Abstract
Purpose
To develop a statistical model for predicting effect of food on the extent of absorption (area under the curve of time–plasma concentration profile, AUC) of drugs based on physicochemical properties.
Materials and Methods
Logistic regression was applied to establish the relationship between the effect of food (positive, negative or no effect) on AUC of 92 entries and physicochemical parameters, including clinical doses used in the food effect study, solubility (pH 7), dose number (dose/solubility at pH 7), calculated Log D (pH 7), polar surface area, total surface area, percent polar surface area, number of hydrogen bond donor, number of hydrogen bond acceptors, and maximum absorbable dose (MAD).
Results
For compounds with MAD ≥ clinical dose, the food effect can be predicted from the dose number category and Log D category, while for compounds with MAD < clinical dose, the food effect can be predicted from the dose number category alone. With cross validation, 74 out of 92 entries (80%) were predicted into the correct category. The correct predictions were 97, 79 and 68% for compounds with positive, negative and no food effect, respectively.
Conclusions
A logistic regression model based on dose, solubility, and permeability of compounds is developed to predict the food effect on AUC. Statistically, solubilization effect of food primarily accounted for the positive food effect on absorption while interference of food with absorption caused negative effect on absorption of compounds that are highly hydrophilic and probably with narrow window of absorption.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Food exerts complicated effect on pharmacokinetic and/or pharmacodynamic profiles of a drug. In this study, the key physicochemical parameters that contribute to the food effect were identified by statistical analysis of the effect of food on the extent of drug absorption. A prediction model was also established using logistic regression.
The effect of food on oral absorption may be attributed to specific mechanism for an individual compound. For example, food may interfere with specific transporters that are involved in absorption of a specific compound (1). Food may increase the splanchnic blood flow rate and increase the bioavailability of compounds that undergo extensive first pass effect (2). Certain compounds, e.g., tetracycline and digoxin, can also chelate to specific components of food leading to reduced bioavailability (3,4). These specific food effects may be difficult to predict based on physicochemical descriptors of compounds.
However, food also exerts general physiological changes and its effect on drug absorption may be statistically predicted for compounds with similar physicochemical properties. With food intake, the gastric pH increases initially to about pH 6, followed by decrease in pH value to 2 in approximately 1 h because of increased acid secretion (5,6). The bile secretion also increases with food intake, which may enhance the solubility of lipophilic compounds (6). It was suggested that the permeability may be reduced in general for poorly permeable compound because food impedes the diffusion of the compound to the mucosal surface (7). Larger volume after food intake, which leads to lower concentration of dissolved compound, also reduces the amount absorbed in a definite period of time. Additionally, general binding between drug and food components and incorporation of drug in the micelles of food may also impede the access of the drug to the epithelium surface and hence absorption. It was also well known that food causes delayed gastric emptying leading to delayed tmax and lower Cmax (8,9), although these parameters were not analyzed in this study.
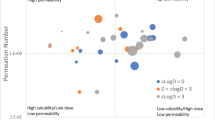
Fleisher et al. summarized the general trend of food effect on drug absorption based on BCS classification (7). BCS class I compounds are likely to have no food effect; BCS class II compounds are likely to have positive effect (increased absorption); BCS class III compounds are likely to have negative effect (decreased absorption) and there is no clear trend for BCS class IV compounds (7). For the 92 entries used in this study, the relationship between BCS classification and the effect of food on the extent of absorption (area under the curve of the time–plasma concentration curve, AUC) was summarized (Table I). If using the criteria that BCS class 1 shows no food effect, BCS classes 2 and 4 show positive food effect and BCS class 3 shows negative food effect as suggested by Fleisher et. al, 67% of entries were predicted into the right category. This result suggests that it is possible to build a statistical model to predict the effect of food on extent of drug absorption based on physicochemical properties. In the current study, more descriptors are used to statistically predict the food effect to improve accuracy for prediction.
MATERIALS AND METHODS
Clinical data of food effect of 90 marketed compounds (92 total entries including hydrochlrothiazide at two different doses with different food effect and free base and mesylate salt of saquinavir) were collected from the literature and Physician Desk Reference (10) (Tables II and III). Hydrochlrothiazide at lower dose is listed in Table II as the dose is less than the maximum absorbable dose (MAD) while the higher dose entry is listed in Table III with the dose > MAD. The food effect on the extent of absorption was separated into three categories: positive food effect (statistically significant increase in AUC with food, 31 entries), negative food effect (statistically significant decrease in AUC with food, 24 entries) and no food effect (no statistically significant difference in AUC, 37 entries).
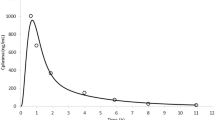
The following physicochemical parameters were collected for these compounds: clinical dose used in the published food effect study, solubility at pH 7, calculated log D at pH 7 using ACD software (11), total surface area (calculated using ACD software), polar surface area (calculated using ACD software), number of hydrogen bond donor (calculated using ACD software), number of hydrogen bond acceptor (calculated using ACD software). The solubility values were collected from the literature (10,12–15). For compounds with solubility reported based on USP definition but without specific value, the lower value of the range defined in the USP was chosen (12). From these parameters, additional parameters were derived. The dose number was calculated as ratio of dose to the solubility at pH 7 (16), which was further assigned into three categories (dose number category): denoted as 1 if dose number <50, 2 if 50 ≤ dose number ≤ 250, and 3 if dose number >250. The Log D was also categorized into three categories (LogD category): denoted as 1 if Log D < −1, 2 if −1 ≤ Log D ≤ 1 and 3 if log D > 1. The maximum absorbable dose (MAD) was calculated using the following equation (17):
where the absorption rate constants of 0.0006, 0.003 and 0.0134 were used for poorly permeable (Caco-2 permeability < 20 nm/sec), moderately permeable (Caco-2 permeability between 20 and 100 nm/sec) and highly permeable (Caco-2 permeability > 100 nm/sec) compounds, respectively (18). The absorption rate constants were estimated based on the correlation between Caco-2 and human permeability of 20 compounds (18). For compounds without reported Caco-2 permeability value, the MAD value was determined from the reported value of percent absorbed in human pharmacokinetics studies. For example, tamsulosin hydrochloride was reported to be 100% absorbed at the clinical dose, the MAD to dose ratio is therefore assigned as 1 (10). This estimation may not be accurate in terms of absolute value of MAD but it is accurate in terms of the relationship between MAD and dose. Since compounds are categorized in the model based on whether the MAD is ≥ or < the dose, the relationship between MAD and dose is important for the model rather than the absolute value of MAD. Since Caco-2 permeability data were not available for all compounds in the study, Caco-2 permeability was not used as an individual parameter for prediction. In the above equation, we used 180 min as the small intestine residence time in human instead of 270 min used in the original paper (5).
All compounds were first separated into two categories: MAD < clinical dose and MAD ≥ clinical dose. The clinical dose is the dose studied for food effect in the published references. For compounds with MAD ≥ clinical dose, complete absorption is achievable. Therefore, theoretically these compounds may not show positive food effect and were fitted into negative food effect and no food effect categories, using logistic regression. Compounds with MAD < clinical dose were fitted into positive food effect, negative food effect and no food effect categories by logistic regression with cross validation using SAS™ 8.2 (19).
Logistic regression is often used to investigate the relationship between binary response (negative and no food effect in the case of MAD ≥ clinical dose) or ordinal responses (negative, no food effect and positive food effect in the case of MAD < clinical dose) and a set of explanatory variables (physicochemical variables in this study).
For the binary response model, the linear logistic model has the following form for the probability (p) of a response given the observed x:
Where α is the intercept parameter and β is the vector of slope parameters, which gives the probability of negative food effect as:
and the probability of no food effect is 1 − p.
For the ordinal response model, the three possible responses of Y were denoted by 1, 2, and 3 (Y = 1 if negative food effect, Y = 2 if no food effect, and Y = 3 if positive food effect) and x was the vector of explanatory variable. The linear logistic regression model with common slopes was fitted using LOGISTIC procedures in SAS™ 8.2 as the following:
where \( p = \Pr {\left( {Y \leqslant i\left| x \right.} \right)} \)is the cumulative probability, which means when i = 2, \( p = \Pr {\left( {Y \leqslant 2\left| x \right.} \right)} = \Pr {\left( {Y = 1\left| x \right.} \right)} + \Pr {\left( {Y = 2\left| x \right.} \right)} \); α1, α2 are two intercept parameters and β is the vector of slope parameters.
This model gives the probabilities of Y being 1 (p 1), 2 (p 2), and 3 (p 3) of given x as:
and
The score chi-square statistics was used to ensure the adequacy of common slope assumption in the ordinal response model.
During model-building, four variable selection methods: forward selection, backward elimination, stepwise selection, and best subset selection were used to select the explanatory variables based on the 0.05 significance level.
RESULTS
From logistic regression, compounds with MAD < clinical dose, the probabilities of positive, negative and no food effect were determined using the following equations:
Probability of negative food effect (p 1):
Probability of positive food effect (p 2):
Probability of no food effect (p 3):
In the above model, the score chi-square test has a p-value of 0.20, indicating adequacy of common slope assumption for the cumulative probability in the logistic model.
For compounds with MAD ≥ clinical dose, the probabilities of negative and no food effect were determined by following equations:
Probability of negative food effect (p 1):
Probability of no food effect (p 2):
The predicted food effect of each compound was assigned based on the highest probability of food effect category. The prediction results are provided in Tables IV and V and are summarized in Table VI. Overall, 74 out of 92 entries (80%) were predicted into the correct category. Compounds with positive food effect can be distinguished more easily as 97% of compounds with positive effect (30 out of 31 entries) were predicted into correct category while 79% (19 out of 24 entries) and 68% (25 out of 37 entries) compounds with negative and no food effect were predicted into correct category, respectively (Table VI). For a given prediction, the probability of correct prediction is 83, 73 and 83% for positive, negative and no food effect, respectively (Table VII). This statistical method provides more accurate prediction than the estimation based on BCS classification with 67% of the entries being predicted correctly (Table I). It should be mentioned that the accuracy of the current model is based on cross-validation, which may not hold true for an external dataset. The parameters used in present prediction are similar to those used to categorize BCS classes. The success of prediction using the current model further validates the importance of parameters used in BCS classification for oral absorption. It’s interesting to note that parameters, such as polar surface area, total surface area, percent polar surface area, number of hydrogen bond donors and acceptors, do not contribute significantly to the food effect based on the statistical analysis. The model also indicates that food effect is sensitive to the category of the properties rather than the individual value, suggesting that compounds in the same category possess similar properties for food effect.
The current model was able to predict all compounds with true positive food effect in the database of this study into the correct category except ribavarin. The model also predicted some compounds with no food effect into positive food effect category. It was more difficult to discriminate compounds with no food effect from compounds with negative food effect. The limitation of the model is described in the Discussion section.
DISCUSSION
In the statistical model, when MAD was greater than clinical dose (complete absorption, Table III), compounds with dose number category 1 (dose number <50) and log D category 1 or 2 (log D <1) were predicted to have negative food effect. Compounds with dose number category 1 and log D category 3 (log D > 1) were predicted to show no food effect. Compounds with dose number category 2 or 3 (dose number >50) and any log D category were also predicted to show no food effect. These results suggest that among compounds that can be completely absorbed, only compounds that are highly soluble (dose number <50) and hydrophilic (Log D <1) are statistically prone to show negative food effect. It has been suggested that food may serve as a physical barrier for drug absorption, which may reduce absorption of compounds with narrow window of absorption (7). Those compounds that are highly soluble and hydrophilic may belong to the class of compounds with narrow window of absorption and therefore show negative food effect.
However, the model failed to predict correctly the compounds with narrow window of absorption that are not highly soluble and hydrophilic. Based on the model, indinavir (log D = 2.66) was predicted to show positive food effect because of its low solubility and high log D value. However, it showed negative food effect in the clinical study and was attributed to its narrow window of absorption (20), which was not statistically predicted based on descriptors used in the current model. On the other hand, some highly soluble and hydrophilic compounds may not exhibit narrow window of absorption, e.g., lamivudine. This compound was predicted to have negative food effect but showed no food effect clinically (71). The root cause of these incorrect predictions is the inaccurate correlation between log D and intestinal permeability. Fexofenadine (negative food effect) was predicted to have no food effect because of high log D value. However, it has poor intestinal permeability (21). In contrast, zidovudine showed no food effect because of moderate permeability despite low log D value (22). It was reported that the correct classification of human permeability based on Log D is 87% for 16 drugs (23). A better prediction in the present model may be achieved if human intestinal permeability data are available.
For compounds with MAD less than clinical dose (incomplete absorption, Table III) with dose number category 2 or 3 (dose number >50), the model predicted to have positive food effect. Therefore, for compounds that cannot be completely absorbed because of limited solubility or dissolution rate, food enhanced their oral absorption statistically. This solubilization effect of food can be explained physiologically. Food, especially high fat meal which is often used in the food effect study, introduces higher concentration of lipids and bile salts, leading to higher solubility and dissolution rate of lipophilic compounds, e.g., halofantrine (24). It should also be noted that, the dose number, in addition being an indicator of solubility dose relationship, may also reflect other properties of a compound that are susceptable to food effect. It was reported that food may in general inhibit both influx and efflux transporters (25). For compounds with high dose number, they are more likely to be substrates of efflux transporters and therefore more likely to show positive food effect. These compounds are also more likely to be absorbed through lymphatic uptake and the postprandial increase in lymphatic flow will cause the positive food effect (26). On the other hand, compounds with low dose numbers are more likely to be the substrate of influx transporters causing negative food effect.
For compounds with incomplete absorption, if the dose number was less than 50, it was predicted to have no food effect. This result suggests that if incomplete absorption is caused by factors other than solubility, food generally exerts no effect on absorption. It is interesting to note that the food effect category is separated by dose number 50 rather than the value 250 used in BCS classification (27). The dose number 50 (the dose that can be solubilized with 50 mL of water at pH 7) was chosen arbitrary in this study to separate compounds that are highly soluble with respect to dose (dose number <50) from those that are moderately soluble (50 ≤ dose number ≤ 250). Indinavir is the only compound with MAD less than clinical dose in the entry showed negative food effect.
It is noted that all poorly soluble weak bases except indinavir in this database showed positive food effect, which suggests that initial higher gastric pH under fed condition does not impede the overall amount of weak bases dissolved as secretion of HCl with food reduces the gastric pH to around 2 within 60 min (5,6). Furthermore, the residence time of the drug in the stomach is longer with food, which may enhance the total amount dissolved. Slower entry to the intestine (delayed gastric emptying), lower duodenal pH and higher concentration of lipid and bile salts under fed conditions may also reduce the precipitation of weak bases in intestine leading to higher bioavailability.
The present model heavily relies on the accuracy of estimated MAD, which is determined by the accuracy of solubility and permeability. However, discrepancy may exist between in vitro estimated solubility and permeability and in vivo absorption. For some lipophilic compounds, the solubility in the intestinal fluid may be significantly higher than the aqueous solubility used in the current calculation, leading to underestimation of MAD values (28). The absorption rate used to calculate MAD is the average value. Some compounds may show higher absorption rate than the average value, which also leads to underestimation of MAD values. The absorption window of 3 h was used to calculate MAD, which may underestimate the MAD value of highly permeable compound with colonic absorption. Imiquimod and rofecoxib were predicted to have positive food effect but showed no food effect clinically. The estimated MADs of these two compounds based on the highest absorption rate suggested in the literature are much lower than the clinical dose because of very high dose number (18). However, it is reported that rofecoxib (29) and imiquimod (30) showed complete oral absorption in clinical study. The Cmax of these two compounds was also unaltered in the presence of food, suggesting lack of food effect on dissolution. The underestimation of MAD values of these 2 compounds lead to incorrect prediction of the food effect. The incorrect prediction for bicalutamide (predicted to have positive food effect but showed no effect clinically) is also caused by underestimated MAD value. Postpandial dosing of bicalutamide resulted in significant increase in Cmax although without effect on AUC (31). The higher Cmax may be caused by increased solubility with food. However due to high permeability, complete absorption was achieved leading to no food effect on AUC (31). It is also worth mentioning that the solubility and permeability values are collected from various sources and therefore may be associated with inaccuracy. We also only used solubility value at pH 7 and the pH effect on solubility was not considered in this study. However, since the model used categorized parameters instead of absolute values, the variability in the source data may be somewhat mitigated.
The prediction accuracy of current model is limited by the physicochemical parameters used in the model, and may not represent all factors contributing to the effect of food on AUC, such as effect on metabolism and specific chelation between food and drug. The current model also cannot predict food effect on the activity of a specific transporter responsible for the absorption of a particular compound as the current understanding of food effect on transporter is limited. Ribavirin is the only entry that showed positive food effect clinically but was not predicted correctly. It is reported that intestinal absorption of ribavirin is mediated by the concentrative Na+ nucleoside purine (CN1) transporter and can be saturated with increasing dose (1). Although the mechanism of food effect on ribavirin is unknown, the current model will not be able to predict its food effect if the activity of nucleoside purine (N1) transporter is altered by food.
The current model considers only the intrinsic properties of a compound and their relationship to the food effect. Formulations may significantly change the intrinsic property of a compound and therefore its food effect. Danazol, when dosed as conventional capsule showed significant positive food effect as predicted (32). However, no food effect was observed when danazol was dosed as an emulsion (32). Itraconazole is another example that the conventional capsule formulation showed positive food effect as predicted from the molecular properties (33) but the hydroxypropyl-β-cyclodextrin solution formulation showed negative food effect as the formulation changed the intrinsic property (solubility) of the compound (33).
Despite the limitation of the model, it successfully predicts the food effect of a compound with reasonable accuracy based on physicochemical properties. The model may be improved if additional parameters could be included when better understanding of effect of food on permeability and metabolism is achieved.
CONCLUSIONS
A statistical model is established to predict the food effect on extent of absorption based on solubility, permeability and dose of a compound. It was found that critical parameters for food effect prediction include maximum absorbable dose (MAD) category (a parameter that combines information of dose, solubility and permeability), category of dose number (a parameter that combines dose and solubility) and category of Log D (an indicator of permeability). For overall 92 entries, 80% were predicted into the correct category. 97, 79 and 68% of entries with positive, negative and no food effect, were predicted into respective correct categories. Given a compound, the probability of correct prediction is 83, 73 and 83% if it is predicted to show positive, negative or no food effect, respectively. Since all parameters used in the model can be estimated during the discovery stage, the model may be used to predict the possible food effect in early discovery.
The statistical analysis revealed that positive food effect on absorption is primarily caused by solubilization effect of food. Statistically, food causes negative effect on absorption because it interferes with absorption of compounds that are highly hydrophilic and probably with narrow window of absorption.
References
S. D. Patil, L. Y. Ngo, P. Glue, and J. D. Unadkat. Intestinal absorption of ribavirin is preferentially mediated by the Na+-nucleoside purine (N1) transporter. Pharm. Res. 15:950–952 (1998).
H. Liedholmand and A. Melander. Concomitant food intake can increase the bioavailability of propranolol by transient inhibition of its presystemic primary conjugation. Clin. Pharmacol. Ther. 40:29–36 (1986).
J. J. Leyden. Absorption of minocycline and tetracycline: effect of food, milk and iron. Int. Congr. Symp. Ser.—R. Soc. Med. 95:87–92 (1985).
D. Brownand and R. Juhl. Decreased bioavailability of digoxacin due to antacids and kaolin-pectin. N. Engl. J. Med. 19:1034–1037 (1976).
J. Dressman. Comparison of canine and human gastrointestinal physiology. Pharm. Res. 3:123–131 (1986).
T. Kararli. Comparison of the gastrointestinal anatomy, physiology, and biochemistry of human and commonly used laboratory animals. Biopharm. Drug Dispos. 16:351–380 (1995).
D. Fleisher, C. Li, Y. Zhou, L.-H. Pao, and A. Karim. Drug, meal and formulation interactions influencing drug absorption after oral administration: clinical implications. Clin. Pharmacokinet. 36:233–254 (1999).
L. Schmidtand and K. Dalhoff. Food-drug interactions. Drugs 62:1481–1502 (2002).
B. Singh. Effects of food on clinical pharmacokinetics. Clin. Pharmacokinet. 37:213–255 (1999).
Physician Desk Reference Electronic Library, http://www.thomsonhc.com/pdrel/librarian/ND_PR/Pdr Accessed 11/2004 – 02/2006.
ACD/PhysChem Batch, version 9.0. Advanced Chemistry Development, Inc. Toronto, Canada.
The United States Pharmacopeia. Authority of the United States Pharmacopeial Convention, 25th ed. National Publishing, Philadelphia, PA 2004.
Analytical Profiles of Drug Substances. Series editor: K. Florey. Academic, New York (1972–1991).
The Merck Index, 13th ed. Merck Research Laboratories, Rahway, NJ (2001).
USP DI Volume III, Approved Drug Products and Legal Requirements, 26th ed. United States Pharmacopeial Convention, Inc. Rockville, MD (2006).
D. Oh, R. Curl, and G. Amidon. Estimating the fraction dose absorbed from suspensions of poorly soluble compounds in humans: a mathematical model. Pharm. Res. 10:264–270 (1993).
W. Curatolo. Physical chemical properties of oral drug candidates in the discovery and exploratory development settings. Pharm. Sci. Technol. Today 1:387–393 (1998).
D. Sun, L. X. Yu, M. A. Hussain, D. A. Wall, R. L. Smith, and G. L. Amidon. In vitro testing of drug absorption for drug ‘developability’ assessment: forming an interface between in vitro preclinical data and clinical outcome. Curr. Opin. Drug Discov. Dev. 7:75–85 (2004).
SAS/STAT® User’s Guide, Version 6, Fourth Edition, Volume 2. Chapter 27, The LOGISTIC procedure, 1071–1126 (1990).
Y. Li. Mechanisms of region-dependent absorption of a weakly basic hiv protease inhibitor, indinavir: clinical ramifications and comparison with nelfinavir, pH. D thesis, University of Michigan, Ann Arbor, MI (2001).
N. Petri, C. Tannergren, D. Rungstad, and H. Lennernaes. Transport characteristics of fexofenadine in the Caco-2 Cell Model. Pharm. Res. 21:1398–1404 (2004).
S. Renand and E. J. Lien. Caco-2 cell permeability vs. human gastro-intestinal absorption: QSAR analysis. Prog. Drug Res. 54:1–23 (2000).
N. A. Kasim, M. Whitehouse, C. Ramachandran, M. Bermejo, H. Lennernas, A. S. Hussain, H. E. Junginger, S. A. Stavchansky, K. K. Midha, V. P. Shah, and G. L. Amidon. Molecular properties of WHO essential drugs and provisional biopharmaceutical classification. Molecular Pharmaceutics 1:85–96 (2004).
A. J. Humberstone, C. J. H. Porter, and N. W. Charman. A physicochemical basis for the effect of food on the absolute oral bioavailability of halofantrine. J. Pharm. Sci. 85:525–529 (1996).
C.-Y. Wu and L. Z. Benet. Predicting drug disposition via application of BCS: transport/absorption/elimination interplay and development of a biopharmaceutics drug disposition classification system. Pharm. Res. 22:11–23 (2005).
J. Fraser and P. Gibson. Mechanisms by which food intake elevates circulating levels of hyaluronan in humans. J. Intern. Med. 258:460–466 (2005).
G. L. Amidon, H. Lennernaes, V. Shah, and J. R. Crison. A theoretical basis for a biopharmaceutic drug classification: the correlation of in vitro drug product dissolution and in vivo bioavailability. Pharm. Res. 12:413–420 (1995).
E. M. Persson, A.-S. Gustafsson, A. S. Carlsson, R. G. Nilsson, L. Knutson, P. Forsell, G. Hanisch, H. Lennernaes, and B. Abrahamsson. The effects of food on the dissolution of poorly soluble drugs in human and in model small intestinal fluids. Pharm. Res. 22:2141–2151 (2005).
N. Ahuja, A. Singh, and B. Singh. Rofecoxib: an update on physicochemical, pharmaceutical, pharmacodynamic and pharmacokinetic aspects. J. Pharm. Pharmacol. 55:859–894 (2003).
E. Lipka, J. M. Hilfinger, C. A. Siersma, Y. Tsume, J. R. Crison, R. E. Ridgewell, and G. L. Amidon. Evaluation of Imiquimod and analogs with respect to their oral delivery potential. Proc. Int. Symp. Control. Release Bioact. Mater. 24:337–338 (1997).
I. D. Cockshott, S. D. Oliver, J. J. Young, K. J. Cooper, and D. C. Jones. The effect of food on the pharmacokinetics of the bicalutamide (‘Casodex’) enantiomers. Biopharm. Drug Dispos. 18:499–507 (1997).
W. N. Charman, M. C. Rogge, A. W. Boddy, and B. M. Berger. Effect of food and a monoglyceride emulsion formulation on danazol bioavailability. J. Clin. Pharmacol. 33:381–386 (1993).
A. Van Peer, R. Woestenborghs, J. Heykants, R. Gasparini, and G. Gauwenbergh. The effects of food and dose on the oral systemic availability of itraconazole in healthy subjects. Eur. J. Clin. Pharmacol. 36:423–426 (1989).
E. Liang, J. Proudfoot, and M. Yazdanian. Mechanisms of transport and structure-permeability relationship of sulfasalazine and its analogs in Caco-2 cell monolayers. Pharm. Res. 17:1168–1174 (2000).
C. Masungi, C. Borremans, B. Willems, J. Mensch, A. van Dijck, P. Augustijns, M. E. Brewster, and M. Noppe. Usefulness of a novel Caco-2 cell perfusion system. I. In vitro prediction of the absorption potential of passively diffused compounds. J. Pharm. Sci. 93:2507–2521 (2004).
E. K. Hussey, K. H. Donn, J. R. Powell, A. P. Lahey, and G. E. Pakes. Albuterol extended-release products: effect of food on the pharmacokinetics of single oral doses of Volmax and Proventil Repetabs in healthy male volunteers. J. Clin. Pharmacol. 31:561–4 (1991).
A. Tronde, B. Norden, H. Marchner, A.-K. Wendel, H. Lennernaes, and U. H. Bengtsson. Pulmonary absorption rate and bioavailability of drugs in vivo in rats: Structure-absorption relationships and physicochemical profiling of inhaled drugs. J. Pharm. Sci. 92:1216–1233 (2003).
J. Fuji, N. Inotsume, and M. Nakano. Effect of food on the bioavailability of bromazepam following oral administration in healthy volunteers. J. Pharmacobio-Dyn. 13:269–271 (1990).
Z. Kopitar, B. Vrhovac, L. Povsic, F. Plavsic, I. Francetic, and J. Urbancic. The effect of food and metoclopramide on the pharmacokinetics and side effects of bromocriptine. Eur. J. Drug Metab. Pharmacokinet. 16:177–181 (1991).
Y. M. Ponce, M. A. C. Perez, V. R. Zaldivar, M. B. Sanz, D. S. Mota, and F. Torrens. Prediction of intestinal epithelial transport of drug in (Caco-2) cell culture from molecular structure using in silico approaches during early drug discovery. Internet Electronic Journal of Molecular Design 4:124–150 (2005).
B. Reigner, J. Verweij, L. Dirix, J. Cassidy, C. Twelves, D. Allman, E. Weidekamm, B. Roos, L. Banken, M. Utoh, and B. Osterwalder. Effect of food on the pharmacokinetics of capecitabine and its metabolites following oral administration in cancer patients. Clin. Cancer Res. (an official journal of the American Association for Cancer Research) 4:941–948 (1998).
Bristol-Myers Squibb Internal Database. Bristol-Myers Squibb Co, New York, NY. Accessed 02/2006.
S. Yamashita, E. Hattori, A. Shimada, Y. Endoh, Y. Yamazaki, M. Kataoka, T. Sakane, and H. Sezaki. New methods to evaluate intestinal drug absorption mediated by oligopeptide transporter from in vitro study using Caco-2 cells. Drug Metab. Pharmacokinet. 17:408–415 (2002).
R. M. Menon and W. H. Barr. Comparison of ceftibuten transport across Caco-2 cells and rat jejunum mounted on modified ussing chambers. Biopharm. Drug Dispos. 24:299–308 (2003).
P. V. Desmond, P. J. Harman, N. Gannoulis, M. Kamm, and M. L. Mashford. The effect of an antacid and food on the absorption of cimetidine and ranitidine. J. Pharm. Pharmacol. 42:352–354 (1990).
A. Avdeef, P. Artursson, S. Neuhoff, L. Lazorova, J. Grasjoe, and S. Tavelin. Caco-2 permeability of weakly basic drugs predicted with the Double-Sink PAMPA pKfluxa method. Eur. J. Pharm. Sci. 24:333–349 (2005).
A. Shah, M.-C. Liu, D. Vaughan, and A. H. Heller. Oral bioequivalence of three ciprofloxacin formulations following single-dose administration: 500 mg tablet compared with 500 mg/10 mL or 500 mg/5 mL suspension and the effect of food on the absorption of ciprofloxacin oral suspension. J. Antimicrob. Chemother. 43:49–54 (1999).
N. M. Griffiths, B. H. Hirst, and N. L. Simmons. Active intestinal secretion of the fluoroquinolone antibacterials ciprofloxacin, norfloxacin and pefloxacin; a common secretory pathway? J. Pharmacol. Exp. Ther. 269:496–502 (1994).
K. Laitinen, A. Patronen, P. Harju, E. Loyttyniemi, L. Pylkkanen, T. Kleimola, and K. Perttunen. Timing of food intake has a marked effect on the bioavailability of clodronate. Bone (New York) 27:293–296 (2000).
J. Raiman, S. Tormalehto, K. Yritys, H. E. Junginger, and J. Monkkonen. Effects of various absorption enhancers on transport of clodronate through Caco-2 cells. Int. J. Pharm. 261:129–136 (2003).
C. Lippert, A. Keung, T. Arumugham, M. Eller, W. Hahne, and S. Weir. The effect of food on the bioavailability of dolasetron mesylate tablets. Biopharm. Drug Dispos. 19:17–19 (1998).
J. Dow, G. F. Di Francesco, and C. Berg. Comparison of the pharmacokinetics of dolasetron and its major active metabolite, reduced dolasetron, in dog. J. Pharm. Sci. 85:685–689 (1996).
J. J. Hanyok. Clinical pharmacokinetics of sotalol. Am. J. Cardiol. 72:19A–26A (1993).
T. D. Bjornsson, W. M. Troetel, and B. P. Imbimbo. Effect of food on the absorption of eptastigmine. Eur. J. Clin. Pharmacol. 54:243–247 (1998).
M. Stoltz, T. Arumugham, C. Lippert, D. Yu, V. Bhargava, M. Eller, and S. Weir. Effect of food on the bioavailability of fexofenadine hydrochloride (MDL 16 455A). Biopharm. Drug Dispos. 18:645–648 (1997).
F. Ingels, B. Beck, M. Oth, and P. Augustijns. Effect of simulated intestinal fluid on drug permeability estimation across Caco-2 monolayers. Int. J. Pharm. 274:221–232 (2004).
T. Shibuta, N. Inotsume, R. Iwaoku, and M. Nakano. Influence of food on pharmacokinetics and pharmacodynamics of furosemide. Byoin Yakugaku 14:12–16 (1988).
H. A. Semple, Y. K. Tam, and R. T. Coutts. Hydralazine pharmacokinetics and interaction with food: an evaluation of the dog as an animal model. Pharm. Res. 7:274–279 (1990).
L. X. Yu, A. B. Straughn, P. J. Faustino, Y. Yang, A. Parekh, A. B. Ciavarella, E. Asafu-Adjaye, M. U. Mehta, D. P. Conner, L. J. Lesko, and A. S. Hussain. The effect of food on the relative bioavailability of rapidly dissolving immediate-release solid oral products containing highly soluble drugs. Molecular Pharmaceutics 1:357–362 (2004).
T. Kosoglou, D. J. Kazierad, J. J. Schentag, J. E. Patrick, L. Heimark, E. Radwanski, D. Christopher, B. E. Flannery, and M. B. Affrime. Effect of food on the oral bioavailability of isosorbide-5-mononitrate administered as an extended-release tablet. J. Clin. Pharmacol. 35:151–158 (1995).
K. H. P. Moore, S. Shaw, A. L. Laurent, P. Lloyd, B. Duncan, D. M. Morris, M. J. O’Mara, and G. E. Pakes. Lamivudine/zidovudine as a combined formulation tablet: bioequivalence compared with lamivudine and zidovudine administered concurrently and the effect of food on absorption. J. Clin. Pharmacol. 39:593–605 (1999).
W. D. Hooper, R. G. Dickinson, and M. J. Eadie. Effect of food on absorption of lomefloxacin. Antimicrob. Agents Chemother. 34:1797–1799 (1990).
D. A. Volpe. Permeability classification of representative fluoroquinolones by a cell culture method. AAPS PharmSci 6: e13 (2004).
U. Busch, G. Heinzel, and H. Narjes. Effect of food on pharmacokinetics of meloxicam, a new nonsteroidal anti-inflammatory drug (NSAID). Agents Actions 32:52–53 (1991).
G. Ranaldi, K. Islam, and Y. Sambuy. Epithelial cells in culture as a model for the intestinal transport of antimicrobial agents. Antimicrob. Agents Chemother. 36:1374–1381 (1992).
N. B. Modi, B. Wang, W. T. Hu, and S. K. Gupta. Effect of food on the pharmacokinetics of osmotic controlled-release methylphenidate HCl in healthy subjects. Biopharm. Drug Dispos. 21:23–31 (2000).
J. Bass, K. V. Shepard, J. W. Lee, and J. Hulse. An evaluation of the effect of food on the oral bioavailability of sustained-release morphine sulfate tablets (ORAMORPH SR) after multiple doses. J. Clin. Pharmacol. 32:1003–1007 (1992).
J. Lettieri, R. Vargas, V. Agarwal, and P. Liu. Effect of food on the pharmacokinetics of a single oral dose of moxifloxacin 400 mg in healthy male volunteers. Clin. Pharmacokinet. 40:19–25 (2001).
M. N. Dudley, C. R. Marchbanks, S. C. Flor, and B. Beals. The effect of food or milk on the absorption kinetics of ofloxacin. Eur. J. Clin. Pharmacol. 41:569–571 (1991).
L. D’Angelo, F. De Ponti, F. Crema, M. Caravaggi, and A. Crema. Effect of food on the bioavailability of pidotimod in healthy volunteers. Arzneim.-Forsch. 44:1473–1475 (1994).
H. Y. Pan, A. R. DeVault, D. Brescia, D. A. Willard, M. E. McGovern, D. B. Whigan, and E. Ivashkiv. Effect of food on pravastatin pharmacokinetics and pharmacodynamics. Int. J. Clin. Pharmacol., Ther., Toxicol. 31:291–294 (1993).
M. A. H. Levine, S. E. Walker, and T. W. Paton. The effect of food and sucralfate on the bioavailability of S(+) and R(−) enantiomers of ibuprofen. J. Clin. Pharmacol. 32:1110–1114 (1992).
F. Faassen, G. Vogel, H. Spanings, and H. Vromans. Caco-2 permeability, P-glycoprotein transport ratios and brain penetration of heterocyclic drugs. Int. J. Pharm. 263:113–122 (2003).
L. I. Harrison, D. J. Riedel, K. E. Armstrong, M. B. Goldlust, and B. P. Ekholm. Effect of food on salsalate absorption. Ther. Drug Monit. 14:87–91 (1992).
G. R. Granneman and D. Mukherjee. The effect of food on the bioavailability of temafloxacin. A review of 3 studies. Clin. Pharmacokinet. 22:48–56 (1992).
D. R. Doose, S. A. Walker, L. G. Gisclon, and R. K. Nayak. Single-dose pharmacokinetics and effect of food on the bioavailability of topiramate, a novel antiepileptic drug. J. Clin. Pharmacol. 36:884–891 (1996).
D. Riendeau, M. D. Percival, C. Brideau, S. Charleson, D. Dube, D. Ethier, J. P. Falgueyret, R. W. Friesen, R. Gordon, G. Greig, J. Guay, J. Mancini, M. Ouellet, E. Wong, L. Xu, S. Boyce, D. Visco, Y. Girard, P. Prasit, R. Zamboni, I. W. Rodger, M. Gresser, A. W. Ford-Hutchinson, R. N. Young, and C. C. Chan. Etoricoxib (MK-0663): preclinical profile and comparison with other agents that selectively inhibit cyclooxygenase-2. J. Pharmacol. Exp. Ther. 296:558–566 (2001).
M. Hashiguchi, H. Ogata, A. Maeda, Y. Hirashima, S. Ishii, Y. Mori, T. Amamoto, T. Handa, N. Otsuka, et al. No effect of high-protein food on the stereoselective bioavailability and pharmacokinetics of verapamil. J. Clin. Pharmacol. 36:1022–1028 (1996).
L. A. Nazareno, A. A. Holazo, R. Limjuco, S. Passe, S. K. Twardy, B. Min, and J. W. Massarella. The effect of food on pharmacokinetics of zalcitabine in HIV-positive patients. Pharm. Res. 12:1462–1465 (1995).
E. J. Seaber, R. W. Peck, D. A. Smith, J. Allanson, N. R. Hefting, J. J. Van Lier, F. A. E. Sollie, J. Wemer, and J. H. G. Jonkman. The absolute bioavailability and effect of food on the pharmacokinetics of zolmitriptan in healthy volunteers. Br. J. Clin. Pharmacol. 46:433–439 (1998).
J. D. Irvine, L. Takahashi, K. Lockhart, J. Cheong, J. W. Tolan, H. E. Selick, and J. R. Grove. MDCK (Madin-Darby canine kidney) cells: a tool for membrane permeability screening. J. Pharm. Sci. 88:28–33 (1999).
M. V. S. Varma, K. Sateesh, and R. Panchagnula. Functional role of P-glycoprotein in limiting intestinal absorption of drugs: contribution of passive permeability to P-glycoprotein mediated efflux transport. Molecular Pharmaceutics 2:12–21 (2005).
G. E. Chittick, C. Gillotin, J. A. McDowell, Y. Lou, K. D. Edwards, W. T. Prince, and D. S. Stein. Abacavir: absolute bioavailability, bioequivalence of three oral formulations, and effect of food. Pharmacotherapy 19:932–942 (1999).
G. Merino, A. I. Alvarez, J. G. Prieto, and R. B. Kim. The anthelmintic agent albendazole does not interact with P-glycoprotein. Drug Metab. Dispos. 30:365–369 (2002).
X. Meng, P. Mojaverian, M. Doedee, E. Lin, I. Weinryb, S. T. Chiang, and P. R. Kowey. Bioavailability of amiodarone tablets administered with and without food in healthy subjects. cAm. J. Cardiol. 87:432–435 (2001).
R. Dixon, A. L. Pozniak, H. M. Watt, P. Rolan, and J. Posner. Single-dose and steady-state pharmacokinetics of a novel microfluidized suspension of atovaquone in human immunodeficiency virus-seropositive patients. Antimicrob. Agents Chemother. 40:556–560 (1996).
H. Emori, S. Yokohama, and T. Nishihata. Small intestinal absorption of bropirimine in rats and effect of bile salt on the absorption. J. Pharm. Pharmacol. 47:487–492 (1995).
H. Emori, K. Yamamoto, S. Yokohama, and T. Nishihata. Bioavailability of bropirimine 250 mg tablet in dogs: effect of food. J. Pharm. Pharmacol. 47:822–826 (1995).
H. Saitoh, B. J. Aungst, M. Tohyama, Y. Hatakeyama, K. Ohwada, M. Kobayashi, H. Fujisaki, and K. Miyazaki. In vitro permeation of b-lactam antibiotics across rat jejunum and its correlation with oral bioavailability in humans. Br. J. Clin. Pharmacol. 54:445–448 (2002).
S. K. Paulson, M. B. Vaughn, S. M. Jessen, Y. Lawal, C. J. Gresk, B. Yan, T. J. Maziasz, C. S. Cook, and A. Karim. Pharmacokinetics of celecoxib after oral administration in dogs and humans: effect of food and site of absorption. J. Pharmacol. Exp. Ther. 297:638–645 (2001).
J. McEwen, G. Strauch, P. Perles, G. Pritchard, T. E. Moreland, J. Necciari, and J. P. Dickinson. Clopidogrel bioavailability: absence of influence of food or antacids. Semin. Thromb. Hemost. 25:47–50 (1999).
A. Nordqvist, J. Nilsson, T. Lindmark, A. Eriksson, P. Garberg, and M. Kihlen. A general model for prediction of Caco-2 cell permeability. QSAR & Combinatorial Science 23:303–310 (2004).
D. G. Blanchett, J. A. Green, A. Nara, R. Pospisil, R. C. Jarvis, R. J. Kasmer, D. A. Boyle, M. J. Cyronak, and C. N. Corder. The effect of food on pharmacokinetics and pharmacodynamics of fenoldopam in class III heart failure. Clin. Pharmacol. Ther. 49:449–456 (1991).
A. Clancy, J. Locke-Haydon, R. J. Cregeen, M. Ireson, and J. Ziemniak. Effect of concomitant food intake on absorption kinetics of fenoldopam (SK&F 82526) in healthy volunteers. Eur. J. Clin. Pharmacol. 32:103–106 (1987).
J. Lavelle, S. Follansbee, C. B. Trapnell, W. C. Buhles, K. G. Griffy, D. Jung, A. Dorr, and J. Connor. Effect of food on the relative bioavailability of oral ganciclovir. J. Clin. Pharmacol. 36:238–241 (1996).
K. A. Milton, G. Edwards, S. A. Ward, M. L. E. Orme, and A. M. Breckenridge. Pharmacokinetics of halofantrine in man: effects of food and dose size. Br. J. Clin. Pharmacol. 28:71–77 (1989).
R. L. Williams, J. Mordenti, R. A. Upton, E. T. Lin, W. L. Gee, C. D. Blume, and L. Z. Benet. Effects of formulation and food on the absorption of hydrochlorothiazide and triamterene or amiloride from combination diuretic products. Pharm. Res. 4:348–352 (1987).
I. Soria, P. Myhre, V. Horton, P. Ellefson, S. McCarville, K. Schmitt, and M. Owens. Effect of food on the pharmacokinetics and bioavailability of oral imiquimod relative to a subcutaneous dose. Int. J. Clin. Pharmacol. Ther. 38:476–481 (2000).
P. J. D. Kuang, C. Yeh, H. Haddix, M. Hesney, V. Hoagland, W. D. Ju, S. J. Justice, B. Osborne, A. T. Sterrett, J. A. Stone, E. Woolf, and S. Waldman. Single-dose pharmacokinetics of indinavir and the effect of food. Antimicrob. Agents Chemother. 42:1308 (1998).
N. N. Vachharajani, W. C. Shyu, D. S. Greene, and H. D. Uderman. Effects of food on the pharmacokinetics of irbesartan/hydrochlorothiazide combination tablet. Clin. Drug Investig. 16:399–404 (1998).
A. Avdeef, P. E. Nielsen, and O. Tsinman. PAMPA—a drug absorption in vitro model 11. Matching the in vivo unstirred water layer thickness by individual-well stirring in microtitre plates. Eur. J. Pharm. Sci. 22:365–374 (2004).
D. Rosillon, A. Stockis, G. Poli, D. Acerbi, R. Lins, and B. Jeanbaptiste. Food effect on the oral bioavailability of Manidipine: single dose, randomized, crossover study in healthy male subjects. Eur. J. Drug Metab. Pharmacokinet. 23:197–202 (1998).
C. Crevoisier, J. Handschin, J. Barre, D. Roumenov, and C. Kleinbloesem. Food increases the bioavailability of mefloquine. Eur. J. Clin. Pharmacol. 53:135–139 (1997).
A. Karim, L. F. Rozek, M. E. Smith, and K. G. Kowalski. Effects of food and antacid on oral absorption of misoprostol, a synthetic prostaglandin E1 analog. J. Clin. Pharmacol. 29:439–443 (1989).
D. S. Greene and R. H. Barbhaiya. Clinical pharmacokinetics of nefazodone. Clin. Pharmacokinet. 33: 260–275 (1997).
S. M. Abdel-Rahman and G. L. Kearns. Single-dose pharmacokinetics of a pleconaril (VP63843) oral solution and effect of food. Antimicrob. Agents Chemother. 42:2706–2709 (1998).
S. M. Abdel-Rahman and G. L. Kearns. Single oral dose escalation pharmacokinetics of pleconaril (VP 63843) capsules in adults. J. Clin. Pharmacol. 39:613–618 (1999).
B. J. Aungst, N. H. Nguyen, J. P. Bulgarelli, and K. Oates-Lenz. The influence of donor and reservoir additives on Caco-2 permeability and secretory transport of HIV protease inhibitors and other lipophilic compounds. Pharm. Res. 17:1175–1180 (2000).
J. Alsenz and E. Haenel. Development of a 7-day, 96-well Caco-2 permeability assay with high-throughput direct UV compound analysis. Pharm. Res. 20:1961–1969 (2003).
R. A. Ronfeld, K. D. Wilner, and B. A. Baris. Sertraline: chronopharmacokinetics and the effect of coadministration with food. Clin. Pharmacokinet. 32:50–55 (1997).
J. Shah, A. Fratis, D. Ellis, S. Murakami, and P. Teitelbaum. Effect of food and antacid on absorption of orally administered ticlopidine hydrochloride. J. Clin. Pharmacol. 30:733–736 (1990).
J. B. Lecaillon, J. Godbillon, J. Campestrini, C. Naquira, L. Miranda, R. Pacheco, R. Mull, and A. A. Poltera. Effect of food on the bioavailability of triclabendazole in patients with fascioliasis. Br. J. Clin. Pharmacol. 45:601–604 (1998).
B. A. Hamelin, S. Allard, L. Laplante, J. Miceli, K. D. Wilner, J. Tremblay, and M. LeBel. The effect of timing of a standard meal on the pharmacokinetics and pharmacodynamics of the novel atypical antipsychotic agent ziprasidone. Pharmacotherapy 18:9–15 (1998).
Acknowledgement
The authors would like to thank the following colleagues at Bristol-Myers Squibb for providing data and useful discussion: B. Vig, N. Mathias S. Lawrence, M. Fakes, S. Badawy, F. Zhao, S. Varia, M. Zheng, K. He, V. Rao.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s11095-007-9337-x
Rights and permissions
About this article
Cite this article
Gu, CH., Li, H., Levons, J. et al. Predicting Effect of Food on Extent of Drug Absorption Based on Physicochemical Properties. Pharm Res 24, 1118–1130 (2007). https://doi.org/10.1007/s11095-007-9236-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-007-9236-1