Abstract
Genipin, an aglycon of geniposide, has been reported to have anti-inflammatory effect. However, the anti-inflammatory activity of genipin on LPS-stimulated BV2 microglial cells has not been reported. In this study, we investigated the molecular mechanisms responsible for the anti-inflammatory activity of genipin both in vivo and in vitro. The levels of TNF-α, IL-1β, NO and PGE2 were detected by ELISA. The expression of Nrf2, HO-1, and NF-κB were detected by western blot analysis. In vivo, genipin significantly attenuated LPS-induced memory deficit in the Morris water maze and passive avoidance tasks. Genipin also inhibited LPS-induced TNF-α and IL-1β expression in brain tissues. In vitro, our results showed that genipin inhibited LPS-induced TNF-α, IL-1β, NO and PGE2 production in a concentration-dependent manner. Genipin also suppressed LPS-induced NF-κB activation. In addition, the expression of Nrf2 and HO-1 were up-regulated by treatment of genipin. Furthermore, the inhibition of genipin on inflammatory mediator production was attenuated by transfection with Nrf2 siRNA. In conclusion, genipin inhibited LPS-induced inflammatory response by activating Nrf2 signaling pathway in BV2 microglia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Microglia, a type of resident macrophage in the brain, has been reported to play critical roles in defensing against pathogens in the central nervous system [1]. Once stimulated by injury or infection, microglia secreted inflammatory mediators and inflammatory cytokines such as NO and PGE2, TNF-α, and IL-1β [2]. However, persistent activation of microglia may lead to various neuronal disorders, such as Alzheimer’s disease and Parkinson’s disease [3, 4]. Overproduction of these inflammatory mediators may lead to neuronal damage and death [5]. Previous studies showed that regulation of inflammatory mediators production could attenuate the severity of neurodegenerative diseases [6]. NF-κB, a critical signaling molecule in inflammation, has been reported to play critical roles in the regulation of inflammatory mediator production [7, 8]. A large body of evidences demonstrated that many natural products had the ability to inhibit NF-κB activation in LPS-stimulated BV2 microglia cells [9, 10].
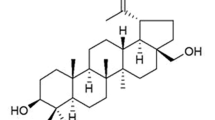
Genipin, an aglycon derived from geniposide, has been reported to have antioxidant and anti-inflammatory effects [11]. Studies showed that genipin could attenuate LPS-induced persistent changes of emotional behaviors and neural activation [12]. Genipin has been reported to inhibit LPS-induced apoptotic liver damage and sepsis in mice [13, 14]. Furthermore, genipin has been reported to inhibit inflammatory mediator production in rat brain microglial cells [15]. However, the anti-inflammatory mechanism of genipin on LPS-stimulated BV2 microglial cells has not been reported. The aim of this study was to investigate the anti-inflammatory effect and mechanism of genipin on LPS-stimulated BV2 microglial cells.
Materials and Methods
Materials
Genipin and LPS (Escherichia coli O55:B5) were purchased from Sigma (St. Louis, MO, USA). Griess reagent was obtained from Beyotime Institute of Biotechnology (Shanghai, China). Primary antibodies specific for Nrf2, HO-1, p65, p-p65, IκBα and p-IκBα were purchased from Cell Signaling Technology (San Francisco, CA, USA). Enzyme-linked immunosorbent assay (ELISA) kits of TNF-α, IL-1β, and PGE2 were purchased from R&D Systems (Minneapolis, MN, USA). All other reagents were of analytical grade.
Cell Culture
BV2 microglia cells were purchased from the Institute of Basic Medical Sciences of the China Science Academy. Cells were cultured in DMEM supplemented with 10% FBS, 100 U/mL penicillin, and 100 μg/mL streptomycin at 37 °C in a humidified incubator under 5% CO2.
Cell Viability Assay
BV2 microglia cells in log phase were seeded in 96 well plates. 12 h later, the cells were treated with different concentrations of genipin. 24 h later, 20 μL MTT (5 μg/mL) was added to each well and incubated for 4 h. Then the supernatants were removed and 200 μL DMSO was added to dissolve formazan crystals. Absorbance was determined at 570 nm.
Nitrite Measurement
BV2 cells were pretreated with genipin for 1 h and stimulated by LPS for 24 h. Then the culture supernatants were collected for measuring nitrite production by Griess reagent assay. The culture supernatants were mixed with an equal volume of Griess reagent and incubated at room temperature for 15 min. Absorbance at 540 nm of the reaction was monitored with a microplate reader.
ELISA Assays
BV2 cells were seeded in 24-well plate at a density of 1 × 105 cells/well and pretreated with different concentrations of genipin for 1 h. After stimulating by LPS for 24 h, the culture supernatants were collected. The levels of TNF-α, IL-1β, and PGE2 in the culture medium were detected by ELISA kits (R&D Systems, Minneapolis, MN) according to the manufacturer’s instruction.
Western Blot Analysis
Total cellular proteins of BV2 cells were extracted using a protein extraction kit according to the manufacturer’s instruction. Protein concentrations were determined by BCA protein assay kit. Proteins were electrophoresed on 10% SDS-polyacrylamide gel and transferred onto a PVDF membrane (Millipore, Bedford, MA). The membranes were blocked in 5% skim milk for 2 h and incubated with the specific primary antibodies (1:1000) for 2 h at room temperature. The membranes were incubated with horseradish peroxidase-conjugated secondary antibody for 2 h at room temperature. The proteins were visualized by enhanced chemiluminescence according to the manufacturer’s instructions.
Transient Transfection with siRNA
BV2 microglia cells were transfected with Nrf2 siRNA (100 nM) or control siRNA (100 nM) using the Lipofectamine 2000 transfection reagent (Thermo, USA). The siRNA sequence targeting NRF2 5′-CAU UGA UGU UUC UGA UCU ATT-3′ was designed and supplied by Qiagen. 36 h later, the cells were treated with genipin and LPS. 24 h later, the production of TNF-α, IL-1β, NO and PGE2 were detected. The inhibition of siRNA on Nrf2 expression was detected by western blot analysis.
In Vivo Experiments
Male ICR mice (2 months old) were provided by the Center of Experimental Animals of Harbin Medical University (Harbin, China). The mice were fed a standard diet. All animal procedures were performed in accordance with NIH guidelines for the care and use of laboratory animals. The animal study proposal was approved by the Institutional Animal Care and Use Committee (IACUC) of the Harbin Medical University with the permit number: SYXK(Hei)2011-022. Sixty mice were randomly divided into five groups: control group, LPS group, LPS + genipin (1, 2.5, 5 mg/kg). LPS was dissolved in sterile saline and injected intraperitoneally (0.25 mg/kg). Genipin was orally administered for 3 weeks prior to LPS injection. The mice were examined 3 day after LPS treatment. The profiles for spatial learning were recorded. The Morris water maze and passive avoidance tasks were based on previous study (Choi et al. 2012). The brain tissues were collected and the expression of TNF-α and IL-1β were detected by Western blot analysis.
Statistical Analysis
Data were presented as the mean ± SD of three independent experiments. Differences between mean values of the data were analyzed using one-way ANOVA and Tukey’s multiple comparison tests. Differences are considered to be significant when p < 0.05 or p < 0.01.
Results
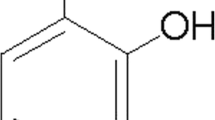
Genipin has No Cytotoxicity on BV2 Cells at Optimal Concentrations
An MTT assay was used to analyze the effect of genipin on BV2 cells viability. As shown in Fig. 1, the results showed that genipin had no cytotoxicity in the concentration range from 0 to 20 µM. Thus, genipin at the concentrations of 5, 10, 20 μM were used in the subsequent studies.
Effects of genipin on the cell viability of BV2 microglial cells. Cells were cultured with different concentrations of genipin (5, 10, 20 μM) in the absence or presence of 0.5 μg/mL LPS for 24 h. The cell viability was determined by MTT assay. The values presented are the means ± SD of three independent experiments
Genipin Attenuates LPS-Induced NO and PGE2 Production
The effects of genipin on LPS-induced inflammatory mediators NO and PGE2 production were detected in this study. Treatment of BV2 cells with LPS alone resulted in significant increases in NO and PGE2 production as compared to the control group. However, genipin concentration-dependently inhibited LPS-induced NO and PGE2 production (Fig. 2a).
a Effects of genipin on LPS-induced NO and PGE2 production. b Effects of genipin on LPS-induced TNF-α and IL-1ß production. The data presented are the means ± SD of three independent experiments and differences between mean values were assessed by one-way ANOVA and Tukey’s multiple comparison tests. # p < 0.05 vs. control group; *p < 0.05, **p < 0.01 vs. LPS group
Genipin Suppresses LPS-Induced TNF-α and IL-1ß Production
The effects of genipin on LPS-induced inflammatory cytokines TNF-α and IL-1ß production were detected in this study. Treatment of BV2 cells with LPS alone resulted in significant increases in TNF-α and IL-1ß production as compared to the control group. However, genipin concentration-dependently inhibited LPS-induced TNF-α and IL-1ß production (Fig. 2b).
Effects of Genipin on LPS-Induced NF-κB Activation
NF-κB has been reported to play vital roles in LPS-induced inflammatory mediator production. In this study, we investigated the effects of genipin on NF-κB activation in BV2 cells. As shown in Fig. 3, LPS stimulation significantly increased the phosphorylation of IκB-α and NF-κB p65. Pretreatment with genipin inhibited LPS-induced NF-κB activation in a concentration-dependent manner.
Genipin Up-Regulates the Expression of Nrf2 and HO-1
Studies showed that Nrf2/HO-1 signaling was involved in NF-κB activation and inflammatory mediator production. Thus, the effects of genipin on Nrf2 and HO-1 expression were detected in this study. The results showed that treatment of genipin augmented the expressions of Nrf2 and HO-1 induced by LPS (Fig. 4).
Genipin Exerts Anti-inflammatory Activity Through Activating Nrf2
To further investigate the anti-inflammatory mechanism of genipin, Nrf2 was knockdown by siRNA. As shown in Fig. 5a, Nrf2 was significantly inhibited by siRNA. Furthermore, the inhibition of genipin on TNF-α, IL-1ß, IL-6 and PGE2 production was reversed by Nrf2 knockdown (Fig. 5b).
a The inhibition of siRNA on Nrf2 expression. b Nrf2 knockdown reversed the anti-inflammatory effects of genipin. The values presented are the means ± SD of three independent experiments and differences between mean values were assessed by one-way ANOVA and Tukey’s multiple comparison tests. # p < 0.05 vs. control group; *p < 0.05, **p < 0.01 vs. LPS group
Genipin Attenuates LPS-Induced Memory Impairments
Compared with the control group, the escape distance and latency of LPS-treated group increased significantly. However, the increases were inhibited by treatment of genipin. Furthermore, the passive avoidance test were used to evaluate contextual memory of mice. The results showed LPS significantly decreased the step-through latency. However, treatment of genipin efficiently blocked the memory impairments (Fig. 6).
Genipin Inhibits LPS-Induced TNF-α and IL-1ß Expression in Brain Tissues
The expression of TNF-α and IL-1ß in brain tissues were detected in this study. As shown in Fig. 7, compared to the control group, the expression of TNF-α and IL-1ß increased significantly in LPS-treated group. However, the increases were dose-dependently inhibited by treatment of genipin.
Discussion
Previous studies indicated that natural compounds had the ability to treat neurological disorders by inhibition of microglial activation [16, 17]. Genipin has been reported to have anti-inflammatory effect. In the present study, we detected the anti-inflammatory effects of genipin on LPS-induced memory impairments and LPS-activated microglial cells. The results of this study showed that genipin significantly attenuated LPS-induced memory impairments in vivo. In vitro, genipin inhibited LPS-induced inflammatory mediator production by activating Nrf2/HO-1 signaling pathway. Genipin may be a therapeutic agent for neurological disorders.
Neuroinflammation has been reported to be caused by immune response to pathogens or damaged cells within the brain [18]. Microglia are the resident macrophage-like cells in the brain [19]. Stimulation of microglia by LPS, the main virulence factor of Gram-negative bacteria, could induce the production of inflammatory mediators [20]. Overproduction of these inflammatory mediators lead to common neuronal diseases [21]. Previous studies showed that NO, PGE2, TNF-α, and IL-1β levels increased in the cerebrospinal fluid of patients suffering from neurological diseases [22]. Controlling of these inflammatory mediators had the ability to attenuate the severity of neurodegenerative diseases [23]. In this study, we found that genipin remarkably suppressed LPS-induced inflammatory mediator production in BV2 microglial cells.
NF-κB, a critical signaling molecule, has been reported to play critical roles in the regulation of inflammatory mediators [24, 25]. Recent studies showed that stimulating of microglia cells with LPS could induce NF-κB activation, which subsequently induced the production of inflammatory mediators NO, PGE2, TNF-α, and IL-1β [26]. Because NF-κB activation is closely related to the production of inflammatory mediators, we investigated whether VA inhibited inflammatory mediators by modulating NF-κB activation. Our results showed that VA suppressed LPS-induced NF-κB activation in a concentration dependent manner. The transcription factor Nrf2 regulates the basal and inducible expression of numerous detoxifying and antioxidant genes, such as HO-1. Activating of Nrf2 could induce the expression of HO-1. Previous studies showed that Nrf2-null mice exhibited exacerbated brain inflammation in response to LPS. Activating Nrf2 could attenuate LPS-induced brain inflammation. These reports suggested that Nrf2 was a therapeutic target against brain inflammation. A large body of data suggests that activating of Nrf2 signaling pathway could inhibit LPS-induced inflammatory response in BV2 microglial cells. In the present study, we found that genipin concentration-dependently up-regulated the expression of Nrf2 and HO-1. Furthermore, the anti-inflammatory effects of genipin can be reversed by Nrf2 knockdown. Therefore, genipin may act through activating the Keap-Nrf2-ARE pathway, which subsequently up-regulated the expression of HO-1.
In summary, our results revealed that genipin activates Nrf2 signaling pathway, which lead to the inhibition of NF-κB activation and inflammatory mediators production in BV2 microglia cells. Genipin may be a therapeutic agent for the treatment of neurological diseases that associated with the overactivation of microglia.
References
Skaper SD, Facci L, Giusti P (2014) Neuroinflammation, microglia and mast cells in the pathophysiology of neurocognitive disorders: a review. CNS Neurol Disord Drug Targets 13:1654–1666
Kang CH, Choi YH, Moon SK, Kim WJ, Kim GY (2013) Quercetin inhibits lipopolysaccharide-induced nitric oxide production in BV2 microglial cells by suppressing the NF-kappaB pathway and activating the Nrf2-dependent HO-1 pathway. Int Immunopharmacol 17:808–813
Hirsch EC, Hunot S (2009) Neuroinflammation in Parkinson’s disease: a target for neuroprotection? Lancet Neurol 8:382–397
Rogers J, Mastroeni D, Leonard B, Joyce J, Grover A (2007) Neuroinflammation in Alzheimer’s disease and Parkinson’s disease: are microglia pathogenic in either disorder? Int Rev Neurobiol 82:235–246
Saliba E, Henrot A (2001) Inflammatory mediators and neonatal brain damage. Biol Neonat 79:224–227
Gao HM, Liu B, Zhang W, Hong JS (2003) Novel anti-inflammatory therapy for Parkinson’s disease. Trends Pharmacol Sci 24:395–401
Hsu CC, Lien JC, Chang CW, Chang CH, Kuo SC, Huang TF (2013) Yuwen02f1 suppresses LPS-induced endotoxemia and adjuvant-induced arthritis primarily through blockade of ROS formation, NFkB and MAPK activation. Biochem Pharmacol 85:385–395
Hirata Y, Masuda Y, Kakutani H, Higuchi T, Takada K, Ito A, Nakagawa Y, Ishii H (2008) Sp1 is an essential transcription factor for LPS-induced tissue factor expression in THP-1 monocytic cells, and nobiletin represses the expression through inhibition of NF-kappa B, AP-1, and Sp1 activation. Biochem Pharmacol 75:1504–1514
Im NK, Zhou W, Na M, Jeong GS (2014) Pierisformoside B exhibits neuroprotective and anti-inflammatory effects in murine hippocampal and microglial cells via the HO-1/Nrf2-mediated pathway. Int Immunopharmacol 24:353–360
Dilshara MG, Lee KT, Lee CM, Choi YH, Lee HJ, Choi IW, Kim GY (2015) New compound, 5-O-isoferuloyl-2-deoxy-D-ribono-gamma-lacton from Clematis mandshurica: anti-inflammatory effects in lipopolysaccharide-stimulated BV2 microglial cells. Int Immunopharmacol 24:14–23
Yu SX, Du CT, Chen W, Lei QQ, Li N, Qi S, Zhang XJ, Hu GQ, Deng XM, Han WY, Yang YJ (2015) Genipin inhibits NLRP3 and NLRC4 inflammasome activation via autophagy suppression. Sci Rep 5:17935
Araki R, Hiraki Y, Yabe T (2014) Genipin attenuates lipopolysaccharide-induced persistent changes of emotional behaviors and neural activation in the hypothalamic paraventricular nucleus and the central amygdala nucleus. Eur J Pharmacol 741:1–7
Kim TH, Yoon SJ, Lee SM (2012) Genipin attenuates sepsis by inhibiting Toll-like receptor signaling. Mol Med 18:455–465
Kim SJ, Kim JK, Lee DU, Kwak JH, Lee SM (2010) Genipin protects lipopolysaccharide-induced apoptotic liver damage in D-galactosamine-sensitized mice. Eur J Pharmacol 635:188–193
Nam KN, Choi YS, Jung HJ, Park GH, Park JM, Moon SK, Cho KH, Kang C, Kang I, Oh MS, Lee EH (2010) Genipin inhibits the inflammatory response of rat brain microglial cells. Int Immunopharmacol 10:493–499
Kim DC, Lee HS, Ko W, Lee DS, Sohn JH, Yim JH, Kim YC, Oh H (2014) Anti-inflammatory effect of methylpenicinoline from a marine isolate of Penicillium sp. (SF-5995): inhibition of NF-kappaB and MAPK pathways in lipopolysaccharide-induced RAW264.7 macrophages and BV2 microglia. Molecules 19:18073–18089
Zhu MD, Zhao LX, Wang XT, Gao YJ, Zhang ZJ (2014) Ligustilide inhibits microglia-mediated proinflammatory cytokines production and inflammatory pain. Brain Res Bull 109:54–60
Rivest S (2009) Regulation of innate immune responses in the brain. Nat Rev Immunol 9:429–439
Gehrmann J, Matsumoto Y, Kreutzberg GW (1995) Microglia: intrinsic immuneffector cell of the brain. Brain Res Rev 20:269–287
Dello Russo C, Lisi L, Tringali G, Navarra P (2009) Involvement of mTOR kinase in cytokine-dependent microglial activation and cell proliferation. Biochem Pharmacol 78:1242–1251
Elenkov IJ (2008) Neurohormonal-cytokine interactions: implications for inflammation, common human diseases and well-being. Neurochem Int 52:40–51
Yu SY, Zuo LJ, Wang F, Chen ZJ, Hu Y, Wang YJ, Wang XM, Zhang W (2014) Potential biomarkers relating pathological proteins, neuroinflammatory factors and free radicals in PD patients with cognitive impairment: a cross-sectional study. BMC Neurol 14:113
Perry VH (2010) Contribution of systemic inflammation to chronic neurodegeneration. Acta Neuropathol 120:277–286
Chuang YF, Yang HY, Ko TL, Hsu YF, Sheu JR, Ou G, Hsu MJ (2014) Valproic acid suppresses lipopolysaccharide-induced cyclooxygenase-2 expression via MKP-1 in murine brain microvascular endothelial cells. Biochem Pharmacol 88:372–383
Yang P, Han Y, Gui L, Sun J, Chen YL, Song R, Guo JZ, Xie YN, Lu D, Sun L (2013) Gastrodin attenuation of the inflammatory response in H9c2 cardiomyocytes involves inhibition of NF-kappaB and MAPKs activation via the phosphatidylinositol 3-kinase signaling. Biochem Pharmacol 85:1124–1133
Oh YT, Lee JY, Lee J, Lee JH, Kim JE, Ha J, Kang I (2010) Oleamide suppresses lipopolysaccharide-induced expression of iNOS and COX-2 through inhibition of NF-kappa B activation in BV2 murine microglial cells. Neurosci Lett 474:148–153
Acknowledgements
This work was supported by grants from First prize of China Postdoctoral Science Foundation; Doctoral Fund of The second affiliated to Harbin Medical University; Foundation for Returness of Ministry of Education of China. This Study was supported by the Grant from Heilongjiang returned overseas science fund project (No. LC2013C40), Chinese Postdoctoral Science Foundation (No. 2014M561373), and Heilongjiang Postdoctoral Science Foundation (No. LBH-Z14144).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Jianjiao Wang and Liang Chen have contributed equally to this article.
Rights and permissions
About this article
Cite this article
Wang, J., Chen, L., Liang, Z. et al. Genipin Inhibits LPS-Induced Inflammatory Response in BV2 Microglial Cells. Neurochem Res 42, 2769–2776 (2017). https://doi.org/10.1007/s11064-017-2289-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-017-2289-6