Abstract
Introduction
Gliomas are tumors of the central nervous system. Despite new classifications, they are still divided in low and high-grade gliomas, being the latter of greater malignancy. The degree of malignancy is directly related with the angiogenic activity in tumoral tissues. We measured VEGF concentrations and angiogenic capacity in cerebrospinal fluid (CSF) from patients with high and low-grade gliomas. The purpose of this study was to find a biomarker that contributes in the differential diagnosis and prognosis of gliomas.
Methods
CSF was obtained from 19 individuals: 8 with low-grade gliomas, 6 with high-grade gliomas and 5 controls. VEGF concentration in CSF was measured by ELISA and the angiogenic capacity was measured by chick chorioallantoic membrane (CAM) test.
Results
The VEGF concentration was higher in patients with high-grade gliomas, compared to patients with low-grade gliomas and controls (2860 pg/mL ± 975 vs. 182.6 ± 37.1 and 47.4 ± 0.4, respectively). On the other hand, CSF from patients with high-grade gliomas generated a higher microvascular density (MVD) than patients with low-grade gliomas and controls (13.23 ± 0.6 vessels/9000μm2 vs. 9.3 ± 0.3 and 7.92 ± 0.2, respectively). Interestingly, there was not statistical differences in both VEGF levels and angiogenic capacity in patients with low-grade gliomas and controls.
Conclusion
Together VEGF levels and angiogenic capacity in CSF can be used as a biological marker of gliomas malignancy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The most common primary brain tumors in adults are gliomas. They can appear anywhere in the CNS but they primarily develop from glial stem cells in the brain [1, 2]. This type of tumors has a growing importance given that each year about 300,000 new cases are diagnosed in the world, and they represent the second cause of cancer mortality in patients under 35 years in the United States [3, 4]. Moreover, high-grade gliomas represent 80.7% of CNS malignant tumors [5].
Gliomas are tumors that present the same histological features as normal glial cells. They comprehend a heterogeneous group of diseases, including astrocytic, oligodendrocytic, ependymomas and mixed gliomas [6]. They range from lesions with a circumscribed growth pattern (WHO grade I pilocytic astrocytoma, pleomorphic xanthoastrocytoma)—showing a frequent mutation of B-Raf (BRAF) -, to diffuse gliomas (WHO grade II, III, and IV). Traditionally, diffuse gliomas were divided into low-grade lesions (WHO Grade II Astrocytoma, Oligodendroglioma, or Oligoastrocytoma) and high-grade lesions (WHO grade III Anaplastic Astrocytoma, Anaplastic Oligodendroglioma, Anaplastic Oligoastrocytoma, and WHO Grade IV Glioblastoma), based on anaplasia, mitotic activity, microvascular proliferation and necrosis [7]. The most aggressive variant is Glioblastoma (GBM) and has a median survival of 16 months in patients with the currently available treatments [3].
The development of integrated genomic analysis and the discovery of the1p/19q codeletion, and the IDH 1 and 2, and H3K27M mutations, revolutionized the understanding of the disease, creating new molecular subtypes in the integrated histological-molecular 2016 WHO classification of gliomas [7]. The IDH1 and IDH2 mutations—both present in the majority of WHO grade II and III gliomas—defined a new subtype associated with a favorable prognosis. When these mutations were combined with the 1p/19q codeletion, as occurred in Oligodendrogliomas, they showed a better response to radiochemotherapy and were associated with a longer survival than diffuse gliomas, where these alterations have not been observed [8-11]. Therefore, the lower-grade glioma concept arises, including WHO grade II and grade III diffuse gliomas, and stratifies them according to their genetic profile [10]. Nevertheless, this new classification has not been massified in clinic, and classic WHO classification continues being the standard diagnosis [5].
In patients with low-grade gliomas, long-term following up is performed by serial MRI, as well as complementary radiotherapy in selected cases. In the case of GBM, the combination of radio and chemotherapy has shown significantly better results [12]. However, gliomas usually tend to increase their degree of malignancy over the time, and low-grade gliomas can become high-grade gliomas [13]. Despite aggressive surgery, radiotherapy and chemotherapy, high-grade gliomas remain being lethal. For progressing, these tumors stimulate the formation of new blood vessels through the process known as angiogenesis, driven mainly by vascular endothelial growth factor (VEGF) [14]. Therefore, glioma malignancy is directly related to its vascularization level. Angiogenic level of a tumor is a predictor of progression, recurrence and metastatic dissemination, which has been demonstrated in several studies of different types of cancer, where VEGF levels were significantly high [15-23].
The monitoring of the angiogenic potential of brain tumors is not simple and requires invasive procedures such as brain biopsies [24]. Moreover, pathological diagnoses based on biopsies may not be accurate due to tumor heterogeneity, vascularization, cellularity and necrosis, and serial biopsies are frequently required [25]. The reduction, recurrence or progression of a glioma responding to therapy is evaluated by serial MRI, but this technique is not capable to distinguish these tumors from the so-called pseudoprogression (MRI pattern that resembles tumor progression without clinical deterioration) [25, 26]. As a result of this, several genomic and epigenomic features have emerged as diagnostic, prognostic and predictor biomarkers of tumor classification and risk stratification, such as the isocytrate dehydrogenase (IDH) mutation, the 1p/19q codeletion, and the O6-methylguanine-DNA-methyltransferase (MGMT) methylation [27]. Nevertheless, more available and cost-effective biomarkers are needed. In this context, numerous potentially diagnostic and prognostic biomarkers have been proposed, including VEGF, its soluble receptor sVEGFR1, basic fibroblast growth factor (bFGF), platelet derived growth factor (PDGF) and angiopoietin 2 (Ang2), all of which can be measured in blood or CSF. These biomarkers would allow developing a better tumor classification, to inform probable prognoses, and to facilitate patient management for elaborating a personalized treatment strategy [13, 28].
The aim of this pilot study is to contribute to the knowledge of tumor angiogenesis in low-grade and high-grade gliomas, by determining VEGF levels in CSF and angiogenic capacity of CSF from patients with high and low-grade gliomas.
Materials and methods
Subjects and collection of samples
The study was approved by the Ethic Committee of Hospital Clínico Universidad de Chile. An informed consent was obtained from participants before the enrollment. CSF samples were obtained from a total of 19 individuals, all without previous antiangiogenic treatment: 14 patients with gliomas, from which 8 has a low-grade gliomas (3 oligodendrogliomas II, 2 pilocytic astrocytoma, 1 subependymoma, 1 gemistocytic astrocytoma, 1 ependymoma) and 6 has a high-grade gliomas (5 glioblastoma, 1 anaplastic astrocytoma), and 5 control adults. Control CSF samples were obtained from joint injury hospitalized patients before spinal anesthesia. Approximately 2 mL of CSF were extracted from each individual by non-traumatic lumbar puncture. Samples were aliquoted and stored at -80° C until analysis.
Determination of VEGF concentration in CSF
VEGF in CSF samples was quantified by ELISA, using the commercial kit Quantikine® Human VEGF Immunoassay (R & D systems, Minn, USA). Briefly, a microtiter plate pre-coated with a monoclonal antibody specific for human VEGF was incubated with 100 µL of CSF sample. Bound VEGF was detected using a second polyclonal antibody for human VEGF conjugated with peroxidase and then, the correspondent substrate. Absorbance was measured at 450 nm. This ELISA kit detects the human isoforms VEGF165 and VEGF121. The lowest detection limit was 31 pg/mL. All samples were tested by triplicated and the intra-assay variation coefficient was 5.5%.
Determination of the angiogenic effect of CSF
The procedure was performed in White Leghorn breed embryonated chicken as described by Sinning et al. [24]. 70 eggs of embryonated chicken were incubated in a chamber at 37°C. 48 h after, an air chamber was drilled to extract approximately 2 ml of albumin egg with a Pasteur pipette. Eggs were disinfected with an iodized alcohol solution and holes were covered with adhesive tape. Maintaining the same incubation position, a window of 2.5 cm wide and 2 cm high was performed at the dorsal level under sterile conditions, to expose the chicken chorioallantoic membrane (CAM).
After 8 days, a methylcellulose filter impregnated with 10 µL CSF sample was placed on each egg CAM to measure the angiogenic effect of CSF components. Each control or glioma patient sample was tested in quintuplicate. 48 h post incubation, CAMs were removed by surgical procedure, and fixed in a buffered 10% formalin solution. All 5 CAMs treated with CSF from the same patient were processed in the same histological block under conventional histological procedures, and serial sections of 5µm thick were stained with Alcian blue and Hematoxylin–eosin for histological study. Using an optical microscope with × 100 magnification, blood vessels (capillaries) were counted in five fields per membrane (each field corresponds to 9000 μm2), which gives 25 fields for each control or glioma patient treated with CSF. For each CSF sample, mean and standard error of the blood vessel count were calculated. Angiogenic effect of the CSF sample was expressed as microvascular density (number of vessels present in 9000 µm2) of CAM and the procedure was performed by blind counting.
Statistical analysis
The VEGF concentration and the number of vessels per area were expressed as mean ± SEM. Normal, high-grade and low-grade groups were analyzed by one-way ANOVA with Bonferroni Multiple Comparison test, using the Graph Pad Prism 5 software. Difference was considered significant when p < 0.05.
Results
VEGF concentration in CSF
The VEGF concentration in CSF obtained from high-grade glioma patients was higher than that measured in low-grade glioma patients or control individuals (p = 0.003). Additionally, the VEGF concentration in CSF obtained from low-grade glioma patients presented a great variation between samples, being 3 of them similar to controls and 5 of them about 5 times higher than controls. VEGF levels of control individuals were all similar (Fig. 1, Table 1).
Distribution of VEGF concentration in CSF from different study groups. HG patients with high-grade gliomas; LG patients with low-grade gliomas; Control healthy individuals; ns not significant; ** p = 0.003. VEGF levels were quantified by ELISA. See material and methods for details
Angiogenic capacity of CSF measured by CAM assay
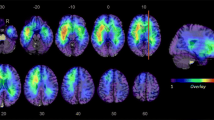
Angiogenic capacity, expressed as microvascular density (MVD) of the CSF of high-grade glioma patients, was higher than that observed in low-grade glioma patients or control individuals (p < 0. 0001 in both comparisons). There was no difference between low-grade glioma patients and control individuals (Fig. 2, Table 1).
Microvascular density (MVD), amount of blood vessels in 9000μm2 in CAM treated with CSF from different study groups. HG: group instilled with CSF obtained from patients with high-grade gliomas; LG: group instilled with CSF obtained from patients with low-grade gliomas; Control: group instilled with CSF obtained from healthy individuals. *** p < 0.0001. ns not significant. See material and methods for details
Individual values of VEGF concentration and microvascular density after CSF treatment are summarized in Table 1.
Discussion
In the present study, we found that VEGF concentration in CSF from patients with high-grade glioma is higher than that measured in low-grade glioma patients or control individuals. Accordingly, the angiogenic capacity of the CSF measured in a chick CAM model was also higher in patients with high-grade gliomas, compared to patients with low-grade glioma or control individuals. Our data provide evidence that supports the use of these parameters as biological markers of glioblastomas. In addition, CSF samples are relatively easier to obtain compared to biopsies and can be obtained serially to following-up each patient case.
In our study, VEGF levels in CSF were increased almost 50-times compared to control values in 4 of the 6 patients with high-grade glioma. These results are in agreement with the metanalysis reported by Chen et al. [29] that observed a correlation in the overexpression of VEGF with the pathological grade of gliomas, and with the observed by Sampath et al. [30], that reported higher VEGF concentrations in CSF from patients with high-grade astrocytomas compared to patients with non-astrocytic tumors.
We observed that VEGF concentration in CSF from some low-grade patients was higher than controls, although not significant. Sampath et al. [30] and Ribom et al. [31] did not detect VEGF in CSF from low-grade glioma patients or control individuals. We observed low but detectable levels of VEGF in CSF from control individuals, using the same commercial kit that both authors used, although Sampath reported their results in a different unit of measurement than ours, so results are not comparable.
It is difficult to propose a biological marker for the detection of low and high-grade gliomas that would be easy to obtain and that deliver reliable results. Tumor growth is associated with local vascularization and for this reason VEGF levels have being studied in fluids such as blood and CSF. Nowacka et al. [32] reported that serum VEGFA values in patients with CNS tumors, are higher than in individuals without tumors. However, the concentration of VEGF in blood can be influenced by different factors so their levels do not reflect exclusively tissue production; Handzhiev et al. [33] analyzed concentration of VEGF and observed that low-grade gliomas have higher VEGF levels than high-grade gliomas, both in pre- and postoperative collection from plasma. In the CNS, VEGF is released directly to the CSF so its concentration in this fluid is a reliable indicator.
Peles et al. [34] analyzed VEGF in both CSF and serum from patients with high and low-grade gliomas. They found differences in the VEGF concentration obtained from CSF but not in that obtained from serum, both in the two types of gliomas. Ribom studied VEGF levels in both fluids from patients with low-grade gliomas and the median of VEGF in serum from low-grade patients was 166.5 pg/mL, while in CSF they did not find detectable values. Serum VEGF was tested as a high grade glioma marker but without positive results when compared with control individuals [35]. Given the enormous variability of VEGF concentration, both in blood and CSF, obtained by different authors, it is necessary to consider another quantification tool of angiogenesis to discriminate between high and low-grade gliomas. It could be possible that, in some tumors, another factor besides VEGF may mediate tissular angiogenesis. To explore this idea, we combined the study of the quantity of angiogenic molecules with the determination of the biological activity in CSF.
By measuring the biological activity of CSF in a CAM bioassay, we observed a higher angiogenic capacity in eggs treated with CSF from high-grade glioma patients, compared to low- grade glioma patients and control individuals. Very few studies have evaluated the angiogenic capacity of CSF from patients with tumors. We previously reported that patients with high-grade gliomas have greater angiogenic capacity than individuals without tumors [24]. Now, using the same assay, we extended the study including low-grade glioma patients and we conclude that this increased capacity is seen only in high-grade gliomas. Given that in our results there were two discordant cases, future studies should consider a correlation between VEGF levels, tumor malignancy and the biological activity of each evaluated patient.
It is important to consider the potential relationship that exists between VEGF levels and angiogenic capacity in CSF. Although we did not study the vascularity of tumors from the patients, we did determine the angiogenic capacity of CSF from these patients using a CAM bioassay. This bioassay allowed checking the presence of some factors that could regulate the formation of blood vessels, as reported by Dai et al. [36] and Sinning et al. [24]. Our purpose was to investigate if some factors in CSF could also act on tumor tissue. The findings of Peles et al. [34] support our idea because they observed a correlation between VEGF or FGF-B levels in CSF and tumor vascularity in patients with astrocytic tumors.
An accurate diagnosis of cerebral tumors led to the determination of an appropriated clinical treatment. However, in some cases, biopsies are too difficult or risky procedures due to the location of the tumor. Efforts have been done to find biological markers for cerebral tumors, which can be obtained and measured in an easy way for guiding the diagnosis, prognosis and serve as a predictor of the efficiency of treatment. Tumoral development is associated with tissue vascularization, and then, it could be expected that angiogenic stimulators could be enhanced in CSF. Therefore, considering both factors, high levels of VEGF and angiogenic capacity in CSF could be together markers of high-grade gliomas, supporting the diagnosis with a procedure less aggressive than a biopsy, and considering that VEGF levels may vary depending on tumor progression or response to treatment; however limited by the fact that some treatments could be interfere with the results.
Conclusion
VEGF levels in CSF and angiogenic capacity could together serve as a progression marker and glioma vascularization, being useful in the diagnosis and clinical evaluation of tumor progression. Future studies should focus on the measurement of these markers in other neoplastic and non-neoplastic diseases involving the CNS. In addition, more studies that correlate the levels of these markers with the outcome of patients and the response to treatment are needed. Thus, the measurement of the pro-angiogenic potential of CSF in gliomas could have important implications in clinical practice, because it would allow to determine the malignancy of tumors and to establish when a low-grade glioma becomes a high-grade glioma. Additionally, it would allow to perform postoperative following-up of patients, evaluate response to therapies, including antiangiogenic complementary therapies, through less expensive and invasive methods that could be implemented routinely.
References
Louis DN (2006) Molecular pathology of malignant gliomas. Annu Rev Pathol Mech Dis 1:97–117
Ostrom QT, Bauchet L, Davis FG, Deltour I, Fisher JL, Langer CE et al (2014) The epidemiology of glioma in adults: a state of the science review. Neuro Oncol 16:896–913
Albert NL, Weller M, Suchorska B, Galldiks N, Soffietti R, Kim MM et al (2016) Response assessment in neuro-oncology working group and european association for neuro-oncology recommendations for the clinical use of PET imaging in gliomas. Neuro Oncol 18:1199–1208
Bray F, Ferlay J, Soerjomataram I et al (2018) Global Cancer Statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Ostrom QT, Gittleman H, Liao P, Vecchione-koval T, Wolinsky Y, Kruchko C et al (2017) Neuro-Oncology CBTRUS statistical report : primary brain and other central nervous system tumors diagnosed in the United States in 2010–2014. Neuro Oncol 19:1–88
Schwartzbaum JA, Fisher JL, Aldape KD, Wrensch M (2006) Epidemiology and molecular pathology of glioma. Nat Clin Pract Neurol 2:494–503
Louis DN, Perry A, Reifenberger G, Von Deimling A, Figarella D, Webster B et al (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131:803–820
Buckner JC, Shaw EG, Pugh SL, Chakravarti A, Gilbert MR, Barger GR et al (2016) Radiation plus procarbazine, CCNU, and vincristine in low-grade glioma. N Engl J Med 374:1344–1355
Cairncross JG, Wang M, Jenkins RB, Shaw EG, Giannini C, Brachman DG et al (2014) Benefit from procarbazine, lomustine, and vincristine in oligodendroglial tumors is associated with mutation of IDH. J Clin Oncol 32:783–790
Cancer Genome Atlas Research Network (2015) comprehensive, integrative genomic analysis of diffuse lower-grade gliomas. N Engl J Med. 372:2481–2498
Van den Bent MJ, Brandes AA, Taphoorn MJ, Kros JM, Kouwenhoven MC, Delattre JY et al (2013) Adjuvant procarbazine, lomustine, and vincristine chemotherapy in newly diagnosed anaplastic oligodendroglioma: long-term follow-up of EORTC Brain Tumor Group Study 26951. J Clin Oncol 31:344–350
Hottinger AF, Hegi ME, Baumert BG (2016) Current management of low-grade gliomas. Curr Opin Neurol 29:782–788
Kros JM, Mustafa DM, Dekker LJM, Smitt PAES, Luider TM, Zheng P (2015) Circulating glioma biomarkers. Neuro Oncol 17:343–360
Jain RK, Di Tomaso E, Duda DG, Loeffler JS, Sorensen AG, Batchelor TT (2007) Angiogenesis in brain tumours. Nat Rev Neurosci 8:610–622
Li H, Takayama K, Wang S, Shiraishi Y, Gotanda K, Harada T et al (2014) Addition of bevacizumab enhances antitumor activity of erlotinib against non-small cell lung cancer xenografts depending on VEGF expression. Cancer Chemoth Pharm 74(6):1297–1305
Plate K, Breier G, Weich H, Risau W (1992) Vascular endothelial growth factor is a potential tumour angiogenesis factor in human gliomas in vivo. Nature 359:845–848
Nowacka A, Smuczyński W, Rość D, Woźniak-Dąbrowska K, Śniegocki M (2018) Serum VEGF-A concentrations in patients with central nervous system (CNS) tumors. PLoS ONE 13(3):e0192395
Karayiannakis AJ, Syrigos KN, Polychronidis A, Zbar A, Kouraklis G, Simopoulos C, Karatzas G (2002) Circulating VEGF levels in the serum of gastric cancer patients: correlation with pathological variables, patient survival, and tumor surgery. Ann Surg 236(1):37–42
Zang J, Li C, Zhao L, Shi M, Zhou YC, Wang JH et al (2013) Prognostic value of vascular endothelial growth factor in patients with head and neck cancer: a meta-analysis. Head Neck 35(10):1507–1514
Luo H, Li J, Yang T, Wang J (2009) Expression and significance of VEGF-C and VEGF-D in differentiated thyroid carcinoma. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 23(12):531–534
Srabovic N, Mujagic Z, Mujanovic-Mustedanagic J, Softic A, Muminovic Z, Rifatbegovic A et al (2013) Vascular endothelial growth factor receptor-1 expression in breast cancer and its correlation to vascular endothelial growth factor A. Int J Breast Cancer 2013:746–749
Blank S, Deck C, Dreikhausen L, Weichert W, Giese N, Falk C et al (2015) Angiogenic and growth factors in gastric cancer. J Surg Res 194(2):420–429
Vonmarschall Z, Cramer T, Hocker M, Burde R, Plath T, Schirner M et al (2000) De novo expression of vascular endothelial growth factor in human pancreatic cancer: evidence for an autocrine mitogenic loop. Gastroenterology 119(5):1358–1372
Sinning M, Letelier R, Rosas C, Fuenzalida M, Lemus D (2012) Angiogenic potential of the cerebrospinal fluid (CSF) of patients with high-grade gliomas measured with the chick embryo chorioallantoic membrane assay (CAM). Biol Res 45:135–138
Hochberg FH, Atai NA, Gonda D, Hughes MS, Mawejje B, Balaj L et al (2014) Glioma diagnostics and biomarkers: an ongoing challenge in the field of medicine and science. Expert Rev Mol Diagn 14:439–452
Kruser TJ, Mehta MP, Robins HI (2013) Pseudoprogression after glioma therapy: a comprehensive review. Expert Rev Neurother 13:389–403
Cohen AL, Colman H (2015) Glioma Biology and Molecular Markers. In: Raizer J, Parsa A (eds) Current understanding and treatment of gliomas. Cancer treatment and research. Springer, Cham, 163 pp 15–30.
Szopa W, Burley TA, Kramer-Marek G, Kaspera W (2017) Diagnostic and Therapeutic Biomarkers in Glioblastoma: Current Status and Future Perspectives. Biomed Res Int. https://doi.org/10.1155/2017/8013575
Chen W, He D, Li Z, Zhang X, Pan D, Chen G (2015) Overexpression of vascular endothelial growth factor indicates poor outcomes of glioma: a systemaic review and meta-analysis. Int J Clin Exp Med 8(6):8709–8719
Sampath P, Weaver CE, Sungarian A, Cortez S, Alderson L, Stopa EG (2004) Cerebrospinal fluid vascular endothelial growth factor and serologic (recoverin) tumor markers for malignant glioma. Cancer Control 11:174–180
Ribom D, Larsson A, Pietras K, Smits A (2003) Growth factor analysis of low-grade glioma CSF: PDGF and VEGF are not detectable. Neurol Sci 24:70–73
Nowacka A, Smuczynski W, Rosc D, Wozniak-Dabrowska K, Sniegocki M (2018) Serum VEGF-A concentrations in patients with central nervous system (CNS) tumors. PLoS ONE 13:e0192395
Handzhiev D, Kiuchukov G, Enchev Y, Avramov T, Georgiev R, Varbanova S (2015) Plasma expression of vascular endothelial growth factor (VEGF) and basic fibroblast growth factor (BFGF) in patients with brain tumors. J IMAB 21:805–809
Peles E, Lidar Z, Simon AJ, Grossman R, Nass D, Ram Z (2004) Angiogenic factors in the cerebrospinal fluid of patients with astrocytic brain tumors. Neurosurgery 55:562–567
Hands JR, Abel P, Ashton K, Dawson T, Davis C, Lea RW, McIntosh AJS, Baker MJ (2013) Investigating the rapid diagnosis of gliomas from serum samples using infrared spectroscopy and cytokine and angiogenesis factors. Anal Bioanal Chem 405:7347–7355
Dai X, Yan J, Fu X, Pan Q, Sun D, Su Y et al (2017) Aspirin inhibits cancer metastasis and angiogenesis via targeting heparanase. Clin Cancer Res 23:6267–6278
Funding
This study was funded by”Iniciación” I08/08–2 of the “Vicerrectoría de Investigación y Desarrollo” of the Universidad de Chile and the grant “Temas Libres” 324/08 of the “Oficina de apoyo a la investigación” of the Hospital Clínico de la Universidad de Chile.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All applicable international, national and/or institutional guidelines for the care and use of animals were followed. All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vera, S., Sinning, M., Vergara, M. et al. Cerebrospinal fluid VEGF levels and angiogenic capacity as potential prognostic markers in patients with gliomas: a pilot study. J Neurooncol 145, 233–239 (2019). https://doi.org/10.1007/s11060-019-03314-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-019-03314-9