Abstract
Type 2 diabetes mellitus (DM) and obesity are known risk factors for poor outcomes in patients with systemic malignancies but are not well-studied in the brain tumor population. In this study we asked if type 2 DM and elevated body mass index (BMI) are independent risk factors for poor prognosis in patients with high-grade glioma (HGG.). We conducted a retrospective cohort study of 171 patients surgically treated for HGG at a single institution. BMI and records of pre-existing type 2 DM were obtained from medical histories. Variables associated with survival in a univariate analysis were included in the multivariate Cox model if P < 0.10. Variables with probability values >0.05 were then removed from the multivariate model in a step-wise fashion. Mean age at diagnosis was 55.0 ± 17.3 years. Fifteen (8.8%) patients had a history of type 2 DM. Fifty-eight (35.8%) patients had a BMI < 25, 55 (34.0%) BMI 25–30, and 49(30.2%) BMI > 30. Radiation therapy, temozolomide, and higher KPS score were independently associated with prolonged survival while increasing age was associated with decreased survival. DM (P = 0.001) and increasing BMI (P = 0.003) were found to be independently associated with decreased survival. Diabetics had a decreased median overall survival (312 vs. 470 days, P = 0.003) and PFS (106 vs. 166 days, P = 0.04) compared to non-diabetics. Increasing BMI (<25, 25–30, and >30) was also associated with decreased median PFS: 195 vs. 165 vs. 143 days, respectively. Pre-existing DM and elevated BMI are independent risk factors for poor outcome in patients with HGG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
High-grade gliomas (HGG) are malignant primary brain tumors which have a poor prognosis even in the setting of aggressive multimodality therapy. The estimated 5 year survival rate for patients with this disease remains very low at 18% for patients with WHO Grade III tumors and <5% for patients with WHO Grade IV tumors, but within this population there is pronounced heterogeneity of outcomes [1, 2]. Understanding prognostic indicators is critical for accurate risk stratification and may highlight future targets for therapeutic interventions. Well-defined risk factors for early progression and shortened survival in patients with HGG include increasing age and decreasing performance status [3–8]. There is also recent evidence linking persistent hyperglycemia to poor outcomes in this population [9, 10].
Abnormal glucose metabolism and hyperinsulinemia have been implicated in neoplasia for some time. Type 2 diabetes mellitus (DM) has been associated with an elevated risk of a number of systemic malignancies including breast, colorectal, pancreatic, liver, and endometrial cancers, as well as lymphoma [11–16]. Elevated body mass index (BMI) is a measure of obesity and has also been demonstrated to be an independent risk factor for the development of a variety of systemic malignancies [17–19]. In addition, patients with pre-existing type 2 DM and those who are obese are not only more likely to develop cancer; they have also been shown to have a higher risk of mortality than non-diabetic and non-obese cancer patients [20, 21].
The links between type 2 DM, obesity, hyperinsulinemia and cancer development and progression are increasingly evident in studies of patients with systemic malignancies, but remain poorly defined in the brain tumor population. Evidence of an association between elevated BMI and risk of glioma development has been described in two large population studies [22, 23]. In addition, the insulin-like growth factor 1 (IGF-1) signaling pathway has been implicated in glioma proliferation and progression in vitro [24–26] and the over-activation of this pathway in states of hyperinsulinemia is well described. We sought to explore the clinical manifestations of this putative connection by analyzing the relative outcomes of patients with HGG and conditions associated with hyperinsulinemia: pre-existing type 2 diabetes and obesity.
Methods
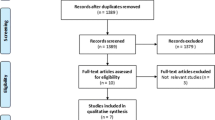
Patient population
We conducted a retrospective cohort study of 171 patients surgically treated for HGG (WHO Grade III and IV gliomas) at a single institution between 2003 and 2010. Two attending neurosurgeons with specialized training in neurosurgical oncology performed all tumor resections. The primary outcome was defined as survival, and progression-free survival (PFS) was evaluated as a secondary outcome.
Data collection
Records of clinical, radiographic, pathological, and operative data were retrospectively obtained from the electronic medical record. Inpatient and outpatient progress notes were available on all patients and were reviewed in all cases. Patient demographics, presenting signs and symptoms, performance status, prior medical conditions, extent of surgical resection, pathologic and radiographic details, peri-operative morbidity, adjuvant radiotherapy and chemotherapy regimens, date of radiographic progression, and date of death were each recorded. Tumor grade was confirmed by the neuropathologist’s assessment as WHO Grade III or IV in each case. Extent of resection was classified as gross-total or subtotal based on the interpretation of the immediate postoperative magnetic resonance imaging (MRI) scan by the neuroradiologist. Date of diagnosis was defined as the date of surgery and subsequent pathologic analysis. Date of progression was defined as the date of the first surveillance MRI scan demonstrating tumor progression/recurrence as interpreted by the neuroradiologist and neuro-oncologist in consensus. For patients in whom a date of death could not be confirmed, date of last contact was identified and they were recorded as lost to followup.
Preoperative anesthesia evaluations were used to obtain BMI, records of pre-existing DM, and lists of pre-admission medications. “Pre-existing DM” was defined as type 2 DM diagnosed by a physician using American Diabetes Association criteria at least 6 months prior to the patient’s presentation with an intracranial lesion. Laboratory tests, including blood glucose levels, were routinely obtained after surgical resection although the timing of these evaluations was not standardized. Peri-operative blood glucose was defined as the average of any values obtained after resection and prior to discharge from the hospital. Postoperative blood glucose was defined as the average of any values obtained in post-operative followup within 30–90 days of resection. Peri-operative hemoglobin A1C data was not available, as it was not routinely obtained in our practice. Prior to the analysis of data, normal BMI was defined as <25 kg/m2. Patients with a BMI of 25–30 were classified as overweight, and those with a BMI > 30 were classified as obese.
Statistical analysis
Survival and PFS as a function of time after resection were expressed as estimated Kaplan–Meier plots. Variables associated with survival in a univariate analysis were included in the multivariate Cox model if P < 0.10. Variables with probability values >0.05 were then removed from the multivariate model in a step-wise fashion.
Results
171 patients were evaluated in this study. 40 (23%) were diagnosed with WHO III astrocytoma, and 131 (77%) were diagnosed with WHO IV astrocytoma, or Glioblastoma Multiforme (GBM). The mean age at diagnosis was 55.0 ± 17.3 years. The median preoperative Karnofsky Performance Status (KPS) score was 70 (range 20–90) and postoperative score was 80 (range 20–100). 88 (51%) patients presented with a focal neurologic deficit, 44 (26%) with new-onset seizures, and 5 (3%) with incidentally diagnosed brain lesions. The remainder presented with non-specific complaints including headache and mental status changes. 37 (22%) patients underwent a gross-total resection (GTR.) 106 (62%) patients underwent a subtotal resection and 28 (16%) patients underwent a biopsy only as the tumor involved eloquent tissue and the surgeon determined that a substantial resection could not be achieved safely. After diagnosis, 152 (89%) patients received radiation therapy and 104 (63%) received temozolomide. 117 (82%) patients developed tumor progression and 118 (69%) died during the review period. 29 (17%) patients were lost to follow-up.
Within the study group as a whole, prognostic factors which were independently associated with prolonged survival included radiation therapy, temozolomide treatment, gross-total resection, and higher post-operative KPS score. Increasing age was associated with decreased survival. These findings are summarized in Table 1.
Data related to presence or absence of a previous diagnosis of DM was available for all patients. Fifteen (9%) patients had a pre-operative history of type 2 DM. There were no significant differences in rates of GTR, radiation, and temozolomide therapy between the diabetic and non-diabetic groups, as summarized in Table 2. After adjusting for independent prognostic factors (age, KPS score, GTR, temozolomide and radiation therapy) DM was independently associated with poor outcome. Diabetics had a decreased median OS (312 vs. 470 days, P = 0.003) and PFS (106 vs. 166 days, P = 0.04) compared to non-diabetics (Fig. 1.) There was no significant difference in mean BMI between the diabetic and non-diabetic patients (27.1 vs. 28.2, respectively, P = 0.48) and no significant differences in mean peri-operative or postoperative blood glucose levels in diabetics versus non-diabetics, as summarized in Table 3. No medication used for the treatment of diabetes was associated with a significant difference in outcome.
Pre-operative BMI values were available for 162 (95%) patients. 58 (36%) patients had a BMI < 25, 55 (34%) had a BMI 25–30, and 49 (30%) had a BMI > 30. After adjusting for independent prognostic factors (age, KPS score, GTR, temozolomide and radiation therapy) patients with higher BMI values demonstrated a decreased PFS. The median PFS for patients with BMI < 25 was 195 days, versus. 165 days for those with BMI 25–30 and 143 days for those with BMI > 30 (P = 0.003, Fig. 2). However, increased BMI had no significant association with OS. Patients with a BMI > 30 had a higher rate of GTR than patients with a BMI < 30 in our analysis, and rates of radiation and temozolomide therapy were equivalent between these groups, as summarized in Table 4.
Blood glucose levels obtained 30–90 days postoperatively were available on 111 (65%) patients. Postoperative hyperglycemia (BG > 180) was significantly associated with decreased OS (323 vs. 546 days, P = 0.01, Table 5). There was no significant difference in concurrent steroid dose between the normoglycemic and hyperglycemic groups. No differences in postoperative blood glucose levels were noted between diabetic and non-diabetic patients, as demonstrated in Table 3.
Discussion
The management of HGG is tremendously challenging. Despite advances in surgical techniques, radiation technologies, and targeted chemotherapy, the life expectancy of a patient diagnosed with HGG has improved only slightly over the last 15 years [2]. However, HGG remains a heterogenous disease and patients exhibit a wide variety of treatment responses. Stratification of patients by risk is critical to the effective analysis of clinical trials and is important when counseling individual patients about their prognosis. Additionally, identification of risk factors for early progression and death offers insights into potential avenues of novel therapeutic intervention.
In our analysis of 171 patients with HGG, we found that pre-existing type 2 DM was an independent risk factor for early progression and death. In concordance with previously published data, in our study population post-operative hyperglycemia was also associated with adverse outcome [10]. This finding was independent of concurrent steroid use. Interestingly, rates of postoperative hyperglycemia were equivalent between diabetics and non-diabetics in our analysis. In addition, we found that obesity was an independent risk factor for early tumor progression.
Obesity, diabetes, hyperglycemia and steroid use are clearly interrelated. In our study population, patients were frequently placed on steroids preoperatively for treatment of intracranial edema. The dose of steroids used was highly variable and related to the severity of the presenting symptoms and the practice patterns of individual referring physicians. In an attempt to limit related biases, we defined “pre-existing DM” conservatively as type 2 diabetes diagnosed at least 6 months prior to presentation and without concurrent steroid use. However, BMI was obtained at the time of pre-operative evaluation, and in some cases patients had been on oral steroids for a short period of time prior to this measurement. As steroid use may induce weight gain, BMI measurements may have been affected by this variable.
Previous studies have demonstrated a link between post-operative hyperglycemia and poor prognosis in this population. In our analysis we were able to validate this finding. Interestingly, there was no significant difference in average peri-operative or post-operative blood glucose levels between diabetic and non-diabetic patients in our population (Table 3). This implies that the pathologic process underlying the early progression and death of diabetic patients with HGG may not be related to glucose levels. Ideally, a more accurate metric for comparison would involve measurement of hemoglobin A1C levels, which give a more precise idea of overall glucose control than individual random glucose measurements. Unfortunately, hemoglobin A1C levels were not available for analysis in this study as they were not routinely recorded during peri-operative and post-operative evaluations. Future prospective collection and analysis of this data could help clarify the relationship between hyperglycemia and prognosis in patients with HGG.
We have demonstrated that type 2 DM and obesity are linked to poor prognosis in patients with HGG, independent of glycemic control. There is an intuitive link between these findings which relates to the state of hyperinsulinemia. Well-controlled type 2 diabetics as well as other obese patients may be normoglycemic while still experiencing high levels of circulating insulin. While this observational study does not allow us to ascribe a specific mechanism to our findings, our results support the hypothesis that hyperinsulinemia may promote tumor development and progression in some cases of HGG.
This pathophysiologic process is likely complex and may involve multiple metabolic pathways, but potential connections to the IGF-1 signaling pathway are particularly interesting. Patients with type 2 DM and patients who are obese have elevated levels of circulating insulin due to acquired insulin resistance. Under normal physiologic conditions, insulin mediates its actions through the insulin receptor but at increased concentrations it may also activate the insulin-like growth factor-1 receptor (IGF-1R) [27]. The IGF-1 pathway is involved in modulation of the cell cycle and thought to play an important role in tumor development in a variety of cell types, including astrocytes [28].
In 1999, Hirano et al. demonstrated that IGF-1 and its receptor are overexpressed by glioma cells, and that the degree of expression correlates with histopathologic grade and proliferation index as measured by Ki-67 labeling. These results suggest that IGF-1 pathway activation promotes astrocytic proliferation and malignant degeneration [28]. Subsequent investigators have demonstrated that overactivation of this pathway increases the invasive potential of GBM and is associated with a poor prognosis [26, 28–33]. Validation of this research has led to the development of experimental therapies aimed at IGF-1 pathway disruption through gene therapy or receptor inhibition, and some results have demonstrated that inhibition of this pathway may result in tumor regression in vitro [29, 34]. Recently, a somatostatin analog with activity against IGF-1 pathways has been demonstrated to have a potent inhibitory effect on glioblastoma growth in cell culture and xenograft models and the IGF-1R inhibitor picropodophyllin was shown to inhibit growth of glioblastoma cell lines in vitro and induce dramatic tumor regression in xenograft animals [35, 36]. These and other similar agents may represent exciting future experimental therapies for patients with GBM.
Despite this compelling biochemical evidence, few investigations into the link between the clinical manifestations of hyperinsulinemia—type 2 DM and obesity—and prognosis in patients with brain tumors have been conducted. Two population-based studies of risk factors for the development of gliomas of all grades have evaluated the relative risk of patients with elevated BMI. One demonstrated a significant increased risk for development of glioma in patients who were obese during adolescence [23]. In the Million Women Study conducted in the UK, obesity was associated with an increased risk of development of glioma, but this effect was not statistically significant [22]. However, neither study evaluated the relative risk of patients with type 2 DM, nor addressed the relative prognosis of obese patients diagnosed with glioma.
One analysis of the effect of BMI on survival in patients with GBM has been previously published. In 2010, Jones et al. [37] reported the results of their prospective analysis of patients treated for GBM at 2 centers from 1991 to 2008. Overall, they found a non-significant increase in risk of early mortality in obese patients. Their analysis relied on self-reports of height and weight, and was performed across a 17 year period during which treatment protocols for GBM changed significantly, and these factors are significant limitations in this study. In another important distinction, this group did not evaluate tumor progression as a secondary endpoint and did not evaluate the relative risk conferred by a pre-existing diagnosis of diabetes.
Our findings indicate that patients with HGG who are obese or are type 2 diabetics should be considered high risk. These findings are very relevant to the care of patients with HGG, as 7% of the US population has type 2 DM, and 34% of US adults are classified as obese (BMI > 30) [20, 38]. Several potential therapeutic interventions are suggested by our findings. First, weight loss, which has been shown to reduce insulin resistance in obese patients, may offer some benefit [39]. In addition, medications which reduce insulin resistance, reducing insulin levels, may be useful. There is growing evidence that metformin, a first-line agent for management of type 2 DM, may have antitumorigenic effects. Metformin is known to lower circulating levels of insulin, and has been shown to promote apoptosis in cancer cells in vitro via the AMP-activated protein kinase pathway [40, 41]. In a large cohort study conducted in Taiwan, Lee et al. [42] reported that type 2 diabetics had a significantly increased risk of developing colorectal, liver, and pancreatic cancer, but that diabetics treated with metformin had a risk which was not significantly different than non-diabetics. Several diabetic patients in our study took metformin, and we did not see a difference in outcome when compared to other diabetic patients. However, our study was likely under-powered to detect a potential association of this kind and larger studies evaluating this potential effect as well as those employing inhibitors of the IGF-1 pathway should be considered.
Conclusion
In our analysis, pre-existing type 2 DM and obesity are each independent risk factors for poor outcome in patients with HGG. The clinical variables of pre-existing type 2 DM and elevated BMI should be considered when stratifying risk for patients with HGG. Future collection and analysis of hemoglobin A1C values would be useful in clarifying the connection between hyperglycemia and prognosis in HGG. In addition, prospective trials targeting control of hyperinsulinemia in this population should be considered and further study of the clinical effect of therapy with medications modulating insulin levels as well as IGF-1R inhibitors encouraged.
References
Central Brain Tumor Registry of the United States (2011) CBTRUS Statistical Report: Primary brain and central nervous system tumors diagnosed in the United States in 2004–2007
Tait MJ, Petrik V, Loosemore A, Bell BA, Papadopoulos MC (2007) Survival of patients with glioblastoma multiform has not improved between 1993 and 2004: analysis of 625 cases. Br J Neurosurg 21:496–500
Buckner JC (2003) Factors influencing survival in high-grade gliomas. Semin Oncol 30:10–14
Burger PC, Green SB (1987) Patient age, histologic features, and length of survival in patients with glioblastoma multiforme. Cancer 59:1617–1625
Lamborn KR, Chang SM, Prados MD (2004) Prognostic factors for survival of patients with glioblastoma: recursive partitioning analysis. Neuro Oncol 6:227–235
Laws ER, Parney IF, Huang W, Anderson F, Morris AM, Asher A et al (2003) Survival following surgery and prognostic factors for recently diagnosed malignant glioma: data from the glioma outcomes project. J Neurosurg 99:467–473
Perry A, Jenkins R, O’Fallon JR et al (1999) Clinicopathologic study of 85 similarly treated patients with anaplastic astrocytic tumors. An analysis of DNA content (ploidy), cellular proliferation, and P53 expression. Cancer 86:672–683
Tortosa A, Vinolas N, Villa S et al (2003) Prognostic implication of clinical, radiologic, and pathologic features in patients with anaplastic gliomas. Cancer 97:1063–1071
Derr RL, Ye X, Islas MU, Desideri S, Saudek CD, Grossman SA (2009) Association between hyperglycemia and survival in patients with newly diagnosed glioblastoma. J Clin Oncol 27:1082–1086
McGirt MJ, Chaichana KL, Gathinji M, Attenello F, Than K, Ruiz AJ, Olivi A, Quinones-Hinojosa A (2008) Persistent outpatient hyperglycemia is independently associate with decreased survival after primary resection of malignant brain astrocytomas. Neurosurgery 62:286–289
El-Serag HB, Hampel H, Javadi F (2006) The association between diabetes and hepatocellular carcinoma: a systematic review of epidemiologic evidence. Clin Gastroenterol Hepatol 4:369–380
Friberg E, Orsini N, Mantzoros CS, Wolk A (2007) Diabetes mellitus and risk of endometrial cancer: a meta-analysis. Diabetologia 50:1365–1374
Huxley R, Ansary-Moghaddam A, Berrington de Gonzalez A, Barzi F, Woodward M (2005) Type 2 diabetes and pancreatic cancer: a meta-analysis of 36 studies. Br J Cancer 92:2076–2083
Larsson SC, Mantzoros CS, Wolk A (2007) Diabetes mellitus and risk of breast cancer: a meta-analysis. Int J Cancer 121:856–862
Larsson SC, Orsini N, Wolk A (2005) Diabetes mellitus and risk of colon cancer: a meta-analysis. J Natl Cancer Inst 97:1679–1687
Mitri J, Castillo J, Pittas AG (2008) Diabetes and risk of non-hodgkins lymphoma: a metaanalysis of observational studies. Diabetes Care 31:2391–2397
Calle EE, Kaaks R (2004) Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer 4:579–591
Calle EE, Rodriquez C, Walker-Thurmond K, Thun MJ (2003) Overweight, obesity and mortality from cancer in a prospectively studied cohort of US adults. NEJM 348:1625–1638
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M (2008) Body mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371:569–578
Barone BB, Yeh HC, Snyder CF, Peairs KS, Stein KB, Derr RL, Wolff AC, Brancati FL (2008) Long-term all-cause mortality in cancer patients with pre-existing diabetes mellitus. JAMA 300:2754–2764
Haydon AM, Macinnis RJ, English DR, Giles GG (2006) Effect of physical activity and body size on survival after diagnosis with colorectal cancer. Gut 55:62–67
Benson VS, Pirie K, Green J, Casabonne D, Beral V, Million Women Study Collaborators (2008) Lifestyle factors and primary glioma and meningioma tumors in the million women study cohort. Br J Cancer 99:185–190
Moore SC, Rajaraman P, Dubrow R et al (2009) Height, body mass index, and physical activity in relation to glioma risk. Cancer Res 69:8349–8355
Belfiore A, Frasca F, Pandini G, Sciacca L, Vigneri R (2009) Insulin receptor isoforms and insulin receptor/insulin-like growth factor receptor hybrids in physiology and disease. Endocr Rev 30:586–623
Trojan J, Cloix JF, Ardourel MY, Chatel M, Anthony DD (2007) Insulin-like growth factor type 1 biology and targeting in malignant gliomas. Neuroscience 145:795–811
Wang H, Wang H, Shen W et al (2003) Insulin-like growth factor-binding protein 2 enhances GBM invasion by activating invasion-enhancing genes. Cancer Res 63:4315–4321
Lammers R, Gray A, Schlessinger J, Ulrich A (1989) Differential signalling potential of insulin and IGF-1 receptor cytoplasmic domains. EMBO J 8:1369–1375
Hirano H, Lopes MB, Laws ER et al (1999) Insulin-like growth factor 1 content and pattern of expression correlates with histopathologic grade in diffusely infiltrating astrocytomas. Neuro Oncol 1:109–119
Zumkeller W, Westphal M (2011) The IGF/IGFBP system in CNS malignancy. Mol Pathol 54:227–229
McDonald KL, O’Sullivan MG, Parkinson JF et al (2007) IQGAP1 and IGFBP2: valuable biomarkers for determining prognosis in glioma patients. J Neuropathol Exp Neurol 66:405–417
Sallinen SL, Sallinen PK, Haapasalo HK et al (2000) Identification of differentially expressed genes in human gliomas by DNA microarray and tissue chip techniques. Cancer Res 60:6617–6622
Santosh V, Arivazhagan A, Sreekanthreddy P et al (2010) Grade-specific expression of insulin-like growth factor-binding proteins 2, 3 and 5 in astrocytomas: IGFBP-3 emerges as a strong predictor of survival in patients with newly diagnosed glioblastoma. Cancer Epidemiol Biomarkers Prev 19:1399–1408
Wang H, Fuller GN, Zhang W (2004) Insulin-like growth factors and insulin-like growth factors binding proteins in CNS tumors. In: Zhang W, Fuller GN (eds) Genomic and molecular neurooncology. Jones and Bartlett, Sudbury, pp 119–130
Gariboldi MB, Ravizza R, Monti E (2010) The IGFR1 inhibitor NVP-AEW541 disrupts a pro-survival and pro-angiogenic IGF-STAT-HIF1 pathway in human glioblastoma cells. Biochem Pharmacol 80:455–462
Pozsgai E, Schally AV, Halmos G, Rick F, Bellyei S (2010) The inhibitory effect of a novel cytotoxic somatostatin analog AN-162 on experimental glioblastoma. Horm Metab Res 42:781–863
Yin S, Girnita A, Stromberg T, Khan Z, Andersson S, Zheng H, Ericsson C, Axelson M, Nister M, Larsson O, Ekstrom TJ, Girnita L (2010) Targeting the insulin-like growth factor-1 receptor by picropodophyllin as a treatment option for glioblastoma. Neuro Oncol 12:19–27
Jones LW, Ali-Osman F, Lipp E, Marcello JE, McCarthy B, McCoy L, Rice T, Wrensch M, Il’yasova D (2010) Association between body mass index and mortality in patients with glioblastoma multiforme. Cancer Causes Control 21:2195–2201
Shields M, Carroll MD, Ogden CL (2011) Adult obesity prevalence in Canada and the United States. NCHS Data Brief, Centers for Disease Control
Dube JJ, Amati F, Toledo FG, Stefanovic-Racic M, Rossi A, Coen P, Goodpaster BH (2011) Effects of weight loss and exercise on insulin resistance, and intramyocellular triacylglycerol, diacylglycerol, and ceramide. Diabetologia 5:1147–1156
Kourelis TV, Siegel RD (2011) Metformin and cancer: new applications for an old drug. Med Oncol. doi:10.1007/s12032-011-9846-7
Micic D, Cvijovic G, Trajkovic V, Duntas LH, Polovina S (2011) Metformin: its emerging role in oncology. Hormones 10:5–15
Lee MS, Hsu CC, Wahlqvist ML, Tsai HN, Chang YH, Huang YC (2011) Type 2 diabetes increases and metformin reduces total, colorectal, liver and pancreatic cancer incidences in Taiwanese representative population prospective cohort study of 800, 000 individuals. BMC Cancer 11:20
Acknowledgments
The authors wish to acknowledge Merry Beth Braswell, Aimee Cutrer, and Daniel Brill for their assistance in collection and maintenance of the clinical database used in this study and Kyle Weaver MD for his contribution of patients for analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chambless, L.B., Parker, S.L., Hassam-Malani, L. et al. Type 2 diabetes mellitus and obesity are independent risk factors for poor outcome in patients with high-grade glioma. J Neurooncol 106, 383–389 (2012). https://doi.org/10.1007/s11060-011-0676-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-011-0676-4