189). In the present study, we clearly show that silencing of TXNIP abolishes Aβ1–42-induced ROS formation, p38 MAPK activation and tau phosphorylation at Ser202/Thr205 in differentiated SH-SY5Y cells. We dissected in detail the signaling pathway induced by TXNIP. Treatment with the anti-oxidant NAC reduced Aβ1–42-induced TXNIP expression, as previously reported (27 #377), as well abolishes p38MAPK phosphorylation and tau phosphorylation at Ser202/Thr205., Since NAC reduces also TXNIP expression, we cannot stress the role of oxidative stress in promoting Sr202/Thr205 tau phosphorylation. On the contrary, inhibition of p38 MAPK activation by SB203580 treatment blocks Aβ1–42-induced Sr202/Thr205 tau phosphorylation, demonstrating that p38 MAPK acts down-steam TXNIP. In agreement, silencing of TXNIP abolishes Aβ1–42-induced p38 MAPK phosphorylation. According to the data obtained by silencing TXNIP in differentiated SH-SY5Y cells, we can conclude that TXNIP mediates Aβ1–42-induced tau phosphorylation at Ser202/Thr205 by activating the p38 MAPK pathway. Verapamil ameliorates Aβ1–42-dependent TXNIP expression, ROS production, p38 MAPK activation and tau phosphorylation at Ser202/Thr205 in differentiated SH-SY5Y cells, strongly suggesting that the beneficial effects of Verapamil in reducing tau phosphorylation are at least in part mediated by the suppression of the TXNIP/ROS/p38 MAPK pathway.
We cannot exclude that Verapamil may prevent tau phosphorylation in other sites and this is not the object of this study. Indeed, herein we clearly focus and show the role of TXNIP in mediating p38 MAPK-dependent tau phosphorylation at Ser202/Thr205. This study provides new findings and describes for the first time a TXNIP-pathway that is involved in the pathogenesis of AD.
We show that oral treatment with Verapamil ameliorates amyloid plaques formation in the 5xFAD mice. These data suggest that Verapamil may have other effect than acting on TXNIP expression in the 5xFAD mice. The use of Verapamil is still debated, since the overdose of Verapamil may produce toxicity and induce patient mortality (44 #918). In the present study we used an oral concentration of Verapamil that has been shown to do not produce toxicity in mice (17 #185; 18 #304). In addition, the animals were treated for a limited time (3 months), in which we did not observe any effect due to a Verapamil overdose. Our study is of interest, because it unveils the effect of Verapamil on tau phosphorylation and on the downstream effects of TXNIP in neuronal cells. Thus, this study can be a support for the understanding of the mechanisms induced by this compound and open the way for the amelioration of this therapy and the prevention of the cytotoxicity induced by a Verapamil overdose.
TXNIP is the inhibitor of Trx (8 #35; 9 #160), which is important to block the cysteine oxidation of tau due to the oxidative stress (5 #903). Such oxidative protein modification reduces the capability of tau to associate with the tubulin (5 #903). For this reason, we first investigated whether Aβ1–42 alters tau capability to bind the microtubules. We show that Aβ1–42 reduces tau capability to interact with the microtubules. Treatment with the anti-oxidant NAC restores Aβ1–42-dependent alterations in tau capability to associate with the microtubules. The same effect is produced by Verapamil and by silencing of TXNIP, showing that TXNIP alters tau capability to binds the microtubules that correlates with enhanced Ser202/thr205 tau phosphorylation. Interestingly, we show that TXNIP co-localizes with tau in the cellular bodies of hippocampal neurons in AD patients. Although we examined a very limited number of human samples, these data are supportive of the role of TXNIP in modulating the activity of tau.
In conclusion, we dissected a signaling pathway induced by TXNIP and leading to tau phosphorylation at Ser202/Thr205, which correlates with impaired tau capability to bind the microtubules. We also show that Verapamil blocks this pathway by inhibiting TXNIP expression, providing a new mechanism of action of this drug that can be a support for the understanding of the Verapamil down-stream effects.
Change history
11 September 2024
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1007/s11095-024-03767-2
Abbreviations
- AD:
-
Alzheimer’s Disease
- APP:
-
Amyloid Precursor Protein
- Aβ1–42 :
-
Amyloid beta peptide 1–42
- DMEM:
-
Dulbecco’s modified eagle medium
- DNA:
-
Deoxyribonucleic acid
- FBS:
-
Fetal bovine serum
- IHC:
-
Immunohistochemistry
- MAPK:
-
Mitogen Activated Protein Kinase
- NAC:
-
N-acetyl-cysteine
- NTFs:
-
Neurofibrillary tangles
- PAGE:
-
Poly acrylamide gel electrophoresis
- PBS:
-
Phosphate buffered saline
- PCR:
-
Polymerase chain reaction
- PS1:
-
Presenilin 1
- ROS:
-
Reactive Oxygen species
- SDS:
-
Sodium Dodecyl Sulfate
- shRNA:
-
Short hairpin RNA
- siRNA:
-
Small interfering RNA
- tau:
-
Tubulin-Associated Unit
- Trx:
-
Thioredoxin
- TXNIP:
-
Thioredoxin Interacting Protein
- WT:
-
Wild-type
References
Selkoe DJ. Alzheimer's disease: genes, proteins, and therapy. Physiol Rev. 2001;81:741–66.
Guo T, Noble W, Hanger DP. Roles of tau protein in health and disease. Acta Neuropathol. 2017;133:665–704.
Frandemiche ML, De Seranno S, Rush T, Borel E, Elie A, Arnal I, et al. Activity-dependent tau protein translocation to excitatory synapse is disrupted by exposure to amyloid-beta oligomers. J Neurosci. 2014;34:6084–97.
Pohanka M. Alzheimer’s disease and oxidative stress: a review. Curr Med Chem. 2014;21:356–64.
Landino LM, Skreslet TE, Alston JA. Cysteine oxidation of tau and microtubule-associated protein-2 by peroxynitrite: modulation of microtubule assembly kinetics by the thioredoxin reductase system. J Biol Chem. 2004;279:35101–5.
Giraldo E, Lloret A, Fuchsberger T, Viña J. Aβ and tau toxicities in Alzheimer's are linked via oxidative stress-induced p38 activation: protective role of vitamin E. Redox Biol. 2014;2:873–7.
Meng G, Liu J, Lin S, Guo Z, Xu L. Microcystin-LR-caused ROS generation involved in p38 activation and tau hyperphosphorylation in neuroendocrine (PC12) cells. Environ Toxicol. 2015;30:366–74.
Chung J, Jeon J, Yoon S, Choi I. Vitamin D3 upregulated protein 1 (VDUP1) is a regulator for redox signaling and stress-mediated diseases. J Dermatol. 2006;33:662–9.
Kim SY, Suh HW, Chung JW, Yoon SR, Choi I. Diverse functions of VDUP1 in cell proliferation, differentiation, and diseases. Cell Mol Immunol. 2007;4:345–51.
Lauretti E, Praticò D. Glucose deprivation increases tau phosphorylation via P38 mitogen-activated protein kinase. Aging Cell. 2015;14:1067–74.
Chen CL, Lin CF, Chang WT, Huang WC, Teng CF, Lin YS. Ceramide induces p38 MAPK and JNK activation through a mechanism involving a thioredoxin-interacting protein-mediated pathway. Blood. 2008;111:4365–74.
Cohen-Kutner M, Khomsky L, Trus M, Ben-Yehuda H, Lenhard JM, Liang Y, et al. Thioredoxin-mimetic peptide CB3 lowers MAPKinase activity in the Zucker rat brain. Redox Biol. 2014;2:447–56.
Liu W, Gu J, Qi J, Zeng XN, Ji J, Chen ZZ, et al. Lentinan exerts synergistic apoptotic effects with paclitaxel in A549 cells via activating ROS-TXNIP-NLRP3 inflammasome. J Cell Mol Med. 2015;19:191949–55.
Perrone L, Devi TS, Hosoya KC, Terasaki T, Singh LP. Thioredoxin Interacting Protein (TXNIP) induces inflammation through chromatin modification in retinal capillary endothelial cells under diabetic conditions. J Cell Physiol. 2009;221:262–72.
Sbai O, Devi TS, Melone MA, Feron F, Khrestchatisky M, Singh LP, et al. RAGE-TXNIP axis is required for S100B-promoted Schwann cell migration, fibronectin expression and cytokine secretion. J Cell Sci. 2010;123:4332–9.
Hokama M, Oka S, Leon J, Ninomiya T, Honda H, Sasaki K, et al. Altered expression of diabetes-related genes in Alzheimer's disease brains: the hisayama study. Cereb Cortex. 2014;24:2476–88.
Chen J, Cha-Molstad H, Szabo A, Shalev A. Diabetes induces and calcium channel blockers prevent cardiac expression of proapoptotic thioredoxin-interacting protein. Am J Physiol Endocrinol Metab. 2009;296:E1133–9.
Xu G, Chen J, Jing G, Shalev A. Preventing β-cell loss and diabetes with calcium channel blockers. Diabetes. 2012;61:848–56.
Popović M, Caballero-Bleda M, Popović N, Bokonjić D, Dobrić S. Neuroprotective effect of chronic verapamil treatment on cognitive and noncognitive deficits in an experimental Alzheimer's disease in rats. Int J Neurosci. 1997;92:79–93.
Perrone L, Sbai O, Nawroth PP, Bierhaus A. The complexity of sporadic Alzheimer's disease pathogenesis: the role of rage as therapeutic target to promote neuroprotection by inhibiting neurovascular dysfunction. Int J Alzheimers Dis. 2012;2012:734956–66.
Oakley H, Cole SL, Logan S, Maus E, Shao P, Craft J, et al. Intraneuronal beta-amyloid aggregates, neurodegeneration, and neuron loss in transgenic mice with five familial Alzheimer's disease mutations: potential factors in amyloid plaque formation. J Neurosci. 2006;26:10129–40.
Cohn RD, Durbeej M, Moore SA, Coral-Vazquez R, Prouty S, Campbell KP. Prevention of cardiomyopathy in mouse models lacking the smooth muscle sarcoglycan-sarcospan complex. J Clin Invest. 2001;107:R1–7.
Mazarguil H, Leveque C, Bartnik D, Fantini J, Gouget T, Funke SA, et al. A synthetic amino acid substitution of Tyr10 in Aβ peptide sequence yields a dominant negative variant in amyloidogenesis. Aging Cell. 2012;11:530–41.
The World Medical Association Declaration of Helsinki. Recommendations guiding physicians in biomedical research involving human subjects. (online publication) Revised October 2000); http://www.wma.net/e/policy/b3.html.
Consensus recommendations for the postmortem diagnosis of Alzheimer's disease. The national institute on aging, and reagan institute working group on diagnostic criteria for the neuropathological assessment of Alzheimer's disease. Neurobiol Aging. 1997;18(4 Supp):S1–S2.
Shipley MM, Mangold CA, Szpara ML. Differentiation of the SH-SY5Y human neuroblastoma cell line. J Vis Exp. 2016;108:53193.
Devi TS, Hosoya K, Terasaki T, Singh LP. Critical role of TXNIP in oxidative stress, DNA damage and retinal pericyte apoptosis under high glucose: implications for diabetic retinopathy. Exp Cell Res. 2013;319:1001–12.
Vincent A, Perrone L, Sullivan K, Backus C, Sastry A, Lastoskie C, et al. Receptor for advanced glycation end products activation injures primary sensory neurons via oxidative stress. Endocrinology. 2007;148:548–58.
Perrone L, Peluso G, Melone MA. RAGE recycles at the plasma membrane in S100B secretory vesicles and promotes Schwann cells morphological changes. J Cell Physiol. 2008;217:60–71.
Perrone L, Mothes E, Vignes M, Mockel A, Figueroa C, Miquel MC, et al. Copper transfer from Cu-Abeta to human serum albumin inhibits aggregation, radical production and reduces Abeta toxicity. Chembiochem. 2010;11:110–8.
Perrone L, Devi TS, Hosoya KC, Terasaki T, Singh LP. Inhibition of TXNIP expression in vivo blocks early pathologies of diabetic retinopathy. Cell Death Dis. 2010;1:e65.
Pines A, Perrone L, Bivi N, Romanello M, Damante G, Gulisano M, et al. Activation of APE1/Ref-1 is dependent on reactive oxygen species generated after purinergic receptor stimulation by ATP. Nucleic Acids Res. 2005;33:4379–94.
Ren QG, Liao XM, Wang ZF, Qu ZS, Wang JZ. The involvement of glycogen synthase kinase-3 and protein phosphatase-2A in lactacystin-induced tau accumulation. FEBS Lett. 2006;580:2503–11.
Al-Gayyar MM, Abdelsaid MA, Matragoon S, Pillai BA, El-Remessy AB. Thioredoxin interacting protein is a novel mediator of retinal inflammation and neurotoxicity. Br J Pharmacol. 2011;164:170–80.
Anekonda TS, Quinn JF, Harris C, Frahler K, Wadsworth TL, Woltjer RL. L-type voltage-gated calcium channel blockade with isradipine as a therapeutic strategy for Alzheimer's disease. Neurobiol Dis. 2011;41:62–70.
Girard SD, Jacquet M, Baranger K, Migliorati M, Escoffier G, Bernard A, et al. Onset of hippocampus-dependent memory impairments in 5XFAD transgenic mouse model of Alzheimer's disease. Hippocampus. 2014;24:762–72.
Selkoe DJ. Soluble oligomers of the amyloid beta-protein impair synaptic plasticity and behavior. Behav Brain Res. 2008;192:106–13.
Arbo BD, Marques CV, Ruiz-Palmero I, Ortiz-Rodriguez A, Ghorbanpoor S, Arevalo MA, et al. 4'-Chlorodiazepam is neuroprotective against amyloid-beta through the modulation of survivin and bax protein expression in vitro. Brain Res. 2016;1632:1691–7.
Azmi NH, Ismail M, Ismail N, Imam MU, Alitheen NB, Abdullah MA. Germinated brown rice alters Aβ(1-42) aggregation and modulates Alzheimer's disease-related genes in differentiated human SH-SY5Y cells. Evid Based Complement Alternat Med. 2015;2015:153684.
Ekinci FJ, Malik KU, Shea TB. Activation of the L voltage-sensitive calcium channel by mitogen-activated protein (MAP) kinase following exposure of neuronal cells to beta-amyloid. MAP kinase mediates beta-amyloid-induced neurodegeneration. J Biol Chem. 1999;274:30322–7.
Liu Y, Lo YC, Qian L, Crews FT, Wilson B, Chen HL, et al. Verapamil protects dopaminergic neuron damage through a novel anti-inflammatory mechanism by inhibition of microglial activation. Neuropharmacology. 2011;60:373–80.
Giannoni P, Arango-Lievano M, Neves ID, Rousset MC, Baranger K, Rivera S, et al. Cerebrovascular pathology during the progression of experimental Alzheimer's disease. Neurobiol Dis. 2016;88:107–17.
Shankar GM, Li S, Mehta TH, Garcia-Munoz A, Shepardson NE, Smith I, et al. Amyloid-beta protein dimers isolated directly from Alzheimer's brains impair synaptic plasticity and memory. Nat Med. 2008;14:837–42.
Tulgar S, Kose HC, Demir Piroglu I, Karakilic E, Ates NG, Demir A, et al. Comparison of effects of separate and combined sugammadex and lipid emulsion administration on hemodynamic parameters and survival in a rat model of verapamil toxicity. Med Sci Monit. 2016;22:984–90.
ACKNOWLEDGMENTS AND DISCLOSURES
This research was supported by a Marie-Curie International Reintegration grant number 224892, within the 7th European Community Framework Program to L.P and by funding from the University Grenoble Alpes to L.P. The authors have no conflict of interest to declare
Author information
Authors and Affiliations
Corresponding author
Additional information
Guest Editor: Davide Brambilla
Electronic Supplementary Material
Supplementary Figure 1
Western blot analysis of Aβ1–42 dimers and trimers solution prepared as described in the Material and Methods section. (GIF 40 kb)
Supplementary Figure 2
The transfection of the Scramble shRNA in SH-SY5Y cells does not alter the response to the treatment with Aβ 1–42 dimers and trimers. A. Western blot analysis of Ser202/Thr205 phosphorylated tau, total tau, phosphorylated p38 MAPK, total MAPK, and actin (normalization) of protein extracts derived from differentiated SH-SY5Y cells treated as described in the figure. This experiment is representative of 4 independent experiments. B. Quantification of the relative Ser202/Thr205 phosphorylated tau protein level in differentiated SH-SY5Y cells treated as indicated in the figure (N = 4, * = p < 0,01). C. Quantification of the relative phosphorylated p38 MAPK protein content in differentiated SH-SY5Y cells treated as indicated in the figure (N = 4, * = p < 0,01). (GIF 38 kb)
About this article
Cite this article
Melone, M.A.B., Dato, C., Paladino, S. et al. Verapamil Inhibits Ser202/Thr205 Phosphorylation of Tau by Blocking TXNIP/ROS/p38 MAPK Pathway. Pharm Res 35, 44 (2018). https://doi.org/10.1007/s11095-017-2276-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-017-2276-2