Purpose
The effect of chitosan and polyethylene glycol (PEG)ylated trimethyl chitosan copolymer structure on the uptake and transport of insulin nanocomplexes was evaluated and transport mechanisms were investigated.
Methods
Insulin nanocomplexes were prepared from chitosan and its copolymers by self-assembly. Complex uptake in Caco-2 cells was quantified by measuring the cell-associated fluorescence and cellular localization was visualized by confocal laser scanning microscopy (CLSM) using tetra-methyl-rhodamine isothiocyanate-labeled insulin. The transport of selected insulin complexes through Caco-2 monolayers was then investigated and compared with in vivo uptake by nasal epithelium in diabetic rats.
Results
All complexes were 200–400 nm in diameter, positively charged, and displayed an insulin loading efficiency of approximately 90%. In vitro release of insulin from the complexes was dependent on the medium pH. Insulin uptake was enhanced by nanocomplex formation, and was dependent on incubation time, temperature, and concentration. Complex uptake in Caco-2 cells was inhibited by 25.2 ± 1.3%, 13.0 ± 1.0%, and 16.6 ± 0.7% in the presence of cytochalasin D, sodium azide, and 2,4-dinitrophenol, respectively. The uptake mechanism was assumed to be adsorptive endocytosis. Additionally, cell uptake efficiency was shown to be influenced by a combination of polymer molecular weight, viscosity, and positive charge density. However, none of the nanocomplexes displayed improved transport properties when compared to insulin transport data after 2 h incubation with Caco-2 monolayers. This result was further confirmed with animal experiments.
Conclusions
Small, stable insulin nanocomplexes were formed using PEGylated trimethyl chitosan copolymers, which significantly enhanced the uptake of insulin in Caco-2 cells by adsorptive endocytosis. However, nanocomplexation did not seem to enhance transcellular insulin transport across cell monolayers, which is in line with animal data in rats. This implies that PEGylated trimethyl chitosan complexes with insulin need further optimization and the Caco-2 cell line is a predictable in vitro cell culture model for drug absorption.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
To maintain blood glucose levels at a near-physiological level and thereby minimize long-term diabetic complications, treatment of insulin-dependent diabetes requires up to four subcutaneous injections per day. To circumvent this tedious regimen of therapy, several attempts have been made to exploit mucosal surfaces for the delivery of macromolecular drugs, especially the nasal, pulmonary, and oral mucosae (1). The nasal route has been a particular focus of recent research as biologically active peptides, such as desmopressin, salmon calcitonin, and corticotrophin, show significant absorption across the nasal mucosa (2).
In fact, the nasal route has been recognized as an attractive alternative to parenteral administration of insulin since 1922 (3). Despite the promise of intranasal administration for the delivery of peptides, the efficacy of the nasal route for the absorption of large peptides, e.g., insulin, is relatively low (4). Therefore, new nasal delivery systems enhancing insulin absorption have been proposed, including surfactants, protease inhibitors, and bioadhesive polymers or microspheres (5,6). Unfortunately, most penetration enhancers such as surfactants, bile salts, and fatty acids cause irreversible damage, or irritation to the nasal mucosa when used at efficacious concentrations (7). By contrast, bioadhesive nanoparticles and microparticles have been demonstrated to be well-tolerated macromolecular carriers (8,9).
Chitosan, a nontoxic and biocompatible cationic polysaccharide produced by partial deacetylation of chitin derived from naturally occurring crustacean shells, was reported to reversibly open tight junctions. The use of chitosan as a nasal delivery system was reviewed recently (10). Intranasal administration of chitosan insulin nanoparticles, formed by a mild ionotropic gelation procedure, enhanced the nasal absorption of insulin to a greater extent than an aqueous solution of chitosan (11). On the other hand, Dyer et al. (12) showed that chitosan nanoparticles did not improve the absorption-enhancing effect of chitosan in solution or powder form and that chitosan powder was the most effective formulation for the nasal delivery of insulin in a sheep model. These discrepancies cast some doubts on the advantage of nanoparticulate carriers for intranasal administration of insulin.
The mechanism of action of chitosan was attributed to be a combination of bioadhesion and a transient opening of tight junctions between epithelial cells (13). However, this absorption enhancing ability was evident only under acidic conditions (pH < 6.5), where most of the amino groups were protonated.
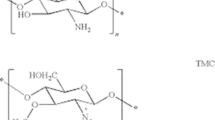
To overcome this problem, polyethylene glycol (PEG)ylated trimethyl chitosan copolymers were synthesized in our laboratory in an attempt to increase the solubility of chitosan at physiological pH and improve the biocompatibility of trimethyl chitosan (TMC) (14). Insulin nanocomplexes were prepared with the copolymers by electrostatic interaction. We speculated that by combining absorption enhancer properties (chitosan) with nanoscale dimensions (complexes), intranasal absorption of insulin could potentially be improved.
The goal of this study was to evaluate the effect of chitosan and PEGylated TMC copolymer structure on the uptake and transport of insulin nanocomplexes, and elucidate their mechanism of transport. For mechanistic studies, Caco-2, a human colon adenocarcinoma cell line, was used as in vitro cell culture model to investigate particle uptake (15,16). Such monolayers formed tight junctions, and exhibited barrier properties similar to those in intestinal and nasal epithelia. The predictive power of cell culture experiments with Caco-2 monolayers was further assessed in animal studies.
Materials and Methods
Polymers
Chitosan (400 kDa) was purchased from Fluka (Steinheim, Germany) with a degree of deacetylation (DD) of 84.7% and depolymerized by oxidative degradation to yield chitosan with molecular weights of ca. 100 and 50 kDa (17). PEGylated TMC copolymers were synthesized as described elsewhere (14). Briefly, TMC dissolved in purified water (10 mg/mL) and N-hydroxysuccinimide (NHS)-mPEG dissolved in dry DMSO (50 mg/mL) were mixed and stirred at room temperature for 24 h. Then the solution was purified by ultrafiltration twice using an Amicon cell equipped with a 10,000-MW (molecular weight) cutoff membrane. The dialyzed solution was finally freeze-dried. The number of PEG chains grafted per TMC macromolecule (graft ratio) was calculated from integrals of the 1H NMR signals for PEG blocks at ∼3.35 ppm (–OCH3) and TMC blocks at ∼3.0 ppm (–N(CH3)2) and ∼3.3 ppm (–N+(CH3)3), using the known molecular weight of mPEG. The graft ratio (wt%) was calculated according to the following equation:
where MWPEG is the molecular weight of PEG, MWTMC is the molecular weight of TMC, and n is the average number of PEG chains per TMC macromolecule calculated by 1H NMR.
The following nomenclature was adopted for the copolymers: PEG(X) n -g-TMC(Y), where X denotes the molecular weight (MW) of polyethylene glycol (PEG) in Da, Y denotes the MW of TMC in kDa, and the subscript n represents the average number of PEG chains per TMC macromolecule of Y kDa.
Preparation and Characterization of Copolymer–Insulin Self-Assembled Nanocomplexes
The complexes were prepared by self-assembly, utilizing the electrostatic interactions between the positively charged polymers and negatively charged insulin (Aventis Pharma AG, Frankfurt, Germany) as a driving force. Briefly, nanocomplexes were prepared by mixing equal volumes of insulin and polymer solution at the desired ratio (Table I) under gentle magnetic stirring, and incubated for a further 20 min at room temperature. For the preparation of chitosan–insulin complex, the pH of chitosan solution was adjusted to 5.5 and the pH of insulin solution was 8.5. In contrast, for the preparation of TMC and copolymer–insulin complex, the polymer solution and insulin solution were adjusted to pH 7.5. Complex sizes and zeta potentials were obtained using dynamic light scattering (DLS) and laser Doppler anemometry (LDA) measurements.
Dynamic Light Scattering
Complex size measurements were carried out with a Zetasizer 3000 HS from Malvern Instruments (Herrenberg, Germany; 10 mW HeNe laser, 633 nm). Scattering light was detected at a 90° angle through a 400-μm pin hole at a temperature of 25°C. Kcps (kilo counts per second), which is a measure of nanocomplexes concentration in a sample, was recorded during the measurement. Particle sizes of polyelectrolyte complexes (PEC) are given as mean ± SD (n = 10).
Laser Doppler Anemometry
The zeta potential measurements of the complexes were carried out in the standard capillary electrophoresis cell of the Zetasizer 3000 HS from Malvern Instruments (Herrenberg, Germany) at 25°C in 0.01 M Tris buffer pH 7.4 except chitosan (0.01 M Tris buffer pH 6.8). Average values of the zeta potential were calculated with the data from ten runs (±SD).
In Vitro Release Studies
Insulin release was determined by incubating the complexes (100 μL) in 1.5 mL Tris buffer (pH 7.4) and acetate buffer (pH 4.0) at 37°C. The concentration of the complex in the release media was adjusted to maintain sink conditions for insulin. At appropriate time intervals (30 min, 45 min, 1 h, 2 h, 4 h, and 6 h) individual samples were centrifuged at 14,000 rpm/min for 30 min and the amount of insulin released from the complexes was evaluated by high-performance liquid chromatography as described elsewhere (18).
Labeling of Polymers and Insulin
Chitosan (100 kDa), PEG(5k)40-g-TMC(100), and PEG(5k)19-g-TMC(50) were labeled with Oregon Green carboxylic acid succinimidyl ester (Oregon Green 488; Molecular Probes, Eugene, OR, USA) following a previously described method (19). Insulin was labeled with tetra-methyl-rhodamine isothiocyanate (TRITC; Sigma, Taufkirchen, Germany). Briefly, insulin was dissolved at a concentration of 4.5 mg/mL in 0.1 M sodium bicarbonate buffer (pH 9.3). A solution of TRITC (1 mg/mL) in dimethyl sulfoxide (DMSO) was added dropwise under stirring (insulin/TRITC molar ratio = 1:2.9) and the mixture was stirred for 18 h at 4°C under light exclusion. The reaction was quenched with an excess of ammonium chloride, and stirred for a further 4 h. Purification was performed on a PD-10 desalting column (Amersham Pharmacia Biotech, Freiburg, Germany) with phosphate-buffered salt (PBS) solution (pH 7.4).
Cell Culture
Mycoplasma-free Caco-2 cells were used at passage numbers 44–50 (HD, DKFZ, German Cancer Research Institute, Heidelberg, Germany) under previously described conditions (20). Cells were seeded at a density of 6 × 104 cells/cm2 on 12-well cell culture plates or 6-well uncoated polycarbonate Transwell™ filter inserts (Costar, Bodenheim, Germany; 0.4 μm pore size, area: 4.71 cm2) and cultivated over 21 days. The medium was changed every second day.
MTT Assay
In vitro cytotoxicity of the polymers was evaluated using an MTT assay with L929 fibroblast cell line, as described previously (17). Briefly, L929 cells were seeded into 96-well microtiter plates at a density of 8000 cells/well. After 24 h, the culture medium was replaced with 100-μL serial dilutions of polymer and cells were incubated for a further 3 h. Subsequently, 20 μL 3-(4,5-dimethyl-thiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) (5 mg/mL) was added to each well. After 4 h incubation, unreacted dye was aspirated and the formazan crystals were dissolved in DMSO (200 μL/well). Absorption was measured at 570 nm with a background correction of 690 nm using a Titertek Plus MS 212 ELISA reader (ICN, Eschwege, Germany). The relative cell viability compared to control cells containing cell culture medium (pH 6.5) without polymer was calculated by [A]test / [A]control. IC50 (the concentration at which cell growth is inhibited by 50%) values were calculated.
Uptake Studies
Cell uptake studies were performed with Caco-2 cell monolayers according to the method described by Behrens et al. (21). The uptake medium was 0.01 M Tris buffer, supplemented with 100 mM glucose, 1.17 mM CaCl2, 1.03 mM MgCl2, pH 7.4. The cell lysate, obtained by solubilizing the cells with 300 μL/well 2% SDS (pH 8.0), was measured for fluorescence with an LS 50B spectrometer (Perkin Elmer, Ueberlingen, Germany) at an excitation wavelength of 543 nm and an emission wavelength of 560 nm. Protein content was determined via bicinchoninic acid (BCA) assay according to the manufacture's protocol (Promega, Mannheim, Germany). Uptake was expressed as the quantity of insulin associated with 1 mg of cellular protein (mean ± SD, n = 3). With PEG(5k)40-g-TMC(100) copolymer–insulin complex, the effect of polymer concentration, incubation time, insulin concentration, and temperature on complex uptake was investigated. To further evaluate the possibility of complex uptake occurring through an active process, cells were preincubated with the metabolic inhibitors sodium azide (10 mM) and 2,4-dinitrophenol (0.2 mM), endocytosis inhibitors cytochalasin D (0.1 μg/mL), and nocodazole (1 μg/mL) (all were obtained from Sigma, Steinheim, Germany) for 30 min prior to complex application and throughout the 2-h uptake experiment.
Confocal Laser Scanning Microscopy
CLSM was utilized to visualize the internalization of insulin nanocomplexes. Caco-2 cells grown on glass cover slips for 7 days were treated with insulin, polymers, and complexes (insulin concentration = 250 μg/mL). After 2 h incubation at 37°C, cells were washed three times with ice-cold transport buffer, fixated with 3.7% paraformaldehyde in PBS (pH 7.4) at room temperature for 30 min, and counterstained with 4,6-diamidino-2-phenylindole (DAPI; 0.2 μg/mL) for 20 min, both under light exclusion. For samples without labeled polymer, cells were counterstained with fluorescein isothiocyanate (FITC)-labeled wheat germ agglutinin (WGA; 0.01 μg/mL) for 30 min. Samples were embedded in FluorSave™ Reagent (Calbiochem, Darmstadt, Germany) and imaged via CLSM (Zeiss Axiovert 100 M Microscope coupled to a Zeiss LSM 510 scanning device; Jena, Germany), which was equipped with a Zeiss Neofluor 63*/1.2 objective. Excitation wavelengths were 364 nm [long pass (LP) filter, 385 nm] for DAPI, 488 nm (LP 505 nm) for Oregon Green 488 and FITC, and 543 nm (LP 567 nm) for TRITC (18,20). All images were recorded using the multitracking mode, in which each fluorescence channel was scanned individually. Additionally, trypan blue was postincubated with cells for 1 min (400 μg/mL in 0.1 M citrate buffer, pH 4.4) after 2 h incubation with the complexes or polymers.
Transport Across Caco-2 Cell Monolayers
Transport studies were performed 21 days postseeding. The integrity of the monolayers was checked by measuring the transepithelial electrical resistance (TEER) values in Hank's balanced salt solution (HBSS; pH 7.4) buffer before and after the experiment, as described previously (20,21). Only cells with TEER values in the range of 250–350 Ω ·cm2 were used for the transport studies. Briefly, filter inserts were rinsed with transport buffer (pH 7.4) (the same as the uptake medium) and allowed to equilibrate at 37°C for 15 min. Experiments were carried out by replacing the apical buffer (1.5 mL) with the samples (insulin 250 μg/mL) and the basolateral buffer with fresh transport buffer (2.5 mL). Every 20 min up to 2 h, a 1.0-mL sample was collected from the basolateral chamber and replaced with fresh buffer. Each experiment was performed in triplicate. To study TEER reversibility, monolayers were rinsed with fresh transport buffer directly after the transport experiment and allowed to regenerate in fresh culture medium under culture conditions. After 24 h, monolayer integrity was checked in HBSS buffer.
Calculations and Statistics
The apparent permeability coefficient (P eff, cm/s) was calculated using the following equation:
where dc/dt (μg/s) represents the time derivative of concentration in the receiver chamber, A (cm2) the surface area of the monolayer, V R (cm3) the volume of the receiver chamber, and C 0 (μg) the initial concentration in the apical compartment. The quantity of all cell-associated insulin was calculated by subtracting the amounts transported and remaining in the apical compartment from the initial amount. Results were expressed as mean value ± SD of three experiments. Significance between the mean values was calculated using one-way ANOVA analysis (Origin 7.0 SRO, Northampton, MA, USA). Probability values (p) less than 0.05 were considered significant.
Animal Experiment
Male Wistar rats of about 250 g (Charles River, Wiga, Germany) were fasted overnight with free access to water. Diabetic rats were obtained after streptozotocin treatment (55 mg/kg) and included into the experiment when blood glucose levels exceeded 250 mg/dL. Rats were anesthetized by ether inhalation for ∼2 min in a sealed glass container, followed by intraperitoneal injection of Avertin. The animals were dosed at 10 μL/g body weight and remained anesthetized for 60–90 min (healthy) and 30–40 min (diabetic) in a supine position. The following formulations were administrated intranasally: (1) control insulin solution (insulin dose, 5 U/kg); (2) PEG(5k)40-g-TMC(100) insulin nanocomplex suspension (pH 7.4; insulin dose, 5 U/kg). They were carefully delivered to the right nostril (∼20 μL) only, using a Hamilton syringe with an attached polyethylene tube, which was inserted about 0.5 cm into the nostril. Blood glucose levels were measured directly in blood collected from the tip of the rat tail using a glucose meter (Glucometer Elite; Bayer Corp., Leverkusen, Germany) at the time points of −10 and −5 min before formulation application and at various time intervals up to 4 h postadministration. The values of the blood glucose baselines were in the range of 350–500 mg/dL for diabetic rats. Glucose concentration was calculated as a percentage of the mean value of the first three measurements for each animal. Mean values of plasma glucose levels (±SD) of four rats in each group and areas under curve were determined. Student's t test was performed to compare both experimental groups with GraphPad (San Diego, USA) software. The animal study was conducted according to the principles outlined in the Guide for the Care and Use of Laboratory Animal Resources (National Academy Press, Washington) and had received approval by the Animal Review Committee at the local authorities.
Results and Discussion
Physicochemical Characteristics of Polymers and Complexes
The properties of the polymers and the self-assembled insulin nanocomplexes are summarized in Table I. All complexes showed a size in the range of 200–400 nm, a positive surface charge and insulin association efficiency (AE) of approximately 90%. The measured particle size of the complexes decreased with the molecular weight (MW) of chitosan (p < 0.05). The size of the copolymer–insulin complexes was comparable to that of 50 kDa chitosan and 50 kDa TMC. The zeta potential of chitosan–insulin complexes was approximately 2-fold lower than that of TMC and copolymers, and a slightly or significantly decreased zeta potential was observed for the copolymers compared to that of TMC. With a similar graft ratio, the zeta potential of PEG(550)228-g-TMC(100) copolymer was lower compared to that of PEG(5k)40-g-TMC(100) due to the increased substitution ratio. The optimal charge ratio between polymer and insulin was polymer structure-dependent: it was 7:1 for chitosan, compared to 3:1 for TMC.
Figure 1 exemplifies the release profiles of insulin from complexes formed with chitosan (100 kDa) and PEG(5k)40-g-TMC(100). Similar profiles were obtained for the two complexes, showing a pH-dependent insulin release. At pH 4.0, both chitosan and insulin were positively charged, rending complexes dissociation due to electrostatic repulsion and therefore, complete insulin release. This is consistent with a previous report (11). In contrast, less than 40% insulin was released from the complex at pH 7.4 Tris buffer in 6 h, which was slow compared to the release of insulin from chitosan–insulin nanoparticles in phosphate buffer of pH 7.4, possibly due to interactions of phosphate ions with chitosan (22). Therefore, 0.01 M Tris buffer (pH 7.4) was selected for further studies.
Mechanism of Insulin Complexes Uptake
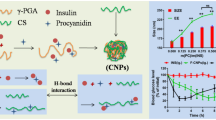
As shown in Fig. 1, after 2 h incubation at 37°C, approximately 40% of insulin was released from the complexes at pH 7.4 in Tris buffer. Therefore, insulin uptake in Caco-2 monolayers comprises both complex bound insulin and free insulin. Based on the results of uptake experiment (Fig. 5), the PEG(5k)40-g-TMC(100) copolymer–insulin complex was selected for further studies as a carrier system. Properties of the complexes were summarized in Table II. The complexes were stable at least for 4 h, which was sufficient for uptake studies.
The effect of polymer concentration, incubation time, insulin concentration, and temperature on uptake was investigated, and results are shown in Fig. 2. Insulin uptake increased with increasing polymer concentration. A 2.5-fold increase was measured when the polymer concentration increased from 125 to 500 μg/mL. Moreover, a linear relationship was established between uptake percentage and polymer concentration in the range studied (Fig. 2a). As shown in Fig. 2b, insulin uptake increased with incubation time, and more than 4-fold uptake was observed by prolonging the incubation time from 0.5 to 4 h. Moreover, the rate of uptake increased with insulin concentration despite the increased particle size, and decreased charge density (Table II) and did not exhibit saturation in the range of 62.5–500 μg/mL (Fig. 2c). The uptake amount increased 5-fold when the concentration increased from 62.5 to 500 μg/mL. However, the uptake efficiency decreased with increasing insulin concentration and leveled off at 250 μg/mL at 37°C (Fig. 2d). At 4°C the uptake efficiency was less than 3% irrespective of insulin concentration. Lowering the temperature from 37 to 4°C abolished uptake of insulin complexes by approximately 70%, indicating that the uptake is temperature-dependent. These results suggest that an energy-dependent endocytic process could be responsible for up to 70% of complexes uptake, and the other 30% attribute to physical adhesion or diffusion.
Effect of polymer concentration, insulin concentration, incubation time, and temperature on complexes uptake in Caco-2 cell line. Error bars represent mean ± SD (n = 3). (a) Effect of PEG(5k)40-g-TMC(100) copolymer concentration on complexes uptake at 37°C. The concentration of insulin was 125 μg/mL. (b) Effect of incubation time on complex uptake at 37°C. Both the concentration of insulin and PEG(5k)40-g-TMC(100) copolymer used was 125 μg/mL. (c) Uptake amount vs. insulin concentration. (d) Uptake efficiency vs. insulin concentration.
Effect of Inhibitors
When the complexes were preincubated with either sodium azide or 2,4-dinitrophenol for 30 min, complexes uptake were reduced by 13.0 ± 1.0% and 16.6 ± 0.7%, respectively, compared to that of control (Fig. 3). This observation suggests that the complex-induced increase in permeability of insulin was, to some extent, regulated by metabolic energy (cell viability, p < 0.05). When the cells were preincubated with 0.1 μg/mL cytochalasin D, an actin microfilament inhibitor, uptake was decreased by 25.2 ± 1.3%, which is significantly different from that of sodium azide or 2,4-dinitrophenol (p < 0.05), implying that uptake may be occurring by adsorptive endocytosis. In contrast, nocodazole, a microtubule inhibitor, caused only a slight reduction in complex uptake of 9.7 ± 0.5%. This is quite reasonable because microtubules are involved in vesicle transport but not in endocytosis (23). Our results are consistent with those reported by Qaddoumi et al. (24) on the uptake of 6-coumarin poly (D,L-lactide-co-glycolide) (PLGA) nanoparticles in rabbit conjunctival epithelial cells. In addition, energy depletion was also found to reduce the opening of tight junctions in Caco-2 cells (25). The reduction in complex uptake as a result of energy depletion and application of endocytosis inhibitors are compatible with adsorptive endocytosis as the main internalization mechanism for insulin complexes in Caco-2 cells.
Visualization by Confocal Laser Scanning Microscopy
To confirm an endocytic uptake mechanism, confocal microscopy was used to provide a direct evidence for complex localization. To distinguish between different cellular structures, cells were double stained with FITC-WGA (membrane, green) and DAPI (blue, nuclei). For uptake and intracellular localization studies of complexes and copolymers, both components were fluorescently labeled. With regard to insulin solution, only a slight reddish fluorescence was observed (Fig. 4D), probably as a result of passive diffusion via the transcellular route. Although there are contradictory reports in the literature concerning the potential of chitosan to be taken up by cells (26), confocal microscopy provided evidence that small amounts of polymers were internalized into Caco-2 cells (Fig. 4C). This is not surprising because other polycations such as poly-L-lysine and PEI are efficiently internalized by cells (27). In contrast, a significantly higher internalization of cell-associated insulin was found for all investigated complexes compared to the insulin control.
Confocal micrograph images of Caco-2 cell monolayers incubated with complexes, copolymer, and insulin for 2 h at 37°C. PEG(5k)40-g-TMC(100) copolymer was labeled with Oregon Green 488, insulin was labeled with tetra-methyl-rhodamine isothiocyanate, and nuclei were labeled with 4,6-diamidino-2-phenylindole. (A) Incubated with PEG(5k)40-g-TMC(100) copolymer insulin complexes (a) blue filter, (b) green filter, (c) red filter, (d) overlay of (a)–(c). (B) Incubated with PEG(5k)40-g-TMC(100) copolymer insulin complexes for 2 h and postincubated with trypan blue. (C) Incubated with PEG(5k)40-g-TMC(100) copolymer and postincubated with trypan blue. (D) Incubated with free insulin solution and postincubated with trypan blue. Cell membrane was labeled with fluorescein isothiocyanate-wheat germ agglutinin.
To test whether complexes dissociation occurred upon incubation with the cells, the samples were viewed under confocal microscopy after 2 h incubation. An exemplary image of PEG(5k)40-g-TMC(100)–insulin complexes is shown in Fig. 4A by using blue, red, and green filters, and an overlay of the images showed perfect congruence of red and green dyes. A large amount of yellow color, resulting from the colocalization of green and red, was distributed within the cytoplasm, in small, rounded vesicles localized in the perinuclear area, on the nuclear membrane, and on the apical cell membrane, suggesting that the complexes were internalized into the cells without dissociation. After uptake into the cytoplasm, the complexes might be sorted into endo-/lysosomal compartment. Due to the acidic environment (pH 4.5–5.0) in the endolysosome, both the polymer and insulin are positively charged and the complex will dissociate. Positively charged polymer will interact with the negatively charged vesicle membrane, leading to insulin release. In this case, endolysosomal escape is a rate-limiting step for insulin transport. This could be used to explain the inconsistency that, after 2 h incubation with Caco-2 cells, less complex dissociation was demonstrated by CLSM. In contrast, approximately 80% of insulin was released in acetate buffer pH 4.0 in 2 h.
Moreover, it is well known that chitosan and its derivatives possess mucoadhesive properties. They can attach on the cell surface and cannot be washed away completely. To distinguish between membrane-associated and internalized complexes, trypan blue, a dye that was reported to inhibit extracellular fluorescence (28), was used. An exemplary image is shown in Fig. 4B. Intracellular staining could be clearly observed in the images. Because viable cells excluded trypan blue molecules, the residual fluorescence implied the existence of a substantial amount of intracellular insulin complexes, rather than cell surface adsorption. Interestingly, it was noted that the complexes were mainly localized in the perinuclear region, suggesting endocytic uptake and transport to the lysosomal compartment.
Effect of Polymer Structure on Complexes Uptake in Caco-2 Cells
To study particulate uptake in vitro, the most common experimental approach is to use fluorescently labeled particles. Then, particle uptake can be indirectly determined by quantitative extraction of the markers from the cells. Moreover, particles labeled with fluorescent marker also provide visual evidence for cellular uptake. Thus, TRITC-labeled insulin was used in this study.
Here Ca2+ and Mg2+ were added to the buffer as they are essential for the tight junction function of the cells except for chitosan–insulin complexes, which was unstable in the presence of Ca2+/Mg2+. In addition, a study was carried out to investigate the effect of buffers with and without Ca2+/Mg2+, as described in detail in the transport part and no significant influence was found.
To facilitate their direct comparison, all chitosans and copolymers were investigated at 250 μg/mL (constant insulin concentration, 125 μg/mL) except for TMC (125 μg/mL), which is cytotoxic according to MTT assay. TMC displayed an IC50 of approximately 100 μg/mL after 3 h incubation with L929 cells, compared to an IC50 > 500 μg/mL for all the copolymers investigated here. The uptake results after 2 h incubation with Caco-2 cells are shown in Fig. 5. Compared to free insulin solution, all complexes improved insulin uptake significantly (p < 0.05), the extent of which depended on the polymer structure. Although the aforementioned study showed that polymer concentration had a significant effect on uptake (Fig. 2), the highest uptake was observed for TMC despite the lower concentration and comparable result was obtained for the copolymer PEG(5k)40-g-TMC(100). With regard to chitosan, insulin uptake efficiency was MW-dependent, and a 2-fold uptake was observed for 100 and 50 kDa chitosan, compared to 400 kDa chitosan. However, an inverse finding was reported by Huang et al. (29), who indicated that higher MW is preferable regarding A549 cellular uptake of chitosan nanoparticles. This discrepancy could be explained by the different molecular weight range investigated and different particle size employed. In Huang et al.'s report, the range of chitosan molecular weight was 213–10 kDa compared to 400–50 kDa in our study. We assume that the influence of molecular weight depends on whether the molecular weight difference is large enough to cause some changes in PEC parameters. It is well known that cell uptake efficiency was particle size-dependent, and smaller size is preferable (30,31). The decreased particle size (226.8 ± 6.3 vs. 376.4 ± 0.3 for 50 and 400 kDa chitosan, respectively) could probably lead to enhanced uptake. Regarding chitosan at 100 and 50 kDa, it is likely that the molecular weight difference is too small to cause significant influence in complex uptake. In terms of the copolymers, PEG(5k)40-g-TMC(100) (MW = 300 kDa) was more effective compared to PEG(5k)19-g-TMC(50) (MW = 145 kDa) with the same graft ratio. Considering that they have comparable particle size, we assume that besides zeta potential difference (18.8 ± 0.3 vs. 15.0 ± 1.2), polymer molecular weight may play an important role in the permeation ability and high molecular weight is preferred. Ranaldi et al. (27) observed a similar phenomenon. Similar results were obtained with PEG(550)228-g-TMC(100), PEG(550)132-g-TMC(50), and PEG(5k)19-g-TMC(50) copolymers, where uptake quantities were comparable to that of chitosan at 50 kDa.
As shown in Fig. 5, complex uptake data were correlated with zeta potential values. The observed high uptake efficiency of 100 and 50 kDa TMC were in line with their high positive charge, and negligible statistical difference was observed between each data set (p > 0.05). However, the cytotoxicity of TMC could possibly be a cause for the high uptake efficiency. With similar graft ratios, the cell uptake efficiency of PEG(5k)40-g-TMC(100) insulin complexes, which was comparable to that of pure TMC, was significantly higher than that of PEG(550)228-g-TMC(100), probably as a consequence of its relatively high positive charge, whereas the other copolymers had lower zeta potential and showed lower cellular uptake. Nevertheless, negligible statistical difference was observed between PEG(5k)19-g-TMC(50) and PEG(550)132-g-TMC(50) insulin complexes (p > 0.05).
Transport Studies
Effect of Calcium and Magnesium in the Transport Buffer
The mechanism of chitosan to enhance the absorption of drug substance is reported to be a combination of mucoadhesion and a transient opening of the tight junctions in the mucosal cell membrane (26). The intactness of tight junction is linked to the presence of Ca2+/Mg2+ ions (32). Reduction of extracellular Ca2+ concentration has been reported to result in an opening of tight junctions and consequently increased the paracellular permeability of epithelial cell monolayers (33). Similarly, Ranaldi et al. (27) reported that the presence of calcium ions significantly reduced the permeability of Caco-2 cells via treatment with 0.002% chitosan, but had no effect for Mg2+. In contrast, the promoting effect of another polycation, poly-l-arginine, has been demonstrated in a calcium-independent manner (34). The influence of Ca2+/Mg2+ on the transport was investigated with PEG(5k)40-g-TMC(100) copolymer–insulin complexes in both cases and their influence was found to be marginal (p > 0.05) (Fig. 6a), implying that insulin complexes could not pass through the tight junction, or at least paracellular transport was not the main pathway despite the ability of chitosan derivatives to open the tight junctions. Although tight junctions are dynamic structure and can open and close to a certain degree, when needed, the mean size of the channels is in the order of less than 10 Å, and the transport of large molecules is rather limited. Our previous study also demonstrated this point (21). It showed that after the incubation with a solution of FITC–BSA mixed with chitosan, the detected fluorescence was significantly lower as compared to chitosan nanoparticles (21). Similarly, if opening the tight junction is the main mechanism, a large amount of insulin should be measured in the basolateral compartment; this, however, is not the case. So far, all data in the literature demonstrated that chitosan derivatives could open the tight junction on a molecular level. No direct evidence was supplied to demonstrate transport of drug substance through a tight junction.
(a) Apparent permeability coefficient (P eff) of different polymer–insulin nanocomplexes in Caco-2 cells during 120 min (n = 3). The concentration of insulin was 250 μg/mL. (b) Percentage of amount of insulin internalized/attached in Caco-2 cell monolayers after 2 h incubation. Each point represents the mean ± SD of three experiments.
On the other hand, the amount of insulin remaining in the apical compartment after 2 h incubation was measured and the amount of internalized or attached insulin was calculated, as shown in Fig. 6b. Complexes considerably enhanced insulin uptake in Caco-2 cells; approximately 50% of insulin was attached or internalized in the cells, 3.5-fold higher compared with free insulin, irrespective of Ca2+/Mg2+.
Effect of Chitosan MW
Transport of chitosan (100 and 50 kDa)–insulin complexes was investigated in transport buffer without Ca2+/Mg2+, and the P eff values are depicted in Fig. 6a. No significant difference was found between each other (p > 0.05,) and both of them were considerably lower compared with that of free insulin. Similarly, Ma and Lim (35) reported no measurable level of fluorescence in the basolateral compartment after 4 h incubation with chitosan nanoparticles. Qaddoumi et al. (24) also observed a low transport value through cell monolayers with 6-coumarin-loaded nanoparticles. Instead, large amount of insulin complexes (30–50%) were internalized or attached on cell monolayers (Fig. 6b).
Effect of TMC MW in the Copolymers
To elucidate the influence of TMC MW in the copolymers on the transport properties of insulin, two copolymers, PEG(5k)40-g-TMC(100) and PEG(5k)19-g-TMC(50), with similar graft ratio were employed. Results are depicted in Fig. 6. In agreement with the cell uptake results, the P eff value of PEG(5k)40-g-TMC(100) insulin complexes was higher than that of PEG(5k)19-g-TMC(50), which, however, is not significantly different due to a high standard deviation (p > 0.05). PEG(5k)40-g-TMC(100) copolymer is advantageous compared to chitosan concerning transport (p < 0.05). No difference was found between PEG(5k)19-g-TMC(50) copolymer and chitosan (p > 0.05). Compared to free insulin solution, only at the initial 40 min did PEG(5k)40-g-TMC(100) copolymer–insulin complexes enhance insulin transport remarkably; the difference became marginal after 1 h (data not shown), and the P eff value was slightly lower than the insulin solution (p > 0.05). Similar to chitosan–insulin complexes, high internalization could be an advantage of PEC over insulin solution (Fig. 6b).
Additionally, TEER values were measured after 2 h incubation with the complexes. A 40–60% decrease in TEER was measured for the copolymers and these effects were reversible. In contrast, TEER decreased approximately by 60% for 100 and 50 kDa chitosan and no reversibility was observed after 24 h. Ranaldi et al. (27) observed the same phenomenon even with 0.01% chitosan. Shortage of calcium and magnesium as a cause could be ruled out, because TEER reversibility was observed after incubation with PEG(5k)40-g-TMC(100) copolymer–insulin complexes in the same buffer. Probably due to the mucoadhesive properties of chitosan, it cannot be washed off completely and the amount left over affects the opening of tight junction.
In Vivo Studies
Based on the uptake and transport data, PEG(5k)40-g-TMC(100) insulin nanocomplexes were selected and the biological efficacy was estimated in diabetic rats by measuring the plasma glucose concentration and compared with that of insulin control solution, as shown in Fig. 7. However, during the 4-h investigation, the decrease in plasma glucose levels was not significantly different from that induced by the insulin control solution (p > 0.05). This is in agreement with the results from the transport data in Caco-2 cells, implying that Caco-2 cell line is a reliable in vitro cell culture model to predict the absorption of drug substance in vivo.
Recently, the pharmacologic response of an insulin–chitosan (MW = 205 kDa, DD =83%) solution formulation was shown to be significantly larger than those produced by equivalent nanoparticle and complex formulations in the rat and sheep models after intranasal administration (12). There was no significant difference between the pharmacokinetic/pharmacodynamic parameters obtained for the chitosan nanoparticles and complexes compared to insulin control solution (12). This is in agreement with our results. In addition, it should be noted that the pharmacodynamics was investigated at pH 7.4 in our study. It is well known that the absorption enhancing capability of chitosan is pH-dependent, and the effect is more pronounced at pH < 6.5. Additionally, a higher charge density will facilitate the interaction with the nasal mucosa, leading to enhanced absorption. In another study, chitosan (CL110, CL210) nanoparticles (300–400 nm) were shown to increase nasal insulin absorption to a greater extent than insulin control solutions in rabbits (11). However, the experiment was performed at pH 4.3 and the nanoparticles were highly positively charged (11). At any rate, the putative advantage of using insulin complexes or nanoparticles for enhancing insulin absorption at physiological pH could not be confirmed. On the other hand, confocal microscopy studies demonstrated that there was still a large amount of insulin complexes available in an intact state within the cells after 2 h incubation. Therefore, the slow release of insulin from the complex might be responsible for the insufficient pharmacological efficiency of the formulation under in vivo conditions. In addition, it means that insulin nanocomplexes inside epithelial cell layers will not escape by transcytosis. At present, strategies are being studied to accelerate complex dissociation in the cells. Moreover, mechanisms to activate transcytosis could be promising for further studies.
Conclusion
Self-assembled insulin nanocomplexes were formed between insulin and chitosan derivatives. The complexes exhibit a small particle size and high loading efficiency. In vitro release of insulin was dependent on the medium pH. Encapsulation of insulin into complexes enhanced association with the Caco-2 cell monolayers up to 3-fold when compared to free insulin solution. The cell uptake efficiency was shown to be a combination of polymer molecular weight, viscosity, and charge density. Uptake of insulin complexes was time-, concentration-, and temperature-dependent. Coincubation with metabolic inhibitors and endocytosis inhibitors prevented complex uptake. Based on studies of uptake and confocal images, internalization of the complexes seems to occur via adsorptive endocytosis, an energy-dependent process occurring by nonspecific interactions of the carrier with the cell membrane, electrostatic interactions between the positively charged complexes and negatively charged membrane, and the mucoadhesive ability of the polymers. However, nanocomplexes did not seem to enhance insulin transport across cell monolayers at physiological pH. This point was further confirmed with in vivo data in diabetic rats. The concept of using nanocomplexes for enhancing peptide uptake through epithelia remains controversial. The Caco-2 cell line seems to be a predictive in vitro model for studying drug absorption based upon nanocomplexes.
References
A. P. Sayani Y. W. Chien (1996) ArticleTitleSystemic delivery of peptides and proteins across absorptive mucosae Crit. Rev. Ther. Drug Carrier Syst. 13 85–184 Occurrence Handle8853960 Occurrence Handle1:CAS:528:DyaK28XlsV2qt7Y%3D
L. Illum (2003) ArticleTitleNasal drug delivery—possibilities, problems and solutions J. Control. Release 87 187–198 Occurrence Handle12618035 Occurrence Handle10.1016/S0168-3659(02)00363-2 Occurrence Handle1:CAS:528:DC%2BD3sXhsFOls7c%3D
R. T. Woodyatt (1922) ArticleTitleThe clinical use of insulin J. Metab. Res. 2 793 Occurrence Handle1:CAS:528:DyaB3sXhvVOrsw%3D%3D
C. McMartin L. E. Hutchinson R. Hyde G. E. Peters (1987) ArticleTitleAnalysis of structural requirements for the absorption of drugs and macromolecules from the nasal cavity J. Pharm. Sci. 76 535–540 Occurrence Handle2889824 Occurrence Handle1:CAS:528:DyaL2sXlvFShurg%3D
V. H. L. Lee (1990) ArticleTitleProtease inhibitors and penetration enhancers as approaches to modify peptide absorption J. Control. Release 13 213–223 Occurrence Handle10.1016/0168-3659(90)90011-H Occurrence Handle1:CAS:528:DyaK3cXmtlOlsL4%3D
N. F. Farraj B. R. Johansen S. S. Davis L. Illum (1990) ArticleTitleNasal administration of insulin using bioadhesive microspheres as a delivery system J. Control. Release 13 253–261 Occurrence Handle10.1016/0168-3659(90)90016-M Occurrence Handle1:CAS:528:DyaK3cXmtlOktr8%3D
F. M. H. M. Merkus N. G. M. Schipper W. A. J. J. Hermens V. S. G. Romeijin J. C. Verhoef (1993) ArticleTitleAbsorption enhancers in nasal drug delivery: efficacy and safety J. Control. Release 24 201–208 Occurrence Handle10.1016/0168-3659(93)90179-9 Occurrence Handle1:CAS:528:DyaK3sXls1OmsLY%3D
L. Illum H. Jorgensen H. Bisgaard O. Krogsgaard N. Rossing (1987) ArticleTitleBioadhesive microspheres as a potential nasal drug delivery system Int. J. Pharm. 39 189–199 Occurrence Handle10.1016/0378-5173(87)90216-X Occurrence Handle1:CAS:528:DyaL2sXmt1eitLw%3D
K. A. Janes P. Calvo M. J. Alonso (2001) ArticleTitlePolysaccharide colloidal particles as delivery systems for macromolecules Adv. Drug Deliv. Rev. 47 83–97 Occurrence Handle11251247 Occurrence Handle10.1016/S0169-409X(00)00123-X Occurrence Handle1:CAS:528:DC%2BD3MXhvVajsrY%3D
L. Illum I. Jabbal-Gill M. Hinchcliffe A. N. Fisher S. S. Davis (2001) ArticleTitleChitosan as a novel nasal delivery system for vaccines Adv. Drug Deliv. Rev. 51 81–96 Occurrence Handle11516781 Occurrence Handle10.1016/S0169-409X(01)00171-5 Occurrence Handle1:CAS:528:DC%2BD3MXmtV2ntLc%3D
R. Fernández-Urrusuno P. Calvo C. Remuñán-López J. Vila-Jato M. Alonso (1999) ArticleTitleEnhancement of nasal absorption of insulin using chitosan nanoparticles Pharm. Res. 16 1576–1581 Occurrence Handle10554100
A. M. Dyer M. Hinchcliffe P. Watts J. Castile I. Jabbal-Gill R. Nankervis A. Smith L. Illum (2002) ArticleTitleNasal delivery of insulin using novel chitosan based formulations: a comparative study in two animal models between simple chitosan formulations and chitosan nanoparticles Pharm. Res. 19 998–1008 Occurrence Handle12180553 Occurrence Handle10.1023/A:1016418523014 Occurrence Handle1:CAS:528:DC%2BD38Xltl2isLk%3D
P. Artursson T. Lindmark S. S. Davis L. Illum (1994) ArticleTitleEffect of chitosan on the permeability of monolayers of intestinal epithelial cells (Caco-2 cells) Pharm. Res. 11 1358–1361 Occurrence Handle7816770 Occurrence Handle10.1023/A:1018967116988 Occurrence Handle1:CAS:528:DyaK2cXls12ltbg%3D
S. Mao X. Shuai F. Unger M. Wittmar X. Xie T. Kissel (2005) ArticleTitleSynthesis, characterization and cytotoxicity of poly(ethylene glycol)-graft-trimethyl chitosan block copolymers Biomaterials 26 6343–6356 Occurrence Handle15913769 Occurrence Handle10.1016/j.biomaterials.2005.03.036 Occurrence Handle1:CAS:528:DC%2BD2MXlsVCktL0%3D
F. Delie (1998) ArticleTitleEvaluation of nano- and microparticle uptake by the gastrointestinal tract Adv. Drug Deliv. Rev. 34 221–233 Occurrence Handle10837679 Occurrence Handle10.1016/S0169-409X(98)00041-6 Occurrence Handle1:CAS:528:DyaK1cXnsFWlt7w%3D
S. McClean E. Prosser E. Meehan D. O'Malley N. Clarke Z. Ramtoola D. Brayden (1998) ArticleTitleBinding and uptake of biodegradable poly-dl-lactide micro- and nanoparticles in intestinal epithelia Eur. J. Pharm. Sci. 6 153–163 Occurrence Handle9795038 Occurrence Handle1:CAS:528:DyaK1cXhsFejt7s%3D
S. Mao X. Shuai F. Unger M. Simon D. Bi T. Kissel (2004) ArticleTitleThe depolymerization of chitosan: effects on physicochemical and biological properties Int. J. Pharm. 281 45–54 Occurrence Handle15288342 Occurrence Handle10.1016/j.ijpharm.2004.05.019 Occurrence Handle1:CAS:528:DC%2BD2cXmtFCmurc%3D
M. Simon M. Wittmar U. Bakowsky T. Kissel (2004) ArticleTitleSelf-assembling nanocomplexes from insulin and water-soluble branched polyesters, poly[(vinyl-3-(diethylamino)-propylcarbamate-co-(vinyl acetate)-co-(vinyl alcohol))-graft-poly(l-lactic acid): a novel carrier for transmucosal delivery of peptides Bioconjug. Chem. 15 841–849 Occurrence Handle15264872 Occurrence Handle10.1021/bc0341627 Occurrence Handle1:CAS:528:DC%2BD2cXlt1ynsro%3D
T. Merdan K. Kunath D. Fischer J. Kopecek T. Kissel (2002) ArticleTitleIntracellular processing of poly(ethylene imine)/ribozyme complexes can be observed in living cells by using confocal laser scanning microscopy and inhibitor experiments Pharm. Res. 19 140–146 Occurrence Handle11883640 Occurrence Handle10.1023/A:1014212630566 Occurrence Handle1:CAS:528:DC%2BD38XitVSmu7k%3D
E. Walter T. Kissel (1995) ArticleTitleHeterogeneity in the human intestinal cell line Caco-2 leads to differences in transepithelial transport Eur. J. Pharm. Sci. 3 215–230 Occurrence Handle1:CAS:528:DyaK2MXntl2htrY%3D Occurrence Handle10.1016/0928-0987(95)00010-B
I. Behrens A. I. V. Pena M. J. Alonso T. Kissel (2002) ArticleTitleComparative uptake studies of bioadhesive and non-bioadhesive nanoparticles in human intestinal cell lines and rats: the effect of mucus on particle adsorption and transport Pharm. Res. 19 1185–1193 Occurrence Handle12240945 Occurrence Handle10.1023/A:1019854327540 Occurrence Handle1:CAS:528:DC%2BD38XmtlGgs7g%3D
J. Z. Knaul S. M. Hudson K. A. M. Creber (1999) ArticleTitleImproved mechanical properties of chitosan fibers J. Appl. Polym. Sci. 72 1721–1732 Occurrence Handle10.1002/(SICI)1097-4628(19990624)72:13<1721::AID-APP8>3.0.CO;2-V Occurrence Handle1:CAS:528:DyaK1MXis1Gmur4%3D
M. M. Zegers K. J. Zaal S. C. IJzendoorn Particlevan K. Klappe D. Hoekstra (1998) ArticleTitleActin filaments and microtubules are involved in different membrane traffic pathways that transport sphingolipids to the apical surface of polarized HepG2 Cells Mol. Biol. Cell. 9 1939–1949 Occurrence Handle9658181 Occurrence Handle1:CAS:528:DyaK1cXkslynsbY%3D
M. G. Qaddoumi H. Ueda J. Yang J. Davda V. Labhasetwar V. H. L. Lee (2004) ArticleTitleThe characteristics and mechanisms of uptake of PLGA nanoparticles in rabbit conjunctival epithelial cell layers Pharm. Res. 21 641–648 Occurrence Handle15139521 Occurrence Handle1:CAS:528:DC%2BD2cXjsVWqs7s%3D
N. G. Schipper K. M. Varum P. Artursson (1996) ArticleTitleChitosans as absorption enhancers for poorly absorbable drugs: 1. Influence of molecular weight and degree of acetylation on drug transport across human intestinal epithelial (Caco-2) cells Pharm. Res. 13 1686–1692 Occurrence Handle8956335 Occurrence Handle10.1023/A:1016444808000 Occurrence Handle1:CAS:528:DyaK28XnsVOhs70%3D
N. G. Schipper S. Olsson J. A. Hoogstraate A. G. deBoer K. M. Vårum P. Artursson (1997) ArticleTitleChitosans as absorption enhancers for poorly absorbable drugs: 2. Mechanism of absorption enhancement Pharm. Res. 14 923–929 Occurrence Handle9244151 Occurrence Handle10.1023/A:1012160102740 Occurrence Handle1:CAS:528:DyaK2sXkvVCitbw%3D
G. Ranaldi I. Marigliano I. Vespiignani G. Perozzi Y. Sambuy (2002) ArticleTitleThe effect of chitosan and other polycations on tight junction permeability in the human intestinal Caco-2 cell line J. Nutr. Biochem. 13 157–167 Occurrence Handle11893480 Occurrence Handle1:CAS:528:DC%2BD38XhvVWktb0%3D Occurrence Handle10.1016/S0955-2863(01)00208-X
C. P. Wan C. S. Park B. H. Lau (1993) ArticleTitleA rapid and simple microfluorometric phagocytosis assay J. Immunol. Methods 162 1–7 Occurrence Handle8509646 Occurrence Handle10.1016/0022-1759(93)90400-2 Occurrence Handle1:CAS:528:DyaK3sXks12ru78%3D
M. Huang E. Khor L.-Y. Lim (2004) ArticleTitleUptake and cytotoxicity of chitosan molecules and nanoparticles: effects of molecular weight and degree of deacetylation Pharm. Res. 21 344–353 Occurrence Handle15032318 Occurrence Handle10.1023/B:PHAM.0000016249.52831.a5 Occurrence Handle1:CAS:528:DC%2BD2cXhtlWqtr4%3D
M. P. Desai V. Labhasetwar E. Walter R. J. Levy G. L. Amidon (1997) ArticleTitleThe mechanism of uptake of biodegradable microparticles in Caco-2 cells is size dependent Pharm. Res. 14 1568–1573 Occurrence Handle9434276 Occurrence Handle10.1023/A:1012126301290 Occurrence Handle1:CAS:528:DyaK2sXotVGnu7c%3D
T. Jung W. Kamm A. Bteitenbach E. Kaiserling J. X. Xiao T. Kissel (2000) ArticleTitleBiodegradable nanoparticles for oral delivery of peptides: is there a role for polymers to affect mucosal uptake? Eur. J. Pharm. Biopharm. 50 147–160 Occurrence Handle10840198 Occurrence Handle1:CAS:528:DC%2BD3cXjslyisrs%3D
L. Gonzalez-Mariscal R. G. Contreras J. J. Bolivar A. Ponce B. Chavez de Ramirez M. Cereijido (1990) ArticleTitleRole of calcium in tight junction formation between epithelial cells Am. J. Physiol. 259 C978–C986 Occurrence Handle2124417 Occurrence Handle1:CAS:528:DyaK3MXnvFejuw%3D%3D
A. B. J. Noach Y. Kurosaki M. C. M. Blom-Rosmalen A. G. Boer Particlede D. D. Breimer (1993) ArticleTitleCell-polarity dependent effect of chelation on the paracellular permeability of confluent Caco-2 cell monolayers Int. J. Pharm. 90 229–237 Occurrence Handle10.1016/0378-5173(93)90195-L Occurrence Handle1:CAS:528:DyaK3sXit1CqtLw%3D
K. Ohtake T. Maeno H. Ueda M. Ogihara H. Natsume Y. Morimoto (2003) ArticleTitlePoly-l-arginine enhances paracellular permeability via serine/rhreonine phosphorylation of ZO-1 and tyrosine dephosphorylation of occludin in rabbit nasal epithelium Pharm. Res. 20 1838–1845 Occurrence Handle14661930 Occurrence Handle1:CAS:528:DC%2BD3sXptVChur4%3D
Z. Ma L. Lim (2003) ArticleTitleUptake of chitosan and associated insulin in Caco-2 cell monolayers: a comparison between chitosan molecules and chitosan nanoparticles Pharm. Res. 20 1812–1819 Occurrence Handle14661926 Occurrence Handle10.1023/B:PHAM.0000003379.76417.3e Occurrence Handle1:CAS:528:DC%2BD3sXptVChtbw%3D
Acknowledgment
Shirui Mao cordially thanks Deutsche Akademische Austauschdienst (DAAD) for the financial support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mao, S., Germershaus, O., Fischer, D. et al. Uptake and Transport of PEG-Graft-Trimethyl-Chitosan Copolymer–Insulin Nanocomplexes by Epithelial Cells. Pharm Res 22, 2058–2068 (2005). https://doi.org/10.1007/s11095-005-8175-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-005-8175-y