ABSTRACT
Purpose
To employ Doxorubicin-loaded liposomes, modified with YSA-peptide to target EphA2, to reduce adverse effects against primary bone cells and maximize toxicity against Saos-2 osteosarcoma cells.
Methods
PEGylated liposomes were prepared by thin film method using Dipalmitoylphosphatidylcholine (DPPC), cholesterol and distearylphosphatidylethanolamine-polyethyleneglycol conjugate (DSPE-mPEG) in 67.9:29.1:3 M ratios, and loaded with DOX (L-DOX) by pH-gradient method. Targeted liposomes (YSA-L-DOX), were prepared by conjugating YSA-peptide to DSPE-mPEG. Liposomes were physicochemically characterized and tested in cellular toxicity assays.
Results
YSA conjugation efficiency was >98%. Size and polydispersity index of both L-DOX and YSA-L-DOX were around 88 nm and 0.188, respectively. Both had similar zeta potential, and 85% DOX loading efficiencies. DOX release kinetics followed the Korsmeyer-Peppa model, and showed comparable release for both formulations from 1–8 h, and a plateau of 29% after 48 h. Both formulations could be stably stored for ≥6 months at 4°C in the dark. Toxicity assays showed a significant 1.91-fold higher cytotoxicity compared to free DOX in the Saos-2 cells, and 2-fold lesser toxicity in primary bone cells compared to the Saos-2 cells. Cellular uptake studies showed higher and more nuclear uptake in YSA-L-DOX compared to L-DOX treated cells.
Conclusions
YSA-L-DOX vesicles might be effective for targeted treatment of osteosarcoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Osteosarcoma (OS) is the most common primary malignant bone tumor in children and adolescents. There is a high tendency to metastatic spread; most metastases develop in the lungs. The 5-year survival rate for localized disease is approximately 65–70%. However, in patients with metastatic or recurrent disease, 5-year survival rates are reduced to 20% (1,2). At present, the gold standard for osteosarcoma treatment consists of neo-adjuvant chemotherapy, radical resection of the primary tumor and when feasible all metastases, followed by adjuvant chemotherapy. Despite this aggressive treatment regimen, treatment outcomes remain poor, especially in patients with metastatic disease (3). Attempts to improve treatment outcomes with dose escalation or variation in compounds used for treatment have thus far been unsuccessful. Apart from insufficient efficacy, the compounds used for chemotherapy in osteosarcoma are often accompanied by serious adverse effects (4). Ultimately, novel treatment strategies for osteosarcoma should improve treatment efficacy and reduce toxicity. Targeted treatment implies targeting tumor specific characteristics in order to enhance current treatments. Means of accomplishing this include, among others, the specific delivery of anticancer drugs to the tumor cells, thereby increasing effective dose in the tumor cells whilst sparing the cells in healthy tissues (5).
Doxorubicin (DOX), a topoisomerase-II inhibitor, is a broad-spectrum anti-neoplastic drug and is one of the key components of osteosarcoma treatment (6). Although broadly applied, Doxorubicin has a number of undesirable side effects, the most notorious of which is its cardiotoxicity, leading to congestive heart failure in patients treated with this compound. The side effects are noted to be dose-related. Local delivery to tumor cells may allow for a dose reduction while preserving Doxorubicin anti-cancer activity. Several studies have been performed on targeting the delivery of Doxorubicin to specific cells, both healthy and tumor cells (7,8). One method to apply in targeted delivery of Doxorubicin is the use of liposomes. Liposomes are spherical vesicles with an aqueous core and a vesicle shell. They contain a single or multiple bilayered membrane structure composed of natural or synthetic lipids. Doxorubicin can be encapsulated in the liposome and transported through the bloodstream without causing toxicity in surrounding tissues. Liposome vesicles themselves cause very little toxic or antigenic reactions and are biologically inert. Some liposomes are capable of delivering their drug load inside the cell and even inside different cell compartments (9). To deliver the Doxorubicin to osteosarcoma cells specifically, the nanovesicles would have to be targeted to cell surface receptors that are characteristic for osteosarcoma, i.e. surface molecules that are abundantly expressed on the tumor cells, but not on healthy cells.
In previous work, we identified the Ephrin Alpha 2 receptor (EphA2) as a surface molecule which is highly upregulated on osteosarcoma cells, both primary and metastatic. Ephrin receptors (Eph) are the largest group of receptor tyrosine kinases and ephrin receptors and ephrin ligands (EFN) have been studied widely in various tumors other than osteosarcoma (10). The Eph family is comprised of the EphA (EphA1 -- 10) or EphB (EphB1 -- 6) subclasses of receptors classified per their sequence homologies and their binding affinity for their ligands, ephrins (Eph receptor interacting protein) (2,3,4). EphA2 was first identified in 1990 (11). EphrinA1 was found to be a ligand for the EphA2 receptor based on its ability to bind the extracellular domain of the EphA2 receptor tagged to an affinity column (12). Interaction of EphA2 with its ligand (ephrinA1) triggers intracellular events that are important in tumorigenesis, such as proliferation, migration and cell survival (13).
Using a mass spectrometry approach, we determined the surface protein expression of osteosarcoma cell lines, primary osteosarcoma cells and healthy bone cells, and verified suitability for targeted delivery by demonstrating differential expression (high in tumor cells, low in normal bone cells). EphA2 expression was confirmed in cell lines and cells in culture by FACS analysis and in human tissue samples by immunohistochemistry (14).
The modification of liposomes with peptide ligands that target the tumor cells is expected to further improve the localization/delivery of drugs specifically to tumor cells. YSA (YSAYPDSVPMMS) is a 12- amino acid peptide which is an ephrin A1 mimic and a ligand for EphA2. Therefore, it could be used in targeted delivery of cytotoxic drugs to cancers such as osteosarcoma (15).
The aim of this proof-of-concept study is enhanced delivery of Doxorubicin to osteosarcoma cells by creating YSA-modified DOX-loaded liposomes, thus improving cellular uptake of Doxorubicin.
MATERIALS AND METHODS
Materials
Doxorubicin hydrochloride (DOX-HCl) was obtained from Ebewe Pharma (Austria). DiPalmitoylphosphatidylcholine (DPPC), Cholesterol and distearylphosphatidylethanolamine (mPEG2000-DSPE) were purchased from Lipoid GmbH (Ludwigshafen, Germany). DSPE-PEG-NHS (hydroxy succinamide, PEG Mw = 2000) was obtained from Nanocs. (New York, NY). Phosphate buffered saline tablets (PBS, pH 7.0) and the MTT (3-[4,5- dimethylthiazol-2-yl]-2,5-diphenyl tetrazolium bromid) assay were obtained from Sigma-Aldrich Co. (St. Louis, MO, USA).
Dialysis bags (MWCO 12000–14,000) were supplied by Jingkehongda Biotechnology Company (Beijing, China). The Saos-2 human osteosarcoma cell line was obtained from the Pasteur Institute (Tehran, Iran). DMEM cell culture medium was purchased from Gibco Invitrogen (GmbH, Karlsruhe, Germany). 4′,6-Diamidino-2-phenylindole (DAPI) and Dimethyl sulfoxide (DMSO) were obtained by Thermo Fisher Scientific (Waltham, Massachusetts, USA) and Sigma-Aldrich (St. Louis, MO), respectively. Chloroform, isopropanol and all other chemicals were analytical grade and were purchased from Merck chemical (Merck Millipore, USA).
YSA Synthesis
YSA peptide was synthesized by solid phase peptide synthesis using Fmoc protected amino acids (OrpegenPharma GmbH, Heidelberg, Germany and Novabiochem, Darmstadt, Germany) in a Syro II synthesizer (Biotage, Uppsala Sweden). YSA peptide was purified to a purity of at least 95% by repetitive RP-HPLC UltiMate 3000 Series (Thermo scientific, Massachusetts, USA) on a Vydac C18 column (218MS510, Vydac, Hesperia, CA, USA) and the authenticity of the YSA peptide was confirmed by MALDI-TOF mass spectrometry on a Microflex LRF mass spectrometer equipped with an additional gridless reflectron (Burker Daltonic, Bremen, Germany) (16).
Conjugation of YSA to PEGylated Lipid
YSA peptide was conjugated to DSPE-PEG2000-NHS in order to link the peptide to the surface of a nanovesicle (15). YSA peptide (24mg) and DSPE-PEG2000-NHS (100 mg) were dissolved in 2 ml dimethylformamide and 100 μl triethyl amine, pH 8.5. YSA peptide solution (1 ml) was mixed with 1 ml of DSPE-PEG2000-NHS solution and incubated for 48 h at RT. Samples were then precipitated by addition of cold diethyl ether and centrifuged (13,200 rpm for 3 times 10 min). The supernatant was decanted and the solid residue dissolved in Milli-Q water and lyophilized.
The lyophilate was dissolved in trifluoroacetic acid (TFA) and applied on a VYDAC C-18 column equilibrated in 0.1% TFA. Elution was performed in a linear gradient, from 10–60% acetonitrile containing 0.1% TFA in 35 min at a flow of 4ml/min (Jasco Corporation,Tokyo,Japan). The absorbance of the column effluent was monitored at 214 nm (Thermo Finnigan detector, San Jose,CA) to identify the proper elution fraction and its purity. The authenticity of DSPE-PEG-YSA was confirmed by MALDI-TOF Microflex (Burker Daltonic, Bremen, Germany).
Preparation of DOX -Liposomes
The lipid composition of non-targeted (L) and targeted (YSA-L) liposomes contained DPPC/ cholesterol/ DSPE-PEG (8.473 mg: 1.914 mg: 1.43 mg, i.e.67.9:29.1:3 M ratios) and DPPC/ cholesterol/ DSPE-PEG/ DSPE-PEG-YSA (8.473 mg: 1.914 mg: 1.14 mg: 0.325 mg; i.e. 67.9:29.1:2.4;0.6 M ratios), respectively. After dissolving the lipid in organic volatile solvent (chloroform), thin films were formed by applying vacuum at 55°C while rotating using a rotary evaporator.
1 cm3 of ammonium sulfate was used for hydration (1 h, 60°C), followed by applying a pH gradient by removing ammonium sulfate and replacing it with PBS (1 M, pH = 7.4, 25°C) using a dialysis membrane (12 kDa cut-off). Then the vesicle size was further reduced to make nano-scale vesicles using an ultra-probe sonicator (E–Chrom Tech Co, Taiwan) for 45 min at 100 W. DOX (1 cm3, 2 mg/ml) was encapsulated into liposomal dispersion with a total lipid-to-drug ratio of 10 (mol/mol) at 60°C for 45 min. Unloaded DOX was separated by size exclusion chromatography on a Sepharose CL-4B column. The prepared formulation was filtered through a 0.22- μm filter in order to sterilize for later use (17).
Physicochemical Characterization of Nanovesicles
As described previously, the measurement of hydrodynamic size and zeta potential of liposome vesicles was carried out by dynamic light scattering (Zeta-Sizer instrument, DLS, Malvern Zatasizer Nano-ZS, Worcestershire, UK) with a detection angle of scattered light at 90° (18). All measurements were performed four times and mean values of vesicle size and zeta potential were reported.
The surface morphology and the bilayers of the vesicles were examined by scanning electron microscopy (KYKY-EM3200-30KV, China) and Cryo-transmission electron microscopy analysis (FEI Tecnai 20, type Sphera, Oregon, USA).
DOX Loading Efficiency
Before conducting further experiments, YSA-L-DOX and L-DOX were extensively purified from free DOX. The loading efficiency of DOX in both liposomal formulations (YSA-L and L) was determined by high-performance liquid chromatography (HPLC UltiMate 3000 Series (Thermo scientific,Massachusetts USA) using a C18 column (150 mm × 4.6 mm, 218MS510, Vydac, Hesperia, CA, USA) at 25°C.
Liposomal DOX was mixed with isopropanol at a ratio of 1:20 (v/v) to break the phospholipid membranes. The mobile phase consisted of 0.1% TFA in water/ acetonitrile 25:75 v/v; the flow rate was set to 1.0 ml/min, the amount of loaded DOX per vesicle was measured at 480 nm wavelength. The chromatographic installation consisted of a Model 1525 pump (Waters Corporation, Milford, MA, USA),a Model 717 Plus auto-injector (Waters Corporation) and a Model 2487 variable wavelength UV detector (Waters Corporation) connected to the Millennium software.
Release Kinetics of DOX
The kinetic release profile of DOX from the vesicles was assessed by preparing 1 ml samples (YSA-L-DOX or L-DOX) in dialysis tubes floating in 10 ml PBS (at 37°C, pH = 7.4) with slight vibration. For 48 h at predetermined time intervals, 1 ml of PBS directly surrounding the dialysis tube was extracted and the absorbance intensity was read using UV/visible spectroscopy (model T80+, PG Instruments, United Kingdom) at 480 nm. The amount of DOX release was calculated by dividing the amount of DOX in the medium by the initial amount of DOX. Several semi-empirical mathematical models (listed in Table I) were used to describe the kinetic release data. Nonlinear regression analysis was performed using MATLAB software (version 7.8). The fitting quality was evaluated by the statistical functions which are noted below, namely χ2, RMSE and R 2:
Lower values of χ2 and RMSE, and also higher values of R 2 indicate better goodness of fit.
Stability Studies
The physical stability of the designed pharmaceutical formulation was monitored as a function of storage time at 4°C. The percentage of stable DOX-loaded liposomes (both targeted YSA-L-DOX and non-targeted L-DOX) as well as vesicle size was monitored at 14 days, 28 days, 3 month and 6 months.
Cell Lines and Culture
The Saos-2 human osteosarcoma cell line and primary bone cells were cultured in high-glucose DMEM supplemented with 10% Fetal Bovine Serum (FBS), 100 mg/mL penicillin and 100 mg/mL streptomycin in an incubator in a humidified atmosphere of 5% CO2 at 37°C.
Cell Viability Assay
An MTT assay was employed to determine cell viability and thus to compare the inhibitory effect of YSA-L-DOX and L-DOX on cell proliferation in Saos-2 and primary bone cells. Briefly, cells were seeded at a density of 104 cells/well in 96-well plates with 200 μL of DMEM, supplemented with 10% FBS for each well and incubated overnight. Then L, YSA-L, L-DOX, YSA-L-DOX and free DOX diluted in 200 μl of fresh medium were added for 48 h. Then 20 μL of MTT solution (5 mg/mL) was added to each well and cells were incubated for another 4 h under the same conditions in incubator. The supernatant of each well was decanted and 100 μL of DMSO was added to dissolve the solid residue. The Color intensity method was used to measure metabolic activity using an EPOCH Microplate Spectrophotometer (synergy HTX, Bio Tek, USA) at a reference wavelength of 570 nm. Cell viability was calculated as follows:
Cellular Transfection of Targeted Liposomal DOX
The in-vitro cellular uptake of YSA-L-DOX and L-DOX was investigated on seeded Saos-2 cells in 6-well plates at a cell density of 2 × 105 cells/well. Cells were grown overnight to reach 80% confluence and then washed two times with warm PBS. The cells were then treated with YSA-L-DOX or L-DOX while incubated during 3 h at 37°C. Then cells were washed three times with PBS and fixed with 4%, paraformaldehyde solution. Finally, the cells were incubated with DAPI solution (0.125 μg/mL) for 15 min. The uptake of DOX was compared between cells treated with YSA-L-DOX and L-DOX using fluorescence microscopy (Olympus, Japan) (27).
Statistical Analysis
All tests were performed at least three times and the results expressed as mean standard deviations. Statistical significance analysis of the data at the 95% confidence level was performed using ANOVA one-way test for all comparisons. A P-value less than 5% was considered significant.
RESULTS
YSA Synthesis & Authentication of YSA to PEGylated Lipid Conjucation
In order to coat the liposome structure with peptide, we conjugated DSPE-PEG-NHS to YSA. The molecular bonding took place between the NHS group of the DSPE-PEG-NHS and the a-amines of the YSA, as was assessed by Maldi-TOF mass spectrometry (Fig. 1). The conjugation efficiency was >98% (after purification unconjugated YSA 1187 Da was not detected). The narrow peak at 1187 Da (Fig. 1a) corresponds to YSA, the broad peak between 1500–2600 Da, centered at ~2000 Da (Fig. 1b) represented the DSPE-PEG-NHS compound, and the successful conjugation product)DSPE-PEG-YSA) is shown in Fig. 1c, with a mass of 2600–3400 Da. We then used the conjugated product for the preparation of YSA-L-DOX.
Physicochemical Characterization of the Nanovesicles
The vesicle size and polydispersity index (PDI) of the nanoparicles were around 88 nm and 0.188, respectively. Peptide incorporation did not influence the mean size or diameter and PDI. The zeta potential of peptide-incorporated formulation was −3.95 for YSA-L-DOX and was −2.34 for the non-peptide-incorporated formulation (L-DOX). Both formulations had a comparable zeta potential and were electrically negative of charge close to netural.
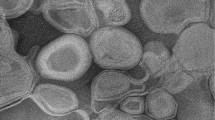
Figure 2 provides the cryo-TEM image of YSA-L-DOX. The TEM image clearly illustrates that our targeted liposome vesicles are round, membrane shapes structures. TEM also confirmed that our liposomal DOX samples consist of a mixture of multilamellar (two bilayers) and unilamellar liposomes and the majority had diameters of less than 100 nm. Additionally, the image shows that the vesicles tend to aggregate and form larger vesicles.
Figure 3 shows the SEM images of YSA-L-DOX. As can be seen, the prepared formulation has a smooth surface and spherical shape with less than 100 nm diameter.
DOX Loading Efficency
DOX was successfully loaded into YSA-L-DOX and L-DOX formulations. The loading efficiency for targeted and non-targeted formulations was 85.94% and 86.97%, respectively. The inclusion of the YSA-moiety in the targeted liposomes thus did not negatively affect the loading efficiency.
Stability Studies
Our stability studies involved two aspects, i.e. maintenance of vesicle size and DOX’ residual loading efficiency of both the targeted and non-targeted DOX-loaded liposome formulations when stored at 4°C in the dark for 6 months. The results (Fig. 4) show only a 4% change in vesicle size and a 6% change in residual loading efficency for L-DOX, and a 1% change in vesicle size and a 4% change in residual loading efficiency for YSA-L-DOX. Thus, both YSA-L-DOX and L-DOX can be stably stored for prolonged periods of time when kept at 4°C and in the dark.
Release Kinetics of DOX
The results of 48 h-release kinetics of DOX from YSA-L-DOX and L-DOX vesicles into surrounding PBS (pH 7.4) at 37°C are indicated in Fig. 5. Since the cut-off permeability of the dialysis membrane was 12–14 kDa, the DOX molecule could pass easily through the pores of membranes and therefore, the dialysis membrane can be considered non-limiting for DOX release. Thus, mainly the liposome formulation affected the DOX transfer from the vesicles into the PBS. DOX was released a little faster from the targeted formulation than from the non-targeted formulation at the start of the experiment (t = 0-1 h). However, at the following time points (t = 8 h), the release of DOX was comparable between the formulations. In both formulations, drug release into PBS took place rapidly. At the end of experiment (t = 48 h) the release of DOX had reached a constant level and did not alter anymore. After 48 h, around 29% of DOX had been released from the vesicles. Drug release was not significantly influenced by the targeting ligand.
To determine which semi-empirical mathematical model (listed in Table I) would best fit our experimental data, we subsequently assessed the fitting quality using three statistical functions, i.e. the χ2, RMSE and R2 methods (see Fig. 6). The kinetic model constants were calculated as well (Table II).
According to the results listed in Fig. 6, the Korsmeyer-Peppa release kinetics model is preferred, since lowest values of χ2 and RMSE, and highest values of R2 (all indicative of optimal curve fit) were obtained applying this model compared to the other models. From Table II, it can be deduced that for this model, the average values of the model coefficients n and k are 0.413 and 0.0664, respectively, when combining the values for the targeted and non-targeted formulations.
Cell Viability Assay
To verify the enhanced antitumor effects of the targeted formulation on osteosarcoma cells, a viability assay was carried out with 5 μg/ml of L, YSA, YSA-L, DOX, L-DOX and YSA-L-DOX. Cell viability results (Fig. 7) showed that the proliferation of Saos-2 and primary bone cells was greatly inhibited by the presence of DOX, and this inhibition was stronger when liposome-encapsulated DOX (L-DOX and YSA-L-DOX) was added. Drug free liposome (L, YSA and YSA-L) did not show any toxicity and even enhanced cell proliferation. Our data showed that non-targeted liposomal delivery (L-DOX) to Saos-2 cells increased the cytotoxicity of DOX 1.27 fold, whereas the targeted DOX formulation (YSA-L-DOX) was significantly (1.91 fold) more effective when compared to free DOX. YSA-L-DOX showed 1.5 fold higher Saos-2 toxicity compared to its non-targeted counterpart (L-DOX). The osteosarcoma cell: primary bone cell kill ratio increased from 1.36 (free DOX) to 1.48 (L-DOX) to 1.82 (YAS-L-DOX). This ratio increase, in combination with the increased Saos-2 cell killing upon targeting, confirmed the postulated added value of targeting.
Cellular Transfection of Targeted Liposomal DOX
Saos-2 cells were treated with L-DOX or YSA-L-DOX and post-labeled with DAPI nuclear staining to study DOX uptake and subcellular localization of DOX. Fig. 8 (a) and (b) display fluorescence microscopy images of Saos-2 cells treated with L-DOX and YSA-L-DOX. Due to the intrinsic red fluorescence of DOX, intracellular DOX localization could be visualized. It was evident that cells treated with YSA-L-DOX showed higher florescence intensity than cells treated with L-DOX. When assessing the cellular compartment localization and distribution of both formulations, YSA-L-DOX mostly accumulated in the nucleus, while L-DOX mostly accumulated in the perinuclear region and cytoplasm.
Intracellular localization by in vitro fluorescence microscopy images of DOX accumulation in Saos-2 cells after 3 h incubation with L-DOX (a) and YSA-L-DOX (b). DOX concentration of both formulations was 0.5 mg/ml. Red fluorescence is for DOX. Blue fluorescence is for DAPI. Superimposition of DAPI and DOX is represented by bright pink color.
Another interesting observation which confirms the impact of targeting was related to a morphological change of cell nucleus, i.e. from spherical to elliptical, which implies decomposition of nucleus.
DISCUSSION
This paper is a proof-of-concept study to evaluate whether enhanced systemic delivery and improved cellular uptake of Doxorubicin by osteosarcoma cells could be achieved by creating YSA-modified DOX-loaded liposomes. Targeted delivery of drugs to tumor cells specifically should protect healthy cells from the cytotoxicity brought about by chemotherapy and may allow clinicians to reduce the dose needed to treat the tumor effectively, and/or to increase the dose to levels not possible with systemic free drug treatment.
We employed the PEGylated liposome formulation which we selected after extensive optimization studies (17), and introduced a targeting moiety by covalent conjugation of YSA peptides to 20% of the DSPE-mPEG 2000 molecules used to create the nanovesicles. Our current studies showed that the YSA conjugation had a very high efficiency (98%). Moreover, comparison of the physicochemical characteristics (vesicle size, polydispersity indexes, morphology, zeta potential, and DOX loading efficiency) of the non-targeted and YSA-targeted formulations demonstrated that the YSA conjugation did not affect the PEGylated liposome characteristics. Similar findings were reported previously (15,16,28,29).
To be clinically relevant, easily applicable, and cost-effective, the liposome formulations should preferably be available as an off-the-shelf product. Therefore, stability studies were performed. Both formulations could be stably stored for ≥6 months at 4°C in the dark, thus confirming their suitability for off-the-shelf use. Although speculative, it could be that the fact that our liposome preparations are electrically negatively charged and close to neutral may contribute to their remarkable stability profile.
Since the liposome preparations are intended for increased systemic safety as well as (targeted) controlled release applications, cell-free DOX release profiles were assessed. As can be deduced from Fig. 5, at pH 7.4 the DOX release from the liposomes showed a rapid, linear release in the first 8 h up till about 24%, whereafter a plateau was reached around 29% after 48 h. We evaluated seven different release kinetics models, and concluded that the DOX release kinetics from our formulations followed the Korsmeyer-Peppa model. This Korsmeyer-Peppa model has been previously used to describe the first step of drug release (30). In the proposed model of drug release, k is the kinetic constant and n is the diffusion exponent describes the mechanism of drug release and depends on the geometry of the under study system. The drug release by the liposome formulation when n is close to 0.45 (for spherical shape) occurs by Fickian diffusion mechanism as a major limited mechanism of drug release (31,32). Another raised advantage is maybe long-term in-vivo maintenance of YSA-L-DOX so that according to the Korsmeyer-Peppa kinetic model a period of 743 h (31 days) is required for complete release of DOX from YSA-L-DOX.
Intuitively, one would argue that this low release would be a disadvantage: a high boost release will kill tumor cells more effectively. However, for systemic use, a boost release prior to docking to the tumor cells should be avoided to prohibit adverse systemic effects. In this regard, our liposomal carriers are optimized in three ways: First, they have previously been shown to release DOX at a higher level under tumor conditions (pH 5.4; see (17)). Second, receptor-mediated internalization and subsequent DOX release intracellularly should enhance DOX efficacy as well (16). The latter was confirmed by our cellular transfection studies, in which cells treated with YSA-L-DOX showed higher DOX florescence intensity than cells treated with L-DOX. Moreover, more pronounced accumulation in the nucleus was observed upon YSA-L-DOX delivery, while in the case of L-DOX most of the DOX was located in the perinuclear region and cytoplasm. Our findings confirm results from other reports (15,16). Last but not least: Our prepared liposomes are negatively charged and close to neutral, so we may assume that electrostatic forces will not play a role to increase cellular uptake. Furthermore, as indicated in DOX release profile (Fig. 5), DOX release from YSA-L-DOX was slow so that the only 6% of DOX released during the 3 hr-incubation for transfection test. So it supports our assumption that most red florescence intensity observed was related to YSA-L-DOX transfected to nucleus.
A further proof of enhanced efficacy of targeted liposomal delivery of DOX was provided in the cellular toxicity tests. For example, YSA-L-DOX (expected, based on the release kinetics profile to release only 28% of its DOX content) caused 1.91-fold higher Saos-2 cell kill than free DOX, and the non-targeted counterpart (L-DOX) showed 1.5 fold lesser cytotoxicity. Since the physicochemical characteristics of L-DOX and YSA-L-DOX formulation were quite similar, this implies that the specific targeting using YSA appears to be the most important factor in increasing toxicity and cellular uptake. It also improved safety profiles: primary bone cells were affected 2-fold less when compared to the Saos-2 cells. This confirms earlier findings of our group (14).
In summary, our data showed that a novel drug delivery system could be prepared to overcome systemic adverse effects of DOX while improving drug delivery to cancer cells. We report that modification of the surface of liposomes with YSA peptide can efficiently target the vesicle to the human Saos2 osteosarcoma cell line, thereby generating a large therapeutic index of prepared formulation compared to free DOX. Although currently demonstrating the therapeutic effects of EphA2 targeted liposomal DOX for osteosarcoma, we envision that this targeted nano-carrier system could be generalized for other cancers as well, particularly those (over)expressing EphA2. Future studies should encompass in vivo studies for further evaluation of the efficacy of YSA-L-DOX for combating osteosarcoma metastatic disease.
ACKNOWLEDGMENTS AND DISCLOSURES
The authors are grateful to Dr. Fatemeh Hakimian, Department of Biophysics, Institute of Biochemistry and Biophysics, University of Tehran, Tehran, Iran for scientific assistance during the project. The authors thank Dr. Fatemeh Montazeri, Recurrent abortion center, Reproductive science institute, Yazd Shahid Sadoughi University of Medical Science, Yazd, Iran.
Abbreviations
- DOX-HCl:
-
Doxorubicin hydrochloride
- Eph:
-
Ephrin receptors
- EphA2:
-
Ephrin Alpha 2 receptor
- exp:
-
Experimental
- L:
-
Liposome
- PDI:
-
Polydispersity index
- pre:
-
Predicted
- YSA-L:
-
Targeted liposome with YSA peptide
REFERENCES
De Boer JP. Towards targeted treatment for osteosarcoma. VU University Medical Center; 2014.
Ta HT, Dass CR, Choong PFM, Dunstan DE. Osteosarcoma treatment: state of the art. Cancer Metastasis Rev. 2009;28(1-2):247–63. Springer
Machak GN, Tkachev SI, Solovyev YN, Sinyukov PA, Ivanov SM, Kochergina NV, et al. Neoadjuvant chemotherapy and local radiotherapy for high-grade osteosarcoma of the extremities. Mayo Clin Proc [Internet]. 2003;78(2):147–55. Elsevier. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0025619611625469
Smeland S, Wiebe T, Böhling T, Brosjö O, Jonsson K, Alvegård T. Chemotherapy in osteosarcoma: the Scandinavian Sarcoma group experience. Acta Orthop Scand. 2004;75(Supplement 311):92–8. Taylor & Francis Group
Szakács G, Paterson JK, Ludwig JA, Booth-Genthe C, Gottesman MM. Targeting multidrug resistance in cancer. Nat Rev Drug Discov. 2006;5(3):219–34. Nature Publishing Group
Tacar O, Sriamornsak P, Dass CR. Doxorubicin: an update on anticancer molecular action, toxicity and novel drug delivery systems. J Pharm Pharmacol. 2013;65(2):157–70. Wiley Online Library
Du C, Deng D, Shan L, Wan S, Cao J, Tian J, et al. A pH-sensitive doxorubicin prodrug based on folate-conjugated BSA for tumor-targeted drug delivery. Biomaterials. 2013;34(12):3087–97. Elsevier
Elbialy NS, Fathy MM, Khalil WM. Doxorubicin loaded magnetic gold nanoparticles for in vivo targeted drug delivery. Int J Pharm. 2015;490(1):190–9. Elsevier
Ahmed M, Moussa M, Goldberg SN. Synergy in cancer treatment between liposomal chemotherapeutics and thermal ablation. Chem Phys Lipids [Internet]. 2012;165(4):424–37. Elsevier. Available from: http://linkinghub.elsevier.com/retrieve/pii/S000930841100363X
Varelias A, Koblar SA, Cowled PA, Carter CD, Clayer M. Human osteosarcoma expresses specific ephrin profiles. Cancer. 2002;95(4):862–9. Wiley Online Library
Lindberg RA, Hunter T. cDNA cloning and characterization of eck, an epithelial cell receptor protein-tyrosine kinase in the eph/elk family of protein kinases. Mol Cell Biol Am Soc Microbiol. 1990;10(12):6316–24.
Bartley TD, Hunt RW, Welcher AA, Boyle WJ, Parker VP, Lindberg RA, Lu HS, Colombero AM, Elliott RL, Guthrie BA, Holst PL. B61 is a ligand for the ECK receptor protein-tyrosine kinase. Nature. 1994;368(6471):558–60.
Pasquale EB. Eph receptors and ephrins in cancer: bidirectional signalling and beyond. Nat Rev Cancer. 2010;10(3):165–80. Nature Publishing Group
Posthumadeboer J, Piersma SR, Pham TV, van Egmond PW, Knol JC, Cleton-Jansen AM, et al. Surface proteomic analysis of osteosarcoma identifies EPHA2 as receptor for targeted drug delivery. Br J Cancer. 2013;109(8):2142–54. Nature Publishing Group
Wang J, Liu Y, Li Y, Dai W, Guo Z, Wang Z, et al. EphA2 Targeted Doxorubicin Stealth Liposomes as a Therapy System for Choroidal Neovascularization in RatsYSA-SSL-DOX Improving DOX Efficacy in CNV Rat. Invest Ophthalmol Vis Sci. 2012;53(11):7348–57. The Association for Research in Vision and Ophthalmology
Shahin M, Soudy R, El-Sikhry H, Seubert JM, Kaur K, Lavasanifar A. Engineered peptides for the development of actively tumor targeted liposomal carriers of doxorubicin. Cancer Lett. 2013;334(2):284–92. Elsevier
Haghiralsadat F, Amoabediny G, Sheikhha MH, Zandieh-doulabi B, Naderinezhad S, Helder MN, Forouzanfar T. New liposomal doxorubicin nanoformulation for osteosarcoma: drug release kinetic study based on thermo and pH sensitivity. Chem Biol Drug Des. 2017. http://onlinelibrary.wiley.com/doi/10.1111/cbdd.12953/full.
Haghiralsadat F, Amoabediny G, Sheikhha MH, Forouzanfar T, Helder MN, Zandieh-doulabi B. A novel approach on drug delivery: investigation of a new nano-formulation of liposomal doxorubicin andbiological evaluation of entrapped doxorubicin on various osteosarcoma cell lines. Cell J (Yakhteh). 2017;19 Suppl 1:55.
Narsimhan B, Mallapragada SK, Peppas NA. Release Kinetics, Data Interpretation. In: Mathiowitz E, editor. Encyclopedia of Controlled Drug Delivery. New York: Wiley; 1999. p. 921.
Bourne DW. Pharmacokinetics In: Modern pharmaceutics. New York: Marcel Dekker Inc; 2002.
Thawatchai P, Tamotsu K, Garnpimol CR. Chitosan citrate as film former: compatibility with water-soluble anionic dyes and drug dissolution from coated tablet. Int J Pharm. 2000;198:97–111.
Hixson AW, Crowell JH. Dependence of reaction velocity upon surface and agitation. Ind Eng Chem. 1931;23(10):1160–8. ACS Publications
Higuchi T. Rate of release of medicaments from ointment bases containing drugs in suspension. J Pharm Sci. 1961;50(10):874–5. Wiley Online Library
Higuchi T. Mechanism of sustained-action medication. Theoretical analysis of rate of release of solid drugs dispersed in solid matrices. J Pharm Sci. 1963;52(12):1145–9. Wiley Online Library
Ritger PL, Peppas NA. A simple equation for description of solute release II. Fickian and anomalous release from swellable devices. J Control Release. 1987;5(1):37–42. Elsevier
Barzegar-Jalali M, Adibkia K, Valizadeh H, Shadbad MRS, Nokhodchi A, Omidi Y, et al. Kinetic analysis of drug release from nanoparticles. J Pharm Pharm Sci. 2008;11(1):167–77. Canadian Society for Pharmaceutical Sciences
Naderinezhad S, Ghasem Amoabediny FH, Naderinezhad S, Amoabediny G, Haghiralsadat F. Co-delivery of hydrophilic and hydrophobic anticancer drugs using biocompatible pH-sensitive lipid-based nano-carrier for multidrug-resistant cancers. RSC Adv [Internet]. 2017;7(48):30008–19. The Royal Society of Chemistry. Available from: https://doi.org/10.1039/C7RA01736G
Yang T, Li B, Qi S, Liu Y, Gai Y, Ye P, et al. Co-delivery of doxorubicin and Bmi1 siRNA by folate receptor targeted liposomes exhibits enhanced anti-tumor effects in vitro and in vivo. Theranostics. 2014;4(11):1096–111. Ivyspring International Publisher
Kibria G, Hatakeyama H, Ohga N, Hida K, Harashima H. Dual-ligand modification of PEGylated liposomes shows better cell selectivity and efficient gene delivery. J Control Release. 2011;153(2):141–8. Elsevier
Mourtas S, Fotopoulou S, Duraj S, Sfika V, Tsakiroglou C, Antimisiaris SG. Liposomal drugs dispersed in hydrogels: effect of liposome, drug and gel properties on drug release kinetics. Colloids Surf B Biointerfaces. 2007;(2):55, 212–221. Elsevier
Sanson C, Schatz C, Le Meins J-F, Soum A, Thévenot J, Garanger E, et al. A simple method to achieve high doxorubicin loading in biodegradable polymersomes. J Control Release. 2010;147(3):428–35. Elsevier
Haghiralsadat F, Amoabediny G, Helder MN, Naderinezhad S, Sheikhha MH, Forouzanfar T, et al. A comprehensive mathematical model of drug release kinetics from nano-liposomes, derived from optimization studies of cationic PEGylated liposomal doxorubicin formulations for drug-gene delivery. Artif Cells, Nanomedicine, Biotechnol [Internet]. 2017:1–9. Available from: https://doi.org/10.1080/21691401.2017.1304403. Taylor & Francis
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haghiralsadat, F., Amoabediny, G., Naderinezhad, S. et al. EphA2 Targeted Doxorubicin-Nanoliposomes for Osteosarcoma Treatment. Pharm Res 34, 2891–2900 (2017). https://doi.org/10.1007/s11095-017-2272-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-017-2272-6