Abstract
Objectives
We sought to determine the occurrence, risk factors, effect of antifungal prophylaxis, and outcomes of invasive fungal infections (IFIs) in patients with acute myeloid leukemia (AML).
Patients and Methods
We performed a retrospective analysis of all adult patients admitted to the University of Michigan Health System for AML over a 3-year period from 2010 to 2013. We determined comorbidities, hematopoietic cell transplant (HCT) status, antifungal prophylaxis, proven and probable IFI, and outcomes at 12 weeks after initiation of appropriate antifungal therapy.
Results
Of 333 patients in our cohort, 116 of whom had received a HCT, 98 (29%) developed an IFI. Of the 30 (9%) patients who had a proven or probable IFI, 18 had breakthrough infection while on micafungin (n = 5), voriconazole (n = 4), posaconazole (n = 5), or fluconazole (n = 4). Breakthrough IFIs were due to Aspergillus species (n = 11), other molds (n = 4), and Candida species (n = 3). Factors associated with breakthrough IFI were prolonged severe neutropenia (p = .05) and having received tacrolimus (p = .04). Antifungal therapy was successful in 7 of the 18 (39%) patients with breakthrough IFI and 8 of the 12 (67%) patients with non-breakthrough IFI, p = .13. Mortality at 12 weeks was 27%, 5 with breakthrough IFI and 3 with non-breakthrough IFI and was associated with prolonged severe neutropenia, p = .04.
Conclusions
Patients with AML remain at risk for IFI despite the use of several different antifungal agents for prophylaxis. Mortality remains high in patients with AML who develop IFI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute myeloid leukemia (AML) is associated with a high mortality rate, not just from the disease itself but also from opportunistic infections, including invasive fungal infections (IFIs). The use of fluconazole as prophylaxis led to a decrease in the incidence of invasive candidiasis, but mold infections remained a problem [1, 2]. The development of mold-active agents, such as voriconazole and posaconazole, further decreased the incidence of IFI [3, 4]. However, breakthrough IFIs with both yeasts and molds continue to be reported among patients with AML who are receiving antifungal prophylaxis. In several series, breakthrough IFI among patients with AML has ranged from 1.2% to as high as 18% [5,6,7,8,9,10].
We studied a large cohort of patients who had AML, many of whom were receiving antifungal prophylaxis, in order to determine the occurrence of IFI, risk factors for developing IFI, the effect of exposure to prophylactic antifungal agents, and clinical outcomes at 12 weeks after initiation of appropriate antifungal therapy.
Methods
Patients and Setting
This was a single-center retrospective cohort study that included all patients ≥ 18 years of age who had AML and who were hospitalized from January 1, 2010, through December 31, 2013, at the University of Michigan Health System, a 1000-bed tertiary care center. Patients were selected and data retrieved by the Honest Broker Office at the University of Michigan. Each patient was followed for two years from entry into the study or until diagnosis of IFI, at which point they were followed for 12 weeks and then excluded from further analysis. Approval to perform this study was granted by the University of Michigan Medical Center Institutional Review Board.
During the study period, patients undergoing chemotherapy for AML typically did not receive antibacterial prophylaxis during initial induction therapy. With relapsed or refractory disease, patients with an absolute neutrophil count (ANC) ≤ 1500/μL received oral levofloxacin until resolution of neutropenia and then again during subsequent episodes of neutropenia. Antifungal prophylaxis with fluconazole, voriconazole, or posaconazole was initiated when ANC fell to ≤ 1500/μL and continued until resolution of neutropenia. Use of micafungin was indicated in patients receiving anthracycline derivatives due to high-risk drug–drug interactions with azoles [11]. Acyclovir was given throughout all chemotherapy cycles for antiviral prophylaxis. Patients receiving purine analogue therapy received inhaled pentamidine monthly for Pneumocystis prophylaxis throughout all chemotherapy cycles, and this prophylaxis was continued for 6 months following the last dose of a purine analogue agent.
Data Collection and Definitions
The electronic medical record was reviewed to obtain the following information: comorbidities, hematopoietic cell transplantation (HCT), antifungal prophylaxis, occurrence and type of IFI, and 12-week outcomes of patients with IFI. Data were entered and stored in a RedCap database.
Patients included in the study met the definitions for AML proposed by the European Leukemia Net [12]. Patients with acute promyelocytic leukemia were excluded from the study because of the distinctive treatment regimens used and the very low associated risk for IFI. The status of AML at the time IFI occurred was categorized as new diagnosis or if chemotherapy had been given, as response or failure, based on the response criteria proposed by the European Leukemia Net [11]. Prolonged severe neutropenia was defined as ANC ≤ 500/μL for at least 10 days prior to an episode of IFI.
EORTC/MSG criteria were used for the definitions of proven, probable, and possible IFI [13]. Pneumocystis jiroveci pneumonia was considered a fungal infection and was defined as noted in the updated EORTC/MSG criteria [14]. Day of IFI was defined as the time when IFI was first suspected based on clinical, radiological, and/or microbiological findings. An IFI that was diagnosed after 7 days of starting or within 7 days of discontinuing an antifungal agent was considered to be a breakthrough IFI, even if the IFI was due to an organism outside the usual spectrum of activity of the antifungal drug to which the patient was exposed. Serum voriconazole and posaconazole trough levels were noted when available; reference range was 1.0–5.5 μg/mL for voriconazole and > 700 ng/mL for posaconazole.
Response to antifungal therapy and mortality in patients with IFI was assessed at 12 weeks after the initiation of appropriate antifungal therapy. Outcome of the IFI, based on previously published EORTC-MSG criteria, was recorded as success, which encompasses complete and partial responses, or failure, which includes stable infection, progression of infection, and death [15].
Statistical Analysis
Comparison of categorical variables was performed using chi-square or Fisher’s exact test, and comparison of means was performed using ANOVA. Logistic regression was used to estimate associations of patient characteristics with development of breakthrough IFI and with 12-week survival. Statistical significance was defined as p value < 0.05. All statistical analyses were completed using SPSS software, version 26.0 (SPSS, Inc., Chicago, IL).
Results
Patients
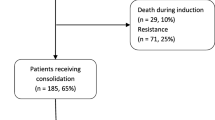
A total of 333 patients with AML were included in the study. The mean age was 59.1 ± 16.1 years, and 200 (60%) were men (Table 1). A total of 116 patients (35%) had received a HCT, of which 108 were allogeneic and 8 were umbilical cord blood. The most common comorbidities were diabetes, chronic pulmonary disease, and chronic kidney disease.
Invasive Fungal Infections
Of the 333 patients, 98 had an IFI (29%), including 30 (9%) who had a proven or probable IFI (Table 2). There were 18 probable IFI and 13 proven IFI in 12 patients; one patient had proven concomitant infection with 2 different molds. A total of 68 patients had possible IFI based on radiographic and clinical criteria per EORTC/MSG definitions and were excluded from further analysis.
Of the 30 cases of proven and probable IFI, 24 (80%) (including one patient with concomitant aspergillosis and mucormycosis) were caused by molds, most commonly Aspergillus sp. (n = 17) (Table 2). Of these 17, the diagnosis was established by a positive galactomannan assay from bronchoalveolar lavage fluid (BAL) in 11 and by culture in 6. Other molds causing IFI included Mucorales (n = 5), Alternaria alternata (n = 2), and Scedosporium apiospermum complex (n = 1). Among the non-mold infections, 4 were invasive Candida infections and 2 were Pneumocystis jiroveci pneumonias.
Among the 30 proven or probable IFI episodes, 12 occurred in patients who were not receiving antifungal prophylaxis at the time of the diagnosis of IFI. Five of these patients developed an IFI less than 7 days after admission for induction chemotherapy; 4 were not neutropenic; 2 had not received Pneumocystis prophylaxis; and 1 had interrupted prophylaxis due to drug–drug interactions. The organisms causing infection in these patients were Aspergillus species (n = 6), Mucorales (n = 3), P. jiroveci (n = 2), A. alternata (n = 1), and Candida glabrata (n = 1) (Table 2).
Breakthrough Invasive Fungal Infections
Among the 30 proven and probable IFI, 18 (60%) were breakthrough IFI. All breakthrough IFI occurred in patients who were receiving antifungal agents for prophylaxis; no breakthrough IFI occurred in patients who were receiving antifungal therapy for a documented IFI. The organisms causing infection among 18 patients receiving antifungal prophylaxis were Aspergillus sp. (n = 11), Mucorales (n = 2), A. alternata (n = 1), S. apiospermum complex (n = 1), C. krusei (n = 2), and C. famata (n = 1) (Table 2).
Breakthrough IFIs occurred with all prophylactic regimens (Table 3). Five patients taking micafungin developed aspergillosis (n = 4) and scedosporiosis (n = 1). Breakthrough invasive aspergillosis (n = 3) and candidemia (n = 1) occurred in patients receiving fluconazole. Among 4 patients who were receiving posaconazole suspension, 3 developed breakthrough infections with Aspergillus sp., and another with A. alternata. The patient who received prophylaxis with posaconazole tablets and had a serum trough concentration > 1000 ng/mL developed a resistant C. famata infection. Four patients who received voriconazole, 3 of whom had therapeutic serum trough levels from 1.5 to 3.2 μg/mL, developed mucormycosis (n = 2), aspergillosis (n = 1), and candidemia (n = 1).
Development of breakthrough IFI was significantly associated with prolonged severe neutropenia at the time of diagnosis (p = 0.05) and having received oral tacrolimus (p = 0.04) (Table 4). Binary logistic regression analysis revealed no independent predictor for breakthrough IFI.
Outcomes
Antifungal therapy was deemed successful at 12 weeks in 15 of the 30 patients (50%) with a proven or probable IFI. Seven of 18 patients (39%) with breakthrough IFI had a successful response to antifungal therapy compared with 8 of 12 patients (67%) with non-breakthrough IFI, p = 0.13. The 4 failures in the non-breakthrough group were due to Mucorales (n = 2), Aspergillus sp. (n = 1), and C. glabrata (n = 1). Mortality at 12 weeks in patients who developed an IFI was 27%; death occurred in 5 patients in the breakthrough IFI group and 3 patients in the non-breakthrough IFI group p = 0.60. By binary logistic regression, prolonged severe neutropenia at the time of IFI diagnosis was a significant risk factor for fatal outcome at 12 weeks among patients with IFI, p = 0.04.
Discussion
Over a 2-year period, we found that 29% of our patients with AML developed a proven, probable, or possible IFI. It is likely that some of the 68 (20%) patients with the diagnosis of a possible IFI, in fact, had another infection or a non-infectious disease, so they were excluded from our analysis. A total of 30 patients (9%) had proven or probable IFI, and 18 (5%) of these 30 had proven or probable IFI in spite of the use of prophylactic antifungal agents. This rate of development of IFI while on prophylaxis is similar to that noted by others [7,8,9,10].
Prolonged neutropenia was associated with the development of breakthrough IFI and was found to be the only independent predictor of poor outcome in the entire cohort. This is similar to findings from other studies of patients with AML and those who have received a HCT [6, 7, 16, 17].
The most common IFI was invasive pulmonary aspergillosis, irrespective of whether antifungal prophylaxis was used and which specific agent was used. It is not unusual to have 3 cases of invasive aspergillosis among patients receiving fluconazole prophylaxis, but it was striking that there were just as many patients with this IFI among those receiving prophylaxis with micafungin and posaconazole. Both of these agents are approved for prophylaxis in patients with acute leukemia and/or HCT [18,19,20].
Micafungin is better tolerated by many patients than the azoles, does not have the drug–drug interactions that preclude the use of azoles for some patients with AML, and is approved for prophylaxis in HCT recipients. However, the dose for prophylaxis, which is approved by the Food and Drug Administration only for yeast infections, is 50 mg daily, and this is unlikely to be effective for preventing aspergillosis [17]. Breakthrough infections with both Candida species and molds have been reported with echinocandin therapy [8, 21,22,23].
The most likely explanation for the failure of posaconazole to prevent invasive aspergillosis is the poor absorption of the oral suspension, which was used in 4 of the 5 patients who had breakthrough IFI [24, 25]. Therapeutic drug monitoring was not performed for 3 of these patients, and the fourth had a sub-therapeutic serum concentration. It is likely that serum concentrations were below those needed to prevent breakthrough IFI in these patients. Introduction of the posaconazole extended release oral tablet allows reliable absorption of this agent for most patients. However, several centers have reported breakthrough IFI in patients taking either posaconazole formulation and with adequate serum concentrations of this drug, and we noted this in one patient [26, 27].
We observed breakthrough IFI due to Mucorales only in patients receiving voriconazole for prophylaxis, but we also noted 3 other IFI due to Mucorales in patients not receiving antifungal prophylaxis. Voriconazole prophylaxis has been implicated as a risk factor for breakthrough mucormycosis in some studies, but not in others, suggesting that the risk for this infection is most likely multifactorial [28].
Another reason for breakthrough IFI while on prophylactic antifungal agents is increasing drug resistance among yeasts and molds [29, 30]. We noted that 3 breakthrough IFIs in our patients were caused by Candida species with known resistance (C. krusei) or variable susceptibilities (C. famata) to many azole agents [30, 31]. We do not have susceptibility data for most of the organisms causing IFI to help explain the development of breakthrough infections; for many of our patients, the diagnosis of probable invasive pulmonary aspergillosis was made by a positive galactomannan assay and established radiological criteria, and cultures were not positive.
Our study showed an overall 12-week mortality of 27% among patients who developed an IFI. The poor outcome of patients with IFI could be explained by the inherent virulence associated with the specific pathogens involved, as well as the very important factor of profound immunosuppression in patients with AML.
The limitations of our study include its retrospective, single-center design and the relatively small sample size. The study was carried out from 2010 to 2013 and thus reflects clinical practice at that time; changes in practice, particularly the introduction of new formulations of azole agents, will impact both the risk for and the outcome of breakthrough IFI and should be studied.
In conclusion, IFIs remain a significant problem among patients with AML despite the use of antifungal prophylaxis. Profound myelosuppression was a significant risk factor for both the development of breakthrough IFI and poor outcomes.
References
Laverdierre M, Rotstein C, Bow EJ, et al. Impact of fluconazole prophylaxis on fungal colonization and infection rates in neutropenic patients. J Antimicrob Chemother. 2000;46:1001–8.
van Burik JH, Leisenring W, Myerson D, et al. The effect of prophylactic fluconazole on the clinical spectrum of fungal diseases in bone marrow transplant recipients with special attention to hepatic candidiasis. An autopsy study of 355 patients. Medicine (Baltimore). 1998;77:246–54.
Cornely OA, Maertens J, Winston DJ, et al. Posaconazole vs fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med. 2007;356:348–59.
Anadah-Rajah MR, Grigg A, Downey MT, et al. Comparative clinical effectiveness of prophylactic voriconazole/posaconazole to fluconazole/itraconazole in patients with acute myeloid leukemia/myelodysplastic syndrome undergoing cytotoxic chemotherapy over a 12-year period. Haematologia. 2012;97:459–63.
Rausch CR, DiPippo AJ, Bose P, et al. Breakthrough fungal infections in patients with leukemia receiving isavuconazole. Clin Infect Dis. 2018;67:1610–2.
Kim S-H, Choi J-K, Cho S-Y, et al. Risk factors and clinical outcomes of breakthrough yeast bloodstream infections in patients with hematological malignancies in the era of newer antifungal agents. Med Mycol. 2018;56:197–206.
Breda GL, Tuon FF, Meis JF, et al. Breakthrough candidemia after the introduction of broad spectrum antifungal agents: a 5-year retrospective study. Med Mycol. 2018;56:406–15.
Lionakis MS, Lewis RE, Kontoyiannis DP. Breakthrough invasive mold infections in the hematology patient: current concepts and future directions. Clin Infect Dis. 2018;67:1621–30.
Auberger J, Lass-Florl C, Aigner M, et al. Invasive breakthrough infections, fungal colonization and emergence of resistant strains in high-risk patients receiving antifungal prophylaxis with posaconazole: real-life data from a single-centre institutional retrospective observational study. J Antimicrob Chemother. 2012;67:2268–73.
Biehl LM, Vehreschild JJ, Liss B, et al. A cohort study on breakthrough invasive fungal infections in high-risk patients receiving antifungal prophylaxis. J Antimicrob Chemother. 2016;71:2634–41.
Cronin S, Chandrasekar P. Safety of triazole antifungal drugs in patients with cancer. J Antimicrob Chemother. 2010;65:410–6.
Dohner H, Estey E, Grimwade D, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129:424–47.
De Pauw B, Walsh TJ, Donnelly JP, et al. Fungal infections cooperative group and the national institute of allergy and infectious disease mycoses study group (EORTC/MSG) consensus group. revised definitions of invasive fungal disease from the European organization for research and treatment of cancer/invasive fungal infections cooperative group. Clin Infect Dis. 2008;46:813–21.
Donnelly PJ, Chen S, Kauffman CA, et al. Revision and update of the consensus definitions of invasive fungal disease from the European organization for research and treatment of cancer and the mycoses study group education and research consortium. Clin Infect Dis. 2019 (in press)
Segal BH, Herbrecht R, Stevens DA, et al. Defining responses to therapy and study outcomes in clinical trials of invasive fungal infections: MSG and EORTC consensus criteria. Clin Infect Dis. 2008;47:674–83.
Gomes MZR, Jiang Y, Mulanovich VE, et al. Effectiveness of primary anti-Aspergillus prophylaxis during remission induction chemotherapy of acute myeloid leukemia. Antimicrob Agents Chemother. 2014;58:2775–800.
Kimura M, Araoka H, Yamamoto H, et al. Clinical and microbiological characteristics of breakthrough candidemia in allogeneic hematopoietic stem cell transplant recipients in a Japanese hospital. Antimicrob Agents Chemother. 2017;61:e01791–e1816.
van Burik JA, Ratanatharathorn V, Stepan DE, et al. Micafungin versus fluconazole for prophylaxis against invasive fungal infection during neutropenia in patients undergoing hematopoietic stem cell transplantation. Clin Infect Dis. 2004;39:407–16.
Ullmann AJ, Lipton JH, Vesole DH, et al. Posaconazole or fluconazole for prophylaxis in severe graft-versus-host disease. N Engl J Med. 2007;356:335–47.
Cornely OA, Maertens J, Winston DJ, et al. Posaconazole vs. fluconazole or itraconazole prophylaxis in patients with neutropenia. N Engl J Med. 2007;356:348–59.
Mattiuzi GN, Alvarado G, Giles FJ, et al. Open-label randomized comparison of itraconazole versus caspofungin for prophylaxis in patients with hematologic malignancies. Antimicrob Agents Chemother. 2006;50:43–7.
Kimura M, Araoka H, Yamamoto H, et al. Micafungin breakthrough fungemia in patients with hematological disorders. Antimicrob Agents Chemother. 2018;62:e02183–e2217.
Pang KA, Godet C, Fekkar A, et al. Breakthrough invasive mould infections in patients treated with caspofungin. J Infect. 2012;64:424–9.
Lerolle N, Raffoux EA, Socie G, et al. Breakthrough invasive fungal disease in patients receiving posaconazole primary prophylaxis: a 4-year study. Clin Microbiol infect. 2014;20:O952–O959959.
Cattaneo C, Panzali A, Passi A, et al. Serum posaconazole levels during acute myeloid leukemia induction therapy: correlations with breakthrough infections. Mycoses. 2015;58:362–7.
Cornely O, Ullmann AJ. Lack of evidence for exposure-response relationship in the use of posaconazole as prophylaxis against invasive fungal infections. Clin Pharmacol Ther. 2011;89:351–2.
Tverdek FP, Heo ST, Aitken SL, et al. Real-life assessment of the safety and effectiveness of the new tablet and intravenous formulations of posaconazole in the prophylaxis of invasive fungal infections via analysis of 343 courses. Antimicrob Agents Chemother. 2017;61:e00188–e217.
Pondas GN, Lewis RE, Samonis G, et al. Voriconazole-associated zygomycosis: a significant consequence of evolving antifungal prophylaxis and immunosuppression practices? Clin Microbiol Infect. 2009;15(Suppl. 5):93–7.
Farmakiotis D, Tarrand J, Kontoyiannis DP. Drug-resistant Candida glabrata infection in cancer patients. Emerg Infect Dis. 2014;20:1833–40.
Lamoth F, Chung SJ, Damonti L, et al. Changing epidemiology of invasive mold infections in patients receiving azole prophylaxis. Clin Infect Dis. 2017;64:1619–21.
Desnos-Ollivier M, Ragon M, Robert V, et al. Debaryomyces hansenii (Candida famata), a rare human fungal pathogen often misidentified as Pichia guilliermondii (Candida guilliermondii). J Clin Microbiol. 2008;46:3237–42.
Funding
Carol A. Kauffman is a member of the Data Safety Monitoring Board for CIDARA. Marisa H. Miceli is a consultant for Astellas and a member of the Data Review Committee for Scynexis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Handling editor: Vishnu Chaturvedi.
Rights and permissions
About this article
Cite this article
Wasylyshyn, A., Linder, K.A., Castillo, C.G. et al. Breakthrough Invasive Fungal Infections in Patients with Acute Myeloid Leukemia. Mycopathologia 185, 299–306 (2020). https://doi.org/10.1007/s11046-019-00418-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-019-00418-8