Abstract
Glioblastoma stands out as the most frequent central nervous system neoplasia, presenting a poor prognosis. The aim of this study was to verify the frequency and clinical significance of the aneuploidy of chromosomes 7 and 10, EGFR amplification, PTEN and TP53 deletions and 1p/19q deficiency in adult patients diagnosed with glioblastoma. The sample consisted of 40 patients treated from November 2011 to March 2015 at two major neurosurgery services from Southern Brazil. Molecular cytogenetic analyses of the tumor were performed through fluorescent in situ hybridization (FISH). The clinical features evaluated consisted of age, sex, tumor location, clinical symptoms, family history of cancer, type of resection and survival. The mean age of the patients was 59.3 years (ranged from 41 to 83). Most of them were males (70%). The median survival was 145 days. Chromosome 10 monosomy was detected in 52.5% of the patients, chromosome 7 polysomy in 50%, EGFR amplification in 42.5%, PTEN deletion in 35%, TP53 deletion in 22.5%, 1p deletion in 5% and 19q deletion in 7.5%. Age was shown to be a prognostic factor, and patients with lower age presented higher survival (p = 0.042). TP53 and PTEN deletions had a negative impact on survival (p = 0.011 and p = 0.037, respectively). Our data suggest that TP53 and PTEN deletions may be associated with a poorer prognosis. These findings may have importance over prognosis determination and choice of the therapy to be administered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma is the most common and more lethal central nervous system (CNS) tumor [1]. It occurs in glial cells, more specifically in astrocytes, and it is an extremely heterogeneous entity, presenting a predominance of poorly differentiated, pleomorphic, fusiform or rounded cells [2, 3]. Glioblastoma has an annual incidence of 3–5 cases/100,000 individuals and, despite the different therapeutic modalities available, such as neurosurgery, chemotherapy and radiotherapy, its prognosis remains poor, with a median survival of 15 months [4]. In the USA, the estimates for 2015 and 2016 were, respectively, 11,890 and 12,120 new glioblastoma cases [5].
In the past years, several cytogenetic and molecular changes, which may contribute to the diagnosis as well as the assessment of prognosis and response to treatment, have been identified. This diversity should be considered in the design of the therapy to be offered to patients, thus selecting more specific treatments for a particular pattern of tumor genetic alterations [6]. This is already done in some types of tumors, such as some kinds of leukemia, where cytogenetic changes have been part of clinical treatment protocols for many years [7].
Thus, our aim was to verify the frequency and clinical significance of aneuploidies of chromosomes 7 and 10, EGFR amplification, PTEN and TP53 gene deletion and 1p/19q deficiency in a sample of adult patients with glioblastoma.
Materials and methods
Sample
The sample consisted of 40 patients diagnosed with glioblastoma treated at the Neurosurgery Service of the Beneficência Portuguesa Hospital and at the Neurosurgery Service of the Hospital Cristo Redentor/Grupo Hospitalar Conceição (GHC) during the period from November 2011 to March 2015. Two pathologists evaluated the cases and confirmed the diagnosis of glioblastoma following the WHO criteria (2007) [3]. For each patient, a research protocol was filled out, containing clinical information and results of complementary tests. These included data such as age, sex, tumor location, clinical symptoms, family history of cancer, type of resection and survival.
For purposes of statistical analysis, patients were subdivided into two age groups (patients >50 years and <50 years) [8]. The anatomical location was defined as “frontal,” “parietal,” “temporal” or “other” and the extent of resection was classified as “subtotal” (10–90% resected) or “total” (more than 90% resected) [9]. We classified the clinical symptoms in five distinct groups: focal disturbance, decreased consciousness, intracranial hypertension (including headache, nausea and vomits), behavioral changes and seizures.
Cytogenetic molecular analysis
The molecular cytogenetic analysis was performed through fluorescence in situ hybridization (FISH) technique. For this, 4-μm sections of paraffin blocks from each case were used, using the LSI EGFR/CEP 7, LSI PTEN/CEP 10, LSI 1p36/LSI 1q25 and LSI 19q13/19p13 Dual C and LSI p53 probes—17p13.1 and CEP17 (Vysis, Abbott Laboratories, Abbott Park, IL, USA). For each probe, the manufacturer's protocol was followed. Only samples with >90% of the nuclei with signals were evaluated. For each case, 200 intact interphase nuclei were analyzed for the presence of the respective hybridization signals of the used probes.
For results interpretation, the following criteria were adopted: EGFR amplification when more than 10% of the nuclei exhibited EGFR/CEP7 > 2; polysomy of chromosome 7 when more than 20% of the nuclei showed 3 or more signals for CEP7, and monosomy of chromosome 10 when only one CEP10 signal was found in >50% of the nuclei [10]. Deletions of the PTEN gene were reckoned when PTEN/CEP10 < 0.8 [11]. The codeletion of 1p/19q was considered when 1p36/1q25 and 19q13/19p13 was <0.86 [12], and TP53 deletion when at least 8% of the nuclei exhibited one red signal and ≥2 green signals [2].
Statistical analysis
The quantitative variables were described in the form of mean and standard deviation, and the categorical variables, through absolute and relative frequencies. For categorical data, chi-square tests with Yates correction and Fisher's exact test were used. To evaluate survival, the Kaplan–Meier method was applied and the curves were compared with the use of the log-rank test. The effect measure used was the hazard ratio (HR) in conjunction with a confidence interval of 95%. The significance level adopted was 5% (p < 0.05) and analyzes were performed in the SPSS program version 21.0.
Results
Detailed clinical and cytogenetic findings of the patients are presented in Table 1. The mean age of the 40 patients was 59.3 years, ranging from 41 to 83 years. Eight individuals (20%) were younger than 50 years old at the time of diagnosis. Most of them were males (70%). Three tumors had previous CNS tumors (7.5%).
The main first clinical symptom presented by the patients was intracranial hypertension (n = 25–62.5%), being the headache described in 55%. Focal disturbances and seizures were reported respectively in 42.5 and 12.5% of the cases. Seven patients (17.5%) had relatives with cancer history, including 2 cases (5%) of CNS tumors. In 27 patients (67.5%), the tumor affected the right cerebral hemisphere, and the frontal and parietal regions were the most affected (30 and 25% of the cases, respectively). From 36 cases in which the type of surgery was known, the tumor resection was total in 19 patients (47.5%) and subtotal in 17 (42.5%; Table 1). The median survival time was 145 days (128–162.1). At end of the study, only three patients (7.5%) were still alive.
There was no statistically significant association between the variables gender, tumor location, clinical symptoms, presence of seizures at diagnosis, extent of tumor resection and patient survival. However, age evaluated in a continuous manner was a prognostic factor, and patients with lower age presented a higher survival (HR = 1.04; CI 95% 1.00–1.08; p = 0.042). There was a 4% increase in risk of death for each year of life.
From the cytogenetic point of view, the most frequent alterations were monosomy of chromosome 10 (52.5%), polysomy of chromosome 7 (50%), EGFR amplification (42.5%) and PTEN deletion (35%). In 14 cases (35%), the first two changes (chromosome 10 monosomy and chromosome 7 polysomy) were identified in association (Table 1).
In 76.5% of cases with EGFR amplification, this change was visualized in association with chromosome 7 polysomy. All cases with EGFR amplification also exhibited alterations in chromosome 10: 15 cases (88.2%) with monosomy of chromosome 10 and 7 cases (41.2%) with PTEN deletion (Table 1).
TP53 deletion was observed in 9 patients (22.5%). The distribution of TP53 deletions verified in our sample ranged from 8.5 to 25% (mean 14.4%). Two cases with TP53 deletion also presented EGFR amplification. In addition, 2 cases (5%) with 1p deletion and 3 cases (7.5%) with 19q deletion were identified. We did not detect cases with 1p/19q codeletion (Table 1).
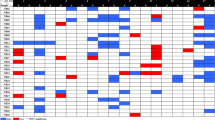
Patients with chromosome 7 polysomy were older (p = 0.016) and tumors with TP53 deletion were more frequently centered in the temporal lobe (p = 0.029). We did not verify an association between survival with EGFR amplification, chromosome 7 polysomy, chromosome 10 monosomy and 1p/19q codeletion. Nevertheless, deletions of TP53 (p = 0.011) and PTEN (p = 0.037) had a negative impact on survival (Fig. 1).
Graphic displaying Kaplan–Meier curves for overall survival times between groups of patients with and without EGFR gene amplification (a), chromosome 7 polysomy (b), chromosome 10 monosomy (c), PTEN deletion (d) and TP53 gene deletion. Note especially that a significant association with poor survival was first noted for PTEN (d) andTP53 deletions (e)
Discussion
According to our literature review, this is the first study with Brazilian patients diagnosed with glioblastoma that investigated the association between aneuploidies of chromosomes 7 and 10, amplification of the EGFR gene, PTEN and TP53 deletions with its clinical status and prognosis. It is noteworthy that there is a scarcity of studies in general involving patients with glioblastoma and FISH analysis not only in Brazil but also in all of Latin America. Pinto et al. [12] investigated 1p and/or 19q losses in a series of 88 Brazilian patients presenting glioblastoma with an oligodendrogial component. We also did not find similar studies in Portuguese and African literature.
Glioblastomas can affect individuals of all age groups, yet it is a rare tumor in children, comprising approximately 2.9% of all brain tumors diagnosed in individuals aged 0–19 years old [5]. It has a higher incidence in individuals aged 45–75 years, with a mean age at diagnosis of 64 years old [1, 5], similar to that observed in our study (59.3 years). We observed an association between lower age at diagnosis and longer survival, what is in agreement with the literature [10, 13, 14].
In our study, most of the individuals were males, which is also in accordance with the literature data (male/female ratio = 1.6:1) [5]. Approximately 5% of patients with malignant gliomas present a family history of this neoplasm. When present, it is associated with a two-fold increased risk of developing the disease. This may be related to rare genetic syndromes, such as neurofibromatosis type 1 and 2 and Li-Fraumeni syndrome [15]. However, in our sample, we did not find patients who filled the clinical criteria for them. First-degree relatives of patients with glioma present a two-fold increased risk of developing the same tumor type, indicating a possible genetic predisposition to the onset of these tumors [16]. In our study, 5% of the cases had a history of tumor occurrence in first-degree relatives.
The initial clinical presentation of glioblastomas is extremely variable, but mainly depends on their location and size. Headache is the most frequent, being present in 50% of patients at time of diagnosis [4]. In our cohort, it was also the first most common clinical symptom, being observed in 22 patients (55%). Toledo et al. [17] described that the occurrence of seizures as one of the first symptoms would be correlated with a better survival, since they could be associated with a reduction in tumor aggressiveness. We also believe that the presence of this finding could draw more attention for an earlier diagnosis of the glioblastoma. In our cohort, we observed that patients with seizures only tended to present a higher survival (p = 0.079). Perhaps, with an increase in our sample, such difference could be really proven.
The use of molecular and cytogenetic techniques has enabled the identification of several genetic alterations in brain tumors, which may contribute to the diagnosis as well as the assessment of prognosis and response to therapy [6]. The expression of the MGMT gene, for example, is a positive predictive marker for newly diagnosed glioma response to the action of alkylating agents [18]. A favorable association has also been described between IDH1/2 and ATRX mutations status and survival [19, 20]. The 2016 WHO incorporated molecular parameters, such as IDH mutations, for the classification of tumors of the CNS in order to group tumors with the same prognostic markers, thus guiding the treatment of biologically similar entities [21].
Amplification of the EGFR gene is a common event in glioblastomas. However, data from different studies have showed that there is a great variability in the frequency of this alteration [13, 22, 23]. This discrepancy can be attributed to tumor heterogeneity, since not all cells show this amplification [24]. Okada et al. [22] identified that cells with a high level of amplification were located mainly at the edges of the tumor, suggesting that EGFR overexpression may be related to tumor invasion. Although it is usual to analyze different quadrants of the slide in order to minimize the loss of areas with amplification, it is still possible that there are regions that may have escaped detection.
In our study, EGFR amplification was observed in 17 cases (42.5%), being associated with chromosome 7 polysomy in 76.5% of them. Several studies have shown that this combination is a frequent event in glioblastomas [10, 25, 26]. In our cohort, patients with chromosome 7 polysomy were older (p = 0.016), which is in accordance with other reports [8].
Similarly to other studies [11, 23, 25,26,27,28], the presence of alterations in chromosome 7 did not have an impact on the overall survival of the patients included in our study. Paradoxically, some authors report that these changes could be correlated with a worse prognosis [8, 10, 13]. Some studies have even observed an improved survival [26]. Although Kleinschmidt-DeMasters et al. [29] have identified the presence of EGFR amplification as a significant predictor of survival time in individuals over 75 years of age, such findings were not evidenced in our sample.
EGFR mutations/amplifications have usually been detected associated with monosomy of chromosome 10 [2, 30]. Similarly, in our cohort, all cases with EGFR amplification exhibited alteration on chromosome 10, from which 15 (88.2%) consisted of chromosome 10 monosomy.
Losses of chromosome 10 are the most common genetic alterations in glioblastoma, and can be identified in up to 60–80% of the cases [31]. In our cohort, they were also frequent, being visualized in 70% of the patients. Chromosome 10 monosomy was identified in 52.5%. However, in an analysis of published studies, there is a great variability in the frequency of this alteration. The frequency observed in our sample is within the expected range from 31.4 to 82.6% [8, 10, 11, 25].
Although most cases present loss of an entire copy of chromosome 10, partial deletions of the gene may also occur and are considered a common finding [32]. The frequency of PTEN deletion ranges from 29.3 to 92.8% in glioblastomas [8, 10, 11, 33, 34], and the frequency of this alteration in our sample was 40%. Some authors have described that losses of the long arm of chromosome 10 could be associated with a worse prognosis [8, 35], in similarity with us. In contrast, other studies do not corroborate these findings [11, 36]. On the other hand, Korshunov et al. [10] demonstrated that losses of 10q are only clinically important in patients >40 years of age. Despite these reports, we did not know how the mutations in the PTEN not detected by FISH analysis may contribute to the results verified in our study. Gene mutations have been described in 24.9–51.2% of the glioblastomas [37, 38].
Mutation or loss of TP53 appears to be one of the most important genetic alteration in glioblastomas, with direct impact on their genesis [2]. Few studies have evaluated the deletion of TP53 through FISH [2, 14, 39]. In our sample, TP53 deletion was visualized in 9 patients (22.5%), an index similar to that described in other studies [2, 14]. It was noteworthy that tumors with TP53 deletion were more frequently centered in the temporal lobe.
Two cases with TP53 deletion of our sample also exhibited EGFR amplification. Although studies have indicated that this event presents a mutually exclusive pattern in a majority of tumors [40], concomitant alterations of EGFR and TP53 have been reported [2, 14, 41]. Okada et al. [22] identified isolated cells with EGFR amplification in different regions of glioblastomas with TP53 mutation, which demonstrates that amplification of this gene at a cellular level may be a frequent event. The authors suggest that genomic instability due to inactivation of p53 may promote gene amplification. According to Ruano et al. [41], the simultaneous deregulation of these two pathways may indicate a relevant deregulation of the cell cycle that results in the formation of a more aggressive tumor.
In our sample, patients with TP53 deletion exhibited a significantly worse prognosis. Although studies have pointed out that TP53 alterations have a limited impact on prognosis [2, 14, 42,43,44], some authors have found that there is an association between them and a worse prognosis [45], besides a loss of response to temozolamide [46, 47]. On the other hand, Tada et al. [48] described TP53 mutation as a marker of better response to radiotherapy, which could imply a significantly longer survival. Shih et al. [45] failed to reproduce these findings, and only evidenced the prognostic value of the TP53 mutation in patients aged ≥57 years, who showed a reduced survival. Momota et al. [49] observed that TP53 mutations are frequent events in diffuse or multiple lesion malignant astrocytomas, suggesting that TP53 abnormalities may affect the aggressive and invasive nature of these tumors. Despite these different outcomes, we did not know how other mutations in the TP53 not detected by FISH analysis and not evaluated in our study might influence the observed results. The frequency of gene mutations of the TP53 ranges from 18.8 to 43% [22, 45].
In our study, two patients with TP53 deletion also presented monosomy of chromosome 10. Leenstra et al. [50] demonstrated that these patients with high-grade astrocytomas had a shorter survival (median 3 months) when compared to patients with only loss of 17p (median 17 months). In our cohort, however, these patients did not have a shorter survival (p = 0.344).
In conventional glioblastomas, although 1p/19q codeletion is an uncommon event, identified in 0–25% of the cases, isolated losses of 1p or 19q are frequent (40 and 30%, respectively) [8, 10, 12, 51,52,53]. In our study, cases with 1p/19q codeletion were not identified, but there were 2 cases (5%) with isolated 1p deletion and 3 (7.5%) with isolated deletion of 19q. In 2013, Clark et al. [53], with the objective of investigating whether the losses of 1p and 19q could have an impact on the evaluation of glioblastomas, investigated a large cohort of 491 patients. Only one case of codeletion was identified. The presence of codeletion as well as the isolated losses of 1p and 19q had no impact on patient survival.
The results of the present study suggest that some cytogenetic markers, alone or together, may be related to some clinical findings and present a potential role in the prognostic of patients with glioblastoma. Our data suggest that especially TP53 and PTEN deletions might have a negative impact on prognosis. Further studies with larger samples will be important to clarify the role of these alterations in the patients survival.
References
Wen PY, Kesari S (2008) Malignant gliomas in adults. N Engl J Med 359(5):492–507
Necesalová E, Vranová V, Kuglík P, Cejpek P, Jarosová M, Pesáková M, Relichová J, Veselská R (2007) Incidence of the main genetic markers in glioblastoma multiforme is independent of tumor topology. Neoplasma 54(3):212–218
Kleihues P, Burger PC, Aldape KD, Brat DJ, Biernat W, Bigner DD, Nakazato Y, Plate KH, Giangaspero F, von Deimling A, Ohgaki H, Cavenee WK (2007) Glioblastoma. In: Louis DN, Ohgaki H, Wiestler OD, Cavanee WK (eds) WHO classification of tumours of the central nervous system. IARC, Lyon, pp 33–49
Preusser M, de Ribaupierre S, Wohrer A, Erridge SC, Hegi M, Weller M, Stupp R (2011) Current concepts and management of glioblastoma. Ann Neurol 70:9–21
Ostrom QT, Gittleman H, Fulop J, Liu M, Blanda R, Kromer C, Wolinsky Y, Kruchko C, Barnholtz-Sloan JS (2015) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2008–2012. Neuro Oncol 17(Suppl 4):iv1–iv62
Hassler M, Seidl S, Fazeny-Doerner B, Preusser M, Hainfellner J, Rössler K, Prayer D, Marosi C (2006) Diversity of cytogenetic and pathohistologic profiles in glioblastoma. Cancer Genet Cytogenet 166(1):46–55
Medinger M, Lengerke C, Passweg J (2016) Novel prognostic and therapeutic mutations in acute myeloid leukemia. Cancer Genomics Proteomics 13(5):317–329
Korshunov A, Sycheva R, Golanov A (2004) Molecular stratification of diagnostically challenging high-grade gliomas composed of small cells: the utility of fluorescence in situ hybridization. Clin Cancer Res 10(23):7820–7826
Lamborn KR, Chang SM, Prados MD (2004) Prognostic factors for survival of patients with glioblastoma: recursive partitioning analysis. Neuro Oncol 6(3):227–235
Korshunov A, Sycheva R, Golanov A (2005) The prognostic relevance of molecular alterations in glioblastomas for patients age <50 years. Cancer 104(4):825–832
Rodriguez FJ, Scheithauer BW, Giannini C, Bryant SC, Jenkins RB (2008) Epithelial and pseudoepithelial differentiation in glioblastoma and gliosarcoma: a comparative morphologic and molecular genetic study. Cancer 113(10):2779–2789
Pinto LW, Araújo MB, Vettore AL, Wernersbach L, Leite AC, Chimelli LM, Soares FA (2008) Glioblastomas: correlation between oligodendroglial components, genetic abnormalities, and prognosis. Virchows Arch 452(5):481–490
Kim B, Myung JK, Seo JH, Park CK, Paek SH, Kim DG, Jung HW, Park SH (2010) The clinicopathologic values of the molecules associated with the main pathogenesis of the glioblastoma. J Neurol Sci 294(1–2):112–118
Klink B, Schlingelhof B, Klink M, Stout-Weider K, Patt S, Schrock E (2011) Glioblastomas with oligodendroglial component-common origin of the different histological parts and genetic subclassification. Cell Oncol (Dordr) 34(3):261–275
Farrel CJ, Plotkin SR (2007) Genetic causes of brain tumors: neurofibromatosis, tuberous sclerosis, von Hippel-Landau and other syndromes. Neurol Clin 25:925–946
Malmer B, Henriksson R, Grönberg H (2003) Familial brain tumours-genetics or environment? A nationwide cohort study of cancer risk in spouses and first-degree relatives of brain tumour patients. Int J Cancer 106(2):260–263
Toledo M, Sarria-Estrada S, Quintana M, Maldonado X, Martinez-Ricarte F, Rodon J, Auger C, Salas-Puig J, Santamarina E, Martinez-Saez E (2015) Prognostic implications of epilepsy in glioblastomas. Clin Neurol Neurosurg 139:166–171
Wang J, Su HK, Zhao HF, Chen ZP, To SS (2015) Progress in the application of molecular biomarkers in gliomas. Biochem Biophys Res Commun 465(1):1–4
Jansen M, Yip S, Louis DN (2010) Molecular pathology in adult neuro-oncology: an update on diagnostic, prognostic and predictive markers. Lancet Neuro 9:717–726
Mur P, Mollejo M, Hernández-Iglesias T, de Lope ÁR, Castresana JS, García JF, Fiaño C, Ribalta T, Rey JA, Meléndez B (2015) Molecular classification defines 4 prognostically distinct glioma groups irrespective of diagnosis and grade. J Neuropathol Exp Neurol 74(3):241–249
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P, Ellison DW (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol 131(6):803–820
Okada Y, Hurwitz EE, Esposito JM, Brower MA, Nutt CL, Louis DN (2003) Selection pressures of TP53 mutation and microenvironmental location influence epidermal growth factor receptor gene amplification in human glioblastomas. Cancer Res 63(2):413–416
Faulkner C, Palmer A, Williams H, Wragg C, Haynes HR, White P, DeSouza RM, Williams M, Hopkins K, Kurian KM (2014) EGFR and EGFRvIII analysis in glioblastoma as therapeutic biomarkers. Br J Neurosurg 20:1–7
Little SE, Popov S, Jury A, Bax DA, Doey L, Al-Sarraj S, Jurgensmeier JM, Jones C (2012) Receptor tyrosine kinase genes amplified in glioblastoma exhibit a mutual exclusivity in variable proportions reflective of individual tumor heterogeneity. Cancer Res 72(7):1614–1620
Benito R, Gil-Benso R, Quilis V, Perez M, Gregori-Romero M, Roldan P, Gonzalez-Darder J, Cerdá-Nicolas M, Lopez-Gines C (2010) Primary glioblastomas with and without EGFR amplification: relationship to genetic alterations and clinicopathological features. Neuropathology 30(4):392–400
Lopez-Gines C, Gil-Benso R, Ferrer-Luna R, Benito R, Serna E, Gonzalez-Darder J, Quilis V, Monleon D, Celda B, Cerdá-Nicolas M (2010) New pattern of EGFR amplification in glioblastoma and the relationship of gene copy number with gene expression profile. Mod Pathol 23(6):856–865
Joensuu H, Puputti M, Sihto H, Tynninen O, Nupponen NN (2005) Amplification of genes encoding KIT, PDGFRalpha and VEGFR2 receptor tyrosine kinases is frequent in glioblastoma multiforme. J Pathol 207(2):224–231
Quan AL, Barnett GH, Lee SY, Vogelbaum MA, Toms SA, Staugaitis SM, Prayson RA, Peereboom DM, Stevens GH, Cohen BH, Suh JH (2005) Epidermal growth factor receptor amplification does not have prognostic significance in patients with glioblastoma multiforme. Int J Radiat Oncol Biol Phys 63(3):695–703
Kleinschmidt-DeMasters BK, Lillehei KO, Varella-Garcia M (2005) Glioblastomas in the older old. Arch Pathol Lab Med 129(5):624–631
Horiguchi H, Hirose T, Sano T, Nagahiro S (1999) Loss of chromosome 10 in glioblastoma: relation to proliferation and angiogenesis. Pathol Int 49(8):681–686
Ohgaki H (2005) Genetic pathways to glioblastomas. Neuropathology 25(1):1–7
James CD, Carlbom E, Dumanski JP, Hansen M, Nordenskjold M, Collins VP, Cavenee WK (1988) Clonal genomic alterations glioma malignancy stages. Cancer Res 48(19):5546–5551
Smith JS, Tachibana I, Passe SM, Huntley BK, Borell TJ, Iturria N, O’Fallon JR, Schaefer PL, Scheithauer BW, James CD, Buckner JC, Jenkins RB (2001) PTEN mutation, EGFR amplification, and outcome in patients with anaplastic astrocytoma and glioblastoma multiforme. J Natl Cancer Inst 93(16):1246–1256
Appin CL, Gao J, Chisolm C, Torian M, Alexis D, Vincentelli C, Schniederjan MJ, Hadjipanayis C, Olson JJ, Hunter S, Hao C, Brat DJ (2013) Glioblastoma with oligodendroglioma component (GBM-O): molecular genetic and clinical characteristics. Brain Pathol 23(4):454–461
Kakkar A, Suri V, Jha P, Srivastava A, Sharma V, Pathak P, Sharma MC, Sharma MS, Kale SS, Chosdol K, Phalak M, Sarkar C (2011) Loss of heterozygosity on chromosome 10q in glioblastomas, and its association with other genetic alterations and survival in Indian patients. Neurol India 59(2):254–261
Houillier C, Lejeune J, Benouaich-Amiel A, Laigle-Donadey F, Criniere E, Mokhtari K, Thillet J, Delattre JY, Hoang-Xuan K, Sanson M (2006) Prognostic impact of molecular markers in a series of 220 primary glioblastomas. Cancer 106(10):2218–2223
Koul D (2008) PTEN signaling pathways in glioblastoma. Cancer Biol Ther 7(9):1321–1325
Xu J, Li Z, Wang J, Chen H, Fang JY (2014) Combined PTEN Mutation and Protein Expression Associate with Overall and Disease-Free Survival of Glioblastoma Patients. Transl Oncol 7(2):196–205.e1
Horiguchi H, Sano T, Hirose T (2001) TP53 deleted cells in de novo glioblastomas using fluorescence in situ hybridization. Pathol Int 51(3):187–192
von Deimling A, von Ammon K, Schoenfeld D, Wiestler OD, Seizinger BR, Louis DN (1993) Subsets of glioblastoma multiforme defined by molecular genetic analysis. Brain Pathol 3(1):19–26
Ruano Y, Ribalta T, de Lope AR, Campos-Martin Y, Fiano C, Perez-Magan E, Hernández-Moneo JL, Mollejo M, Meléndez B (2009) Worse outcome in primary glioblastoma multiforme with concurrent epidermal growth factor receptor and p53 alteration. Am J Clin Pathol 131(2):257–263
Rich JN, Hans C, Jones B, Iversen ES, McLendon RE, Rasheed BKA, Dobra A, Dressman HK, Bigner DD, Nevins JR, West M (2005) Gene expression profiling and genetic markers in glioblastoma survival. Cancer Res 65:4051–4058
Felsberg J, Rapp M, Loeser S, Fimmers R, Stummer W, Goeppert M, Steiger HJ, Friedensdorf B, Reifenberger G, Sabel MC (2009) Prognostic significance of molecular markers and extent of resection in primary glioblastoma patients. Clin Cancer Res 15:6683–6693
Stancheva G, Goranova T, Laleva M, Kamenova M, Mitkova A, Velinov N, Poptodorov G, Mitev V, Kaneva R, Gabrovsky N (2014) IDH1/IDH2 but not TP53 mutations predict prognosis in Bulgarian glioblastoma patients. Biomed Res Int 2014:654727
Shih HA, Betensky RA, Dorfman MV, Louis DN, Loeffler JS, Batchelor TT (2005) Genetic analyses for predictors of radiation response in glioblastoma. Int J Radiat Oncol Biol Phys 63(3):704–710
Wang X, Chen JX, Liu JP, You C, Liu YH, Mao Q (2014) Gain of function of mutant TP53 in glioblastoma: prognosis and response to temozolomide. Ann Surg Oncol 21(4):1337–1344
Wang X, Chen JX, Liu YH, You C, Mao Q (2013) Mutant TP53 enhances the resistance of glioblastoma cells to temozolomide by up-regulating O(6)-methylguanine DNA-methyltransferase. Neurol Sci 34(8):1421–1428
Tada M, Matsumoto R, Iggo RD, Onimaru R, Shirato H, Sawamura Y, Shinohe Y (1998) Selective sensitivity to radiation of cerebral glioblastomas harboring p53 mutations. Cancer Res 58(9):1793–1797
Momota H, Narita Y, Matsushita Y, Miyakita Y, Shibui S (2010) p53 abnormality and tumor invasion in patients with malignant astrocytoma. Brain Tumor Pathol 27(2):95–101
Leenstra S, Bijlsma EK, Troost D, Oosting J, Westerveld A, Bosch DA, Hulsebos TJ (1994) Allele loss on chromosomes 10 and 17p and epidermal growth factor receptor gene amplification in human malignant astrocytoma related to prognosis. Br J Cancer 70(4):684–689
Nagasaka T, Gunji M, Hosokai N, Hayashi K, Ikeda H, Ito M, Inao S (2007) FISH 1p/19q deletion/imbalance for molecular subclassification of glioblastoma. Brain Tumor Pathol 24(1):1–5
Kaneshiro D, Kobayashi T, Chao ST, Suh J, Prayson RA (2009) Chromosome 1p and 19q deletions in glioblastoma multiforme. Appl Immunohistochem Mol Morphol 17(6):512–516
Clark KH, Villano JL, Nikiforova MN, Hamilton RL, Horbinski C (2013) 1p/19q testing has no significance in the workup of glioblastomas. Neuropathol Appl Neurobiol 39(6):706–717
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This study was approved by the Ethics in Research Committee of the Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA) – number 881/09.
Rights and permissions
About this article
Cite this article
Koshiyama, D.B., Trevisan, P., Graziadio, C. et al. Frequency and clinical significance of chromosome 7 and 10 aneuploidies, amplification of the EGFR gene, deletion of PTEN and TP53 genes, and 1p/19q deficiency in a sample of adult patients diagnosed with glioblastoma from Southern Brazil. J Neurooncol 135, 465–472 (2017). https://doi.org/10.1007/s11060-017-2606-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-017-2606-6