Abstract
Purpose
Nanoparticles formulated from the biodegradable co-polymer poly(lactic-co-glycolic acid) (PLGA), were investigated as a drug delivery system to enhance tissue uptake, permeation, and targeting for PSC-RANTES anti-HIV-1 activity.
Materials and Methods
PSC-RANTES nanoparticles formulated via a double emulsion process and characterized in both in vitro and ex vivo systems to determine PSC-RANTES release rate, nanoparticle tissue permeation, and anti-HIV bioactivity.
Results
Spherical, monodisperse (PDI = 0.098 ± 0.054) PSC-RANTES nanoparticles (d = 256.58 ± 19.57 nm) with an encapsulation efficiency of 82.23 ± 8.35% were manufactured. In vitro release studies demonstrated a controlled release profile of PSC-RANTES (71.48 ± 5.25% release). PSC-RANTES nanoparticle maintained comparable anti-HIV activity with unformulated PSC-RANTES in a HeLa cell-based system with an IC50 of approximately 1pM. In an ex vivo cervical tissue model, PSC-RANTES nanoparticles displayed a fivefold increase in tissue uptake, enhanced tissue permeation, and significant localization at the basal layers of the epithelium over unformulated PSC-RANTES.
Conclusions
These results indicate that PSC-RANTES can readily be encapsulated into a PLGA nanoparticle drug delivery system, retain its anti-HIV-1 activity, and deliver PSC-RANTES to the target tissue. This is crucial for the success of this drug candidate as a topical microbicide product.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Today, sexually transmitted infections (STIs), such as HIV-1, are a significant medical concern throughout the world. The number of HIV-1 infections is increasing every year. According to the World Health Organization, at the end of 2007, there were 33.2 million people infected with HIV-1 with 2.5 million new infections occurring that year. Of the new infections, 1.7 million of them occurred in sub-Saharan Africa, with nearly 66% of these infections occurring in women (1). Current strategies in HIV-1 prevention have been limited to condom use and behavioral modification; however, in high HIV-1 prevalent areas of the world, condom use is low due to social stigmas (2). As such, sexual transmission is one of the primary modes of HIV-1 infection in these parts of the world (3). Given the lack of significant progress in developing a vaccine to immunize people against HIV-1 infection, other strategies for HIV-1 prevention are needed.
Currently, there are no candidate vaccines in the pipeline that can provide immunity to and protect against HIV-1 infection. Therefore, there is an urgent need for alternative forms of HIV-1 protection. One such strategy in preventing sexually transmitted HIV-1 is the development of topical microbicides to prophylactically inhibit transmission of STIs, including HIV-1 (4,5). The topical microbicide product would be applied intravaginally by women to inactivate pathogens deposited into the genital tract during sexual intercourse. Due to the low compliance of condom use by men, the increasing number of women infected with HIV-1, and other social issues, the development of topical microbicides would provide women with a female controlled form of protection (6).
During HIV-1 infection, macrophages, T-cells, and dendritic cells located in the subepithelial layers of the vaginal and cervical mucosa have been identified as potential targets for the virus (7–9). However, despite several studies investigating the transmission of HIV-1, the exact mechanism of how HIV-1 gains entry into the vaginal mucosa to these target cells is not completely understood. It has been suggested that HIV-1 transmission through the multi-cellular layer of stratified squamous epithelial cells occurs through uptake by Langerhans cells that might extend near to, or into the mucosal lumen (10). Additionally, micro-abrasions in the vaginal mucosa could increase the risk of HIV-1 infection by allowing the virus to pass through the epithelial barrier (11). Regardless of the cell type, HIV-1 infection typically requires the binding of the virus to CD4 receptor and either of the chemokine co-receptor molecules CXCR4 or CCR5 to induce fusion between the virus membrane to the cell membrane through conformational changes in the viral envelope glycoproteins (12,13). Since the subepithelial stromal tissue is densely populated with CD4 and CCR5 expressing targets, any breach in the epithelial layer drastically increases the risk of HIV-1 infection by allowing the virus direct access to the target cells (14).
Therefore, using a modulator that reduces CCR5 expression on the cell surface may be a viable method for preventing the sexual transmission of HIV-1 (15). One such modulator is RANTES (Regulated upon Activation, Normal T Expressed and Secreted), a naturally occurring chemokine that specifically binds to T lymphocytes and monocytes. RANTES has been shown in vitro to inhibit R5-tropic HIV-1 by blocking virus binding to CCR5 (16–18). Several analogs of RANTES have been developed to improve the affinity of the drug to the CCR5 co-receptor (19–22). Unlike the natural chemokine, these analogs have the capacity to inhibit the recycling of internalized CCR5 resulting in profound and prolonged co-receptor sequestration (23). PSC-RANTES is an engineered amino terminus-modified analog of the chemokine RANTES. PSC-RANTES has more potent anti-viral activity than earlier analogs, blocks CCR5 expression, and when used as a topical treatment has demonstrated high levels of in vitro HIV-1 protection and in vivo activity against SHIVSF162P3 in the rhesus macaque model (24). However, the dosage necessary in rhesus macaque in vivo studies required orders of magnitude greater PSC-RANTES to inhibit SHIVSF162P3 than the sub-nanomolar IC50 observed in vitro (25). It is hypothesized that the disparity in the results comes from incomplete drug distribution, failure to penetrate the submucosal target tissue, or the degradation or inhibition of the protein in vivo. Additionally, reduced in vivo efficacy may be the result of possible pro-inflammatory side-effects that may occur with repeated and long term exposure to PSC-RANTES (26) and may even lead to detrimental effects upon the vaginal mucosa (27).
To overcome the potential issues involved in peptide drug delivery, the use of nanoparticle encapsulation has been proposed as a solution for many of the obstacles (28). Such protein drug delivery through biodegradable polymeric nanoparticles can be achieved using the co-polymer poly(lactic-co-glycolic acid) (PLGA). PLGA is one of the most widely accepted biodegradable polymers used in encapsulation drug delivery (28). Nanoparticles composed of biodegradable polymers such as PLGA are commonly used due to their ability to be reabsorbed by the body and to show lower toxicity than non-degradable polymers (29,30). Additionally, work with PLGA nanoparticles was shown to reduce immunogenic response, increase blood circulation lifetimes, protect against degradation, enhance tissue penetration, and provide sustained drug release (31–38). The sub-micron size of nanoparticles allows them to penetrate into the tissue through interstitial spaces to be readily taken up by the cells (39). As a drug delivery system, nanoparticle encapsulation is being investigated for therapeutic applications in oral, nasal, transdermal, brain, and cardio-vascular systems (40–46).
In this study, we investigated the ability of PLGA nanoparticles to encapsulate PSC-RANTES and their ability to enhance tissue permeability and drug targeting. The results of this study demonstrate that the topical microbicide agent PSC-RANTES encapsulated in a PLGA nanoparticle drug delivery system may facilitate therapeutic distribution by enhancing mucosal tissue penetration and providing sustained controlled drug release for the prevention of HIV-1 infection.
MATERIALS AND METHODS
Materials
Poly(d,l-lactide-co-glycolide) with molar ratios of 50:50, 65:35, 75:25 and 85:15 were purchased from Sigma (St. Louis, MO). Streptavidin labeled FITC was purchased from MP Biomedicals (Solon, OH). All other reagents used for nanoparticle formulation were purchased from Fisher Scientific (Pittsburgh, PA).
PSC-RANTES
PSC-RANTES was synthesized by the Peptide Synthesis Facility at the University of Pittsburgh (Pittsburgh, PA). Additionally, a biotinylated version of PSC-RANTES was synthesized by the Peptide Synthesis Facility at the University of Pittsburgh. For the biotinylated PSC-RANTES, the biotin modification occurs at the Lys33 position. The molecular weight of the PSC-RANTES was confirmed by mass spectrometry.
Nanoparticle Preparation
Blank control 50:50 PLGA nanoparticles were manufactured at room temperature using a double emulsion-solvent evaporation method as previously described (47). Briefly, water (100 μL) was emulsified in a solution of PLGA (100 mg) in ethyl acetate (1 mL) using a 130W, 3mm probe sonicator for 20s (Vibra-Cell, Sonics and Materials, Newton, CT). The subsequent water-in-oil emulsion was again emulsified in 2 mL of 2% w/v aqueous solution of polyvinyl alcohol (PVA) by sonication for 20s at 130W to form a nanoscopic water-in-oil-in-water emulsion. The resulting nanoparticle solution was diluted with 10 mL of a 0.3% w/v aqueous solution of PVA. The emulsion was magnetically stirred overnight (approximately 12 h) at room temperature to allow the ethyl acetate to evaporate. The hardened nanoparticles in suspension were centrifuged twice for 45 min at 25,000 × g (Sorvall Ultra 80, Waltham, MA). The PVA supernatant was removed and 1 mL of fresh 0.3% PVA solution was added to the nanoparticles. The nanoparticles were lyophilized for 24 h under vacuum at 0.120mbarr and at −50°C (Freezone 6, Labconco, Kansas City, MO). Nanoparticles loaded with protein was prepared similarly to the control nanoparticles except 0.001% to 1% w/w, expressed as initial amount of bulk protein added with respect to the polymer, of europium as a control or PSC-RANTES-biotin was added in the internal aqueous phase. Nanoparticles containing other molar ratios of PLGA (65:35, 75:25, and 85:15) were prepared similarly to the 50:50 PLGA nanoparticles. The dried nanoparticles were stored in aliquots in glass vials at 4°C until use.
Nanoparticle Characterization
Particle Size and Zeta Potential
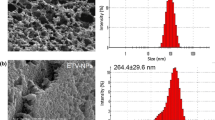
Particle size and size distribution were determined at multiple points (after second sonication, after centrifugation, and after final lyophilization) in the nanoparticle fabrication process by dynamic light scattering (DLS) equipment (Zetasizer Nano series, Malvern, Worcestershire, UK). Images of the formulated nanoparticles were taken by scanning electron microscopy (SEM). The lyophilized nanoparticles were placed on the SEM stage via carbon tape and coated for 110s in a Cressington Sputter Carbon Coater 108 Auto (Watford, UK) under argon vacuum. The images were taken at a magnification of 5,000× to 25,000× using a Philips Excel 30 FEG SEM instrument (Philips, Andover, MA) through the Department of Materials Science and Engineering of the University of Pittsburgh (Pittsburgh, PA). The zeta potential of the PLGA nanoparticles both unloaded and loaded, in pH7.4 buffer, was measured using the zeta potential analysis mode in the Zetasizer Nano series Malvern instrument.
Drug Loading
The amount of europium-streptavidin control (Perkin Elmer, Norton, OH) encapsulated in the nanoparticles was determined by analyzing the europium content in the supernatant from the nanoparticle preparation to quantify encapsulation efficiency. Briefly, the europium content was determined by fluorescent assay as previously described (48). Into the stirring nanoparticle supernatant, 2 mL of Dissociation-Enhanced Lanthanide Fluorescent Immunoassay (DELFIA) (Perkin Elmer) enhancement solution was added and allowed to incubate at room temperature for 15 min. Aliquots of the solution were transferred to a 96-well plate and measured by time-resolved fluorescence on a Beckman Coulter DTX880 Multimode Detector (Fullerton, CA).
The amount of PSC-RANTES-Biotin encapsulated in the nanoparticles was determined by analyzing the PSC-RANTES content in the nanoparticle supernatant by HPLC methods. Briefly, an HPLC system (Waters Corporation, Milford, MA) equipped with an auto injector model 717 (Waters Corporation), a quaternary pump model 600 (Waters Corporation), and an ultraviolet (UV) detector model 2487 (Waters Corporation) at 280 nm was used. Separation of the compound of interest was achieved by using a Phenomenex Jupiter 5 µ 300Å (250 × 4.6 mm) column (Phenomenex, Torrance, CA) protected by a guard cartridge Jupiter C12 (4.0 × 3 mm) (Phenomenex). A gradient consisted of mobile phase A (0.1% trifluoroacetic acid (TFA) in Milli Q water), and mobile Phase B (0.1% TFA in acetonitrile) at a flow rate of 1.0 mL/min was used. Retention time of PSC-RANTES was approximately 17 minutes and the total run time was 40 min. Empower Pro 2 software (Waters Corporation) was used to control the HPLC system. The final amount of drug encapsulated into the nanoparticles was calculated using mass balance by subtracting the amount of drug present in the supernatant from the total bulk drug added.
PSC-RANTES and PSC-RANTES-biotin Comparison
To ensure the validity of PSC-RANTES-biotin as a substitute for PSC-RANTES, various characterizations were performed. Circular dichroism (CD) was used to monitor conformational changes in the secondary structure of the proteins. CD measurements were performed on an AVIV circular dichroism spectrophotometer model 202 (AVIV Biomedical, Lakewood, NJ) equipped with a 0.1 cm path length quartz cell. Spectra were recorded between 198 and 300 nm at 25°C from a 500 μg/mL protein solution in 1 mM phosphate–buffered saline (PBS). Three scans were averaged and subtracted from buffer background over the same wavelength range. HPLC analysis was performed as described above, to compare retention times for control samples of PSC-RANTES and PSC-RANTES-biotin. Finally, using a cell-based HIV-1 infection assay described in “Anti-HIV activity of PSC-RANTES nanoparticles”, the bioactivity of PSC-RANTES and PSC-RANTES-biotin was compared.
In vitro Release from PLGA Nanoparticles
To determine the amount and rate of PSC-RANTES released from the nanoparticles an in vitro release study was conducted over a 30 day period. In this study, the nanoparticles were maintained in 1M PBS adjusted to pH4.6 with 10% hydrochloric acid (HCl). The pH4.6 condition was chosen for the in vitro release studies because of its physiological relevance to the vagina. PSC-RANTES loaded nanoparticles were dispersed in 5 mL of this buffer with continuous mixing at room temperature. At predetermined intervals, the nanoparticles were isolated via centrifugation and the entire buffer solution was decanted for analysis. The nanoparticles were then suspended in fresh PBS (pH = 4.6) and returned to the in vitro release set-up. To determine the effect of pH on drug release, in vitro release studies were also performed in 1M PBS at pH7.4. The amount of PSC-RANTES released into the pH7.4 PBS solution was determined by HPLC methodology as previously detailed. Additionally, the effect that PLGA composition has on the in vitro release of PSC-RANTES in physiological relevant pH4.6 PBS was measured by formulating nanoparticles composed of PLGA at various ratios of lactide to glycolide (50:50, 65:35, 75:25 and 85:15) as described above. The amount of PSC-RANTES released into the PBS solution was determined by HPLC methodology as previously detailed.
Anti-HIV-1 Activity of PSC-RANTES Nanoparticles
The cell toxicity and anti-HIV-1 activity of PSC-RANTES nanoparticles was studied in a cell based assay with a TZM-bl indicator cell line obtained through the NIH AIDS Research and Reference Reagent Program, Division of AIDS, NIAID, NIH (49). TZM-bl is a HeLa cell line derivation that stably expresses high levels of CCR5, CD4, and CXCR4 receptors. The cells enable simple and quantitative analysis of HIV through luciferase or β-galactosidase reporters that activate through HIV expression. The cells were cultured in DMEM medium supplemented with 10% fetal bovine serum (FBS), 100 U/mL penicillin, and 100 μg/mL streptomycin (DMEM+) at 37°C in 5% CO2 atmosphere. The TZM-bl cells were added to a 96-well Packard ViewPlate at a concentration of 5 × 103 cells per well in 100 μL of DMEM+ medium and allowed to adhere for 24 h at 37°C (50,51). Treatments of PSC-RANTES, PSC-RANTES-biotin, and PSC-RANTES nanoparticles were exposed to the cells at dosing levels ranging from 1 mM to 1fM for 4 h. Identical but separate plates were set-up to measure cell toxicity and bioactivity. Cell toxicity was assessed by the addition of 100 μL of Cell Titer-Glo™ (Promega Corp., Madison, WI) to each well. Luminescence was then measured using a Beckman Coulter DTX880 Multimode Detector to determine toxicity. Loss of luminescence indicates a loss of ATP activity which is indicative of toxicity. For the bioactivity evaluation, HIV-1BaL at approximately 3,600 50% tissue culture infectious dose (TCID50) was added to each pre-treated well in the presence of 40 μg/mL of DEAE-Dextran. Viral infection was allowed to proceed for 2 h at 37°C, in 100 μL of DMEM+. An additional 100 μL of DMEM+ was added to bring the total volume in each well to 200 μL. After 48 h, 100 μL of Bright-Glo™ reagent (Promega) was added to each well, and luciferase activity was measured on a Beckman Coulter DTX880 Multimode Detector. In all luminescence measurements, results were reported in relative luminescent units (RLU). All measurements were done in triplicate. Untreated wells with cells only served as luminescent background controls while wells with cells and HIV-1 served as positive controls.
Franz Cell Human Tissue Study
To determine the biocompatibility and localization of the PSC-RANTES-biotin drug loaded nanoparticles in tissue, human cervical tissue was obtained from patients (age 35 to 50 years old) undergoing hysterectomy through the Magee-Womens Hospital Tissue Procurement Center (Pittsburgh, PA) as per approved IRB protocol. Tissue targeting and permeability studies were preformed in a Franz cell system as previously described (52). Briefly, the Franz cells were maintained at 37°C. Sink conditions were maintained throughout the experiment. Fresh human cervical tissue was placed on top of a 7-mm Franz cell opening. A suspension of PSC-RANTES-biotin PLGA nanoparticles (100 mg/mL) in 1M PBS buffer (pH = 4.6) was added to the donor compartment. At regular time intervals from 0 to 4 h, 200 μL samples were taken from the receptor compartment (4.9 mL) and replaced with fresh buffer. HPLC analysis was conducted to quantify PSC-RANTES present in the receptor compartment at that time point. Tissue concentrations of PSC-RANTES were determined by mass balance. Histological evaluation was conducted on all tissue specimens tested. Retained tissue from each test specimen was fixed for histology and processed prior to the experiment in order to compare with post-experimental histology. Tissue was fixed in Clark’s solution (ethanol-acetic acid [75:25]) for 24 h, transferred to ethanol for 24 h, and subsequently embedded in paraffin. Tissue sections of 5 µm were cut and stained with hematoxylin and eosin (H&E). Histology was conducted to determine any gross morphological changes in the tissue during the exposure period when compared to pre-exposed tissue. To image the tissue uptake and targeting of the nanoparticles, the mounted tissue was washed in decreasing amounts of alcohol and then incubated for 1 hour with FITC labeled streptavidin in a darkroom. One drop of Vectashield DAPI (Vector, Burlington, CA) was added to stain the nuclei of the cells in the tissue. The tissue was then imaged on a Zeiss Axioskop 40 inverted phase-contrast microscope (Thornwood, NY) with an EXFO X-cite 120 Fluorescent Illumination System (Quebec, Canada) at 40×.
Statistics
All differences were evaluated by Student’s t test. P < 0.05 was considered statistically significant. All error bars represent standard deviations.
RESULTS
PLGA Nanoparticle Characterization
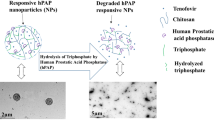
In manufacturing the PLGA nanoparticles via the double emulsion method, it was found that sonication duration and intensity were significant factors in controlling nanoparticle size (47). From the sonication parameters described in the methods section, nanoparticles with diameters ranging from 231.75 ± 14.46 nm (unloaded nanoparticles) to 256.58 ± 19.57 nm (PSC-RANTES nanoparticles), with a polydispersity of 0.074 ± 0.015 and 0.098 ± 0.054, respectively, were fabricated. Zeta potential measurements also resulted in minimal change from unloaded to loaded state, with values of −8.82 ± 0.48 mV and −10.35 ± 1.89 mV, respectively, at a pH of 7.4. SEM imagery of the PLGA nanoparticles confirmed their monodispersity and spherical shape (Fig. 1A). A PSC-RANTES encapsulation efficiency of 82.23 ± 8.35% was obtained from the manufactured PLGA nanoparticles.
Comparisons Between PSC-RANTES and PSC-RANTES-biotin Show Similar Behavior
In comparing PSC-RANTES and PSC-RANTES-biotin to ensure similar structure and behavior, circular dichroism, HPLC analysis, and bioactivity measurements were performed. Measurements via circular dichroism showed no modification of the secondary structures between PSC-RANTES and PSC-RANTES-biotin (Fig. 1B). The retention times observed in HPLC analysis were consistent between each other. Finally, from a 48 h TZM-bl HeLa cell-based assay, the bioactivity against HIV-1 infection remained consistent between PSC-RANTES and PSC-RANTES-biotin both with a calculated 50% inhibitory concentration (IC50) of 1.12 and 1.19pM, respectively.
In vitro Release Studies of the PLGA Nanoparticles Resulting in Controlled Steady Release
The in vitro release of PSC-RANTES from PLGA nanoparticles was measured over 30 days at pH4.6 (Fig. 2). The in vitro release of PSC-RANTES from the nanoparticles followed a biphasic release profile: an initial burst release from time 0–5 days, followed by a slow steady release over the remaining 25 days. After 5 days, 60.20 ± 2.85% of the PSC-RANTES was released from the nanoparticles. Over the next 25 days, an additional 11.28 ± 2.41% was released. The total amount of drug released over the 30 day period was 71.48 ± 5.25%.
The effect that pH has on the in vitro release of the PLGA nanoparticles was measured at pH4.6 and 7.4 for a period of 10 days (Fig. 3). In vitro release profiles obtained for nanoparticles suspended in pH7.4 buffer solution displayed a slower burst release by day5 during which only 35.80 ± 7.80% of the protein was released whereas in a pH4.6 buffer solution, 60.20 ± 2.85% of the protein was released.
Additionally, the effect that co-polymer composition of the PLGA nanoparticles has upon in vitro release was studied. The ratio of lactide to glycolide was changed to increase or decrease the hydrophobicity of the nanoparticles. Using lactide to glycolide ratios of 50:50, 65:35, 72:25, and 85:15 the in vitro release of protein from the nanoparticles was measured at pH 4.6 was measured for 10 days (Fig. 4). The increase of lactic acid in the nanoparticle structure decreased the degradation rate of the nanoparticle, thus resulted in reduced burst release and an overall decrease in total amount released.
PSC-RANTES PLGA Nanoparticle Toxicity and anti-HIV-1 Activity
The toxicity of nanoparticle formulated PSC-RANTES was compared to unformulated PSC-RANTES using the TZM-bl cell line following a 24 h exposure (Fig. 5). PLGA nanoparticles and unformulated PSC-RANTES at concentrations ranging from 1 mM to 10 pM resulted in no significant reduction (<3 standard deviation loss: 100% ± 12%) of viability of the TZM-bl cells as compared to untreated TZM-bl cells.
Toxicity of PSC-RANTES treatment to TZM-bl cells with a 24 h exposure. In 96-well plates TZM-bl were exposed to decreasing amounts of unformulated PSC-RANTES (black) and PSC-RANTES nanoparticles (white) for 24 h at 37°C. Luminescence was measured after the addition of Cell Titer-Glo in percent viability based on positive controls. A non-toxic response was determined if the % viability of the unformulated PSC-RANTES or PSC-RANTES nanoparticles did not fall below 3 standard deviations of the control. N = 3 independent experiments. *p < 0.05 by Student’s t test.
The ability of PSC-RANTES nanoparticles compared to unformulated PSC-RANTES to protect against HIV-1BaL infection was evaluated using the TZM-bl cell line (Fig. 6). A range of PSC-RANTES concentrations (1 mM to 1 pM) was studied. Anti-HIV-1 protection was measured in % relative luminescence units (RLU) compared to unprotected TZM-bl cells exposed to HIV-1BaL. The encapsulation of PSC-RANTES in PLGA nanoparticles slightly shifted the IC50 from 1.12pM for the unformulated PSC-RANTES to 426fM for the PSC-RANTES nanoparticles. The PLGA nanoparticle themselves did not offer any protection against HIV-1 infection as treatments of unloaded nanoparticles did not prevent luciferase activity by the TZM-bl cells (Fig. 6).
Luciferase luminescent readings of PSC-RANTES treated TZM-bl cells exposed to HIV-1. TZM-bl cells were treated with control empty nanoparticles (closed triangles), unformulated PSC-RANTES (filled diamond) or PSC-RANTES encapsulated nanoparticles (open squares) at a dosing range of 1 mM to 1 fM for 4 h at 37°C. Presented are data from 1 nM to 1 fM. After treatment, HIV-1BaL was added with DEAE-dextran and allowed to culture for 48 additional hours. Results are reported on a log scale of PSC-RANTES dosing levels in percent of relative luminescent units (RLU) as compared to untreated TZM-bl cells infected with HIV-1. (*p < 0.05 by Student’s t test comparing unformulated PSC-RANTES to PSC-RANTES nanoparticles).
PLGA Nanoparticle Permeability and Targeting into Human Ectocervical Tissue
The distribution and permeability of PSC-RANTES nanoparticles and unformulated PSC-RANTES into tissue was performed using a Franz cell apparatus. From mass balance, the amount of PSC-RANTES within the tissue was calculated by subtracting the total amount released in the receptor compartment from the initial donor compartment concentration. To ensure that PSC-RANTES did not bind to the walls of the donor cell compartment, control studies were preformed which showed that an insignificant amount of PSC-RANTES non-specifically adsorbed to the donor compartment walls (0.31 ± 0.01%). When ectocervical tissue was exposed to PSC-RANTES, the PLGA nanoparticles displayed a 5-fold increase in tissue uptake over unformulated PSC-RANTES.
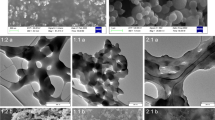
From H&E staining and imaging of the epithelial layer of the tissue, no gross morphological changes were identified over the time course of the study (Fig. 7A, B). Using a dual staining and labeling method for FITC and DAPI, release and localization of PSC-RANTES-biotin was evaluated. Unformulated PSC-RANTES remained at the superficial epithelial layer (Fig. 7C, D). Conversely, the majority of the PSC-RANTES nanoparticles permeated through the superficial epithelium and accumulated at the basal epithelium (Fig. 7E, F).
Representative H&E microscopy images of ecto-cervical tissue pre-nanoparticle exposure (A) and post nanoparticle exposure (B). Representative fluorescent microscopy images of ecto-cervical tissue with FITC (green) or DAPI (blue) staining at 40× magnification. Ecto-cervical tissue treated with unformulated PSC-RANTES for 4 hours with stained with DAPI (C) or FITC (D). Ecto-cervical tissue treated with PSC-RANTES encapsulated nanoparticles for 4 h stained with DAPI (E) or FITC (F).
DISCUSSION
PSC-RANTES, a CCR5 chemokine receptor inhibitor, has demonstrated high efficacy against the HIV-1 virus. However, in vivo activity was significantly reduced from that observed in vitro requiring orders of magnitude greater PSC-RANTES to inhibit viral infection. This study shows that by nanoparticle encapsulation, PSC-RANTES can obtain enhanced tissue distribution, penetration, and targeting. While nanoparticle encapsulation as a drug delivery system is being investigated in numerous therapeutic fields, currently, there is little work done within the microbicide field. Therefore, to track the microbicide drug candidate PSC-RANTES within tissue, a modified PSC-RANTES protein was used: PSC-RANTES-biotin. The addition of the biotin tag did not affect any of the characteristic properties of PSC-RANTES. From characteristic CD and HPLC measurements comparing the two proteins, PSC-RANTES and PSC-RANTES-biotin resulted in similar overall secondary structure and partitioning behavior. And the bioactivity of both PSC-RANTES and PSC-RANTES-biotin in an anti-HIV-1 cell-based assay resulted in an IC50 of 1.12 and 1.19 pM, respectively, against HIV-1BaL, which are equivalent to the published “sub-nanomolar” IC50 against SHIVSF162 (25) and 8 pM against HIV-1C-92BR025 (53).
In this paper, PLGA nanoparticles were used to encapsulate an anti-HIV-1 microbicide candidate PSC-RANTES. Successful encapsulation of PSC-RANTES nanoparticles resulted in monodispersed, spherical particles that maintain anti-HIV-1 bioactivity. The constant negative zeta potential of the nanoparticles from unloaded state to loaded state suggests that the hydrophilic microbicide is being encapsulated rather than adsorbed onto the surface of the nanoparticles. In these studies, the double emulsion fabrication of PSC-RANTES nanoparticles yielded an encapsulation efficiency greater than 80%. Additionally, SEM imagery displayed smooth spherical surfaces further supporting that little surface adsorption has occurred.
Controlled release of loaded protein is one of the defining characteristics of PLGA nanoparticles. The in vitro drug release profile from the nanoparticles was characterized by two stages: the initial burst release and a sustained release of drug over extended time. In vitro release studies for PSC-RANTES nanoparticles showed that a significant amount of drug (71.48 ± 5.25%) was released over a 30 day period. Similar results were observed in the control europium-streptavidin which suggests that nanoparticle release may be independent of the encapsulated molecule properties and due solely to the polymer degradation of the PLGA nanoparticle. The polymer degradation is expected to undergo bulk hydrolic degradation where hydration relaxes the polymer chains until the matrix becomes more porous and falls apart.
The in vitro release of the protein from the nanoparticle can be affected by both the environmental conditions and the composition of the PLGA shell. Under normal conditions, the vaginal environment has an acidic pH (approximately 4.6) (54). As such, in vitro release studies conducted at pH 4.6 resulted in significant release (>70%) of PSC-RANTES. However, when pH was increased to pH 7.4, the resulting release was reduced. These studies showed that specific changes in the pH environment can affect the release profile of PSC-RANTES from the PLGA nanoparticles. These data imply that when the pH of the vagina increases, as it does with the introduction of semen or in pathogenic situation, the release of PSC-RANTES into vagina may be altered. Further studies are needed to characterize the impact of this phenomenon in an in vivo system.
Additionally, the release of PSC-RANTES from nanoparticles can be controlled through the modification of the PLGA composition. The degradation of PLGA films and micro/nano-spheres has been shown to be strongly dependent upon the ratio of lactide to glycolide (55,56). As the hydrophobicity of the PLGA increases, the slower the drug release becomes. With a range of lactide to glycolide ratios tested in this study, we observed that as the hydrophobicity of the nanoparticles was increased, the rate and cumulative release of protein was reduced. The hydrophobicity of the PLGA nanoparticles affects the uptake of water and subsequently the release rate of drug. Therefore, the more hydrophilic 50:50 PLGA nanoparticles displayed a faster burst release over the more hydrophobic 85:15 PLGA nanoparticles. Such behavioral profiles in PLGA nanoparticles allow a degree of predictability in controlling the microbicide drug candidate release.
To prevent HIV-1 infection, PSC-RANTES needs to bind to the target cell surface to inhibit CCR5 expression. Therefore, nanoparticles need to effectively transport and release PSC-RANTES into the surrounding target tissue to bind to the cell surface. In a HeLa cell line based system (TZM-bl), the presence of PSC-RANTES and PLGA nanoparticles displayed no toxicity over a 24 hours period. Furthermore, in excised human ectocervical tissue, no gross morphological changes in the tissue were observed when exposed to both unloaded and drug loaded PLGA nanoparticles. These results suggest that the PSC-RANTES PLGA nanoparticles are biocompatible with vaginal tissue, non-toxic, and thus are a safe vector for drug delivery into the female reproductive tract. Furthermore, encapsulation did not result in any reduction of PSC-RANTES bioactivity. The ability of PSC-RANTES nanoparticles to protect TZM-bl cells against HIV-1BaL infection after 48 h parallels that seen in unformulated PSC-RANTES. The unformulated PSC-RANTES and PSC-RANTES nanoparticles displayed IC50 values of 1.12 pM and 426 fM, respectively. The two fold change in IC50 is statistically and biologically significant in this cell-based assay. However, the change in bioactivity is less than a log. Therefore it is unknown whether or not this difference will have any effect in vivo. Additionally, empty PLGA nanoparticle provided no protection against HIV-1 infection, demonstrating that there was no baseline steric inhibition which results from the PLGA nanoparticles themselves.
The encapsulation of PSC-RANTES into nanoparticles has been shown to enhance the uptake of PSC-RANTES into tissue and to mediate transfer to the target cells. The intracellular uptake and targeting of the nanoparticles has been shown to be directly related to the physical characteristics of the nanoparticles themselves. The size of the particle can affect tissue uptake and interstitial trafficking (57). The zeta potential of the nanoparticle is an important factor, with negatively charged nanoparticles displaying greater tissue permeability preventing rapid uptake by cellular membranes (35). As such, the PLGA nanoparticles formulated in this study with the particular physical characteristics, hydrophilicity, and zeta potential afford it increased tissue uptake and permeation into excised human ectocervical tissue over unformulated PSC-RANTES. The 5-fold increase in tissue uptake and permeation through the stratified squamous epithelium to passively target the basal layer demonstrated the advantage of nanoparticle encapsulation over unformulated PSC-RANTES, which was only capable of permeating the outer most superficial layers of the epithelium. HIV has been shown to transmigrate throughout the epithelium (9), therefore these data are important in illustrating the ability of PSC-RANTES nanoparticles to localize in areas where the virus may be.
Additional research is required to further develop nanoparticles as a drug delivery method for PSC-RANTES. Further investigation into the exact transport mechanisms and degradation process in the targeted tissue is required. Additionally, encapsulation of PSC-RANTES may provide this microbicide drug candidate protection against overall degradation in the vaginal environment. Therefore a thorough evaluation of the effect of nanoparticle encapsulation on PSC-RANTES stability must be conducted. Finally, to address potential pro-inflammatory responses from PSC-RANTES, alternatives to PSC-RANTES, such as recombinant variants (58,59), coupled with nanoparticle encapsulation may be developed to further optimize RANTES as a microbicide product.
CONCLUSION
In this study, PSC-RANTES was formulated into a non-toxic nanoparticle drug delivery system that displays increased tissue uptake, permeation, drug targeting to the site of action, and anti-HIV-1 activity over extended periods of time. The formulation of biodegradable nanoparticles to encapsulate PSC-RANTES additionally provides a release rate from the nanoparticles that is both predictable and controllable. The ability of nanoparticles to successfully deliver PSC-RANTES to the target tissue is important for the development of chemokine inhibitors as a microbicide product.
References
UNAIDS. AIDS Epidemic Update. (2007).
R. Pool, G. Hart, G. Green, S. Harrison, S. Nyanzi, and J. Whitworth. Men’s attitudes to condoms and female controlled means of protection against HIV and STDs in south-western Uganda. Cult. Health Sex. 2:197–211 (2000). doi:10.1080/136910500300804.
M. M. Lederman, R. E. Offord, and O. Hartley. Microbicides and other topical strategies to prevent vaginal transmission of HIV. Nat. Rev. Immunol. 6:371 (2006). doi:10.1038/nri1848.
J. Turpin. Considerations and development of topical microbicides to inhibit the sexual transmission of HIV. Expert. Opin. Investig. Drugs. 11:1007–1097 (2002). doi:10.1517/13543784.11.8.1077.
P. Harrison, Z. Rosenberg, and J. Bowcut. Topical microbicides for disease prevention: status and challenges. Clin. Infect. Dis. 36:1290–1294 (2003). doi:10.1086/374834.
T. R. Moench, T. Chipato, and N. S. Padian. Preventing disease by protecting the cervix: the unexplored promise of internal vaginal barrier devices. AIDS. 15:1595–1602 (2001). doi:10.1097/00002030-200109070-00001.
T. Kawamura, S. S. Cohen, D. L. Borris, E. A. Aquilino, S. Glushakova, L. B. Margolis, J. M. Orenstein, R. E. Offord, A. R. Neurath, and A. Blauvelt. Candidate microbicides block HIV-1 infection of human immature langerhans cells within epithelial tissue explants. J. Exp. Med. 192:1491–1500 (2000). doi:10.1084/jem.192.10.1491.
T. Kawamura, S. E. Kurtz, A. Blauvelt, and S. Shimada. The role of Langerhans cells in the sexual transmission of HIV. J. Dermatol. Sci. 40:147 (2005). doi:10.1016/j.jdermsci.2005.08.009.
K. M. Fahrbach, S. M. Barry, S. Ayehunie, S. Lamore, M. Klausner, and T. J. Hope. Activated CD34-Derived langerhans cells mediate transinfection with human immunodeficiency virus. J. Virol. 81:6858–6868 (2007). doi:10.1128/JVI.02472-06.
F. Hladik, P. Sakchalathorn, L. Ballweber, G. Lentz, M. Fialkow, D. Eschenbach, and M. J. McElrath. Initial events in establishing vaginal entry and infection by human immunodeficiency virus type-1. Immunity. 26:257–270 (2007). doi:10.1016/j.immuni.2007.01.007.
M. K. Norvell, G. I. Benrubi, and R. J. Thompson. Investigation of microtrauma after sexual intercourse. J. Reprod. Med. 29:269–271 (1984).
J. P. Moore, and M. Stevenson. New targets for inhibitors of HIV-1 replication. Nat. Rev. Mol. Cell Biol. 1:40 (2000). doi:10.1038/35036060.
H. Deng, R. Liu, W. Ellmeier, S. Choe, D. Unutmaz, M. Burkhart, P. D. Marzio, S. Marmon, R. E. Sutton, C. M. Hill, C. B. Davis, S. C. Peiper, T. J. Schall, D. R. Littman, and N. R. Landau. Identification of a major co-receptor for primary isolates of HIV-1. Nature. 381:661 (1996). doi:10.1038/381661a0.
C. J. Miller, and R. J. Shattock. Target cells in vaginal HIV transmission. Microbes Infect. 5:59 (2003). doi:10.1016/S1286-4579(02)00056-4.
T. N. C. Wells, A. E. I. Proudfoot, and C. A. Power. Chemokine receptors and their role in leukocyte activation. Immunol. Lett. 65:35 (1999). doi:10.1016/S0165-2478(98)00121-7.
G. Alkhatib, C. Combadiere, C. C. Broder, Y. Feng, P. E. Kennedy, P. M. Murphy, and E. A. Berger. CC CKR5: A RANTES, MIP-1alpha, MIP-1beta receptor as a fusion cofactor for macrophage-Tropic HIV-1. Science. 272:1955–1958 (1996). doi:10.1126/science.272.5270.1955.
M. Mack, B. Luckow, P. J. Nelson, J. Cihak, G. Simmons, P. R. Clapham, N. Signoret, M. Marsh, M. Stangassinger, F. Borlat, T. N. C. Wells, D. Schlondorff, and A. E. I. Proudfoot. Aminooxypentane-RANTES induces CCR5 internalization but inhibits recycling: a novel inhibitory mechanism of HIV infectivity. J. Exp. Med. 187:1215–1224 (1998). doi:10.1084/jem.187.8.1215.
F. Cocchi, A. L. DeVico, A. Garzino-Demo, S. K. Arya, R. C. Gallo, and P. Lusso. Identification of RANTES, MIP-1 alpha, and MIP-1 beta as the major HIV-suppressive factors produced by CD8+ T cells. Science. 270:1811–1815 (1995). doi:10.1126/science.270.5243.1811.
V. S. Torre, A. J. Marozsan, J. L. Albright, K. R. Collins, O. Hartley, R. E. Offord, M. E. Quinones-Mateu, and E. J. Arts. Variable sensitivity of CCR5-Tropic human immunodeficiency virus type 1 isolates to inhibition by RANTES analogs. J. Virol. 74:4868–4876 (2000). doi:10.1128/JVI.74.10.4868-4876.2000.
D. E. Mosier, G. R. Picchio, R. J. Gulizia, R. Sabbe, P. Poignard, L. Picard, R. E. Offord, D. A. Thompson, and J. Wilken. Highly potent RANTES analogues either prevent CCR5-Using human immunodeficiency virus type 1 infection in vivo or rapidly select for CXCR4-Using variants. J. Virol. 73:3544–3550 (1999).
G. Simmons, P. R. Clapham, L. Picard, R. E. Offord, M. M. Rosenkilde, T. W. Schwartz, R. Buser, T. N. Wells, and A. E. Proudfoot. Potent inhibition of HIV-1 infectivity in macrophages and lymphocytes by a novel CCR5 antagonist. Science. 276:276–279 (1997). doi:10.1126/science.276.5310.276.
A. E. I. Proudfoot, R. Buser, F. Borlat, S. Alouani, D. Soler, R. E. Offord, J.-M. Schroder, C. A. Power, and T. N. C. Wells. Amino-terminally modified RANTES analogues demonstrate differential effects on RANTES receptors. J. Biol. Chem. 274:32478–32485 (1999). doi:10.1074/jbc.274.45.32478.
A. Mueller, E. Kelly, and P. G. Strange. Pathways for internalization and recycling of the chemokine receptor CCR5. Blood. 99:785–791 (2002). doi:10.1182/blood.V99.3.785.
O. Hartley, H. Gaertner, J. Wilken, D. Thompson, R. Fish, A. Ramos, C. Pastore, B. Dufour, F. Cerini, A. Melotti, N. Heveker, L. Picard, M. Alizon, D. Mosier, S. Kent, and R. Offord. Medicinal chemistry applied to a synthetic protein: Development of highly potent HIV entry inhibitors. Proc. Natl. Acad. Sci. U.S.A. 101:16460–16465 (2004). doi:10.1073/pnas.0404802101.
M. Lederman, R. Veazey, R. Offord, D. Mosier, J. Dufour, M. Mefford, M. Piatak Jr., J. Lifson, J. Salkowitz, B. Rodriguez, A. Blauvelt, and O. Hartley. Prevention of vaginal SHIV transmission in rhesus macaques through inhibition of CCR5. Science. 306:485–487 (2004). doi:10.1126/science.1099288.
P. Kuna, R. Alam, U. Ruta, and P. Gorski. RANTES induces nasal mucosal inflammation rich in eosinophils, basophils, and lymphocytes in vivo. Am. J. Respir. Crit. Care Med. 157:873–879 (1998).
R. Cone, T. Hoen, X. Wong, R. Abusuwwa, D. Anderson, and T. Moench. Vaginal microbicides: detecting toxicities in vivo that paradoxically increase pathogen transmission. BMC Infect. Dis. 6:90 (2006). doi:10.1186/1471-2334-6-90.
I. Bala, H. S, and K. MN. PLGA nanoparticles in drug delivery: the state of the art. Crit. Rev. Ther. Drug Carr. Syst. 21:387–422 (2004). doi:10.1615/CritRevTherDrugCarrierSyst.v21.i5.20.
S.-S. Feng. Nanoparticles of biodegradable polymers for new-concept chemotherapy. Expert Rev. Med. Devices. 1:115–125 (2004). doi:10.1586/17434440.1.1.115.
X. Gao, W. Tao, W. Lu, Q. Zhang, Y. Zhang, X. Jiang, and S. Fu. Lectin-conjugated PEG-PLA nanoparticles: Preparation and brain delivery after intranasal administration. Biomaterials. 27:3482 (2006). doi:10.1016/j.biomaterials.2006.01.038.
I. J. Castellanos, G. Flores, and K. Griebenow. Effect of the molecular weight of poly(ethylene glycol) used as emulsifier on alpha-chymotrypsin stability upon encapsulation in PLGA microspheres. J. Pharm. Pharmacol. 57:1261 (2005). doi:10.1211/jpp.57.10.0004.
J. M. Anderson, and M. S. Shive. Biodegradation and biocompatibility of PLA and PLGA microspheres. Adv. Drug Deliv. Rev. 28:5 (1997). doi:10.1016/S0169-409X(97)00048-3.
A. Lamprecht, N. Ubrich, M. Hombreiro Perez, C. M. Lehr, M. Hoffman, and P. Maincent. Biodegradable monodispersed nanoparticles prepared by pressure homogenization-emulsification. Int. J. Pharm. 184:97 (1999). doi:10.1016/S0378-5173(99)00107-6.
J. E. Oh, Y. S. Nam, K. H. Lee, and T. G. Park. Conjugation of drug to poly(D,L-lactic-co-glycolic acid) for controlled release from biodegradable microspheres. J. Control. Release. 57:269–280 (1999). doi:10.1016/S0168-3659(98)00123-0.
J. Panyam, S. K. Sahoo, S. Prabha, T. Bargar, and V. Labhasetwar. Fluorescence and electron microscopy probes for cellular and tissue uptake of poly(-lactide-co-glycolide) nanoparticles. Int. J. Pharm. 262:1 (2003). doi:10.1016/S0378-5173(03)00295-3.
T. G. Park. Degradation of poly(lactic-co-glycolic acid) microspheres: effect of copolymer composition. Biomaterials. 16:1123 (1995). doi:10.1016/0142-9612(95)93575-X.
M. Penco, S. Marcioni, P. Ferruti, S. D’Antone, and R. Deghenghi. Degradation behaviour of block copolymers containing poly(lactic-glycolic acid) and poly(ethylene glycol) segments. Biomaterials. 17:1583 (1996). doi:10.1016/0142-9612(95)00323-1.
D. K. Pettit, J. R. Lawter, W. J. Huang, S. C. Pankey, N. S. Nightlinger, D. H. Lynch, J. A. C. L. Schuh, P. J. Morrissey, and W. R. Gombotz. Characterization of Poly(glycolide-co-D,L-lactide)/Poly(D,L-lactide) microspheres for controlled release of GM-CSF. Pharm. Res. 14:1422–1430 (1997). doi:10.1023/A:1012176823155.
S. V. Vinogradov, T. K. Bronich, and A. V. Kabanov. Nanosized cationic hydrogels for drug delivery: preparation, properties and interactions with cells. Adv. Drug Deliv. Rev. 54:135 (2002). doi:10.1016/S0169-409X(01)00245-9.
T. Peng, S.-X. Cheng, and R.-X. Zhuo. Synthesis and characterization of poly-alpha, beta-[N-(2-hydroxyethyl)-L-aspartamide]-g-poly(L-lactide) biodegradable copolymers as drug carriers. J. Biomed. Mater. Res. Part A. 76A:163–173 (2006). doi:10.1002/jbm.a.30550.
C. Coester, P. Nayyar, and J. Samuel. In vitro uptake of gelatin nanoparticles by murine dendritic cells and their intracellular localisation. Eur. J. Pharm. Biopharm. 62:306 (2006). doi:10.1016/j.ejpb.2005.09.009.
L. A. Dailey, N. Jekel, L. Fink, T. Gessler, T. Schmehl, M. Wittmar, T. Kissel, and W. Seeger. Investigation of the proinflammatory potential of biodegradable nanoparticle drug delivery systems in the lung. Toxicol Appl. Pharmacol. 215:100 (2006). doi:10.1016/j.taap.2006.01.016.
N. Dinauer, S. Balthasar, C. Weber, J. Kreuter, K. Langer, and H. von Briesen. Selective targeting of antibody-conjugated nanoparticles to leukemic cells and primary T-lymphocytes. Biomaterials. 26:5898 (2005). doi:10.1016/j.biomaterials.2005.02.038.
M. J. Heffernan, and N. Murthy. Polyketal nanoparticles: A new pH-Sensitive biodegradable drug delivery vehicle. Bioconjugate Chem. 16:1340–1342 (2005). doi:10.1021/bc050176w.
C. Roney, P. Kulkarni, V. Arora, P. Antich, F. Bonte, A. Wu, N. N. Mallikarjuana, S. Manohar, H.-F. Liang, A. R. Kulkarni, H.-W. Sung, M. Sairam, and T. M. Aminabhavi. Targeted nanoparticles for drug delivery through the blood-brain barrier for Alzheimer’s disease. J. Control. Release. 108:193 (2005). doi:10.1016/j.jconrel.2005.07.024.
U. Westedt, M. Kalinowski, M. Wittmar, T. Merdan, F. Unger, J. Fuchs, S. Schaller, U. Bakowsky, and T. Kissel. Poly(vinyl alcohol)-graft-poly(lactide-co-glycolide) nanoparticles for local delivery of paclitaxel for restenosis treatment. J. Control. Release. 119:41 (2007). doi:10.1016/j.jconrel.2007.01.009.
U. Bilati, E. Allemann, and E. Doelker. Sonication parameters for the preparation of biodegradable nanocapsules of controlled size by the double emulsion method. Pharm. Dev. Technol. 8:1–9 (2003). doi:10.1081/PDT-120017517.
M. Suonpaa, E. Markela, T. Stahlberg, and I. Hemmila. Europium-labelled streptavidin as a highly sensitive universal label: Indirect time-resolved immunofluorometry of FSH and TSH. J. Immunol. Methods. 149:247–253 (1992). doi:10.1016/0022-1759(92)90256-S.
X. Wei, J. M. Decker, H. Liu, Z. Zhang, R. B. Arani, J. M. Kilby, M. S. Saag, X. Wu, G. M. Shaw, and J. C. Kappes. Emergence of resistant human immunodeficiency virus type 1 in patients receiving fusion inhibitor (T-20) monotherapy. Antimicrob. Agents Chemother. 46:1896–1905 (2002). doi:10.1128/AAC.46.6.1896-1905.2002.
J. E. Cummins, Jr., J. M. Villanueva, T. Evans-Strickfaden, S. M. Sesay, S. R. Abner, T. J. Bush, T. A. Green, J. L. Lennox, T. Wright, T. M. Folks, C. E. Hart, and C. S. Dezzutti. Detection of infectious human immunodeficiency virus type 1 in female genital secretions by a short-term culture method. J. Clin. Microbiol. 41:4081–4088 (2003). doi:10.1128/JCM.41.9.4081-4088.2003.
C. M. Finnegan, S. S. Rawat, A. Puri, J. M. Wang, F. W. Ruscetti, and R. Blumenthal. Ceramide, a target for antiretroviral therapy. Proc. Natl. Acad. Sci. U.S.A. 101:15452–15457 (2004). doi:10.1073/pnas.0402874101.
A. B. Sassi, K. D. McCullough, M. R. Cost, S. L. Hillier, and L. C. Rohan. Permeability of tritiated water through human cervical and vaginal tissue. J. Pharm. Sci. 93:2009–2016 (2004). doi:10.1002/jps.20107.
T. Kawamura, S. E. Bruce, A. Abraha, M. Sugaya, O. Hartley, R. E. Offord, E. J. Arts, P. A. Zimmerman, and A. Blauvelt. PSC-RANTES Blocks R5 human immunodeficiency virus infection of langerhans cells isolated from individuals with a variety of CCR5 diplotypes. J. Virol. 78:7602–7609 (2004). doi:10.1128/JVI.78.14.7602-7609.2004.
D. H. Owen, and D. F. Katz. A vaginal fluid simulant. Contraception. 59:91 (1999). doi:10.1016/S0010-7824(99)00010-4.
R. Bodmeier, K. H. Oh, and H. Chen. The effect of the addition of low molecular weight poly(DL-lactide) on drug release from biodegradable poly(DL-lactide) drug delivery systems. Int. J. Pharm. 51:1–8 (1989). doi:10.1016/0378-5173(89)90068-9.
L. Mu, and S. S. Feng. A novel controlled release formulation for the anticancer drug paclitaxel (Taxol(R)): PLGA nanoparticles containing vitamin E TPGS. J. Control. Release. 86:33 (2003). doi:10.1016/S0168-3659(02)00320-6.
M. P. Desai, V. Labhasetwar, G. L. Amidon, and R. J. Levy. Gastrointestinal uptake of biodegradable microparticles: Effect of particle size. Pharm. Res. 13:1838 (1996). doi:10.1023/A:1016085108889.
H. Gaertner, R. Offord, P. Botti, G. Kuenzi, and O. Hartley. Semisynthetic analogues of PSC-RANTES, a potent anti-HIV protein. Bioconjugate Chem. 19:480–489 (2008). doi:10.1021/bc7003044.
L. Vangelista, M. Secchi, and P. Lusso. Rational design of novel HIV-1 entry inhibitors by RANTES engineering. Vaccine. 26:3008 (2008). doi:10.1016/j.vaccine.2007.12.023.
Acknowledgments
The work presented was supported through grants from the National Institute of Allergy and Infectious Diseases (NIAID) at the National Institute of Health (AI-51649, Principle Investigator: Michael Lederman, Case Western Reserve University), the Pendleton Charitable Trust Fund, and the Irene McLenahan Young Investigator Research Fellowship. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIAID. We would like to thank the Department of Material Sciences and Engineering of the University of Pittsburgh for the provision of access to the electron microscopy instrumentation and for assistance with the execution of this part of the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ham, A.S., Cost, M.R., Sassi, A.B. et al. Targeted Delivery of PSC-RANTES for HIV-1 Prevention using Biodegradable Nanoparticles. Pharm Res 26, 502–511 (2009). https://doi.org/10.1007/s11095-008-9765-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-008-9765-2