Abstract
A body of work has developed over the last 20 years that explores facial emotion perception in Borderline Personality Disorder (BPD). We identified 25 behavioural and functional imaging studies that tested facial emotion processing differences between patients with BPD and healthy controls through a database literature search. Despite methodological differences there is consistent evidence supporting a negative response bias to neutral and ambiguous facial expressions in patients. Findings for negative emotions are mixed with evidence from individual studies of an enhanced sensitivity to fearful expressions and impaired facial emotion recognition of disgust, while meta-analysis revealed no significant recognition impairments between BPD and healthy controls for any negative emotion. Mentalizing studies indicate that BPD patients are accurate at attributing mental states to complex social stimuli. Functional neuroimaging data suggest that the underlying neural substrate involves hyperactivation in the amygdala to affective facial stimuli, and altered activation in the anterior cingulate, inferior frontal gyrus and the superior temporal sulcus particularly during social emotion processing tasks. Future studies must address methodological inconsistencies, particularly variations in patients’ key clinical characteristics and in the testing paradigms deployed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Borderline Personality Disorder (BPD) is a common severe mental disorder. Its prevalence is between 1.4 and 5.9 % in the general population (Aragonès et al. 2012), increasing to over 20 % in psychiatric outpatient samples (Korzekwa et al. 2008) and over 40 % in inpatient settings (Grilo et al. 1998; Marinangeli et al. 2000).
Along with disruption of interpersonal relationships, self-identity and impulse control (Gunderson and Lyons-Ruth 2008), emotional dysregulation that encompasses both the personal experience of emotion as well as the recognition of emotion in others, lies at the core of BPD diagnostic criteria (Sanislow et al. 2002; Putnam and Silk 2005). This dysregulation is linked to self-injurious and suicidal behaviour and can radically impede treatment engagement (Brodsky et al. 2006). As a consequence, establishing the cognitive basis of disordered affect in BPD remains an unmet research priority (Linehan 1993; Conklin et al. 2006).
Emotion detection tasks involve the identification of an emotional stimulus without specifically labelling the affective state (Schulze et al. 2012). Emotion recognition is the explicit labelling of a perceived emotional stimulus (Derntl et al. 2009). Facial affect detection and recognition are key components of non-verbal communication and social interactions (Unoka et al. 2011), that may be compromised in BPD. The precise nature and balance of the deficits remains contentious, for example it may be that patients with BPD have particular difficulty decoding facial information (Dyck et al. 2009; Domes et al. 2011) or they may experience profound sensitivity to at least some aspects of facial emotional stimuli (Linehan 1993). Indeed these seemingly discrepant hypotheses have led to the formulation of a central paradox in BPD (Krohn 1974), in short that patients experience subtle impairments in basic facial emotion recognition (FER), yet a heightened sensitivity to negative emotions, and a negative appraisal bias when interpreting ambiguous stimuli in others (Domes et al. 2009).
Beyond basic facial emotion detection and recognition it may be that a subcomponent, ‘eye-reading’ ability, is central to complex social judgements and mental state appraisal for conditions such as guilt, admiration and flirtatiousness (Baron-Cohen et al. 2001). This concept has stretched experimental paradigm design from the classic Ekman faces to affect stimuli focussed on the eye region (Adolphs et al. 2005) embodied in the Reading the Mind in the Eyes Test (RMET) (Baron-Cohen et al. 1997), an advanced affective theory of mind task.
Early functional imaging work linked facial emotion processing (FEP) deficits to heightened amygdala activity (Donegan et al. 2003; Minzenberg et al. 2007). Newer work now considers functional connectivity across distributed anatomical and functional networks that underpin the functional deficits in emotional processing in this disorder (Cullen et al. 2011).
In this review we set out to summarise and evaluate the existing evidence for altered facial emotion processing in BPD and its neural underpinnings through a systematic literature review and meta-analysis.
Methods
Screening Procedure
We searched The Web of Knowledge, Scopus, CINAHL, PsycINFO, Embase and the Cochrane Central databases in November 2012 for relevant papers, with no date restrictions. We included published articles from peer reviewed journals and unpublished sources including doctoral dissertations, master’s theses and conference presentations. We used the keywords (and synonyms) “BPD” or “Borderline Personality Disorder” combined with “facial expression”, “emotion”, “recognition”, “detection”, “discrimination”, “affect”, “sensitivity” and “perception”. The additional terms “functional neuroimaging”, “fMRI” and “functional connectivity” were also incorporated into the search strategy.
One author (A.M.) screened the title and abstract of returned articles for inclusion while the reference lists and citations of all included studies and relevant reviews were manually searched for additional studies. We attempted to contact corresponding authors if further information was needed or to obtain the full text of unpublished manuscripts. Eligibility of the articles was assessed independently by A.M and M.P. Studies were included if they met the following criteria: firstly the diagnosis of BPD was made according to DSM-III, DSM-III-R, DSM-IV, ICD-9, ICD-10 or research diagnostic criteria (RDC) or using a validated BPD specific (full diagnostic or screening) instrument. Studies had to include adolescents or adults with BPD and a comparison group (healthy control or a clinical comparison). The experimental paradigms could use stimuli ranging from full faces or subcomponents, for example the eyes, to study emotion detection or recognition. Studies of a range of target emotions from positive to negative were included, as were those of facial expressions of neutral or ambiguous conditions. Functional neuroimaging studies were included if they used a paradigm designed to index implicit or explicit facial emotion processing. Only English language studies were included.
Meta-Analysis for Individual Negative Emotions
In order to augment our narrative analysis we compared effect sizes derived from facial affect recognition studies. We restricted the analysis to negative facial emotions on the basis of the qualitative review and data availability after applying the following additional inclusion criteria:
-
The studies reported results separately for at least one of the four basic negative emotions: anger, fear disgust, or sadness.
-
The studies reported data that allowed calculation of percentage accuracy (or means that could be converted to percentage) and standard deviation (SD).
Using the extracted mean and SD data, we calculated Hedge’s g; a measure of effect size equivalent to Cohen’s d but that includes a correction for small sample sizes (Hedges 1981). Analysis of the effect sizes was conducted using Comprehensive Meta-Analysis Software (Borenstein et al. 2005). Negative effect sizes indicate worse performance by the BPD group; each study was weighted by an estimation of the inverse variance. Depending on the negative emotion, either 4 (Disgust and Sadness) or 5 (Fear and Anger) studies contributed data, that included data from up to 92 participants with BPD, that met inclusion criteria (Dyck et al. 2009; Guitart-Masip et al. 2009; Lynch et al. 2006; Robin et al. 2012; Wagner and Linehan 1999). Both fixed and random effects analyses of effect sizes for each negative emotion were conducted.
Functional Amygdala Effect Size Estimation
For any functional magnetic resonance imaging study that reported amygdala response signal changes and between group comparisons, a quantitative estimate of the magnitude of this deficit was determined by computing a standardised effect size for each study using estimated Hedges g from the reported t or F-statistics with one numerator df.
Results
The search yielded 25 sources (Fig. 1). One or more individual sub-experiments within four manuscripts (Levine et al. 1997; Minzenberg et al. 2006a, b; Merkl et al. 2010; Preissler et al. 2010) were subsequently excluded for failing to meet inclusion criteria. Overall, 18 behavioural and 7 functional MRI studies were identified, of which 4 reported both data types. These were classified into three paradigm categories (1) basic emotion recognition and detection, (2) complex social emotional recognition (3) functional imaging data.
Basic Facial Emotion Recognition in BPD
Stimulus Sets and Presentation
Sixteen papers investigated basic facial emotion (FE) recognition in BPD (Table 1), many used the standard Ekman stimuli ‘Pictures of Facial Affect Series’ (POFA) (Ekman and Friesen 1976). These are black and white images of the whole face of male and female adult Caucasians with posed emotional expressions. The number of experimental trials varied between studies, which included up to six emotions–happy, sad, fear, anger, disgust and surprise. Fear and anger was presented in every study. One study Dyck et al. (2009) focused exclusively on neutral and negative emotions and employed the Fear, Anger, Neutral Test (FAN test) (Gur et al. 2002).
Eight of these studies investigated FE recognition to ambiguous facial emotional information by presenting neutral or mixed emotions, in which blends of two basic facial expressions were created by gradually morphing one emotion to another in 10 % stages (Calder 1996). Typically, static, full intensity images were used for the six basic emotions, but in five studies this was dynamic, the Ekman faces morphed from neutral to full expressive intensity within a single emotion (Blair et al. 2001). One combined visual (facial) and auditory (prosodic) emotional stimuli using the Bell-Lysaker Emotion Recognition Test (BLERT) (Bell et al. 1997), a 21-item videotaped presentation that, like the Ekman POFA, shows six different emotional states with participants required to identify the emotional label from a fixed options set. Two studies measured detection and recognition of happy and angry faces, one used stimuli from the Karolinska Directed Emotional Faces (KDEF) stimulus set (Lundqvist et al. 1998; Schulze et al. 2012), the other implemented a novel visual search task (Hagenhoff et al. 2013), in which incongruent emotions were presented in a crowd of neutral stimuli.
Ambiguous and Neutral FER
In participants with BPD, some of the most consistent deficits were in the recognition of neutral or ambiguous facial expressions. The data suggested a tendency for patients with BPD to inaccurately recognise or misclassify ambiguous facial expressions as negative (Domes et al. 2008; Dyck et al. 2009; Wagner and Linehan 1999). The studies suggested that this effect or bias may be influenced by heightened anxiety and negative affect (Domes et al. 2008), prior sexual abuse (Wagner and Linehan 1999) or response speed (Dyck et al. 2009). Six studies failed to find any significant differences in neutral facial expression recognition accuracy (Levine et al. 1997; Bland et al. 2004; Minzenberg et al. 2006a, b; Merkl et al. 2010; Mier et al. 2012; Hagenhoff et al. 2013).
Positive FER
Studies that presented happy faces at full intensity found no recognition differences between patients and healthy controls. At lower emotional intensity the results were more mixed with evidence of both heightened and reduced sensitivity compared to healthy controls (Lynch et al. 2006; Robin et al. 2012). Task type may have influenced the processing of positive expressions. Hagenhoff et al. (2013) reported that BPD patients take longer to detect happy faces compared to angry faces in a task that required implicit appraisal, but no differences were observed when a standard explicit emotion recognition task was used. Schulze et al. (2012) found that by increasing a tasks’ cognitive demands BPD patients demonstrated enhanced detection of happy faces.
Unoka et al. (2011) found surprise to be the only emotion rated more accurately in an inpatient BPD sample compared to controls while Domes et al. (2008) observed higher error rates in their BPD group, a significant proportion of who also had PTSD (44 %) and sexual abuse histories (64 %). Domes et al. (2011) replicated the latter finding in a similar cohort and noted a relationship between self-reported difficulty in mood identification and the detection threshold for surprised and fearful faces.
Integrated Facial and Prosodic Emotion Recognition
Minzenberg et al. (2006b) reported that when facial emotional expressions are presented with additional emotional speech prosodic information, recognition accuracy across basic emotions was impaired in BPD patients relative to controls; while either source in isolation led to no differences in accuracy or reaction time. This was interpreted to suggest that BPD patients were unable to meet the demands of the more cognitively challenging task.
Negative FER
In contrast to the negative bias to neutral stimuli reported above, several studies reported recognition deficits in people with BPD compared to healthy controls for a range of negative emotions (Bland et al. 2004; Levine et al. 1997; Unoka et al. 2011; Dyck et al. 2009) or for specific negative emotions (Lynch et al. 2006; Wagner and Linehan 1999). However two (Lynch et al. 2006; Wagner and Linehan 1999) reported enhanced sensitivity, especially to fear, with evidence also of a response bias to that emotion, where the sensitivity to fear was correlated to the severity of borderline symptoms (Merkl et al. 2010) and linked to childhood sexual abuse (Wagner and Linehan 1999).
Overall effect sizes and their confidence intervals indicated that there were no significant differences between patients with BPD and healthy controls for any of the four negative emotions tested (Table 2 and Fig. 2).
I 2 values for each emotion were examined using fixed effects models. I 2 represents the percentage of total variation across studies due to heterogeneity rather than chance. It suggested no observable heterogeneity for Sadness, though Anger, Fear and Disgust had moderate to high I 2 values (35.1 to 77.3) indicating a significant degree of inconsistency for those emotions.
Social Emotion Sensitivity in BPD
Of five studies that used the RMET to examine FER to social emotion cues (Table 3), two, one in inpatients (Preissler et al. 2010) and one in outpatients (Schilling et al. 2012), reported no differences between the BPD and HCs in response accuracy, though in the latter the BPD patients were more confident even when incorrect.
Three studies reported overall enhanced response accuracy in BPD patients compared to HCs, but in the context of subtle differences in the overall results patterns. One (Fertuck et al. 2009) reported greater accuracy in the BPD group compared to controls for total, neutral and positive eye gaze, though the significant differences for positive gaze were lost when depressive symptoms were taken into account. In fact, as with some of the basic FER studies above, depressive symptoms were significantly associated with enhanced mental state discrimination both overall and more specifically for negative affect.
Scott et al. (2011) reported enhanced social emotion recognition in high compared to low BPD trait healthy subjects. Accuracy was greatest for negative eye gazes, though this was in the context of a general negative response bias across the entire range of stimuli. Most recently Frick’s et al. (2012) behavioural data from an fMRI study found that the women with BPD had a significantly higher discrimination rate for both positive and negative eye gazes, independent of depressive symptoms.
Functional Neuroimaging of Facial Emotion Processing in BPD
Functional neuroimaging studies have used a variety of implicit (Donegan et al. 2003; Minzenberg et al. 2007; Cullen et al. 2011) and explicit (Guitart-Masip et al. 2009; Frick et al. 2012; Mier et al. 2012; Radaelli et al. 2012) emotional expression experimental paradigms and analytical methods to assess the underlying functional biology in BPD (Table 4). The majority tested for group differences in regional activation, often on the basis of hypothesis driven a priori regions of interest (ROI). One (Cullen et al. 2011) contrasted functional connectivity in BPD and control groups, measured as correlations in neural activity between two anatomically distinct brain areas.
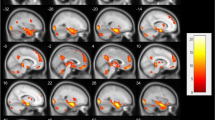
Across studies, patients with BPD exhibited increased activation in the right and left amygdala. Large effect sizes suggest the robustness of this finding in tasks that used both basic and complex social facial stimuli (Donegan et al. 2003; Mier et al. 2012; Frick et al. 2012; Minzenberg et al. 2007). Minzenberg et al. (2007) found heightened activation of the amygdala in response to fear (g = 0.68; 95 % CI = −0.14–1.5) in BPD participants relative to controls, a finding supported by Donegan et al. (2003) (g = 1.29; 95 % CI = 0.51–2.08). Donegan’s findings also suggested that there was aberrant amygdala responsiveness to neutral stimuli (g = 0.84; 95 % CI = 0.09–1.58).
Other regional differences in activation were also detected. Mier et al. (2012) reported reduced activation in the inferior frontal gyrus (IFG) and the superior temporal sulcus (STS), modulated by task complexity in the healthy controls but absent in BPD. Frick et al. (2012) reported reduced activation in the hippocampus, right superior temporal sulcus, left parietal lobe, and the posterior cingulate cortex (PCC) in response to positive eye gaze, though the right inferior frontal gyrus showed less activation during negative eye gazes. However others reported increases in the left middle and inferior temporal cortex to both positive and negative valence stimuli in the BPD group (Guitart-Masip et al. 2009). Further rostral and subgenual anterior cingulate cortex difference, increases to anger and decreases to fear, were found (Minzenberg et al. 2007).
Cullen et al. (2011) reported evidence of reduced functional connectivity between the amygdala and cingulate cortex in BPD compared to HC, while the results correlated with subjects’ hostility and anxiety levels. The BPD patients however showed enhanced connectivity between the amygdala and anterior cingulate to overt fear and to ‘masked’ fear greater connectivity between the right amygdala, caudate and thalamus bilaterally.
Finally only one study has tried to explore the link with affective disorders by comparing patients with BPD and bipolar I disorder, bipolar I disorder alone and healthy controls on a face matching paradigm (Radaelli et al. 2012). There were no amygdala differences between the groups but activation in the right anterior cingulate and hippocampus, and decreased activation in dorsolateral prefrontal cortex in patients with BPD and bipolar I compared to the controls.
Discussion
A number of conclusions can be drawn from this systematic review and meta-analysis of facial emotion processing studies in BPD.
Ambiguous or Neutral Stimuli Interpreted Negatively
First, there is considerable experimental evidence to support the conclusion that ambiguous or neutral facial expressions are more likely to be interpreted negatively by people with BPD. Beck has suggested that BPD may be underpinned by an underlying cognitive bias that others are dangerous and malevolent (Beck and Freeman 1990). This may manifest as a tendency to interpret ambiguous and neutral expressions in the context of hyper-vigilance with a negative bias (Arntz and Veen 2001; Baer et al. 2012). Besides the experimental importance, these findings have important implications for day-to-day social functioning in people with BPD as any cognitive bias to misperceive facial emotions as hostility or anger, could contribute to a cascade of negative attributions that compromise neutral social interactions in a predictable manner (Couture et al. 2006).
Many studies failed to incorporate neutral stimuli that would have allowed negative response biases to facial affect processing to be assessed more explicitly. Furthermore, as Dyck et al. (2009) have proposed, a time constraint may compromise performance in emotion recognition of ambiguous expressions (Dyck et al. 2009), possibly through increased cognitive difficulty, that exposes that bias more overtly. The relevance of this for patients in rapidly unfolding day to day social interactions is obvious (Dyck et al. 2009). Future investigation should introduce neutral stimuli and variable time limits to FE tasks to explore the basis of these observations.
Altered Perception of Negative Facial Emotions
No clear, robust and consistent pattern has emerged of BPD patients’ performance when interpreting negative facial expressions compared to healthy controls. While several individual studies identified impairments, their pattern remains elusive. Most often reported in individual studies was evidence for reduced accuracy and sensitivity recognising a range of negative emotions (Levine et al. 1997; Bland et al. 2004; Jovev et al. 2011; Unoka et al. 2011; Robin et al. 2012).
Any deficits in negative FER may be linked to the negative emotional and arousal states typically experienced by people with BPD (Gunderson 1984). This hypothesis is supported by two studies; in the first Levine et al. (1997) reported negative correlations between reduced recognition accuracy and intense emotional responses on an Affect Intensity Measure (Larsen and Diener 1987) and in the second Bland et al. (2004) noted an inverse association between negative emotion recognition accuracy and underlying negative affect. This interpretation is however at variance with the mood-congruency hypothesis in affective states that assimilates affect into an associative model of memory. It suggests that stimuli whose affective significance matches the person’s emotional state will provoke greater attention, faster perception and more elaborate processing (Bower 1981). Furthermore, in several other studies subjects with BPD, even those who were more depressed, performed better at negative facial expression recognition (Lynch et al. 2006), but that could be the result of a specific negative response bias in emotion recognition also seen in depression (Raes et al. 2006). An alternative explanation may be that it is the subjects’ with the greatest rates of childhood trauma and abuse (Bandelow et al. 2005; Lobbestael et al. 2009), that experience the greatest deficits in social cognitive function and the greatest impairments in negative emotion recognition, that is in part consistent with Bland et al. (2004) and Dyck et al. (2009).
It is also possible that methodological differences between the studies accounted for some of the differences in the response deficits seen. For example Wagner and Linehan (1999) used a free response format in contrast to all the other studies that used a forced choice strategy. Previous work has shown that participants will select a response label from a list, even if they would have failed to generate that same option under free-response conditions (Rosenberg and Ekman 1995).
Findings from the meta-analysis revealed non-significant effect sizes for all negative emotions. The heterogeneity data suggest that the datasets are simply too demographically and clinically diverse to allow any further integration of studies at this time.
From a narrative perspective the systematic data suggest that people with BPD are particularly sensitive to identify fear (Wagner and Linehan 1999; Merkl et al. 2010), notably those with severe sexual abuse histories or high PTSD symptoms, possibly through hyper-vigilance for negative stimuli (Sieswerda et al. 2007). This has led to one formulation of a cognitive model of BPD, where patients develop cognitive schemas underpinned by hyper-vigilance for negative environmental cues (Sieswerda et al. 2007). Wagner and Linehan (1999) also noted over attribution of fear in BPD compared to HC. Such a response bias, rather than greater accuracy was largely unaddressed in most studies. Use of signal detection theory would allow response accuracy to be teased apart from response bias in a manner that is essential to understand if there actually is a greater sensitivity to the detection and recognition of certain emotional cues (Tsoi et al. 2008).
A number of studies identified differences relating to disgust (Bland et al. 2004; Guitart-Masip et al. 2009; Jovev et al. 2011), as well a tendency to incorrectly attribute this emotion to other facial expressions (Unoka et al. 2011). New work is emerging that suggests that disgust may play a prominent role in BPD pathology, with elevated self-report rates and implicit ratings linking disgust to BPD even more closely than anxiety (Rusch et al. 2011). Future work should include and perhaps focus on that facial emotion in BPD.
Happy faces were recognized more accurately than angry, sad, or neutral faces (Hess et al. 1997; Ridout et al. 2003; D’Argembeau and Van der Linden 2007) in a manner consistent with a large body of work outside BPD. This is an important finding which suggest difficulties with facial emotion processing may vary across emotions. Two studies reported subtle differences to positive stimuli in BPD patients compared to HC using a dynamic experimental design (Lynch et al. 2006; Robin et al. 2012). Superior facial affect recognition (Lynch et al. 2006) was rare, and could have reflected a truly greater sensitivity in BPD though could have been accounted for by a more heterogeneous symptom severity (Lynch et al. 2006). The one report of reduced sensitivity to happy expressions may be linked to the use of a younger participant group (Robin et al. 2012).
Response Speed
There may be a complicated relationship between response time and accuracy, with for example more impulsive responses to happy faces in BPD (Jovev et al. 2011). The data for other emotions is very limited. For surprise (Domes et al. 2008, 2011) which was over attributed (Unoka et al. 2011), there could be an underlying emotional processing deficit (Du and Martinez 2011). That deficit has been linked to theory of mind deficits (Domes et al. 2011), that are also seen in other mental disorders including depression and obsessive–compulsive disorder-that are themselves linked to deficits in facial emotion recognition (Pedrosa Gil et al. 2009).
Integrating FER with Prosodic Information
The requirement to integrate multimodal emotional information compromised recognition further in BPD (Minzenberg et al. 2006a, b). This ability is essential for successful social communication (Lambrecht et al. 2012). These deficits were associated with greater interpersonal hostility, especially suspiciousness and assaultiveness and suggest that individual differences in higher order integration of emotional perceptions may be drivers of the interpersonal dysfunction seen clinically in BPD. This type of study may prove to be the most informative about how BPD patients process information and stimuli in complicated emotional and social situations.
Enhanced Emotion Detection
Schulze et al. (2012) suggests that patients with BPD may experience enhanced detection of emotional stimuli, especially for angry expressions. It may be that enhanced emotion detection is due to an attention bias towards certain emotional stimuli in BPD (Schulze et al. 2012), linked to cognitive distortions, or a frank impairment of attentional disengagement from negative emotional stimuli in BPD that may contribute to greater sensitivity and apparent recognition accuracy to those emotions (Von Ceumern-Lindenstjerna et al. 2009).
Enhanced Social Judgement ToM
On the basis of current evidence complex social judgements were not greatly compromised in patients with BPD. In fact, the patient groups were usually as accurate (Preissler et al. 2010; Schilling et al. 2012) if not better at detecting emotional cues in the mental state discrimination task when total accuracy scores were accounted for (Fertuck et al. 2009; Scott et al. 2011; Frick et al. 2012). These data support the BPD ‘paradox’ wherein those with BPD exhibit enhanced mental state discrimination abilities but impaired interpersonal relationship skills (Krohn 1974; Franzen et al. 2011), that together might contribute to social difficulties (Franzen et al. 2011).
The positive, negative and neutral subscales of the RMET however did lead to inconsistent results. Greater accuracy was reported variously for neutral and positive (Fertuck et al. 2009), positive/negative (Frick et al. 2012), and negative-only stimuli (Scott et al. 2011). The sole study that did not classify the stimuli by valence failed to detect any significant differences (Preissler et al. 2010). This suggests that there may be a genuine performance difference in BPD between the emotional valence cues, but that these need to be explored experimentally in greater detail, addressing issues also of impulsivity and overconfidence (Schilling et al. 2012), and paradigm and stimulus inconsistency (Fertuck et al. 2009; Scott et al. 2011; Schilling et al. 2012).
Degree of BPD Traits and Comorbidity
Participants with high BPD traits identified more negative mental states to RMET stimuli than those with low BPD traits (Scott et al. 2011), a finding consistent with data from basic ER emotion recognition paradigms (Wagner et al. 2009; Unoka et al. 2011). These data suggest that future studies should include and quantify degree of BPD related dysfunction, including nonclinical populations with BPD traits (Trull et al. 1997) as this would allow a dose response relationship to be explored.
The degree of co-morbidity, for example of depression, may also have a moderating effect on task performance, with higher levels associated with better RMET performance (Fertuck et al. 2009). When these were addressed statistically previously significant RMET performance differences fell away. Given the risk of co morbidity between mood disorders and BPD, and this evidence of enhanced performance (Harkness et al. 2005), future studies must adequately assess mood symptoms in subjects (Scott et al. 2011) and control for them in statistical models (Zimmerman and Mattia 1999; Bellino et al. 2005)
Functional Magnetic Resonance Imaging
The pathophysiology of borderline personality disorder is likely to be complex. It involves complex interacting pathways between cortical, subcortical and limbic nodes. Key nodes in this circuit are illustrated in the model (Fig. 3).
A hypothetical model of brain circuitry in FER in borderline personality disorder. The Fusiform Gyrus (FG) has object, including facial specific processing functions that are fed from the visual cortex. Disordered structural and functional connectivity between modulatory regions such as the ACC/BA25 (Anterior Cingulate Cortex/Broadmann Area 25) or prefrontal cortex (IFG-Inferior Frontal Gyrus) and the amygdala may contribute to disordered functional feedback that normally modulates amygdala processing of environmental stimuli. Abnormal amygdala processing of emotional cues contributes to disordered hippocampal and lateral temporal activity (M/STG Middle/Superior Temporal Gyrus), that is expressed as heightened sensitivity to emotional stimuli and psychotic like experiences in the context of the resulting heightened arousal (Lis et al. 2007; Meyer-Lindenberg and Weinberger 2006; O’Neill and Frodl 2012)
Functional neuroimaging has provided largely consistent evidence of abnormal neural activation in the amygdala, the Mirror Neuron System (MNS) including regions of the inferior frontal gyrus and the anterior cingulate cortex (ACC) during emotional processing tasks in BPD. Altered activity was also more sporadically reported in the hippocampus, temporal poles and cortices, dorsolateral prefrontal cortex and medial frontal gyrus, and somatosensory regions.
A role for increased amygdala activation during FEP in BPD extending across basic and social emotion processing emerged consistently across studies (Donegan et al. 2003; Frick et al. 2012; Mier et al. 2012; Minzenberg et al. 2007), large effect sizes were found to support this across the neuroimaging studies. The amygdala is postulated to have a central role in the appraisal of emotionally significant data, guiding social context decisions and behaviours (Baron-Cohen et al. 1994). As hypothesised (Domes et al. 2009) hyperactivity in BPD could interfere with, or be a marker of abnormal social cognitive processing, hyper vigilance and over-arousal (Donegan et al. 2003; Mier et al. 2012), as indexed by facial emotion processing tasks. Notably the exclusion of any Axis-I co-morbidity in one study (Guitart-Masip et al. 2009) may have been critical to the lack of significant difference between the BPD and control groups in the amygdala in that study. Amygdala hyperactivation has been linked to FEP deficits in for example depression (Peluso et al. 2009), bipolar disorder (Surguladze et al. 2010) and anxiety (Monk et al. 2008).
What remains less clear from these results is whether amygdala hyper-activation in BPD is generalised across emotional stimuli or is fine-tuned to some expressions, for example fear, in which large effect sizes were found (Minzenberg et al. 2007; Donegan et al. 2003). The nature of the emotional stimuli has been found to play a role in determining the amygdala response (Fusar-Poli et al. 2009; Radaelli et al. 2012), with heightened activity to aversive stimuli (Phillips et al. 2003; Dickstein and Leibenluft 2006). Indeed this may underpin, or reflect, pathological negative emotion processing in borderline personality disorder (McCloskey et al. 2005; Koenigsberg et al. 2009), in a manner quite consistent with the behavioural data (Wagner and Linehan 1999; Merkl et al. 2010). Furthermore, the large amygdala hyperactivation effect size to neutral facial stimuli (Donegan et al. 2003), may be part of the neural substrate supporting the BPD misattribution response bias, labelling negative emotions to ambiguous data. From a methodological perspective it may have been the limited choice of stimuli deployed in some studies that contributed to their failure to detect significant differences in neural activation underlying basic emotion recognition.
Cullen’s et al. (2011) report that patients with BPD developed greater connectivity between the amygdala and rostral anterior cingulate cortex (rACC) when fearful stimuli were explicitly presented, and with the right caudate and bilateral thalamus when automatically processed compared to controls, suggests disordered functional connectivity. Increasingly, cerebral pathology is conceptualised as being underpinned by aberrant anatomical or functional connections between nodes of neural networks, rather than discrete regional differences. Thus such a model may well play a role in functional differences underpinning symptoms in BPD. These differences may well involve distinct neural correlates based on conscious and unconscious emotion perception and processing.
Impaired fronto-limbic connectivity during emotionally neutral conditions in the same study could reflect altered baseline response to emotionally neutral stimuli, that in turn predispose the individual to comparative hyper-connectivity of the amygdala in the context of more emotionally charged stimuli (Cullen et al. 2011). Alternatively they may represent the neural substrate of the predisposed vulnerability to negatively appraise a neutral stimulus or face with a negative bias.
The anterior cingulate (ACC), as part of the rostral limbic system and involved in the response to emotional states, is also consistently implicated in disordered emotional processing in BPD, particularly in those studies which focussed on it using the region of interest approach (Minzenberg et al. 2007; Frick et al. 2012; Radaelli et al. 2012). Activity in the subgenual ACC seems implicated to the processing of negative facial emotions, although the nature of the ACC response is inconsistent. Some studies reported increases to broad negative emotions (Radaelli et al. 2012) and others decrease to fearful stimuli and the opposite to angry stimuli (Minzenberg et al. 2007). Sample characteristics may have introduced confounding factors with some studies including co-morbid Bipolar Disorder but others including only subjects free from axis I pathology and psychotropic medicines. However this evidence suggests that the proposed model of emotional dysregulation in BPD linked to reduced engagement of anterior brain regions still remain speculative (New et al. 2008; Mauchnik and Schmahl 2010).
While limbic hyperactivity may be relatively robust, the reverse has been reported in other brain regions. Most notably the inferior frontal gyrus, the superior temporal sulcus and gyrus and the insula (Frick et al. 2012; Mier et al. 2012). This part of the neural ‘network’ has been implicated in processes underpinning normal social cognition, including empathy, theory of mind, and facial processing (Gallese 2006; Pelphrey and Morris 2006; Enticott et al. 2008).
Findings suggest an overall deactivation in this network that is unaffected by task complexity in a manner that differs from healthy controls where hyperactivation is seen in response to increasing task difficulty (Mier et al. 2012). Furthermore, specifics of the experimental paradigms may play a key role in the nature of the response in the insula and superior temporal region that may be particularly sensitive to paradigms with more overt ToM components, such as the RMET (Frick et al. 2012; Dziobek et al. 2011). A pattern that is also seen in for example RMET tasks in autism (Baron-Cohen et al. 1999).
Limitations and Future Directions
Despite a considerable body of work particularly in the last 5 years (Domes et al. 2009), the precise nature of facial emotion processing deficits in BPD at both behavioural and neural levels remains elusive. Successful integration of the range of studies is undermined by the often modest sample sizes. Male subjects, while perhaps aetiologically and pathophysiologically distinct, remain largely unexplored. Medication and psychological treatment status is rarely considered, as is the influence of study setting, and the implications for illness severity and current phenomenology. While some studies matched well for potential confounders such as age, others considerations such as ethnicity or intelligence were largely unreported (Bland et al. 2004; Minzenberg et al. 2006a, b; Guitart-Masip et al. 2009; Wagner et al. 2009; Jovev et al. 2011). The specificity of any findings to BPD has also been questioned given the high rates of co-morbidity with for example PTSD and depressive disorders.
From the perspective of the experimental paradigms time limited stimuli and response windows, as well as fixed versus free choice formats, and the overrepresentation of negative emotional stimuli may also have contributed to the findings. Technological advances that have led a trend away from static stimuli towards dynamic, complex and more ecologically valid stimuli which tap into the sensitive detection of subtle, moment-to-moment changes in self and others’ affective states that could be fundamental to the nature of social interactions and the underlying deficits (Yoshikawa and Sato 2008).
Few studies included non-emotional facial or other control stimuli that would have allowed more robust conclusions about the nature of face and object perception in BPD and the identification of a response bias. Only three studies incorporated such a control and indeed two found no deficits (Robin et al.; Dyck et al. 2009)
Other methodological inconsistencies included the broad range of cognitive subtraction stimuli, from crosshairs (Donegan et al. 2003) to emotionally neutral but complex stimuli (Minzenberg et al. 2007; Frick et al. 2012), and passive versus active emotional recognition, that make the integration of functional results challenging. Future meta analysis should attempt to synthesise fMRI studies of facial emotion processing to help aid the understanding of the amygdalar involvement in BPD and to examine variables that may moderate the magnitude of between group differences in amygdala activation.
Investigating sources of heterogeneity will be a constructive step; however symptom severity, psychotropic medicines, current depression or PTSD rates, and histories of trauma are reported too infrequently to examine their potential moderator effects at present.
From the patient’s perspective, these results suggest that BPD is associated with altered emotional processing and recognition of emotions in others. A pattern of negative emotion appraisal and response bias is plausible. Future studies should address the methodological limitations highlighted in this review and include larger, better described samples, with both more ‘primitive and real social world paradigms. There is a need for us to get a better understanding of how these functional deficits impact on our patients’ everyday lived experiences. Studies encouragingly suggest that we will be able to describe the pathophysiological substrate of borderline personality disorder in time.
References
Adolphs, R., Gosselin, F., Buchanan, T. W., Tranel, D., Schyns, P., & Damasio, A. R. (2005). A mechanism for impaired fear recognition after amygdala damage. Nature, 433(7021), 68–72.
Aragonès, E., Salvador-Carulla, L., López-Muntaner, J., Ferrer, M., Piñol, J. L. (2012). Registered prevalence of borderline personality disorder in primary care databases. Gaceta Sanitaria, 27(2), 171–174.
Arntz, A., & Veen, G. (2001). Evaluations of others by borderline patients. Journal of Nervous and Mental Disease, 189(8), 513.
Baer, R. A., Peters, J. R., Eisenlohr-Moul, T. A., Geiger, P. J., & Sauer, S. E. (2012). Emotion-related cognitive processes in borderline personality disorder: a review of the empirical literature. Clinical Psychology Review, 32(5), 359–369.
Bandelow, B., Krause, J., Wedekind, D., Broocks, A., Hajak, G., & Rüther, E. (2005). Early traumatic life events, parental attitudes, family history, and birth risk factors in patients with borderline personality disorder and healthy controls. Psychiatry Research, 134(2), 169–179.
Baron-Cohen, S., Ring, H., Moriarty, J., Schmitz, B., Costa, D., & Ell, P. (1994). Recognition of mental state terms. Clinical findings in children with autism and a functional neuroimaging study of normal adults. The British Journal of Psychiatry, 165(5), 640–649.
Baron-Cohen, S., Jolliffe, T., Mortimore, C., & Robertson, M. (1997). Another advanced test of theory of mind: evidence from very high functioning adults with autism or Asperger syndrome. Journal of Child Psychology and Psychiatry, 38(7), 813–822.
Baron-Cohen, S., Ring, H. A., Wheelwright, S., Bullmore, E. T., Brammer, M. J., Simmons, A., et al. (1999). Social intelligence in the normal and autistic brain: an fMRI study. European Journal of Neuroscience, 11(6), 1891–1898.
Baron-Cohen, S., Wheelwright, S., Hill, J., Raste, Y., & Plumb, I. (2001). The “Reading the mind in the eyes” test revised version: a study with normal adults, and adults with asperger syndrome or high-functioning autism. Journal of Child Psychology and Psychiatry, 42(2), 241–251.
Beck, A. T., & Freeman, A. (1990). Cognitive therapy of personality disorders. New York: Guilford.
Bell, M., Bryson, G., & Lysaker, P. (1997). Positive and negative affect recognition in schizophrenia: a comparison with substance abuse and normal control subjects. Psychiatry Research, 73(1), 73–82.
Bellino, S., Patria, L., Paradiso, E., Di Lorenzo, R., Zanon, C., Zizza, M., et al. (2005). Major depression in patients with borderline personality disorder: a clinical investigation. Canadian Journal of Psychiatry, 50(4), 234–238.
Blair, R. J. R., Colledge, E., Murray, L., & Mitchell, D. (2001). A selective impairment in the processing of sad and fearful expressions in children with psychopathic tendencies. Journal of Abnormal Child Psychology, 29(6), 491–498.
Bland, A. R., Williams, C. A., Scharer, K., & Manning, S. (2004). Emotion processing in borderline personality disorders. Issues in Mental Health Nursing, 25(7), 655–672.
Borenstein, M., Hedges, L., Higgins, J., & Rothstein, H. (2005). Comprehensive meta-analysis version 2. Englewood: Biostat.
Bower, G. H. (1981). Mood and memory. American Psychologist, 36(2), 129.
Brodsky, B. S., Groves, S. A., Oquendo, M. A., Mann, J. J., & Stanley, B. (2006). Interpersonal precipitants and suicide attempts in borderline personality disorder. Suicide and Life-Threatening Behavior, 36(3), 313–322.
Calder, A. J. (1996). Facial emotion recognition after bilateral amygdala damage: differentially severe impairment of fear. Cognitive Neuropsychology, 13(5), 699–745.
Conklin, C. Z., Bradley, R., & Westen, D. (2006). Affect regulation in borderline personality disorder. Journal of Nervous and Mental Disease, 194(2), 69–77.
Couture, S. M., Penn, D. L., & Roberts, D. L. (2006). The functional significance of social cognition in schizophrenia: a review. Schizophrenia Bulletin, 32(1), 44–63.
Cullen, K. R., Vizueta, N., Thomas, K. M., Han, G. J., Lim, K. O., Camchong, J., et al. (2011). Amygdala functional connectivity in young women with borderline personality disorder. Brain Connectivity, 1(1), 61–71.
D’Argembeau, A., & Van der Linden, M. (2007). Facial expressions of emotion influence memory for facial identity in an automatic way. Emotion, 7(3), 507–515.
Derntl, B., Habel, U., Windischberger, C., Robinson, S., Kryspin-Exner, I., Gur, R. C., et al. (2009). General and specific responsiveness of the amygdala during explicit emotion recognition in females and males. BMC Neuroscience, 10(1), 91.
Dickstein, D. P., & Leibenluft, E. (2006). Emotion regulation in children and adolescents: boundaries between normalcy and bipolar disorder. Development and Psychopathology, 18(4), 1105–1131.
Domes, G., Czieschnek, D., Weidler, F., Berger, C., Fast, K., & Herpertz, S. C. (2008). Recognition of facial affect in borderline personality disorder. Journal of Personality Disorders, 22(2), 135–147.
Domes, G., Schulze, L., & Herpertz, S. C. (2009). Emotion recognition in borderline personality disorder-a review of the literature. Journal of Personality Disorders, 23(1), 6–19.
Domes, G., Grabe, H. J., Czieschnek, D., Heinrichs, M., & Herpertz, S. C. (2011). Alexithymic traits and facial emotion recognition in borderline personality disorder. Psychotherapy and Psychosomatics, 80(6), 383–385.
Donegan, N. H., Sanislow, C. A., Blumberg, H. P., Fulbright, R. K., Lacadie, C., Skudlarski, P., et al. (2003). Amygdala hyperreactivity in borderline personality disorder: implications for emotional dysregulation. Biological Psychiatry, 54(11), 1284–1293.
Du, S., & Martinez, A. M. (2011). The resolution of facial expressions of emotion. Journal of Vision, 11(13), 24.
Dyck, M., Habel, U., Slodczyk, J., Schlummer, J., Backes, V., Schneider, F., et al. (2009). Negative bias in fast emotion discrimination in borderline personality disorder. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences, 39(5), 865–874.
Dziobek, I., Preißler, S., Grozdanovic, Z., Heuser, I., Heekeren, H. R., & Roepke, S. (2011). Neuronal correlates of altered empathy and social cognition in borderline personality disorder. NeuroImage, 57(2), 539–548.
Ekman, P., & Friesen, W. (1976). Pictures of facial affect. Palo Alto: Consulting Psychologists Press.
Enticott, P. G., Johnston, P. J., Herring, S. E., Hoy, K. E., & Fitzgerald, P. B. (2008). Mirror neuron activation is associated with facial emotion processing. Neuropsychologia, 46(11), 2851–2854.
Fertuck, E., Jekal, A., Song, I., Wyman, B., Morris, M., Wilson, S., et al. (2009). Enhanced ‘Reading the Mind in the Eyes’ in borderline personality disorder compared to healthy controls. Psychological Medicine: A Journal of Research in Psychiatry and the Allied Sciences, 39(12), 1979–1988.
Franzen, N., Hagenhoff, M., Baer, N., Schmidt, A., Mier, D., Sammer, G., et al. (2011). Superior ‘theory of mind’ in borderline personality disorder: an analysis of interaction behavior in a virtual trust game. Psychiatry Research, 187(1–2), 224–233.
Frick, C., Lang, S., Kotchoubey, B., Sieswerda, S., Dinu-Biringer, R., Berger, M., et al. (2012). Hypersensitivity in borderline personality disorder during mindreading. PLoS ONE. doi:10.1371/journal.pone.0041650.
Fusar-Poli, P., Placentino, A., Carletti, F., Landi, P., Allen, P., Surguladze, S., et al. (2009). Functional atlas of emotional faces processing: a voxel-based meta-analysis of 105 functional magnetic resonance imaging studies. Journal of Psychiatry and Neuroscience, 34(6), 418–432.
Gallese, V. (2006). Intentional attunement: a neurophysiological perspective on social cognition and its disruption in autism. Brain Research, 1079(1), 15–24.
Grilo, C. M., McGlashan, T. H., Quinlan, D. M., Walker, M. L., Greenfeld, D., & Edell, W. S. (1998). Frequency of personality disorders in two age cohorts of psychiatric inpatients. American Journal of Psychiatry, 155(1), 140–142.
Guitart-Masip, M., Carlos Pascual, J., Carmona, S., Hoekzema, E., Berge, D., Perez, V., et al. (2009). Neural correlates of impaired emotional discrimination in borderline personality disorder: an fMRI study. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 33(8), 1537–1545.
Gunderson, J. G. (1984). Borderline personality disorder. Washington: American Psychiatric Association Press.
Gunderson, J. G., & Lyons-Ruth, K. (2008). BPD’s interpersonal hypersensitivity phenotype: a gene-environment-developmental model. Journal of Personality Disorders, 22(1), 22–41.
Gur, R. C., Sara, R., Hagendoorn, M., Marom, O., Hughett, P., Macy, L., et al. (2002). A method for obtaining 3-dimensional facial expressions and its standardization for use in neurocognitive studies. Journal of Neuroscience Methods, 115(2), 137–143.
Hagenhoff, M., Franzen, N., Gerster, L., Koppe, G., Sammer, G., Netter, P., et al. (2013). Reduced sensitivity to emotional facial expressions in borderline personality disorder: effects of emotional valence and intensity. Journal of Personality Disorders, 27(1), 19–35.
Harkness, K., Sabbagh, M., Jacobson, J., Chowdrey, N., & Chen, T. (2005). Enhanced accuracy of mental state decoding in dysphoric college students. Cognition & Emotion, 19(7), 999–1025.
Hedges, L. V. (1981). Distribution theory for Glass’s estimator of effect size and related estimators. Journal of Educational Statistics, 6(2), 107–128.
Hess, U., Blairy, S., & Kleck, R. E. (1997). The intensity of emotional facial expressions and decoding accuracy. Journal of Nonverbal Behavior, 21(4), 241–257.
Jovev, M., Chanen, A., Green, M., Cotton, S., Proffitt, T., Coltheart, M., et al. (2011). Emotional sensitivity in youth with borderline personality pathology. Psychiatry Research, 187(1–2), 234–240.
Koenigsberg, H. W., Siever, L. J., Lee, H., Pizzarello, S., New, A. S., Goodman, M., et al. (2009). Neural correlates of emotion processing in borderline personality disorder. Psychiatry Research: Neuroimaging, 172(3), 192–199.
Korzekwa, M. I., Dell, P. F., Links, P. S., Thabane, L., & Webb, S. P. (2008). Estimating the prevalence of borderline personality disorder in psychiatric outpatients using a two-phase procedure. Comprehensive Psychiatry, 49(4), 380–386.
Krohn, A. (1974). Borderline “empathy” and differentiation of object representations: a contribution to the psychology of object relations. International Journal of Psychoanalytic Psychotherapy, 3(2), 142.
Lambrecht, L., Kreifelts, B., & Wildgruber, D. (2012). Age-related decrease in recognition of emotional facial and prosodic expressions. Emotion, 12(3), 529–539.
Larsen, R. J., & Diener, E. (1987). Affect intensity as an individual difference characteristic: a review. Journal of Research in Personality, 21(1), 1–39.
Levine, D., Marziali, E., & Hood, J. (1997). Emotion processing in borderline personality disorders. Journal of Nervous and Mental Disease, 185(4), 240–246.
Linehan, M. M. (1993). Cognitive behavioral treatment of borderline personality disorder. New York: Guilford Press.
Lis, E., Greenfield, B., Henry, M., Guilé, J. M., & Dougherty, G. (2007). Neuroimaging and genetics of borderline personality disorder: a review. Journal of Psychiatry and Neuroscience, 32(3), 162.
Lobbestael, J., Arntz, A., Harkema-Schouten, P., & Bernstein, D. (2009). Development and psychometric evaluation of a new assessment method for childhood maltreatment experiences: the interview for traumatic events in childhood (ITEC). Child Abuse & Neglect, 33(8), 505–517.
Lundqvist, D., Flykt, A., & Öhman, A. (1998). The Karolinska directed emotional faces-KDEF (CD-ROM). Stockholm: Department of Clinical Neuroscience, Psychology section, Karolinska Institutet.
Lynch, T. R., Rosenthal, M. Z., Kosson, D. S., Cheavens, J. S., Lejuez, C. W., & Blair, R. J. R. (2006). Heightened sensitivity to facial expressions of emotion in borderline personality disorder. Emotion, 6(4), 647–655.
Marinangeli, M., Butti, G., Scinto, A., Di Cicco, L., Petruzzi, C., Daneluzzo, E., et al. (2000). Patterns of comorbidity among DSM-III-R personality disorders. Psychopathology, 33(2), 69–74.
Mauchnik, J., & Schmahl, C. (2010). The latest neuroimaging findings in borderline personality disorder. Current Psychiatry Reports, 12(1), 46–55.
McCloskey, M., Phan, K. L., & Coccaro, E. (2005). Neuroimaging and personality disorders. Current Psychiatry Reports, 7(1), 65–72.
Merkl, A., Ammelburg, N., Aust, S., Roepke, S., Reinecker, H., Trahms, L., et al. (2010). Processing of visual stimuli in borderline personality disorder: a combined behavioural and magnetoencephalographic study. International Journal of Psychophysiology, 78(3), 257–264.
Meyer-Lindenberg, A., & Weinberger, D. R. (2006). Intermediate phenotypes and genetic mechanisms of psychiatric disorders. Nature Reviews Neuroscience, 7(10), 818–827.
Mier, D., Lis, S., Esslinger, C., Sauer, C., Hagenhoff, M., Ulferts, J., et al. (2012). Neuronal correlates of social cognition in borderline personality disorder. Social Cognitive and Affective Neuroscience. doi:10.1093/scan/nss028.
Minzenberg, M. J., Poole, J. H., & Vinogradov, S. (2006a). Adult social attachment disturbance is related to childhood maltreatment and current symptoms in borderline personality disorder. Journal of Nervous and Mental Disease, 194(5), 341–348.
Minzenberg, M. J., Poole, J. H., & Vinogradov, S. (2006b). Social-emotion recognition in borderline personality disorder. Comprehensive Psychiatry, 47(6), 468–474.
Minzenberg, M. J., Fan, J., New, A. S., Tang, C. Y., & Siever, L. J. (2007). Fronto-limbic dysfunction in response to facial emotion in borderline personality disorder: an event-related fMRI study. Psychiatry Research: Neuroimaging, 155(3), 231–243.
Monk, C. S., Telzer, E. H., Mogg, K., Bradley, B. P., Mai, X., Louro, H. M., et al. (2008). Amygdala and ventrolateral prefrontal cortex activation to masked angry faces in children and adolescents with generalized anxiety disorder. Archives of General Psychiatry, 65(5), 568–576.
New, A. S., Goodman, M., Triebwasser, J., & Siever, L. J. (2008). Recent advances in the biological study of personality disorders. Psychiatric Clinics of North America, 31(3), 441–461.
O’Neill, A., & Frodl, T. (2012). Brain structure and function in borderline personality disorder. Brain Structure & Function, 217(4), 767–782.
Pedrosa Gil, F., Ridout, N., Kessler, H., Neuffer, M., Schoechlin, C., Traue, H. C., et al. (2009). Facial emotion recognition and alexithymia in adults with somatoform disorders. Depression and Anxiety. doi:10.1002/da.20456.
Pelphrey, K. A., & Morris, J. P. (2006). Brain mechanisms for interpreting the actions of others from biological-motion cues. Current Directions in Psychological Science, 15(3), 136–140.
Peluso, M. A. M., Glahn, D. C., Matsuo, K., Monkul, E. S., Najt, P., Zamarripa, F., et al. (2009). Amygdala hyperactivation in untreated depressed individuals. Psychiatry Research: Neuroimaging, 173(2), 158–161.
Phillips, M. L., Drevets, W. C., Rauch, S. L., & Lane, R. (2003). Neurobiology of emotion perception I: the neural basis of normal emotion perception. Biological Psychiatry, 54(5), 504–514.
Preissler, S., Dziobek, I., Ritter, K., Heekeren, H. R., & Roepke, S. (2010). Social cognition in borderline personality disorder: evidence for disturbed recognition of the emotions, thoughts, and intentions of others. Frontiers in Behavioral Neuroscience, 4, 182.
Putnam, K. M., & Silk, K. R. (2005). Emotion dysregulation and the development of borderline personality disorder. Development and Psychopathology, 17(4), 899–925.
Radaelli, D., Poletti, S., Dallaspezia, S., Colombo, C., Smeraldi, E., & Benedetti, F. (2012). Neural responses to emotional stimuli in comorbid borderline personality disorder and bipolar depression. Psychiatry Research, 203(1), 61–66.
Raes, F., Hermans, D., & Williams, J. M. (2006). Negative bias in the perception of others’ facial emotional expressions in major depression: the role of depressive rumination. Journal of Nervous and Mental Disease, 194(10), 796–799.
Ridout, N., Astell, A., Reid, I., Glen, T., & O’Carroll, R. (2003). Memory bias for emotional facial expressions in major depression. Cognition & Emotion, 17(1), 101–122.
Robin, M., Pham-Scottez, A., Curt, F., Dugre-Le Bigre, C., Speranza, M., Sapinho, D., et al. (2012). Decreased sensitivity to facial emotions in adolescents with borderline personality disorder. Psychiatry Research, 200(2–3), 417–421.
Rosenberg, E. L., & Ekman, P. (1995). Conceptual and methodological issues in the judgment of facial expressions of emotion. Motivation and Emotion, 19(2), 111–138.
Rusch, N., Schulz, D., Valerius, G., Steil, R., Bohus, M., & Schmahl, C. (2011). Disgust and implicit self-concept in women with borderline personality disorder and posttraumatic stress disorder. European Archives of Psychiatry and Clinical Neuroscience, 261(5), 369–376.
Sanislow, C. A., Grilo, C. M., Morey, L. C., Bender, D. S., Skodol, A. E., Gunderson, J. G., et al. (2002). Confirmatory factor analysis of DSM-IV criteria for borderline personality disorder: findings from the Collaborative Longitudinal Personality Disorders Study. American Journal of Psychiatry, 159(2), 284–290.
Schilling, L., Wingenfeld, K., Löwe, B., Moritz, S., Terfehr, K., Köther, U., et al. (2012). Normal mind-reading capacity but higher response confidence in borderline personality disorder patients. Psychiatry and Clinical Neurosciences, 66(4), 322–327.
Schulze, L., Domes, G., Köppen, D., & Herpertz, S. C. (2012). Enhanced detection of emotional facial expressions in borderline personality disorder. Psychopathology. doi:10.1159/000341730.
Scott, L. N., Levy, K. N., & Pincus, A. L. (2009). Adult attachment, personality traits, and borderline personality disorder features in young adults. Journal of Personality Disorders, 23(3), 258–280.
Scott, L. N., Levy, K. N., Adams, R. B., Jr., & Stevenson, M. T. (2011). Mental state decoding abilities in young adults with borderline personality disorder traits. Personality Disorders: Theory, Research, and Treatment, 2(2), 98–112.
Sieswerda, S., Arntz, A., Mertens, I., & Vertommen, S. (2007). Hypervigilance in patients with borderline personality disorder: specificity, automaticity, and predictors. Behaviour Research and Therapy, 45(5), 1011–1024.
Surguladze, S., Marshall, N., Schulze, K., Hall, M. H., Walshe, M., Bramon, E., et al. (2010). Exaggerated neural response to emotional faces in patients with bipolar disorder and their first-degree relatives. NeuroImage, 53(1), 58–64.
Trull, T. J., Useda, D., Conforti, K., & Doan, B. T. (1997). Borderline personality disorder features in nonclinical young adults: 2. Two-year outcome. Journal of Abnormal Psychology, 106(2), 307–314.
Tsoi, D. T., Lee, K. H., Khokhar, W. A., Mir, N. U., Swalli, J. S., Gee, K. A., et al. (2008). Is facial emotion recognition impairment in schizophrenia identical for different emotions? A signal detection analysis. Schizophrenia Research, 99(1–3), 263–269.
Unoka, Z., Fogd, D., Fuezy, M., & Csukly, G. (2011). Misreading the facial signs: specific impairments and error patterns in recognition of facial emotions with negative valence in borderline personality disorder. Psychiatry Research, 189(3), 419–425.
Von Ceumern-Lindenstjerna, I. A., Brunner, R., Parzer, P., Mundt, C., Fiedler, P., & Resch, F. (2009). Attentional bias in later stages of emotional information processing in female adolescents with borderline personality disorder. Psychopathology, 43(1), 25–32.
Wagner, A. W., & Linehan, M. M. (1999). Facial expression recognition ability among women with borderline personality disorder: implications for emotion regulation. Journal of Personality Disorders, 13(4), 329–344.
Wagner, S., Baskaya, Ö., Lieb, K., Dahmen, N., & Tadić, A. (2009). The 5-HTTLPR polymorphism modulates the association of serious life events (SLE) and impulsivity in patients with borderline personality disorder. Journal of Psychiatric Research, 43(13), 1067–1072.
Yoshikawa, S., & Sato, W. (2008). Dynamic facial expressions of emotion induce representational momentum. Cognitive, Affective, & Behavioral Neuroscience, 8(1), 25–31.
Zimmerman, M., & Mattia, J. I. (1999). Axis I diagnostic comorbidity and borderline personality disorder. Comprehensive Psychiatry, 40(4), 245–252.
Acknowledgments
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. St Andrew’s, a not-for-profit registered charity which provides psychiatric treatment, funds the St Andrew’s Academic Centre and its staff.
Conflict of Interest
The authors declare that no conflicts of interest are associated with the preparation of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mitchell, A.E., Dickens, G.L. & Picchioni, M.M. Facial Emotion Processing in Borderline Personality Disorder: A Systematic Review and Meta-Analysis. Neuropsychol Rev 24, 166–184 (2014). https://doi.org/10.1007/s11065-014-9254-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11065-014-9254-9