Abstract
Purpose
The neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) have been studied in many diseases. However, their roles in cryptococcal meningitis (CM) are unclear. The purpose of this article was to analyse the roles of the PLR and NLR in CM patients during treatment.
Methods
139 newly diagnosed CM patients were enrolled. We divided patients into two groups: the successful group (n = 121) and the failure group (n = 18) based on the prognosis of patients. Then, we analyzed changes in clinical data of two groups, which were measured at the time of admission, after 2 weeks and 4 weeks in the hospital. Then the patients were divided into HIV group (n = 26) and non-HIV group (n = 113) to determine whether HIV status had an impact on the prognosis and clinical data of patients.
Results
Most patients were male living in rural areas; headache was the most common symptom before admission. In the subgroup analysis based on HIV status, there were significantly fewer patients with HIV (26 individuals) than without HIV (113 individuals), and 40.7% non-HIV CM patients had no underlying diseases. There was no significant difference in prognosis (p = 0.746), lymphocytes (p = 0.109) or neutrophils (p = 0.269) between patients with and without HIV. A mixed-effect model indicated that there was no difference (p = 0.171) in PLR between successful group and failure group. However, the change of NLR was statistically significant (p = 0.004 < 0.05) between successful group and failure group.
Conclusion
An increase in the NLR during treatment may be used as an indicator of treatment failure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cryptococcal meningitis is an invasive fungal disease mainly caused by Cryptococcus neoformans [1] with a high morbidity and mortality [2]. Cryptococcal meningitis mainly occurs in immunocompromised individuals such as HIV patients. In 2014, it was estimated that there were over 220,000 new cases of cryptococcal meningitis worldwide, leading to more than 180,000 deaths and 15% of all AIDS-related deaths [2]. Although highly active antiretroviral therapy (HAART) has been widely used, the one-year mortality of cryptococcal patients in North America ranges from 10 to 30%, and in low-income countries, it is up to 50–100% [3,4,5]. In addition, organ transplantation, the use of corticosteroids and immunosuppressive therapies are common risk factors for the pathogenesis of cryptococcal meningitis [6, 7]. Antifungal drug therapy remains the mainstay of treatment for cryptococcal meningitis. The timely evaluation of therapeutic effects is necessary. Neutrophils and lymphocytes play a non-negligible role in inflammatory diseases [8], and the NLR has been identified as a useful index for inflammatory diseases [9, 10]. Eduarda Cristina Martins et al. [11] found that the NLR can be used as an indicator for early sepsis detection. CaoYuan Yao et al. [12] found that the NLR may be a simple and useful prognostic marker for hospital mortality in patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD). Similar to the NLR, the PLR is also a useful index in patients with inflammatory diseases and cancer [13]. Hakyemez et al. showed that there was significant difference in NLR between different outcome of CM patients. [14] However, the association of the change in NLR and PLR of cryptococcal meningitis patients during treatment in hospital has not been clarified. In this article, we collected clinical data of patients at admission and after 2 weeks and 4 weeks in the hospital to determine the specific roles of the PLR and NLR during treatment for CM.
Materials and Methods
We retrospectively collected clinical data from 154 CM patients who were first recruited at Jiangxi Chest Hospital from January 2014 to December 2019. All patients were newly diagnosed and had not received any antifungal drug therapy. All HIV patients received HAART. A total of 139 patients were enrolled in this study, and 15 patients were excluded due to a lack of clinical data. The clinical data included white blood cells, platelets, lymphocytes, neutrophils, the PLR and NLR at admission and after 2 weeks and 4 weeks in the hospital. We divided patients into two groups based on prognosis: the successful group (121 persons) and failure group (18 persons). If there were any differences, we next divided patients into the HIV group (26 persons) and non-HIV group (113 persons) to determine whether HIV status had an impact on the prognosis and clinical data of patients. All the patients were followed up for 6 months. Written approval for this study was obtained from the ethics committee of Jiangxi Chest Hospital. All patients or their family members provided written consent in accordance with the ethical committee standards during their hospital stay or outpatient follow-up.
Categorical variables were analyzed by the chi-squared test or Fisher's exact test if any expected value was below five. Continuous variables with a normal distribution were analyzed by Student’s t test and are represented as the mean and standard deviation. Variables with a nonnormal distribution were tested by the Wilcoxon sum rank test and are represented as the median and interquartile range. A p value < 0.05 was considered to indicate statistical significance. ANOVA was implemented to test the difference in changes in clinical data between two groups. A mixed-effect model for repeated measures was applied to measure the change in the NLR and PLR between two groups of patients. The model includes the group and visit as covariates, the intercept as the random effect, and the baseline as the fixed effect, and with an unstructured covariance matrix to model repeated observations, estimates the overall difference in the NLR and PLR between two groups.
Results
Clinical Characteristics of Patients
A total of 139 patients were enrolled in this study. The average age in the successful group was lower than that in the failure group, although there was no significant difference (Table 1). More than half (64.7%) of CM patients were male, and most patients (73.3%) lived in rural areas. The time from onset to diagnosis in the successful group was shorter than that in the failure group; however, there was no significant difference (Table 1). The most common symptom before admission in patients was headache (36%), followed by nausea and vomiting (24.5%), fever (20.1%) and disturbance of consciousness (19.4%). In the subgroup analysis based on HIV status, there were significantly fewer patients with HIV (26 persons) than without HIV (113 persons). A total of 40.7% of CM patients without HIV had no underlying diseases; in the other 67 patients, the most common risk factor was diabetes mellitus (DM) (29.9%), followed by the use of corticosteroids or other immunosuppressants (20.9%), organ transplantation and surgery (17.9%), tuberculosis (11 cases; 3 with CNS infection and 8 with lung infection) (16.4%), hepatitis B infection (14.9%), systemic lupus erythematosus (SLE) 7.5% and other underlying diseases (13.4%).
Changes of the NLR and PLR in CM Patients of Different Groups
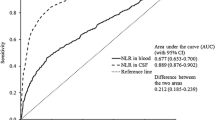
The changes in white blood cells, platelets, lymphocytes, neutrophils, the NLR and PLR on admission and after 2 weeks and 4 weeks in the hospital are shown in Fig. 1. We used the value at the time of admission as the covariate and the group (success and failure) as the independent variable to analyse the data for covariance. There was no significant difference in white blood cells and platelets after 2 weeks in the hospital (p = 0.731, p = 0.978) and 4 weeks in the hospital (p = 0.746, p = 0.0542) in the two groups. Compared with the failure group, the average number of lymphocytes and neutrophils in the success group at 4 weeks in-hospital was 0.397*109/L higher (p = 0.004) and 1.813*109/L lower (p = 0.009), respectively. The mixed-effect model was used to estimate the change in the NLR and PLR and showed that there was a significant difference in the NLR (p = 0.040) between the two groups; the value of the success group was 2.495 lower than that of the failure group. However, there was no difference in the PLR (p = 0.171) between the two groups.
HIV Status did not Impact the Prognosis or the Value of Lymphocytes and Neutrophils
We next divided the patients into the HIV and non-HIV groups to determine whether HIV status has any impact on the prognosis and the value of lymphocytes and neutrophils. There was no significant difference in prognosis between the HIV group and the non-HIV group (p = 0.704 Table 2). We used covariance analysis to examine the impact of HIV status on lymphocytes and neutrophils, and there was no significant difference between the HIV and non-HIV groups (p = 0.109, p = 0.269).
Discussion
Our statistical analysis of the clinical data of CM patients at admission and after 2 weeks and 4 weeks in the hospital indicates that the NLR showed a decreasing trend in successfully treated patients, while in the failure group, it showed a decreasing trend and then an increasing trend after 2 weeks in the hospital. There was no clear difference in the PLR between the two groups. The NLR may be used as a clinical indicator to evaluate the prognosis of CM patients. Similar to this conclusion, Li Minjia et al. [15] found that a moderate reduction in the NLR during chemotherapy is conducive to prolonging the survival of patients with advanced cancer.
In this study, we found that most CM patients in China did not have HIV, and 40.7% of non-HIV CM patients had no underlying diseases, which may be associated with multiple polymorphisms in the genes encoding mannose-binding lectin (MBL) and Fc-gamma receptor 2B (FCGR2B) in the Han population, a major ethnic group in China [1]. When CM patients are first admitted to the hospital, they receive 2 weeks of induction therapy and then consolidation therapy based on the guidelines. Therefore, we chose to collect the clinical data at admission and after 2 weeks and 4 weeks in the hospital. We also found that there were differences in lymphocytes and neutrophils between the successful group and failure group, indicating their unique roles in inflammatory diseases [16]. Furthermore, in this study, HIV status had no impact on prognosis and the value of lymphocytes and neutrophils and may be associated with HAART [17]
In this article, we first found an association between the NLR and CM and the potential role of the NLR in predicting the prognosis of CM using a mixed-effect model. The values obtained from patients at admission and after 2 weeks and 4 weeks in the hospital were all calculated to make the results more informative. This model regards the whole as multilevel data and considers the time and group influence on the outcome to make the results more robust and convincing.
There were some weaknesses in our study. First, the number of patients in the failure group was small, and all the patients came from one hospital. Second, this study was designed as a retrospective study lacking longitudinal observations. Finally, we did not divide the patients into different subgroups based on the underlying disease due to the small number of patients. Hence, additional studies are needed to improve the generalizability of these data to further confirm our results.
In conclusion, the NLR may be used as a clinical indicator to evaluate the prognosis of CM patients, and an increase in the NLR during treatment may be used as an indicator of treatment failure.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to privacy policy but are available from the corresponding author on reasonable request.
References
Fang W, Fa ZZ, Liao WQ. Epidemiology of cryptococcus and cryptococcosis in China. Fungal Genet Biol. 2015;7(8):7–15. https://doi.org/10.1016/j.fgb.2014.10.017.
Mourad A, Perfect JR. The war on cryptococcosis: a review of the antifungal arsenal. Mem Inst Oswaldo Cruz, Rio de Janeiro. 2018;113(7):e170391.
Rajasingham R, Smith RM, Park BJ, et al. Global burden of disease of HIV-associated crypto coccal meningitis: an updated analysis. Lancet Infect Dis. 2017;17(8):873–81.
Williamson PR, Jarvis JN, Panackal AA, et al. Cryptococcal meningitis: epidemiology, immunology, diagnosis and therapy. Nat Rev Neurol. 2017;13(1):13–24.
Williamson PR. The relentless march of cryptococcal meningitis. Lancet Infect Dis. 2017;17(8):790–1.
HRSA-Organ Procurement and Transplantation Network. (2017) Available from: https://optn.transplant.hrsa.gov/data/view-datareports/national-data/.
Messina JA, Maziarz EK, Spec A, Kontoyiannis DP, Perfect JR. Disseminated cryptococcosis with brain involvement in patients with chronic lymphoid malignancies on ibrutinib. Open Forum Infect Dis. 2017;4(1):ofw261.
Qin BD, Ma N, Tang QQ, et al. (2015) Neutrophil to lymphocyte ratio (NLR), platelet to lymphocyte ratio (PLR)were Useful Markers in Assessment of Inflammatory Response and Disease Activity in SLE patients. Mod Rheumatol. 2015. https://doi.org/10.3109/14397595.2015.1091136.
Motomura T, Shirabe K, Mano Y, et al. Neutrophil- lymphocyte ratio reflects hepatocellular carcinoma recurrence after liver transplantation via inflammatory microenvironment. J Hepatol. 2013;58:58–64.
Balta S, Aparci M, Ozturk C, Demirkol S, Celik T. Neutrophil-lymphocyte ratio as an useful mortality marker. Am J Emerg Med. 2014;32(12):1546–7. https://doi.org/10.1016/j.ajem.2014.09.040.
Martins EC, da Fe SL, Viegas K, et al. Neutrophil-lymphocyte ratio in the early diagnosis of sepsis in an intensive care unit: a case-control study. Rev Bras Ter Intensiva. 2019;31(1):63–70.
Yao CY, Liu XL, Tang Z. Prognostic role of neutrophil–lymphocyte ratio and platelet–lymphocyte ratio for hospital mortality in patients with AECOPD. Int J COPD. 2017;12:2285–90.
Feng JF, Huang Y, Chen QX. Preoperative platelet lymphocyte ratio (PLR) is superior to neutrophil lymphocyte ratio (NLR) as a predictive factor in patients with esophageal squamous cell carcinoma. World J Surg Oncol. 2014;12:58.
Hakyemez IN, Erdem H, Beraud G, et al. Prediction of unfavorable outcomes in cryptococcal meningitis: results of the multicenter Infectious Diseases International Research Initiative (ID-IRI) cryptococcal meningitis study. Eur J Clin Microbiol Infect Dis. 2017. https://doi.org/10.1007/s10096-017-3142-1.
Li MJ, Spakowicz D, Burkart J, et al. Change in neutrophil to lymphocyte ratio during immunotherapy treatment is a non-linear predictor of patient outcomes in advanced cancers. J Cancer Res Clin Oncol. 2019;145(10):2541–6. https://doi.org/10.1007/s00432-019-02982-4.
Zahorec R. Ratio of neutrophil to lymphocyte counts–rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy. 2001;102:5–14.
Palella FJ Jr, Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection HIV Outpatient Study Investigators. N Engl J Med. 1998;338(13):853–60.
Funding
This work was supported by the Major National R&D Projects of the National Health Department (2018ZX10101003), National Natural Science Foundation of China (31770161), National Natural Science Foundation of China (82072257), Shanghai Science and Technology Committee (17DZ2272900 and 14495800500), Chinese Academy of Engineering (2019-XY-33), Shanghai Municipal Commission of Health and Family Planning (2017ZZ01024-001) and Shanghai Sailing Program (19YF1448000).
Author information
Authors and Affiliations
Contributions
Keming Zhang, Hang Li, Lei Zhang contributed equally to this work: Conceptualization (lead); Data curation (lead); Formal analysis (lead); Methodology (lead); Writing‐original draft (lead); Writing‐review & editing (lead); Wanqing LIAO, Liangqi Cai, Xinhua Li provided the clinical data and financial support (supporting); Weihua Pan, Qilong Zhang: Supervision (equal).
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict interest.
Ethical Approval
The study obtained approval by the review board of Jiangxi Chest Hospital.
Informed Consent
Not applicable for this study as data were retrospectively collected.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Handling Editor: Weida Liu
Rights and permissions
About this article
Cite this article
Zhang, K., Li, H., Zhang, L. et al. The Change in the Neutrophil/Lymphocyte Ratio Predicts the Prognosis of Patients with Cryptococcal Meningitis. Mycopathologia 186, 857–862 (2021). https://doi.org/10.1007/s11046-021-00553-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-021-00553-1