Abstract
The aim of this study was to evaluate tooth crown size in patients with cleft lip and palate (CLP), right cleft lip and palate (RCLP), and left cleft lip and palate (LCLP) subtypes and compare them between each other and between class I control group. A total of 110 patients, 55 patients’ records with CLP (28 male, 27 female) and the same number of 55 patients’ records with class I (27 male, 28 female) as control group, have been included. All plaster models were scanned with dental scanner and then analyzed using digital program to measure tooth size. When comparing right and left side of LCLP group, mesio-distal (MD) and labio-lingual (LL) dimensions of the centrals have the significant difference, where the largest dimensions were the right centrals (p < 0.05). When comparing right and left side of RCLP group, labio-lingual (LL) dimensions of the canines have the significant difference, where the largest dimensions were the right canines (p < 0.05). In class I group, there were no significant differences between right and left sides. There was a significant mean difference in Centrals MD, Centrals LL, and Canines LL (p < 0.05) between all groups when comparing the right sides and left sides alone, where class I group has the largest mean between all groups. Cleft lip and palate patients were noticed to have significant dental anomalies that affect the number, shape, and size of the teeth. These anomalies can impair function and affect the psychology of the patients. Therefore, a dental analysis focusing on restoring the esthetics as much as function should be considered when treating these patients. Dental materials with nanoparticles ranged from 1 to 100 nm showed to have better integration with dental tissues and the future of nanotechnology is very exciting in dental practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Orofacial clefts, which include cleft lip, cleft palate, and cleft lip and palate, resemble a range of disorders affecting the lips and oral cavity of which the causes remain largely unknown. Effects on speech, hearing, appearance, and psychology can lead to long-lasting adverse outcomes for health and social integration. Affected children have higher morbidity and mortality throughout life than do unaffected individuals where they need multidisciplinary care––nursing, plastic surgery, maxillofacial surgery, speech therapy, audiology, psychology, genetics, orthodontics, and dentistry––from birth until adulthood to manage the condition (Christensen et al. 2004; Ngai et al. 2005; Jaksˇić et al. 2002)
Around the 6th week of embryogenesis, the medial nasal processes fuse with one another and with the maxillary processes on each side leads to the formation of the upper lip and the primary palate. The paired palatal shelves, which initially grow vertically down the sides of the developing tongue, rise to a horizontal position above the tongue and come into contact and fuse to form the secondary palate, which happens around the 8th week of embryogenesis. Then the secondary palate fuses with the primary palate and the nasal septum. These fusion processes are complete by the 10th week of embryogenesis. Any insult during these periods can disrupt the development processes resulting in clefts of the lip or/and palate (Mitchell 2007).
With improved ultrasound screening, the management of this condition starts prenatally by early detection which allows the parents to be counseled and prepared for the arrival of the child. Since a child with CLP will have difficulty sucking milk, suitable bottles are now available for babies with clefts. Some centers use acrylic plates designed to help feed the baby. Lip repair surgery usually is done by the age of 3 months. At 9 months, hard and soft palate repair is undertaken to separate the nasal cavity from the oral cavity and to facilitate normal velopharyngeal function and closure for comprehensible speech. Before the time of permanent upper canine eruption at 9–10 years old, an alveolar bone grafting surgery is carried out to provide an intact arch to allow canine eruption (Mitchell 2007).
Since CLP patients deal with a considerable physiological and psychological impairment during a long period of their lives and since the physiological damage is due to their upper palate, upper arch and/or upper lip is considerably large; this study aims to test the theory that CLP would not only affect the surrounding tissues of the maxillary teeth but also the teeth. To do that, we collected digital models of CLP patients’ casts and compared them with normal patients’ casts.
Materials and methods
We examined the pretreatment orthodontic digital dental casts of 110 patients, divided into 3 groups: group 1, ULCLP (41 subjects: 21 males, 20 females; mean age, 17.5 years); group 2, URCLP (14 subjects: 7 males, 7 females; mean age, 16.9 years); and group 3 (control) class I (55 subjects: 27 males, 28 females; mean age, 15.6 years). The control group included those with class I occlusion, proper overjet and overbite, well-aligned dental arches, normal dentoskeletal pattern, and harmonious profile, with minor or no crowding.
All patients were adolescents in the permanent dentition stage. All plaster casts of CLP patients were selected from the archives of the Department of Orthodontics at Ankara University in Turkey. Plaster casts of (class I) patients were selected from the archives of the Department of Orthodontics at the Near East University in TRNC. Only Caucasian patients with good-quality dental casts were included. Casts with large restorations or crowns were excluded from the study.
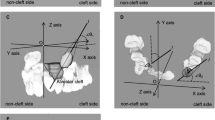
All plaster casts were scanned using an intraoral scanner (3Shape TRIOS® 3 intraoral scanner). Measurements were done by using a digital software (3Shape Ortho Viewer. Ink) according to the method of Hunter and Priest (Stuart Hunter and Priest 1960), as follows: MD, the longest distance between the anatomic mesial to the distal contact point; LL (diameter), measured the longest distance between the labial and lingual surface of the tooth perpendicular to the MD axis of the tooth (Figs. 1 and 2). The same examiner (A.I.) made all the measurements to eliminate interexaminer variability.
Statistical analysis
Statistical analyses were performed using SPSS software version 25. Descriptive analyses were presented using means, standard deviations, median, minimum, and maximum values for continuous data. The variables are investigated using the Kolmogorov-Smirnov test to determine whether or not they are normally distributed. Homogeneity of the variances between the groups was tested by Leneve’s test. Since the variables were normally distributed, two independent samples t test was used to compare the affected and not affected groups. Since the variables are not normally distributed, the Mann-Whitney U test was used to compare these groups. Since the variables are normally distributed and variances are homogeneous, an ANOVA test was used to compare three groups’ means. If the variances are not homogenous, the Welch ANOVA was used to compare three group’s means. Tukey’s or Dunnett’s T3 test which is appropriate was performed to test the significance of pairwise differences. Since the variables are not normally distributed, the Kruskal-Wallis test was conducted to compare the medians of three groups. The Mann-Whitney U test was performed to test the significance of pairwise differences using the Bonferroni correction adjusting for multiple comparisons. A 5% type-I error level was used to infer a statistical significance.
Results
We found 17% of the teeth were congenitally absent in the CLP groups. In the RCLP group, mostly laterals were absent with a percentage of 64%. And in the LCLP group, also laterals were absent with a percentage of 85% with canines and second premolars next with 29%. Also, several malformation of the teeth has been noticed; 83 teeth of a total of 546 teeth of the CLP groups were malformed. Enamel hypoplasia was mostly noticed, then followed by peg-shaped teeth mostly laterals and polydiastima (spacing of the teeth). And the less noticed are supernumerary teeth, macrodontia, and mulberry molars.
In group 1, there is only a statistically significant mean difference between the right and left centrals’ mesiodistal and between right and left centrals’ labiolingual measurements between affected and not affected sides p < 0.05. In these measurements, not affected (right) side has a higher mean than the affected (left) side (Table 1).
In group 2, there is only a statistically significant mean difference in the right and left canines’ labiolingual measurement between the affected and not affected sides p < 0.05. In this measurement, the affected (right) side has a higher mean than the not affected (left) side (Table 2).
In group 3, there is no statistically significant mean difference between the right side and left side (p > 0.05). Table 3 shows the values of mesiodistal and labiolingual measurements of the right and left sides of class III (control group).
When comparing the (right) sides between all three groups, we found a statistically significant mean difference in centrals’ mesiodistal, centrals’ labiolingual, and canines’ labiolingual measurements between groups (p < 0.05). And pairwise comparisons between groups were evaluated by the Mann-Whitney U test. The Bonferroni adjustment was done to the p values for centrals’ mesiodistal measurement. For centrals’ mesiodistal measurement, there was a statistically significant difference between group 2 and group 3 (p = 0.000), and group 1 and group 3 (p = 0.023). Group 3 mean was higher than in other groups. For centrals’ labiolingual and canines’ labiolingual measurements, pairwise comparisons between groups were evaluated by Dunnett’s T3 test. For 11 labiolingual measurements there was a statistically significant difference between group 2 and group 3 (p = 0.019), and group 1 and group 3 (p = 0.015). Group 3 mean was higher than in other groups. For canines’ labiolingual measurement, there was a statistically significant difference between group 2 and group 3 (p = 0002), and group 1 and group 3 (p = 0.004). Group 3 mean was higher than in other groups (Table 4).
When comparing the left sides between all three groups, we found a statistically significant mean difference in centrals’ mesiodistal, centrals’ labiolingual, and canines’ labiolingual measurements between groups p < 0.05. For centrals’ mesiodistal measurement, pairwise comparisons between groups were evaluated by the Tukey test. For centrals’ mesiodistal measurement, there was a statistically significant difference between group 1 and group 3 (p = 0.000). Group 3 mean was higher than in other groups. For centrals’ labiolingual and canines’ labiolingual measurements, pairwise comparisons between groups were evaluated by Dunnett’s T3 test. For centrals’ labiolingual measurement, there was a statistically significant difference between group 1 and group 3 (p = 0.001). Group 3 mean was higher than in other groups. For canines’ labiolingual measurement, there was a statistically significant difference between group 1 and group 3 (p = 0.020). Group 3 mean was higher than in other groups (Table 5).
Discussion
In our study, we chose patients in class I as the control group because they represent an ideal occlusion, to minimize the dental malocclusion and malformation found in class II and class III as some literatures have claimed (Cua-Benward et al. 1992; Mitchell 2007; Sassouni 1969). And as the contradictory results in different literatures which some found that there are no differences in malocclusion as an effect of gender and some found that there is sexual dimorphism as larger teeth in males than females, Lavelle (1972) and Foster and Lavelle (1971) who reported significantly larger dimensions of several teeth in females than in males, we decided not to divide the sample to subgroups according to patients’ gender, where general researches reported smaller teeth in CLP patients, which might be explained by the compromised growth that occurs in CLP patients, where these patients’ maxilla is found to be in class III relationship due to inadequate growth (Werner and Harris 1989; Nie and Lin 1999; Al-Khateeb et al. 2006; Bishara et al. 1989)
Leifert et al. (2009) and the vast majority of literatures reporting about the 3D models’ accuracy and reproducibility of plaster models and the accuracy of 3D analyzing programs, we preferred to use digital scanner and digital program in our study. Mullen et al. (2007) and Răducanu (2015) compared between a digital program and a plaster model when analyzing Bolton ratios and arch length to determine accuracy and speed (Araujo and Souki 2003; Basaran et al. 2006). They found that there is no significant difference between the two methods in accuracy, and the digital program can produce accurate measurements as close as the traditional method, where they found speed wise that digital program is faster than the traditional method (Kasparova et al. 2013). Keating et al. (2008) evaluate the accuracy and reproducibility of 3D scanning device compared with traditional method using digital clippers. Their method was to scan the plaster models and analyze both plaster and digital models, and then reproduce the models using a 3D printer and analyzing the measurements again. He found no statistical difference between the original plaster models and 3D models, but he found a significant difference in the reproduced models compared with the original plaster models (Asquith and McIntyre 2012; Kusnoto and Evans 2002).
Nanotechnology is an emerging field that is rapidly developing and recently has brought massive changes to medicine and dentistry and can change medical and dental practices furthermore in the near future. Nanotechnology has been used with some significant success in the development of restorative materials in dentistry where they improved the biointegration of the restorative materials with the dental tissues. Nanoparticles have been also incorporated into dental composites or dental adhesives to inhibit bacterial growth and disrupt the biofilm formation on tooth surfaces to act as an antibacterial agent. Nanotechnology also proved to help in delivering medication and analgesic drugs to specific areas to help treat oral cancers and reduce pain accurately. Dental tissue repair and regeneration are found to be possible with the help of nanotechnologies where combining the technologies of scaffold matrices with the regenerative power of stem cells gave the ability to engineer tissues that mimic the dental tissues. Nanotechnology offers a huge success in improving dental materials like composites, sealers, and other dental materials. A range of synthetic nanoparticles such as hydroxyapatite, bioglass, titanium, zirconia, and silver nanoparticles ranging from 1 to 100 nm are proposed for dental restoration, where now treating dental hypersensitivity and providing better root canal sealing is possible (Abou Neel et al. 2015). The might of nanotechnology combined with additive manufacturing (3D printing) is soon to be realized. 3D printing with nanoscale materials ranging from 1 to 100 nm will produce better restorations, splints, mouthguards, more accurate diagnostic models, and better dental materials in general (Hales et al. 2020). Nanotechnology offers a promising future in preventive and regenerative dentistry. In the near future, we could be able to complete orthodontic realignment in a single visit or even regenerate missing teeth all with the help of nanotechnology. Another emerging technology in the field of dentistry is the Internet of things (IoT) and it is easy to predict the novelties of this new aspect of the technology in dentistry. This new domain can be used to improve the dentist’s office to make it way less intimidating to patients. Connected thermometers, music stations, VR glasses, smart walls, or even ceilings can be used to create a comfortable atmosphere for a patient according to their preferences and even stress levels. This new technology benefits from the cloud-based network to help prevention and management of diseases by monitoring patients at all times using wireless sensors, cameras, or other input devices (Konstantinidis et al. 2015). Computer-aided design/computer-aided manufacturing (CAD/CAM), 3-dimensional (3D) printing, cone beam computed tomography (CBCT), digital records, digital radiography, digital impressions, and teledentistry all are digital technologies utilized nowadays in dentistry that help in diagnoses, treatment, and monitoring patients and could be part of the IoT network in dental practice (Salagare and Prasad 2020).
The 3D scanning device that been used in this study to collect the materials has the ability to be integrated into the IoT network and also could be used with a 3D printer with nanoscale ability to produce more accurate models on the nanoscale level. The collected data could be shared with ease anywhere anytime with the IoT network to be analyzed, stored, and used to treat and monitor patients. After scanning the plaster casts, a digital copy will be saved to the system. This digital copy could be sent to any clinic in the world via the IoT network to be analyzed; after being analyzed, a diagnosis and treatment plan will be created. Afterwards, the treatment plan could be carried out after the patients’ consent. As an example of treatments that could be carried out in orthodontics, clear aligners depend on this new technology. The scanned cast will be analyzed by an orthodontic professional to give a treatment prescription. Then, a 3D printer will produce this prescription by printing 3D models to be used to manufacture a specific set of clear aligners to treat the patient (Dawood et al. 2015).
Most literatures included occlusal-gingival (OG) width in their studies where labial-palatal or labial-lingual width had less attention by researchers which made us to include this measurement rather than occlusal-gingival width in our research. Ngai (2005) reported statistically significant differences between premolar and first molar OG width between the CLP and class I groups. The right lateral incisor OG width in the RCLP group was found to be statistically smaller than that of the class I group. The left lateral incisor and left canine OG width were smallest in the LCLP group and significantly smaller than in the control group. The right lateral incisor OG width was smallest in the RCLP group and statistically smaller when compared with the class I group.
Akcam (2008) found that there were differences in the right first and second premolar MD dimensions between the LCLP group and the class I group and between the RCLP group and the class I group. The class I group had smaller MD dimensions than both RCLP and LCLP groups. They found that left lateral incisor MD dimensions in LCLP group were smaller than those of the RCLP and the control group, where they did not find any deference between right lateral incisors in the RCLP group and the control group. And they found that all LL dimensions in the incisor region (canine to canine) in the CLP groups were smaller than in the class I control group. In our study, we found for the LL measurements of centrals and canines were statistically significant. Surprisingly, we did not find any significant difference in the low number of laterals that were not absent. And also, we did not find any significant difference in the first and second premolars between CLP groups and the class I group (Menezes and Vieira 2008).
Ranta (1986) and other studies (Camporesi et al. 2010) reported that CLP patients have higher incidences of hypodontia in both jaws and especially the deciduous and permanent lateral in the cleft region. And also, the timing of tooth formation and eruption in the permanent dentition is delayed in children from all cleft groups compared with noncleft children. It is also reported that the size of the permanent teeth in CLP patients is smaller than in noncleft children, and enamel defects and abnormalities in shape and size of both deciduous and permanent teeth are far more common in patients affected with CLP than in normal subjects. Our findings are mostly compatible with these findings. We found higher rates of hypodontia of the teeth in CLP patients than in class I patients especially the lateral incisor in the CLP region. We also found that CLP patients are highly affected by hypoplasia more than class I patients. We have noticed more incidents of malformed, misshaped teeth in CLP patients compared with the class I normal patients, such as supernumerary and peg-shaped teeth (Akcam et al. 2010; Paranaiba et al. 2013; Smith et al. 2000; Wangpichit et al. 2001).
In this study, the biggest challenge and even a limitation was the low number of CLP patient records. Even with the low number of records, we found there were a number of cases where the record was damaged and unusable in our research. Some of the records had large restoration or carious lesions and all of these records were disclosed. Also, the high number of missing lateral teeth could affect the accuracy of the results.
Conclusion
This study revealed that:
-
a high frequency of dental anomalies in number, size, and shape such as (tooth hypodontia, supernumerary teeth, enamel hypoplasia, and misshaped teeth).
-
In LCLP, MD, and LL dimensions of the right centrals were greater than the left centrals.
-
In RCLP, all LL dimensions of the right canines were greater than the left canines.
-
MD and LL dimensions of the centrals and the LL dimensions of the canines were greater in the control group compared with the other groups.
-
Dental-size analysis should be included in planning orthodontic treatment.
-
Technology use is growing rapidly in orthodontics and dental fields in general, where they can provide faster more practical solutions to professionals. And we believe they should be incorporated in clinics. Dental practice and orthodontics specifically will hugely benefit from both nanotechnology and IoT technology.
Change history
12 August 2021
A Correction to this paper has been published: https://doi.org/10.1007/s11051-021-05224-2
References
Abou Neel EA, Bozec L, Perez RA, Kim HW, Knowles JC (2015) Nanotechnology in dentistry: prevention, diagnosis, and therapy. Int J Nanomedicine 10:6371
Akcam MO, Toygar TU, Özer L, Özdemir B (2008) Evaluation of 3-dimensional tooth crown size in cleft lip and palate patients. Am J Orthod Dentofac Orthop 134(1):85–92
Akcam MO, Evirgen S, Uslu O, Memikoğlu UT (2010) Dental anomalies in individuals with cleft lip and/or palate. Eur J Orthodontics 32(2):207–213
Al-Khateeb SN, Abu Alhaija ES (2006) Tooth size discrepancies and arch parameters among different malocclusions in a Jordanian sample. Angle Orthodontist 76(3):459–465
Araujo E, Souki M (2003) Bolton anterior tooth size discrepancies among different malocclusion groups. Angle Orthodontist 73(3):307–313
Asquith JA, McIntyre GT (2012) Dental arch relationships on three-dimensional digital study models and conventional plaster study models for patients with unilateral cleft lip and palate. Cleft Palate-craniofac J 49(5):530–534
Basaran G, Selek M, Hamamcı O, Akkuş Z (2006) Intermaxillary Bolton tooth size discrepancies among different malocclusion groups. Angle Orthodontist 76(1):26–30
Bishara SE, Jakobsen JR, Treder JE, Stasl MJ (1989) Changes in the maxillary and mandibular tooth size-arch length relationship from early adolescence to early adulthood: a longitudinal study. Am J Orthod Dentofac Orthop 95(1):46–59
Camporesi M, Baccetti T, Marinelli A, Defraia E, Franchi L (2010) Maxillary dental anomalies in children with cleft lip and palate: a controlled study. Int J Paediatr Dent 20(6):442–450
Christensen K, Juel K, Herskind AM, Murray JC (2004) Long term follow up study of survival associated with cleft lip and palate at birth. Bmj 328(7453):1405
Cua-Benward GB, Dibaj S, Ghassemi B (1992) The prevalence of congenitally missing teeth in class I, II, III malocclusions. J Clin Pediatr Identistry 17(1):15–17
Dawood A, Marti BM, Sauret-Jackson V, Darwood A (2015) 3D printing in dentistry. Br Dent J 219(11):521–529
Foster TD, Lavelle CB (1971) The size and dentition in complete cleft lip and palate. Cleft Palate J 8(2):177–184
Hales S, Tokita E, Neupane R, Ghosh U, Elder B, Wirthlin D, Kong YL (2020) 3D printed nanomaterial-based electronic, biomedical, and bioelectronic devices. Nanotechnology 31(17):172001
Jaksˇić N, Sˇćepan I, Glisˇić B, Stamenic E, Stamenković Z (2002) Mesiodistal size of deciduous teeth in subjects with unilateral cleft lip and palate. Orthod Craniofacial Res 5(1):17–21
Kasparova M, Grafova L, Dvorak P, Dostalova T, Prochazka A, Eliasova H, Prusa J, Kakawand S (2013) Possibility of reconstruction of dental plaster cast from 3D digital study models. Biomed Eng Online 12(1):49
Keating AP, Knox J, Bibb R, Zhurov AI (2008) A comparison of plaster, digital and reconstructed study model accuracy. J Orthod 35(3):191–201
Konstantinidis EI, Bamparopoulos G, Billis A, Bamidis PD (2015) Internet of things for an age-friendly healthcare. In MIE (pp. 587-591)
Kusnoto B, Evans CA (2002) Reliability of a 3D surface laser scanner for orthodontic applications. Am J Orthod Dentofac Orthop 122(4):342–348
Lavelle CLB (1972) Maxillary and mandibular tooth size in different racial groups and in different occlusal categories. Am J Orthod Dentofac Orthop 61(1):29–37
Leifert MF, Leifert MM, Efstratiadis SS, Cangialosi TJ (2009) Comparison of space analysis evaluations with digital models and plaster dental casts. Am J Orthod Dentofac Orthop 136(1):16–e1
Menezes R, Vieira AR (2008) Dental anomalies as part of the cleft spectrum. Cleft Palate-Craniofac J 45(4):414–419
Mitchell L (2007) An introduction to orthodontics. Oxford University Press, Oxford
Mullen SR, Martin CA, Ngan P, Gladwin M (2007) Accuracy of space analysis with emodels and plaster models. Am J Orthod Dentofac Orthop 132(3):346–352
Ngai CW, Martin WL, Tonks A, Wyldes MP, Kilby MD (2005) Are isolated facial cleft lip and palate associated with increased perinatal mortality? A cohort study from the West Midlands region, 1995–1997. J Matern Fetal Neonatal Med 17(3):203–206
Nie Q, Lin J (1999) Comparison of intermaxillary tooth size discrepancies among different malocclusion groups. Am J Orthod Dentofac Orthop 116(5):539–544
Paranaiba LMR, Coletta RD, Swerts MSO, Quintino RP, De Barros LM, Martelli-Júnior H (2013) Prevalence of dental anomalies in patients with nonsyndromic cleft lip and/or palate in a Brazilian population. Cleft Palate-Craniofac J 50(4):400–405
Răducanu AM, Didilescu AC, Feraru IV, Dumitrache MA, Hănţoiu TA, Ionescu E (2015) Considerations on morphological abnormalities of permanent teeth in children with cleft lip and palate. Romanian J Morphol Embryol 56(2):453–457
Ranta R (1986) A review of tooth formation in children with cleft lip/palate. Am J Orthod Dentofac Orthop 90(1):11–18
Salagare S, Prasad R (2020) An overview of internet of dental things: new frontier in advanced dentistry. Wirel Pers Commun 110(3):1345–1371
Sassouni V (1969) A classification of skeletal facial types. Am J Orthod 55(2):109–123
Smith SS, Buschang PH, Watanabe E (2000) Interarch tooth size relationships of 3 populations: “does Bolton’s analysis apply?”. Am J Orthod Dentofac Orthop 117(2):169–174
Stuart Hunter W, Priest WR (1960) Errors and discrepancies in measurement of tooth size. J Dent Res 39(2):405–414
Wangpichit K, Huntington NL, Kapala JT (2001) Comparison of three nonradiographic methods of mixed dentition analysis in cleft lip and palate patients. Pediatr Dent 23(6):476–480
Werner SP, Harris EF (1989) Odontometrics of the permanent teeth in cleft lip and palate: systemic size reduction and amplified asymmetry. Cleft Palate J 26(1):36–41
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
This article is part of the topical collection: Role of Nanotechnology and Internet of Things in Healthcare
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been retracted. Please see the retraction notice for more detail: https://doi.org/10.1007/s11051-021-05224-2
About this article
Cite this article
Idrys, A., Kamiloğlu, B. & Altuğ, A.T. RETRACTED ARTICLE: A multicenter retrospective 3D study of cleft lip and palate casts to evaluate dental shape, size, and anomalies in eruption around the cleft area before fixed orthodontic treatment. J Nanopart Res 22, 213 (2020). https://doi.org/10.1007/s11051-020-04937-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11051-020-04937-0