Abstract
Purpose
The goal of this article is to review the outcomes of insular glioma surgery and discuss strategies to minimize postoperative morbidity.
Methods
The authors reviewed the published literature on low- and high-grade insular gliomas with a focus on glioma biology, insular anatomy, and surgical technique.
Results
Maximal safe resection of insular gliomas is associated with improved survival and is the primary goal of surgery. Protecting patient speech and motor function during insular glioma resection requires versatile integration of insular anatomy, cortical mapping, and microsurgical technique. Both the transsylvian and transcortical corridors to the insula are associated with low morbidity profiles, but the transcortical approach with intraoperative mapping is more favorable for gliomas within the posterior insular region.
Conclusions
Surgical strategy for insular gliomas is dependent on biological, anatomical, and clinical factors. Technical mastery integrated with intraoperative technologies can optimize surgical results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gliomas within the insular region represent one of the most challenging problems in neurosurgical oncology. Tumor resection improves survival, but increasing extent of resection poses a risk of neurological compromise. Despite being surrounded by eloquent cortex and microvasculature, gliomas within the insula commonly invoke seizures, and patients often present with only mild focal deficits [1, 2]. Considering the risks associated with surgical resection, operative mastery is required to produce optimal clinical outcomes. The surgical strategy for insular gliomas has thus evolved with our understanding of glioma biology, subcortical white matter neuroanatomy, and advancements in microsurgical technique. In this article, the authors review the role of surgical resection for patients with low- and high-grade insular gliomas and discuss operative techniques to maximize extent of tumor resection.
Methods
The authors performed a literature search in PubMed for published reports on insular region anatomy, insular glioma resection techniques, and clinical outcomes following insular glioma resection from 1990 to 2019. Articles were selected for inclusion to address to the two main questions posed in this review: (1) how does insular region anatomy influence the morbidity of different surgical approaches to insular gliomas? and (2) how do brain mapping and other intraoperative technologies improve the surgical outcomes of insular glioma resection? An emphasis was placed on recent biological, anatomical, and clinical factors associated with optimized insular glioma resection outcomes.
Results
Goals of surgery
The effect of microsurgical resection on the natural history of gliomas is being revisited in the context of tumor genetics [3]. In low-grade glioma, early, aggressive resection has been associated with seizure freedom, decreased malignant transformation, and improved overall survival [4,5,6]. Recently, data suggests that this association between extent of resection (EOR), malignant transformation, and overall survival may not exist for 1p/19q co-deleted gliomas, which may be due to a more indolent and chemosensitive nature [7,8,9]. Similarly, in high-grade glioma, increasing EOR has been shown to improve overall survival, and an EOR threshold as low as 80% may provide a meaningful benefit in both newly diagnosed and recurrent tumors [10, 11]. Supratotal resection of up to 53% of the FLAIR abnormality beyond the enhancing tumor margin may provide an enhanced survival benefit [12, 13]. However, in a study of 335 patients with supratotal resection of high-grade gliomas, this survival benefit was only observed in patients with gliomas that carried an IDH-1 mutation [14].
Despite their unpredictable natural history, the association between EOR and survival has been observed in insular gliomas. In a study of 70 WHO Grade II insular gliomas, increasing EOR led to a stepwise improvement in overall survival [1]. A ≥ 90% EOR led to 100% 5-year survival, compared to 84% 5-year survival for EOR < 90%. Increasing EOR also predicted both radiographic and malignant PFS. In this same study, EOR was strongly associated with overall survival and radiographic PFS in 45 patients with WHO Grade III–IV insular gliomas. A ≥ 90% EOR led to 91% 2-year survival, compared to 75% 2-year survival for EOR < 90%. These findings were confirmed in a recent study of 255 consecutive transcortical resections of insular gliomas, in which EOR correlated with survival in both LGG (p = 0.001) and HGG (p = 0.008) [15]. Considering the survival benefit associated with insular glioma resection, maximal safe cytoreduction is the primary goal of surgical management.
Insular anatomy
Gross anatomy
The insula is a pyramid-shaped structure covered by the frontal, temporal, and parietal opercula within the depths of the Sylvian fissure. It is defined anatomically by the anterior, superior, and inferior peri-insular sulci [16]. The central insular sulcus divides the insula into anterior and posterior zones and is in line with the central sulcus of the cerebral hemispheres; the anterior insula is composed of three short gyri, while the posterior insula is composed of two long gyri [16,17,18,19]. The limen insulae is the anterior–inferior aspect of the insular cortical surface and conjoins the inferior insular point, anterior perforated substance, and temporal-mesial surface [20]. Basal ganglia structures including the internal capsule, putamen, external capsule, claustrum, and extreme capsule lie medial to the insula. The insula receives its blood supply from short M2 perforators, and venous drainage is superficial through the Sylvian venous network [16, 21].
Functional connectivity
The insula has been implicated in a wide variety of limbic, sensory, and cognitive modalities. Connections to the insula’s rostro-ventral allocortex include the amygdala, cingulate cortex, and orbitofrontal cortex, suggesting a role in emotional and olfactory function [16, 17, 22, 23]. The dorso-caudal neocortex is involved in sensory function, receiving a wide array of thalamic and cortical sensory afferents for gustatory, somatosensory, and vicerosensory relays [16]. Further, thalamic afferents for bodily sensations (hunger, pain, thirst, oxygenation) are organized topographically in the insular cortex, and patients with left-sided insular gliomas have been shown to have significantly greater heart rate variability compared to control patients, suggesting a role in autonomic sensory input integration [17, 22, 24]. Lastly, the disgranular zone of the insula is believed to contribute to cognitive function, such as attention, memory, and language processing [16]. It remains unknown whether patients with insular gliomas experience lasting neurological deficits as the result of tumors within these sensory afferent subcortical regions.
Surgical anatomy
The insula is surrounded by eloquent speech and motor pathways, as well as their microvascular supply. In the dominant hemisphere, the peri-Sylvian language network overlies the insular cortex superficially, while the uncincate fasciculus and inferior frontal occipital fasciculus extend through the insula’s deeper subcortical region [25]. Medial to the insula lies the basal ganglia and internal capsule, as well as the traversing lenticulostriate arteries. While short M2 perforators supply the insula and can be sacrificed, these must be differentiated from long M2 perforators, which travel past the insular region to the corona radiata to supply the descending corticospinal tract.
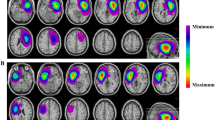
It is crucial for surgical approaches to the insula to respect the functional cortex, connectivity, and microvasculature of this region. The Berger-Sanai classification of insular gliomas was introduced with these anatomical considerations in mind [1]. The insula is divided into four zones, with the anterior–posterior border defined by a line bisecting the foramen of Monro, and the superior–inferior border defined by the Sylvian fissure (Fig. 1). This classification scheme allows for evaluation of insular gliomas in relation to their relevant functional anatomy, such as the peri-Sylvian language network (Zones I–III), the primary motor and sensory areas (Zone II), Heschl’s gyrus (Zone III), and the deep lenticulostriate arteries (Zone IV) [26]. The Berger-Sanai classification has been shown to predict both EOR and operative morbidity [2, 26].
Surgical approaches
Yasargil et al. [27], in 1992, classically described the transsylvian approach to 240 tumors of the limbic and paralimbic system. This landmark publication revitalized the notion that insular gliomas typically respect the anatomical boundaries of the limbic system and do not invade into the deep neocortical structures. Thus, despite earlier reports that tumors in this region were too difficult to resect, Yasargil achieved an excellent long-term morbidity rate of 5% following aggressive surgical treatment. Advancements in microsurgical technique and awake cortical mapping have continued to improve the safety of insular glioma resection in the current neurosurgical era. A recent meta-analysis of 890 insular glioma patients found the pooled incidences of new permanent motor and speech deficits following surgery to be 4% and 2%, respectively [28].
Transsylvian approach
A wide Sylvian fissure split is typically performed to obtain complete exposure of the insular region. Potts et al. [29] have recommend a two-part fissure split, divided into anterior and posterior segments. The anterior fissure split proceeds from distal to proximal, following cortical arteries to opercular arteries to the M2 segments at the base of the MCA bifurcation. This dissection exposes the anterior zone of the insula through several windows of MCA vessels. The posterior fissure split then proceeds from proximal to distal. This dissection becomes more difficult as the Sylvian cistern ends posteriorly and the frontal–temporal opercula become attached at their pial margins, as described in detail by Safaee et al. [30]. Due to constraints in space and surgical positioning, the posterior fissure split may require the assistance of fixed retraction or the sacrifice of superficial Sylvian veins (Fig. 2) [29, 31]. However, a key advantage of the transsylvian approach is the sparing of the frontal and temporal opercula in the dominant hemisphere, which minimizes the risk of direct surgical injury to the language network. In modern series, long-term neurological morbidity following the transsylvian approach for insular gliomas has ranged from 9 to 11% [2, 32].
Transcortical approach
The transcortical approach to the insula has gained popularity with the evolution of intraoperative mapping techniques. Awake language mapping is performed for dominant-sided insular gliomas, and subcortical motor mapping is performed at the medial plane of resection for identification of the internal capsule. For large gliomas, multiple cortical windows are made through non-functional cortex and connected at the level of the resection cavity, preserving the functional cortex and critical Sylvian vessels above [1, 26] (Fig. 3).
Typically, the incision and craniotomy are tailored to the size and location of the glioma. Dominant hemisphere cortical stimulation may yield both “positive” and “negative” sites of language function, but more focused exposures may only yield “negative” results. In an analysis of 250 patients who underwent awake resection of gliomas in the dominant hemisphere, 3094 of 3281 (94.3%) cortical stimulation sites were negative, and zero “positive” language sites were identified in 105 (42%) of their patients [33]. In patients with only “negative” results, glioma resection proceeded through the presumed non-functional cortex. Using this strategy of “negative mapping,” the 1-year rate of worsened language function remained very low (1.6%), demonstrating that focused exposures of the dominant hemisphere, even in the absence of identification of “positive” language sites, can permit most gliomas to be resected without language deficits. This technique followed the assumption that language pathways descend perpendicular to their cortical site of origin, and, thus, undercutting “negative” cortical sites was safe [33]. Subcortical language mapping techniques have evolved since that time, and experienced mapping surgeons have reported success with identification of important subcortical language tracts, such as the arcuate fasciculus and the inferior frontal occipital fasciculus [17, 34]. While there is risk of direct surgical injury to functional tissue with the transcortical approach, advancements in mapping techniques have led to low rates of neurological morbidity in recent series (3–9%) [1, 2, 26, 35, 36].
Discussion
Optimizing insular glioma surgery
Surgical approach
The transsylvian approach requires meticulous subarachnoid dissection and direct manipulation of critical vasculature. For larger exposures, it may also require opercular retraction, which can compress the M3 branches and lead to frontal lobe ischemia [31, 32]. Conversely, the transcortical approach includes frontal and/or temporal corticectomies, necessitating the expertise and adding the risks of direct cortical stimulation techniques. Traditionally, the choice of transsylvian versus transcortical corridors has been based on historical practice at individual institutions or anecdotal experiences of individual surgeons. Recently, clinical and cadaveric studies have used insular glioma anatomy to inform a neurosurgeon’s decision as to which approach is associated with the lowest rate of neurological morbidity [2, 26, 31].
A recent retrospective study comparing both approaches in 100 consecutive patients reported that surgeons were more likely to choose the transcortical approach over the transsylvian approach for larger gliomas (p = 0.02) and for gliomas located in Zone III (p < 0.01) [2]. Further, for tumors located in Zone II, the transcortical approach was associated with a significantly lower incidence of tissue ischemia on postoperative MRI scans (p = 0.02). It was hypothesized that this was the result of excessive retraction of the frontal opercula or sacrifice of Sylvian vessels in order to gain adequate access to Zone II gliomas (Fig. 2). These results correlated with an anatomical analysis in cadaveric subjects by Benet et al. [31] in which the transcortical approach was associated with more surgical freedom to the posterior zones of the insula (Zones II and III) than the transsylvian approach. Additionally, the transsylvian approach to the posterior insula often required frontal lobe retraction and sacrifice of Sylvian veins for complete exposure, which was deemed unsafe in 30% of their cadaveric subjects. Thus, while both techniques are associated with an acceptable morbidity profile, the transcortical approach appears to be favored over the transsylvian approach for larger gliomas with significant posterior extension, as it provides a direct view to this insular region, preserves surgeon comfort, and maximizes surgical exposure (Fig. 3).
Giant insular gliomas
Giant insular gliomas (all Zones) have been associated with increased neurological morbidity and decreased overall survival following resection [15, 26]. Giant gliomas are also more likely to extend into the putamen, and putamen involvement has been identified as an independent predictor of poor survival [37]. This may relate to an underlying difference in the molecular profile of these tumors. A recent study demonstrated differential expression of genes involved in cell proliferation, cell migration, and DNA repair in putamen-involved tumors compared to non-involved tumors, suggesting a more malignant natural history [38].
A combined approach utilizing the benefits of both the transsylvian and transcortical corridors has been advocated to yield optimal results for giant tumors [30, 39]. A transsylvian dissection is first performed to access and resect the anterior aspect of the tumor while sparing the overlying, uninvolved opercula. Intraoperative mapping of both motor and language function is then used to identify safe entry points to resect invasive areas of tumor. The transcortical approach, which maximizes surgeon comfort and surgical freedom to the posterior insula, is then utilized to resect the posterior aspect of the tumor. The medial border of the tumor is lastly dissected to the internal capsule with the aid of intraoperative navigation and subcortical motor mapping.
Protecting critical vasculature
For both surgical approaches, preservation of critical vasculature, including the M2 vessels, long M2 perforators, lenticulostriate arteries, and major Sylvian veins, is paramount. Cortical and subcortical ischemia following insular glioma resection is commonly seen on postoperative MRI scans—up to 23% of patients—and is a major source of neurological morbidity [2]. Identification of the lenticulostriate arteries intraoperatively can be particularly challenging because they travel directly through the substance of the brain and do not have a protective pial margin. Lang et al. [32] have suggested dissecting the M1 vessel to the most lateral lenticulostriate branch and then using its parasagittal plane as the most medial aspect of resection. Extensive dissection of the M1 and M2 vessels into their opercular branches can additionally help prevent inadvertent coagulation of normal vasculature, as well as aid in identification of long M2 perforators off of the posterior segments of the M2 vessels.
Complimentary technology
Functional MRI (fMRI) and diffusion tensor imaging (DTI) tractography are often employed to aid in safe insular glioma resection. fMRI can establish the dominant hemisphere preoperatively and serve as a starting point for identification of functional language cortex during direct cortical stimulation. However, fMRI has not been shown to be a suitable alternative to awake language mapping. A meta-analysis of nine studies assessing the correlation between language fMRI and direct cortical stimulation found a sensitivity ranging from 59 to 100% and specificity ranging from 0 to 97% [40]. The inconsistency in these results may be due to the influence of the pathological features of gliomas on fMRI, such as parenchymal invasion and angiogenesis. Gliomas can cause both biochemical and architectural changes in the local cerebral microenvironment, including alterations in neurotransmitter concentration and cortical reorganization of eloquent function [40, 41]. Similarly, DTI tractography is effective—but not completely reliable—in delineating the pathways of descending motor fibers. In a prospective cohort of 58 patients, the concordance rate of DTI tractography and pyramidal tract mapping had a sensitivity of 92.6% and specificity of 93.2%, with a distance between positive stimulation sites and imaged DTI tracts ranging from 2 to 14.7 mm [42].
Diffusion tensor imaging tractography can be used in combination with intraoperative navigation and subcortical motor mapping to identify the medial tumor plane. During the transsylvian approach, egress of CSF from a wide Sylvian fissure split can lead to brain relaxation, and, thus, negatively impact the accuracy of the navigation software. In such cases, intraoperative MRI may be an additional technology to employ [43]. Intraoperative MRI can help assess the degree of residual tumor at the medial border and allow for re-registering of the navigation software during late stages of the resection [44]. Fluorescence-guided surgery with 5-aminolevulinic acid (5-ALA) may also help delineate the tumor at the medial edge of dissection for high-grade lesions. Although the benefits of 5-ALA have not been investigated for insular location specifically, in a randomized trial of 322 patients undergoing resection of glioblastoma, fluorescence-guided resection with 5-ALA led to a higher rate of gross-total resection (65% vs. 36%; p < 0.0001) and improved PFS (41.0% vs. 21.1%, p = 0.0003) compared to resection with white light [45]. Because high-grade pathology is an independent predictor of neurological morbidity in insular glioma surgery, such techniques to maximize safe resection should be embraced [2, 46]. Complimentary technology may be particularly useful in the resection of recurrent insular gliomas, in which anatomical planes are further blurred by scar tissue and radiation-induced changes. Surgeon experience in combination with modern cortical mapping technology permits these tumors to be resected safely despite their anatomical and functional complexities [47].
Conclusions
Surgical strategy for insular gliomas is dependent on biological, anatomical, and clinical factors. Maximal safe resection to improve patient survival is the primary goal of surgery. Technical mastery integrated with intraoperative technologies can optimize surgical results. Collectively, a versatile skill set is required to treat this challenging group of tumors.
References
Sanai N, Polley MY, Berger MS (2010) Insular glioma resection: assessment of patient morbidity, survival, and tumor progression. J Neurosurg 112(1):1–9. https://doi.org/10.3171/2009.6.JNS0952
Przybylowski CJ, Baranoski JF, So VM, Wilson J, Sanai N (2019) Surgical morbidity of transsylvian versus transcortical approaches to insular gliomas. J Neurosurg. https://doi.org/10.3171/2018.12.JNS183075
Morshed RA, Young JS, Hervey-Jumper SL (2018) Sharpening the surgeon’s knife: value of extent of resection for glioma in molecular age. World Neurosurg 117:350–352. https://doi.org/10.1016/j.wneu.2018.06.149
Roelz R, Strohmaier D, Jabbarli R, Kraeutle R, Egger K, Coenen VA, Weyerbrock A, Reinacher PC (2016) Residual tumor volume as best outcome predictor in low grade glioma—a nine-years near-randomized survey of surgery vs. biopsy. Sci Rep 6:32286. https://doi.org/10.1038/srep32286
Ius T, Isola M, Budai R, Pauletto G, Tomasino B, Fadiga L, Skrap M (2012) Low-grade glioma surgery in eloquent areas: volumetric analysis of extent of resection and its impact on overall survival. A single-institution experience in 190 patients: clinical article. J Neurosurg 117(6):1039–1052. https://doi.org/10.3171/2012.8.JNS12393
Capelle L, Fontaine D, Mandonnet E, Taillandier L, Golmard JL, Bauchet L, Pallud J, Peruzzi P, Baron MH, Kujas M, Guyotat J, Guillevin R, Frenay M, Taillibert S, Colin P, Rigau V, Vandenbos F, Pinelli C, Duffau H, d'Etude des Glimoes FR (2013) Spontaneous and therapeutic prognostic factors in adult hemispheric World Health Organization Grade II gliomas: a series of 1097 cases: clinical article. J Neurosurg 118(6):1157–1168. https://doi.org/10.3171/2013.1.JNS121
Snyder LA, Wolf AB, Oppenlander ME, Bina R, Wilson JR, Ashby L, Brachman D, Coons SW, Spetzler RF, Sanai N (2014) The impact of extent of resection on malignant transformation of pure oligodendrogliomas. J Neurosurg 120(2):309–314. https://doi.org/10.3171/2013.10.JNS13368
Ding X, Wang Z, Chen D, Wang Y, Zhao Z, Sun C, Chen D, Tang C, Xiong J, Chen L, Yao Z, Liu Y, Wang X, Cahill DP, de Groot JF, Jiang T, Yao Y, Zhou L (2018) The prognostic value of maximal surgical resection is attenuated in oligodendroglioma subgroups of adult diffuse glioma: a multicenter retrospective study. J Neurooncol 140(3):591–603. https://doi.org/10.1007/s11060-018-2985-3
Alattar AA, Brandel MG, Hirshman BR, Dong X, Carroll KT, Ali MA, Carter BS, Chen CC (2018) Oligodendroglioma resection: a surveillance, epidemiology, and end results (SEER) analysis. J Neurosurg 128(4):1076–1083. https://doi.org/10.3171/2016.11.JNS161974
Sanai N, Polley MY, McDermott MW, Parsa AT, Berger MS (2011) An extent of resection threshold for newly diagnosed glioblastomas. J Neurosurg 115(1):3–8. https://doi.org/10.3171/2011.2.JNS10998
Oppenlander ME, Wolf AB, Snyder LA, Bina R, Wilson JR, Coons SW, Ashby LS, Brachman D, Nakaji P, Porter RW, Smith KA, Spetzler RF, Sanai N (2014) An extent of resection threshold for recurrent glioblastoma and its risk for neurological morbidity. J Neurosurg 120(4):846–853. https://doi.org/10.3171/2013.12.JNS13184
Fujii Y, Muragaki Y, Maruyama T, Nitta M, Saito T, Ikuta S, Iseki H, Hongo K, Kawamata T (2018) Threshold of the extent of resection for WHO Grade III gliomas: retrospective volumetric analysis of 122 cases using intraoperative MRI. J Neurosurg 129(1):1–9. https://doi.org/10.3171/2017.3.JNS162383
Li YM, Suki D, Hess K, Sawaya R (2016) The influence of maximum safe resection of glioblastoma on survival in 1229 patients: can we do better than gross-total resection? J Neurosurg 124(4):977–988. https://doi.org/10.3171/2015.5.JNS142087
Beiko J, Suki D, Hess KR, Fox BD, Cheung V, Cabral M, Shonka N, Gilbert MR, Sawaya R, Prabhu SS, Weinberg J, Lang FF, Aldape KD, Sulman EP, Rao G, McCutcheon IE, Cahill DP (2014) IDH1 mutant malignant astrocytomas are more amenable to surgical resection and have a survival benefit associated with maximal surgical resection. Neuro Oncol 16(1):81–91. https://doi.org/10.1093/neuonc/not159
Hameed NUF, Qiu T, Zhuang D, Lu J, Yu Z, Wu S, Wu B, Zhu F, Song Y, Chen H, Wu J (2018) Transcortical insular glioma resection: clinical outcome and predictors. J Neurosurg. https://doi.org/10.3171/2018.4.JNS18424
Michaud K, Duffau H (2016) Surgery of insular and paralimbic diffuse low-grade gliomas: technical considerations. J Neurooncol 130(2):289–298. https://doi.org/10.1007/s11060-016-2120-2
Hervey-Jumper SL, Berger MS (2019) Insular glioma surgery: an evolution of thought and practice. J Neurosurg 130(1):9–16. https://doi.org/10.3171/2018.10.JNS181519
Ture U, Yasargil DC, Al-Mefty O, Yasargil MG (1999) Topographic anatomy of the insular region. J Neurosurg 90(4):720–733. https://doi.org/10.3171/jns.1999.90.4.0720
Naidich TP, Kang E, Fatterpekar GM, Delman BN, Gultekin SH, Wolfe D, Ortiz O, Yousry I, Weismann M, Yousry TA (2004) The insula: anatomic study and MR imaging display at 1.5 T. AJNR Am J Neuroradiol 25(2):222–232
Guenot M, Isnard J, Sindou M (2004) Surgical anatomy of the insula. Adv Tech Stand Neurosurg 29:265–288
Tanriover N, Rhoton AL Jr, Kawashima M, Ulm AJ, Yasuda A (2004) Microsurgical anatomy of the insula and the sylvian fissure. J Neurosurg 100(5):891–922. https://doi.org/10.3171/jns.2004.100.5.0891
Maffei A, Haley M, Fontanini A (2012) Neural processing of gustatory information in insular circuits. Curr Opin Neurobiol 22(4):709–716. https://doi.org/10.1016/j.conb.2012.04.001
Augustine JR (1996) Circuitry and functional aspects of the insular lobe in primates including humans. Brain Res Brain Res Rev 22(3):229–244
Mishra A, John AP, Shukla D, Sathyaprabha TN, Devi BI (2018) Autonomic function in insular glioma: an exploratory study. World Neurosurg 118:e951–e955. https://doi.org/10.1016/j.wneu.2018.07.107
Herbet G, Moritz-Gasser S, Duffau H (2017) Direct evidence for the contributive role of the right inferior fronto-occipital fasciculus in non-verbal semantic cognition. Brain Struct Funct 222(4):1597–1610. https://doi.org/10.1007/s00429-016-1294-x
Hervey-Jumper SL, Li J, Osorio JA, Lau D, Molinaro AM, Benet A, Berger MS (2016) Surgical assessment of the insula. Part 2: validation of the Berger-Sanai zone classification system for predicting extent of glioma resection. J Neurosurg 124(2):482–488. https://doi.org/10.3171/2015.4.JNS1521
Yasargil MG, von Ammon K, Cavazos E, Doczi T, Reeves JD, Roth P (1992) Tumours of the limbic and paralimbic systems. Acta Neurochir 118(1–2):40–52. https://doi.org/10.1007/bf01400725
Lu VM, Goyal A, Quinones-Hinojosa A, Chaichana KL (2019) Updated incidence of neurological deficits following insular glioma resection: a systematic review and meta-analysis. Clin Neurol Neurosurg 177:20–26. https://doi.org/10.1016/j.clineuro.2018.12.013
Potts MB, Chang EF, Young WL, Lawton MT, Project UBAS (2012) Transsylvian-transinsular approaches to the insula and basal ganglia: operative techniques and results with vascular lesions. Neurosurgery 70(4):824–834. https://doi.org/10.1227/NEU.0b013e318236760d
Safaee MM, Englot DJ, Han SJ, Lawton MT, Berger MS (2016) The transsylvian approach for resection of insular gliomas: technical nuances of splitting the Sylvian fissure. J Neurooncol 130(2):283–287. https://doi.org/10.1007/s11060-016-2154-5
Benet A, Hervey-Jumper SL, Sanchez JJ, Lawton MT, Berger MS (2016) Surgical assessment of the insula. Part 1: surgical anatomy and morphometric analysis of the transsylvian and transcortical approaches to the insula. J Neurosurg 124(2):469–481. https://doi.org/10.3171/2014.12.JNS142182
Lang FF, Olansen NE, DeMonte F, Gokaslan ZL, Holland EC, Kalhorn C, Sawaya R (2001) Surgical resection of intrinsic insular tumors: complication avoidance. J Neurosurg 95(4):638–650. https://doi.org/10.3171/jns.2001.95.4.0638
Sanai N, Mirzadeh Z, Berger MS (2008) Functional outcome after language mapping for glioma resection. N Engl J Med 358(1):18–27. https://doi.org/10.1056/NEJMoa067819
Duffau H, Peggy Gatignol ST, Mandonnet E, Capelle L, Taillandier L (2008) Intraoperative subcortical stimulation mapping of language pathways in a consecutive series of 115 patients with Grade II glioma in the left dominant hemisphere. J Neurosurg 109(3):461–471. https://doi.org/10.3171/JNS/2008/109/9/0461
Di Carlo DT, Cagnazzo F, Anania Y, Duffau H, Benedetto N, Morganti R, Perrini P (2019) Post-operative morbidity ensuing surgery for insular gliomas: a systematic review and meta-analysis. Neurosurg Rev. https://doi.org/10.1007/s10143-019-01113-4
Mandonnet E (2019) Transopercular resection of IDH-mutated insular glioma: a critical appraisal of an initial experience. World Neurosurg. https://doi.org/10.1016/j.wneu.2019.08.071
Wang Y, Wang Y, Fan X, Li S, Liu X, Wang J, Jiang T (2017) Putamen involvement and survival outcomes in patients with insular low-grade gliomas. J Neurosurg 126(6):1788–1794. https://doi.org/10.3171/2016.5.JNS1685
Zhou C, Wang Y, Liu X, Liang Y, Fan Z, Jiang T, Wang Y, Wang L (2018) Molecular profiles for insular low-grade gliomas with putamen involvement. J Neurooncol 138(3):659–666. https://doi.org/10.1007/s11060-018-2837-1
Rey-Dios R, Cohen-Gadol AA (2013) Technical nuances for surgery of insular gliomas: lessons learned. Neurosurg Focus 34(2):E6. https://doi.org/10.3171/2012.12.FOCUS12342
Giussani C, Roux FE, Ojemann J, Sganzerla EP, Pirillo D, Papagno C (2010) Is preoperative functional magnetic resonance imaging reliable for language areas mapping in brain tumor surgery? Review of language functional magnetic resonance imaging and direct cortical stimulation correlation studies. Neurosurgery 66(1):113–120. https://doi.org/10.1227/01.NEU.0000360392.15450.C9
Duffau H (2005) Lessons from brain mapping in surgery for low-grade glioma: insights into associations between tumour and brain plasticity. Lancet Neurol 4(8):476–486. https://doi.org/10.1016/S1474-4422(05)70140-X
Zhu FP, Wu JS, Song YY, Yao CJ, Zhuang DX, Xu G, Tang WJ, Qin ZY, Mao Y, Zhou LF (2012) Clinical application of motor pathway mapping using diffusion tensor imaging tractography and intraoperative direct subcortical stimulation in cerebral glioma surgery: a prospective cohort study. Neurosurgery 71(6):1170–1183. https://doi.org/10.1227/NEU.0b013e318271bc61
Senft C, Bink A, Franz K, Vatter H, Gasser T, Seifert V (2011) Intraoperative MRI guidance and extent of resection in glioma surgery: a randomised, controlled trial. Lancet Oncol 12(11):997–1003. https://doi.org/10.1016/S1470-2045(11)70196-6
Scherer M, Jungk C, Younsi A, Kickingereder P, Muller S, Unterberg A (2016) Factors triggering an additional resection and determining residual tumor volume on intraoperative MRI: analysis from a prospective single-center registry of supratentorial gliomas. Neurosurg Focus 40(3):E4. https://doi.org/10.3171/2015.11.FOCUS15542
Stummer W, Pichlmeier U, Meinel T, Wiestler OD, Zanella F, Reulen HJ, Group AL-GS (2006) Fluorescence-guided surgery with 5-aminolevulinic acid for resection of malignant glioma: a randomised controlled multicentre phase III trial. Lancet Oncol 7(5):392–401. https://doi.org/10.1016/S1470-2045(06)70665-9
Schramm J, Aliashkevich AF (2008) Surgery for temporal mediobasal tumors: experience based on a series of 235 patients. Neurosurgery 62(6 Suppl 3):1272–1282. https://doi.org/10.1227/01.neu.0000333792.36715.29
Morshed RA, Young JS, Han SJ, Hervey-Jumper SL, Berger MS (2018) Perioperative outcomes following reoperation for recurrent insular gliomas. J Neurosurg. https://doi.org/10.3171/2018.4.JNS18375
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no potential conflicts of interest related to this manuscript.
Ethical approval
This is a review article. Thus, there were no human or animal subjects involved.
Informed consent
This is a review article. Thus, informed consent was not needed or required for the completion of this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Przybylowski, C.J., Hervey-Jumper, S.L. & Sanai, N. Surgical strategy for insular glioma. J Neurooncol 151, 491–497 (2021). https://doi.org/10.1007/s11060-020-03499-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03499-4