Abstract
The yield of echocardiography in cancer patients with acute ischemic stroke is unknown. We identified adult patients with active systemic cancer diagnosed with acute ischemic stroke at a tertiary-care cancer center from 2005 through 2009 who underwent transthoracic (TTE) or transesophageal echocardiography (TEE). Two neurologists independently reviewed all clinical data, including TTE and TEE reports, and adjudicated whether echocardiographic studies revealed a definite or possible source of stroke according to pre-defined criteria. Patients were classified as having suspected cardioembolic strokes if imaging showed embolic-appearing infarcts in more than one vascular territory. Among 220 patients with cancer and ischemic stroke who underwent echocardiography, 216 (98 %) had TTE and 37 (17 %) had TEE. TTE revealed a definite source in 15 (7 %, 95 % CI 4–10 %) patients and a possible source in 42 (19 %, 95 % CI 14–25 %), while TEE revealed a definite source in 10 (27 %, 95 % CI 12–42 %) patients and a possible source in 14 (38 %, 95 % CI 21–54 %). In 92 patients with suspected cardioembolic strokes who underwent TTE, 6 (7 %, 95 % CI 1–12 %) had a definite source, including 4 with marantic endocarditis, and 20 (22 %, 95 % CI 13–30 %) had a possible source. Twenty-one of these patients also underwent TEE, which demonstrated a definite or possible source in 16 (76 %, 95 % CI 56–96 %) patients, including marantic endocarditis in 4 (19 %). The yield of TTE for detecting marantic endocarditis and other cardiac sources of stroke in cancer patients is low, but TEE may provide a higher yield in targeted patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cancer and stroke are the second and fourth leading causes of death in the United States and independently account for a large burden of morbidity and mortality [1]. Stroke occurs in up to 15 % of patients with cancer and is caused by both traditional risk factors and cancer-specific mechanisms often related to acquired hypercoagulability [2–4]. Stroke in patients with cancer may disrupt cancer therapy and is typically associated with short life expectancy [5, 6].
The cause of stroke in cancer patients often differs from the general population [2–4]. Cardiac sources of embolism account for 15–30 % of ischemic strokes in the general stroke population [7, 8]. Conversely, in cancer patients, the occurrence of cardioembolic strokes is thought to be higher, with about 40 % exhibiting a cardioembolic pattern of stroke on neuroimaging [4, 9]. In addition, 46 % of cancer patients with acute ischemic stroke have evidence of microemboli—a surrogate of cardiac embolism—on transcranial Doppler studies [10]. Furthermore, a large autopsy study demonstrated that marantic endocarditis, which consists of sterile platelet–fibrin vegetations on cardiac valves, is the most common cause of symptomatic ischemic stroke in cancer patients [2]. However, the vegetations in marantic endocarditis are generally small and friable and thus may be difficult to detect on clinical imaging [2, 11, 12].
Transthoracic echocardiography (TTE) is frequently used to evaluate stroke patients for potential cardiac sources of emboli. In the general stroke population, depending on patients’ age and risk factors, the yield of TTE ranges from 5–19 % and the yield of transesophageal echocardiography (TEE) ranges from 41–60 % [13–17]. In cancer patients with stroke, echocardiography is often used to evaluate for marantic endocarditis and other cardioembolic sources, but its yield is uncertain. One study reported that TEE identified a definite cardiac source of embolism in 47 % of cancer patients with stroke, including marantic endocarditis in 18 %; however, this study included only 51 patients and did not evaluate TTE, which is more commonly performed [11]. Therefore, we performed a large retrospective study to better evaluate the yield of TTE and TEE in patients with systemic cancer and ischemic stroke. Our hypothesis was that TEE would be superior to TTE in detecting potential sources of cardioembolism.
Methods
Study design
We identified all adult patients (age ≥ 18 years) with active systemic cancer diagnosed with an acute ischemic stroke at Memorial Sloan Kettering Cancer Center (MSKCC) from January 1, 2005 to December 31, 2009. Active systemic cancer was defined as in previous studies as the diagnosis of, or treatment for, any systemic cancer besides local basal cell or squamous cell carcinoma of the skin within the prior 6 months, or known recurrent or metastatic disease [4, 10, 18]. Acute ischemic stroke was defined as a new neurological deficit with corresponding evidence of acute ischemia on brain MRI without any clinical or radiographic evidence of a non-cerebrovascular etiology.
Study subjects
As previously described [5], patients were identified using an administrative database search for International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for ischemic stroke (codes 433.01, 433.11, 433.21, 433.31, 433.81, 433.91, 434.01, 434.11, 434.91), and by reviewing the MSKCC Department of Neurology’s prospective clinical database for diagnoses of “ischemic stroke”, “stroke”, or “transient ischemic attack”. We excluded patients whose stroke was based solely on CT imaging as cerebral metastases can mimic stroke and differentiating the two can be difficult. In addition, patients were excluded if their stroke was diagnosed as an outpatient, as these patients were less likely to have complete diagnostic evaluations. After these initial screens, all charts were reviewed by a board-certified neurologist to determine final eligibility. Our institutional review board approved this study and the requirement of informed consent was waived due to minimal risk to patients.
Measurements
In accordance with the recommended guidelines for cohort studies, data were collected using a standardized abstraction form that had undergone several revisions prior to official use based on pilot abstractions and investigator meetings [19, 20]. This data abstraction form and a data dictionary containing a list of all predefined variables were used by a reviewing neurologist to collect data about patients’ demographics, comorbidities, type and extent of cancer, brain and vascular imaging, echocardiographic studies, and clinical outcomes [21]. Only echocardiography studies performed at the time of ischemic stroke were abstracted. Medical records were reviewed for clinical outcomes from the time of the index stroke until death or July 31, 2012.
After reviewing all clinical, laboratory, radiological, and pathological data, two board-certified neurologists determined by consensus each patient’s specific stroke mechanism (if known) and stroke subtype according to the modified Trial of ORG 10172 in Acute Stroke Treatment Study (TOAST) criteria [22]. Marantic endocarditis was diagnosed only if there was echocardiographic or pathologic evidence of cardiac valve vegetation(s) without positive blood cultures or other signs of infection. Reviewing neurologists also classified patients by their radiographic infarction pattern; patients whose brain MRI demonstrated wedge-shaped or cortical infarctions in multiple vascular territories were suspected to have cardioembolic stroke [23].
All TTEs and TEEs performed to evaluate patients’ strokes were reviewed. Relevant findings were classified as definite or possible cardiac sources of stroke based on a modified version of previously established criteria by Dutta et al. [11]. Our study used a more inclusive approach than that used by Dutta et al. in that left ventricular thrombus, severe cardiomyopathy, cardiac tumor, dyskinetic left ventricular segment, spontaneous echocardiography contrast, and simple aortic arch atheroma were also considered relevant findings [11]. Definite cardiac sources included complex aortic arch atheroma (proximally located atheroma >0.4 cm or with ulceration or thrombus), valve vegetation, left atrial or ventricular thrombus, patent foramen ovale (PFO) with documented venous thromboembolism (evidence of right-to-left shunt with concomitant deep vein thrombosis or pulmonary embolism), severe cardiomyopathy (ejection fraction less than 30 %), or cardiac tumor. Possible cardiac sources consisted of PFO without venous thromboembolism, atrial septal aneurysm, dyskinetic left ventricular segment (echocardiographic evidence of focal segmental wall motional abnormality), spontaneous echocardiography contrast (suggesting clot-in-formation), and simple aortic arch atheroma (proximally located atheroma <0.4 cm and without ulceration or thrombus).
Statistical analysis
Descriptive statistics were used to characterize patients’ baseline characteristics and outcome rates. Fisher’s exact test or the Chi squared test was used to compare dichotomous baseline characteristics in patients who had TTE as compared to those who had TEE; while the Student’s t test or Wilcoxon rank-sum test was used for continuous variables. Our primary outcome was a definite or possible cardiac source of stroke discovered by echocardiography. TTE and TEE were evaluated both individually and together, and separate analyses were performed for the entire cohort and for patients with suspected cardioembolic stroke based on their radiographic infarction pattern. Significance was defined as a p value of <0.05.
Results
Description of the cohort
Among 263 patients with active cancer and acute ischemic stroke, 220 (84 %) had echocardiography and were included in our final analysis. Of these 220 patients, 216 (98 %) had a TTE and 37 (17 %) had a TEE; both studies were performed in 33 (15 %) patients. Patients who did not have echocardiography generally had terminal cancer, and had fewer diagnostic stroke evaluations (i.e., vessel imaging), worse functional status at hospital discharge, and worse overall survival (median 25 days versus 109 days, p < 0.01) than patients who had echocardiography. Among patients who lived beyond 30 days, 90 % had echocardiography. In addition, patients who had TEE more often had vessel imaging (95 vs. 81 %, p = 0.05), good functional outcomes at discharge (57 vs. 39 %, p = 0.05), and disposition to home (70 vs. 55 %, p = 0.08) than patients who only had TTE.
Mean patient age was 66 years (SD 13), 51 % were women, and most patients were white (80 %); there were no significant demographic differences between patients who had TTE versus those who had TEE. Most underlying cancers were solid tumors of adenocarcinoma histology, particularly of the lung, gastrointestinal tract, or genitourinary system (Table 1). Other solid tumors, including breast and gynecological malignancies, were less common, while liquid tumors only accounted for 10 % of cases. Median time from cancer diagnosis to stroke was 10 months (interquartile range 2–34). Disseminated cancer was common at the time of stroke with most patients having known metastases to other organs and more than half having received cancer treatment within 30 days.
Stroke classification
Based on TOAST criteria, stroke subtypes for patients who had echocardiography were 24 % cardioembolism, 15 % large artery atherosclerosis, 7 % small vessel occlusion, 4 % other determined causes, and 50 % undetermined. Marantic endocarditis was diagnosed in only 5 % (n = 10). Among the entire cohort, 93 patients (42 %) were suspected to have a cardioembolic stroke based on their radiographic infarction pattern; among those with an undetermined stroke mechanism, 63 (57 %) were suspected to have a cardioembolic stroke.
Yield of echocardiography
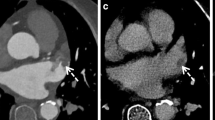
TTE revealed a definite cardiac source of stroke in 15 (7 %, 95 % CI 4–10 %) patients, a possible source in 42 (19 %, 95 % CI 14–25 %), and a definite or possible source in 48 (22 %, 95 % CI 17–28 %; some studies revealed both a definite and possible source thus individual percentages do not add up equally). TEE revealed a definite source in 10 (27 %, 95 % CI 12–42 %) patients, a possible source in 14 (38 %, 95 % CI 21–54 %), and a definite or possible source in 23 (62 %, 95 % CI 46–79 %) (Fig. 1). Among 168 patients with an unremarkable TTE, 27 also had TEE, of which 14 (52 %, 95 % CI 32–72 %) revealed a definite or possible source of stroke.
In the subgroup of patients with suspected cardioembolic stroke based on their radiographic infarction pattern (n = 93), 72 had TTE alone, 20 had both TTE and TEE, and 1 had TEE alone. Among this group, TTE revealed a definite cardiac source in 6 (7 %, 95 % CI 1–12 %) patients, a possible source in 20 (22 %, 95 % CI 13–30 %), and a definite or possible source in 22 (24 %, 95 % CI 15–33 %). In contrast, TEE revealed a definite cardiac source in 7 patients (33 %, 95 % CI 11–55 %), a possible source in 10 (48 %, 95 % CI 24–71 %), and a definite or possible source in 16 (76 %, 95 % CI 56–96 %) (Fig. 2).
Diagnostic yield of echocardiography in cancer patients with ischemic stroke and suspected cardioembolism based on radiographic infarct pattern. Bar graph showing frequency and associated 95 % confidence interval of definite and possible cardiac sources of stroke in cancer patients with acute ischemic stroke and suspected cardioembolism based on radiographic infarct pattern
Relevant echocardiographic findings varied and included typical stroke mechanisms such as PFO, as well as atypical mechanisms unique to the cancer population such as cardiac tumor (Table 2). Four vegetations were seen on TTE, all from marantic endocarditis, while six vegetations were seen on TEE, four from marantic endocarditis and two from infective endocarditis. Of the six vegetations diagnosed by TEE, none were seen on TTE. Among patients with suspected cardioembolic stroke, marantic endocarditis was detected in 19 % with TEE and 4 % with TTE (Table 3).
Discussion
In this large cohort of cancer patients with stroke, the yield of TTE for the detection of cardiac sources of emboli was low, even when a cardioembolic source was suspected. However, the yield of TEE in cancer patients with stroke was considerably higher and may be particularly helpful in targeted patients. For example, in patients with suspected cardioembolic stroke based on infarction pattern, TEE identified a potential cardiac source of stroke in 76 %.
To our knowledge, only one prior study has examined the yield of echocardiography in cancer patients with stroke [11]. This study evaluated the diagnostic yield of TEE in 51 patients, and reported that 47 % had a definite cardiac source of stroke and 55 % had a definite or possible (termed probable by authors) cardiac source [11]. Our study evaluated the yield of both TTE and TEE, and TEE identified a definite cardiac source in 27 % and a definite or possible source in 62 %. Therefore, our study identified fewer definite cardiac sources of stroke but more possible sources. A potential reason for this discrepancy is that our study used a slightly different set of definitions for cardiac sources of stroke. For example, we included left ventricular thrombus, severe cardiomyopathy, and cardiac tumor as definite cardiac sources, and dyskinetic left ventricular segment, spontaneous echocardiography contrast, and simple aortic arch atheroma as possible sources, while Dutta et al. excluded these potential stroke mechanisms [11]. Differences in patient characteristics between the two studies could also have affected TEE findings. Our patients had more advanced cancer (68 % with systemic metastases vs. 21 %), which could have resulted in an enriched group of patients with cancer-specific stroke mechanisms, as cancer stage is associated with marantic endocarditis and other unconventional stroke mechanisms [2, 4, 10, 11].
The yield of TTE and TEE in the general stroke population is variable, ranging from 5 to 19 % for TTE and 41 to 60 % for TEE [13–17]. In our cohort of patients with stroke and cancer, the yield of both TTE and TEE was similar to the general stroke population—22 % for TTE and 62 % for TEE—despite the higher incidence of cardioembolic strokes in the cancer population. This conceptual discrepancy may be explained by the fact that marantic endocarditis is a frequent cause of cardioembolic stroke in patients with cancer; however, the vegetations from marantic endocarditis are typically small and friable and therefore may be frequently missed on echocardiography [2, 11, 12].
In our cohort, TEE outperformed TTE in the detection of marantic endocarditis (11 vs. 2 %). Based on an autopsy study of 500 cancer patients with cerebrovascular disease, marantic endocarditis was the most common cause of symptomatic ischemic stroke, accounting for 32 % of cases [2]. However, marantic endocarditis is notoriously difficult to visualize, even with TEE [11, 12]. In our study, only 10 of 220 patients were definitively diagnosed with marantic endocarditis, although the yield was higher with TEE (19 %) when performed in patients suspected to have cardioembolic strokes. In addition, TEE detected vegetations in six patients that were missed on TTE, suggesting that TEE is superior to TTE for the evaluation of marantic endocarditis. Diagnosing marantic endocarditis may be clinically meaningful because recent data suggest that these cancer patients have shorter survival and higher rates of recurrent thromboembolism than cancer patients with stroke from other mechanisms [5, 24]. However, TEE is more invasive than TTE and its use is cancer patients can be limited by several clinical factors, including poor clinical status, encephalopathy, and severe coagulopathy. Therefore, physicians will need to decide on a case-by-case basis whether the incremental diagnostic yield of TEE justifies its increased procedural risk and invasiveness.
Our study has several limitations. First, this was a retrospective single-center study performed at an urban, tertiary-care cancer hospital and thus our results may not generalize to other settings. Second, echocardiographic evaluations were not standardized or complete and only 17 % of patients had TEE. This may have introduced a selection bias resulting in inflated diagnostic yields, particularly for TEE. In addition, the low absolute numbers for TEE resulted in diagnostic yield estimates that were imprecise as evident by the wide confidence intervals. Third, our interpretation of echocardiographic findings was based on clinical reports and not actual image review and thus some findings may have been missed or incorrect. Finally, our study was underpowered to evaluate the association between specific chemotherapy agents and echocardiography findings; future studies should be performed to evaluate this potential relationship.
In summary, the yield of TTE in cancer patients with acute ischemic stroke is low, even if a cardiac source of stroke is suspected. However, TEE may have a higher yield for detecting cardiac sources of stroke, particularly when cardioembolism is suspected based on the radiographic infarction pattern. Furthermore, TEE appears superior to TTE in the detection of marantic endocarditis. Our results should be validated in a prospective community-based cohort with standardized evaluations. If confirmed, these observations may be helpful in determining the optimal diagnostic evaluation strategy for ischemic stroke in cancer patients.
References
Centers for Disease Control and Prevention: Leading Causes of Death (2012). http://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm. Accessed 28 June 2014
Graus F, Rogers LR, Posner JB (1985) Cerebrovascular complications in patients with cancer. Medicine 64:16–35
Schwarzbach CJ, Schaefer A, Ebert A, Held V, Bolognese M, Kablau M, Hennerici MG, Fatar M (2012) Stroke and cancer: the importance of cancer-associated hypercoagulation as a possible stroke etiology. Stroke 43:3029–3034. doi:10.1161/STROKEAHA.112.658625
Kim SG, Hong JM, Kim HY, Lee J, Chung PW, Park KY, Kim GM, Lee KH, Chung CS, Bang OY (2010) Ischemic stroke in cancer patients with and without conventional mechanisms: a multicenter study in Korea. Stroke 41:798–801. doi:10.1161/STROKEAHA.109.571356
Navi BB, Singer S, Merkler AE, Cheng NT, Stone JB, Kamel H, Iadecola C, Elkind MS, DeAngelis LM (2014) Recurrent thromboembolic events after ischemic stroke in patients with cancer. Neurology 83:26–33. doi:10.1212/WNL.0000000000000539
Saposnik G, Kapral MK, Liu Y, Hall R, O’Donnell M, Raptis S, Tu JV, Mamdani M, Austin PC, Network IotRotCS, Group SORCSW (2011) IScore: a risk score to predict death early after hospitalization for an acute ischemic stroke. Circulation 123:739–749. doi:10.1161/CIRCULATIONAHA.110.983353
Ferro JM (2003) Cardioembolic stroke: an update. Lancet Neurol 2:177–188
Pepi M, Evangelista A, Nihoyannopoulos P, Flachskampf FA, Athanassopoulos G, Colonna P, Habib G, Ringelstein EB, Sicari R, Zamorano JL, Sitges M, Caso P, Echocardiography EAo (2010) Recommendations for echocardiography use in the diagnosis and management of cardiac sources of embolism: European Association of Echocardiography (EAE) (a registered branch of the ESC). Eur J Echocardiogr 11:461–476. doi:10.1093/ejechocard/jeq045
Kim JM, Jung KH, Park KH, Lee ST, Chu K, Roh JK (2013) Clinical manifestation of cancer related stroke: retrospective case-control study. J Neurooncol 111:295–301. doi:10.1007/s11060-012-1011-4
Seok JM, Kim SG, Kim JW, Chung CS, Kim GM, Lee KH, Bang OY (2010) Coagulopathy and embolic signal in cancer patients with ischemic stroke. Ann Neurol 68:213–219. doi:10.1002/ana.22050
Dutta T, Karas MG, Segal AZ, Kizer JR (2006) Yield of transesophageal echocardiography for nonbacterial thrombotic endocarditis and other cardiac sources of embolism in cancer patients with cerebral ischemia. Am J Cardiol 97:894–898. doi:10.1016/j.amjcard.2005.09.140
Asopa S, Patel A, Khan OA, Sharma R, Ohri SK (2007) Non-bacterial thrombotic endocarditis. Eur J Cardiothorac Surg 32:696–701. doi:10.1016/j.ejcts.2007.07.029
Zhang L, Harrison JK, Goldstein LB (2012) Echocardiography for the detection of cardiac sources of embolism in patients with stroke or transient ischemic attack. J Stroke Cerebrovasc Dis 21:577–582. doi:10.1016/j.jstrokecerebrovasdis.2011.01.005
Pearson AC, Labovitz AJ, Tatineni S, Gomez CR (1991) Superiority of transesophageal echocardiography in detecting cardiac source of embolism in patients with cerebral ischemia of uncertain etiology. J Am Coll Cardiol 17:66–72
Sansoy V, Abbott RD, Jayaweera AR, Kaul S (1995) Low yield of transthoracic echocardiography for cardiac source of embolism. Am J Cardiol 75:166–169
Cujec B, Polasek P, Voll C, Shuaib A (1991) Transesophageal echocardiography in the detection of potential cardiac source of embolism in stroke patients. Stroke 22:727–733
de Bruijn SF, Agema WR, Lammers GJ, van der Wall EE, Wolterbeek R, Holman ER, Bollen EL, Bax JJ (2006) Transesophageal echocardiography is superior to transthoracic echocardiography in management of patients of any age with transient ischemic attack or stroke. Stroke 37:2531–2534. doi:10.1161/01.STR.0000241064.46659.69
Lee AY, Levine MN, Baker RI, Bowden C, Kakkar AK, Prins M, Rickles FR, Julian JA, Haley S, Kovacs MJ, Gent M (2003) Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med 349:146–153. doi:10.1056/NEJMoa025313
Lowenstein SR (2005) Medical record reviews in emergency medicine: the blessing and the curse. Ann Emerg Med 45:452–455. doi:10.1016/j.annemergmed.2005.01.032
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Initiative S (2007) Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 335:806–808. doi:10.1136/bmj.39335.541782.AD
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19:604–607
Adams HP, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41
Kang DW, Chalela JA, Ezzeddine MA, Warach S (2003) Association of ischemic lesion patterns on early diffusion-weighted imaging with TOAST stroke subtypes. Arch Neurol 60:1730–1734. doi:10.1001/archneur.60.12.1730
Navi BB, Singer S, Merkler AE, Cheng NT, Stone JB, Kamel H, Iadecola C, Elkind MS, DeAngelis LM (2014) Cryptogenic subtype predicts reduced survival among cancer patients with ischemic stroke. Stroke 45:2292–2297. doi:10.1161/STROKEAHA.114.005784
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The Florence Gould Endowment for Discovery in Stroke and an NIH award administered to BN (KL2TR000458-06).
Author information
Authors and Affiliations
Corresponding author
Additional information
Alexander E. Merkler and Babak B. Navi have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Merkler, A.E., Navi, B.B., Singer, S. et al. Diagnostic yield of echocardiography in cancer patients with ischemic stroke. J Neurooncol 123, 115–121 (2015). https://doi.org/10.1007/s11060-015-1768-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-1768-3