Abstract
Infections due to Cryptococcus neoformans cause severe disease, mostly in AIDS patients. The antifungal drug recommended for the initial treatment of these infections is amphotericin B with or without flucytosine, but treatment failure occurs, associated with high mortality. Thus, antifungal susceptibility testing is needed. However, the in vitro susceptibility tests available for C. neoformans are not useful to detect isolates that are not susceptible to antifungal agents such as amphotericin B. The aims of the present study were: (1) to determine and compare the in vitro activity of amphotericin B against C. neoformans clinical isolates by using different dilution and diffusion methods; (2) to evaluate the concordance among the methods used and the reference method; (3) to evaluate which method could be the best to correlate with the clinical outcome. The reference method EDef 7.2 from the European Committee on Antimicrobial Susceptibility Testing and commercial Etest strips were used to determine the minimal inhibitory concentration against amphotericin B. curves, minimal fungicidal concentration, and a disk diffusion method were also developed to evaluate the cidal activity of amphotericin B. The time–kill curve assay showed correlation (p < 0.05) with clinical outcome, whereas EDef 7.2, minimal fungicidal concentration, Etest, and disk diffusion showed no correlation (p > 0.05). Thus, the time–kill curve assay could be a potential tool to guide a more efficient treatment when amphotericin B is used.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infections due to Cryptococcus neoformans cause severe disease, mostly in AIDS patients, and are an unresolved problem. In Argentina, the mortality rate is high, reaching up to 35 % during the first month of diagnosis, while survival is estimated as 1–2 years post-diagnosis [1, 2]. The antifungal drug recommended for the initial treatment of these infections is amphotericin B with or without flucytosine, followed by fluconazole at the consolidation period [3]. However, the response to conventional therapy is erratic; recurrence is common, with 20–30 % of treatment failure, and fatal outcome in most cases [1, 2].
For Candida spp. and C. neoformans, the available reference methods M27-A3-S4 and EDef 7.2 of the Clinical Laboratory and Standards Institute (CLSI) and the European Committee on Antimicrobial Susceptibility Testing (EUCAST), respectively, are useful to determine the in vitro susceptibility against antifungal drugs [4, 5]. These two reference methods are important tools to guide therapy. However, they have technical limitations for in vitro tests due to the difficulties in the growth of C. neoformans, being growth, inoculum size, culture medium, and inter- and intra-laboratory reproducibility the most important issues to be considered [6, 7].
Several studies have been conducted to determine the susceptibility profile of C. neoformans [8–12], whereas others have also evaluated the correlation with outcome [13–16]. However, to date, the in vitro methods available are not useful to detect C. neoformans isolates that are not susceptible to antifungal agents. Regarding the detection of resistance to amphotericin B, it has been demonstrated that it could be influenced according to the pH and the culture medium in which the assay is performed, i.e., acidic conditions have been found to raise the MICs of amphotericin B [7, 17]. In addition, in some diseases such as meningitis, osteomyelitis, and endocarditis, it is necessary to know the cidal activity of drugs, because the patient’s survival depends on a rapid action and efficient treatment [18–21].
In clinical bacteriology, other techniques, the most common and simple of which is the in vitro determination of time–kill curve (TKC), are used to estimate the microbicidal ability of an antimicrobial [20–22]. The TKC allows monitoring the antimicrobial activity over time by counting the number of surviving microorganisms and provides important information about its action on the organism’s life cycle [19–21]. The usefulness of TKC has been studied to explore the interaction of antifungal drugs against Candida spp. and Cryptococcus spp. [18, 19, 23–27]. However, for C. neoformans, few studies have been conducted to evaluate the correlation with clinical outcome [18, 19, 28].
The aims of the present study were: (1) to determine and compare the in vitro activity of amphotericin B against C. neoformans clinical isolates by using different dilution and diffusion methods; (2) to evaluate the concordance between the methods used and the reference method; (3) to evaluate which method could be the most useful to predict the clinical outcome.
Materials and Methods
Study Design
A retrospective laboratory-based study was conducted. The study subject population consisted of 60 adult patients of both genders, who developed AIDS-associated cryptococcal meningitis between 2000 and 2013. Patients who had more than one episode were also included. Recidivism or recurrence was defined as the appearance of clinical signs and symptoms after negative cultures, new hospitalization, or change of the antifungal treatment.
The epidemiological, clinical, and laboratory data collected from of all patients remained confidential and were encrypted to avoid tracing to the institutional medical history document source. Data were reviewed from January 2000 to December 2013 to analyze CD4 values, viral charge, marker diseases, comorbidities, date of the first isolate, outcome, and date of death.
Samples and Microorganisms
The samples were collected from cerebral spinal fluid (CSF). Seventy-four C. neoformans isolates, 60 of which were obtained during the first episode and 14 of which belonged to eight patients who developed one or more recurrent episodes, were included in the analysis.
Isolates were identified to species level according to Kurtzman procedure based on the study of the microscopic morphology on liquid malt extract (malt extract 3 %), urea and phenoloxidase tests, carbohydrate assimilation, and fermentation [29]. To differentiate C. neoformans from Cryptococcus gattii, the selective medium canavanine glycine blue was used; C. gattii NIH 112B and C. neoformans ATCC 90112 were used as quality control strains. Strains were deposited at the culture collection of the Departamento Micologia, Instituto Nacional de Enfermedades Infecciosas, “Dr. C. G. Malbrán,” and were conserved at −20 °C in 20 % glycerol. For determining assays, an aliquot of each original strain was conserved at 4 °C until use.
Serotypes were studied according to the agglutination test proposed by Ikeda et al. [30]. The quality control strains were: NIH 112B (serotype B) and NIH 52D (serotype D), gently provided by Dr. E. Castañeda, UCLA 381-C (serotype C), gently provided by Dr. W. Meyer, and ATCC 62067 (serotype A).
Susceptibility Tests
The minimal inhibitory concentration (MIC) was determined following the reference method EDef 7.2 (EUCAST) (MIC-RM) [5].
Antifungal Agent
A 10 mg/L stock solution of amphotericin B was prepared in dimethylsulfoxide and stored at −70 °C until needed. A final concentration of 0.03–16 mg/L was used. RPMI 1640 medium (RPMI) buffered with 3-(N-morpholino)propanesulfonic acid (MOPS) at pH 7.0 was used. Amphotericin B and reagents were all purchased from Sigma-Aldrich, Quimica, Argentina.
Inoculum
Isolates were cultured on YM agar (malt extract 0.3 %, yeast extract 0.3 %, peptone 0.5 %, glucose 1 %, and agar 2 %) at 30 °C. Then, a suspension of 0.5 McFarland (1–5 × 106 CFU/mL) was prepared in 0.15 M sterile sodium chloride solution (saline solution 0.85 %). The final inoculum was 1–5 × 105 CFU/mL. Microplates were incubated on agitated condition at 350 r.p.m., 30 °C, for 48 ± 2 h. The reading was performed at 405 nm using a spectrophotometer (Labsystems Multiskan Multisoft, Basingstoke, UK).
Quality Control Strains
Candida parapsilosis ATCC 22019, Candida krusei ATCC 6258, and C. neoformans ATCC 90112 were included in all the susceptibility tests performed.
End Points
The MIC-RM end point was defined as the lowest concentration of drug that caused a prominent reduction (MIC-0 or >90 %) in growth compared with that of a drug-free growth control well. To date, no breakpoints have been established for antifungal agents against C. neoformans. However, according to recent studies, strains can be considered resistant when the MIC-RM values for amphotericin B are ≥2 mg/L [11]. The MIC90, range, geometric mean, and mode were calculated.
Minimal Fungicidal Concentration (MFC)
To determine the amphotericin B MFC, 100 µL from each well of the microplate MIC-RM with growth inhibition was plated on YM agar. The plates were incubated at 30 °C for 48 h. Killing >99.9 % of CFU/mL after 48 h incubation was considered as the end point of the MFC. Thus, the MFC was defined as the lowest drug concentration that yielded three of fewer yeast colonies on the YM plate.
Time–Kill Curves
The TKC were developed according to previous studies [19]. Thus, an amphotericin B 1 mg/L working solution was prepared by serial tenfold dilutions in RPMI medium.
Inoculum
Strains were grown overnight at 35 °C in agitated condition (350 r.p.m.) in RPMI medium. The initial inoculum was adjusted to 0.5 McFarland (1–5 × 106 CFU/mL). Then, 1 mL of this suspension was diluted tenfold in MOPS-buffered RPMI. This medium contained amphotericin B at a final concentration of 1 mg/L. A control growth tube (10 mL of RPMI) without drug was included. The tubes were incubated at 35 °C in agitated conditions (350 r.p.m.). Then, 1-mL samples from each tube were extracted, and serial tenfold dilutions were performed at 0, 6, 12, 24, 48, and 72 h, respectively. From each of these serial tenfold dilutions, 100 µL was plated on YM agar medium. After 72 h at 35 °C, colony counts were determined. Killing >99.9 % of CFU/mL (reduction of >3 log CFU/mL) was considered as the end point of the TKC. For each isolate, a curve of inhibition was performed by plotting the log10 CFU/mL against time. Tests were performed in duplicate.
Interpretation
To analyze the data, we created a numerical scale, where 1–5 referred to susceptible strains when growth inhibition was at 6, 12, 24, 48, and 72 h, respectively, and 6 referred to not susceptible strains. Then, data were adjusted with clinical outcome (live 1, dead 0) to a generalized linear model of binomial family.
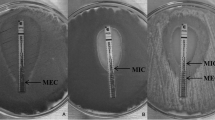
Diffusion Methods
Amphotericin B Etest strips (0.002–32 mg/L) (bioMérieux) on RPMI 1640-2 % glucose agar and amphotericin B Neo-Sensitabs™ Rosco tablets (10 μg) on Mueller Hinton + 2 % glucose agar + 0.5 % Methylene Blue were used. Susceptibility testing, reading, and interpretation of the results were performed according to the manufacturer’s instructions [31] [www.bioMerieux.com].
Determination of the Inhibition Zone
For both agar diffusion methods, end points were read visually. Therefore, for Etest strips, the MIC value was where the inhibition ellipse intersects the strip and a MIC value of ≤1 mg/L was considered as susceptible.
Etest strips contain a continuous gradient of drug tested instead of the log2 drug dilution scheme of the reference methods. Thus, the Etest MICs between twofold dilutions were converted to the next higher concentration to facilitate comparison of the results.
For the Neo-Sensitabs™ tablets, the zone diameter end point was measured with a ruler in which there was no visible growth. Colonies inside the inhibition zone must be considered resistant mutants. The interpretative criterion was according to the manufacturer’s instructions as follows: susceptible (≥15 mm), dose-dependent (14–10 mm), and resistant (≤10 mm) [www.rosco.uk Document: 3.15.0].
Statistical Analysis
To describe quantitative and qualitative variables, average and percentage were, respectively, used. The MIC-RM was correlated with inhibition zone diameters (in mm) around amphotericin B tablets and the MIC value of Etest strips. The gamma coefficient (G) was used to evaluate the association between the reference method and the diffusion method.
Essential agreement was defined as the MIC-RM and MIC-Etest results in exact agreement or discrepancies in results of no more than ±2 fold dilutions. The categorical agreements and percentages of discrepancies were evaluated for the Etest strips and Neo-Sensitabs™ tablet results. Discrepancies between methods were considered as: very major errors when the reference method categorized the organism as resistant, but the diffusion method categorized the organism as susceptible (falsely susceptible); major errors when the reference method categorized the isolate as susceptible, but the diffusion method categorized it as resistant (falsely resistant); and minor errors when the reference method categorized an organism as susceptible or resistant and the diffusion method categorized it as susceptible dose-dependent (or intermediate) or the reference categorized it as susceptible dose-dependent (or intermediate) and the diffusion method categorized it as susceptible or resistant. The Pearson Chi-square test was used to compare categorical variables. Variables recognized as statistically significant in univariate analysis (defined as a p value of <0.05) were used. To analyze the interdependence between variables, a multiple correspondence factor analysis (MCA) was performed. The MCA shows affinities between two or more variables, and both frequency and average values were presented in a contingency table. To facilitate interpretation, a graphical representation of the factors was performed.
Data were analyzed using the Statistical Package for the Social Sciences version 15.0 software (SPSS 15.0) and Statistica version 7.1 data analysis software system. StatSoft, Inc. (2005) (www.statsoft.com).
Results
Clinical Data
Patients were identified as 1–60 to avoid tracing to the institutional medical history document source. The fungal isolates were most frequently found in males (male–female ratio = 48:10); the sex was unknown in two patients. Range age 22–47 years; mean 33.8, SD 5.9.
All the patients developed cryptococcal meningitis (cm); in some patients, the following diseases were also diagnosed: toxoplasmosis (tx) (n = 6), tuberculosis (tb) (n = 7), pneumocystosis (pn) (n = 3), Herpes Zoster (hz) (n = 4), hepatitis B (hb) (n = 1) nd hepatitis C (hc) (n = 2), cytomegalovirus (cv) (n = 6), and oropharyngeal candidiasis (co) and genital candidiasis (cg) (n = 2).
The association between diseases and outcome was analyzed, and we observed that tb–cm is more associated with died event than the others diseases. Meanwhile, a lower association between cm–cv and survived event was observed (Fig. 1).
Association between different diseases and outcome. Tuberculosis plus cryptococcal meningitis was more associated with died event than the other diseases. cm cryptococcal meningitis, tb tuberculosis, co oropharyngeal candidiasis, genital candidiasis, tx toxoplasmosis, cv cytomegalovirus, hb hepatitis B, and N/D no data
The median CD4 count was 37, range 4–601 cells/mL. For 52 (87 %) patients, the CD4 count was ≤200 cells/mL, among them, 33 (63.5 %) died, 16 (30.7 %) survived, and in three (5.8 %) the outcome was unknown. On the contrary, among the eight (13 %) patients with CD4 count >200 cells/mL, four (50 %) died and four (50 %) survived. In spite of these findings, no significant association between CD4 counts and outcome was obtained (χ 2 = 1.48; p = 0.4783).
Treatment and Outcome
All the patients received amphotericin B (0.7 mg/kg/day) as initial treatment, followed by fluconazole (200–1800 mg/day) for a minimum of 8 weeks, while patients 47, 48, 56, and 58 received voriconazole (400 mg/day).
In spite of treatment, 37 (61.7 %) patients died within the first 5 years post-diagnosis. To note, among the 37 patients who died, 20 (54 %) patients, of which eight were female and 12 were male died within the same year of diagnosis (range 1–11 months).
Despite the high mortality observed in the female group, no association was observed between the patients’ gender and their outcome (p = 0.465). In Table 1, the distribution of outcome (survived/died) over time is recorded.
Patients 16, 37, 42, 50, 56, 59, 47, and 39 showed recidivism of 2, 2, 2, 2, 2, 2, 3, and 7 episodes, respectively. In Table 2, the clinical data, susceptibility test, treatment, and outcome of this group of patients are summarized. For susceptibility testing results, the MIC-RM, MIC-Etest, and tablet values were similar between initial and relapsed isolates, indicating that isolates were susceptible to amphotericin B.
For MFC, the highest values (≥2 mg/L) were obtained from isolates whose MIC-RM range was 0.03–0.5 mg/L. In spite of relapsed episodes, three patients survived, one of them had a kill curve that indicated tolerance to amphotericin B.
Microorganisms
Cryptococcus neoformans var. grubii (serotype A) was observed in 96.7 % (n = 58) of the samples, whereas C. neoformans var. neoformans (serotype D) was observed in 3.3 % (n = 2).
Susceptibility Test and Outcome
All strains were susceptible to amphotericin B by using MIC-RM, Etest strips, and Neo-Sensitabs™ tablets. For MIC-RM, the range of amphotericin B was 0.03–0.5 mg/L and the MIC-90 and mode value were coincident (0.25 mg/L), whereas for the Etest strips, the range of amphotericin B was lower ≥1 dilution (0.002–0.25 mg/L) compared with that for MIC-RM.
Regarding the essential agreement, 12.2 % (n = 9) of isolates showed exact agreement, 25.7 % (n = 19) were concordant within ≤2 dilutions and 62.1 % (n = 46) within >2 dilutions. Despite these results, no categorical discrepancies were observed. No significant association was found between MIC-RM and MIC-Etest values (G = 0.205; p = 0.075).
For Neo-Sensitabs™ tablets, the range of amphotericin B was 22–50 mm; 100 % categorical agreement with the reference method was observed. However, no significant association was found between Neo-Sensitabs™ tablets and MIC-RM values (G = −0.195; p = 0.79). Results are summarized in Table 3.
Minimal Fungicidal Concentration
For the MFC, 27 (36.5 %) strains were not susceptible against amphotericin B (MFC value ≥2 mg/L). Twenty strains (74 %) were from 17 patients who died, six (22.2 %) from five patients who survived, and one (3.7 %) from one patient with no data recorded. The MIC-RM, MFC, and Etest values distribution are shown in Fig. 2, where the MFC bars placed to right of the graphic indicate the isolates that were not susceptible to amphotericin B (≥2 mg/L), meanwhile the MIC-RM and the Etest bars are all placed to left of the graphic indicating that isolates were all susceptible to amphotericin B.
Distribution of amphotericin B MIC-RM, MFC, and MIC-Etest values for 74 C. neoformans isolates. The MFC-AB bars disposed to right of the graphic indicate that some isolates were not susceptible to amphotericin B (≥2 mg/L). MIC-RM AB minimal inhibitory concentration-reference method, MFC-AB minimal fungicidal concentration, MIC-Etest AB minimal inhibitory concentration Etest, AB amphotericin B
Although MFC identified several isolates as not susceptible to amphotericin B, no correlation between MFC and clinical outcome was observed (p = 0.145).
Also, results of amphotericin B MIC-RM, MIC-Etest, and Neo-Sensitabs™ tablets did not correlate with clinical outcome (p > 0.05; Table 4).
Time–Kill Curves
Thirty-seven (50 %) strains were not susceptible against amphotericin B 1 mg/L, showing no reduction in growth after 72 h of incubation, and were categorized as six in the 1–6 scale. These strains were isolated from 26 patients, 25 of whom (96.1 %) died. In contrast, 37 (50 %) strains were susceptible to amphotericin B and a ≥99.99 killing rate was detected throughout the experiment (6–72 h). These susceptible strains were isolated from 34 patients, 20 of whom survived, 13 died and one patient from whom no data of outcome were obtained. The range of MIC-RM of these strains was 0.03–0.5 mg/L, and no significant differences were observed between the MIC/TKC values from the first and relapsed isolates. In Table 4, the results of susceptibility tests and patient’s outcome are summarized. Data used were obtained from the initial isolate.
In Figs. 3 and 4, representative susceptible and not susceptible kill curves for amphotericin B 1 mg/L are shown.
Representative time–kill curve plots for amphotericin B susceptible C. neoformans clinical strains. Strains were isolated from patients identified as pink 1, light green 4, violet 25, brown 33, and dark green 44. CC dark blue control growth. The concentration of amphotericin B tested was 1 mg/L. (Color figure online)
Representative time–kill curve plots for amphotericin B not susceptible C. neoformans clinical strains. The strains were isolated from patients identified as pink 5, red 16, light blue 18, and violet 39. CC dark blue control growth. The concentration of amphotericin B tested was 1 mg/L. (Color figure online)
Despite several patients died, a significant correlation between TKC and outcome (death or survival) was observed (p < 0.05).
The association between MFC, CD4 count, kill curves, and outcome was analyzed, and a clear association between kill curve categorized as 6 (not susceptible) and died event was observed. A minor association between MFC not susceptible, CD4 count <200 cells/mL, and outcome was observed. On the other hand, the kill curve categorized as 1 (susceptible) was associated with survived event (Fig. 5).
Association between the variables MFC, CD4, kill curves, and outcome. Kill curve categorized as 6 (not susceptible) is more associated with died event. A minor association between MFC not susceptible, CD4 count <200 cells/mL and outcome was observed. MFC: NS minimal fungicidal concentration not susceptible, MFC: S minimal fungicidal concentration susceptible, KC 1–KC 5 indicate susceptible to amphotericin B, KC 6 indicates not susceptible to amphotericin B
Discussion
Although the reference method M27-A3-S4 and EDef 7.2 of the CLSI and EUCAST, respectively, and different commercial techniques have been used to evaluate the in vitro susceptibility of C. neoformans against antifungal drugs [13, 31–34], all these methods fail to discriminate between isolates of C. neoformans resistant against antifungal drugs and outcome [13, 14].
In addition, no clinical breakpoints are currently established for C. neoformans for any drug. However, epidemiological cutoff values based on MIC distribution have been recently proposed for some antifungal drugs. Thus, the epidemiological cutoff value of amphotericin B ≤1 mg/L was proposed [9–11]. Nevertheless, the interpretation of MIC values as a predictor of the outcome is poorly understood, and its usefulness to guide therapy is controversial [13, 21].
In the present study, different susceptibility in vitro test were used to evaluate the cidal activity of amphotericin B against 74 C. neoformans clinical strains isolated from 60 patients who developed cryptococcal meningitis AIDS-associated. The association of in vitro assays and clinical outcome was also analyzed.
Outcome
Despite treatment, 37 (61.7 %) patients died within the first 5 years post-diagnosis. The mortality rate among patients with cryptococcal meningitis remains high in agreement with previous reports [1, 2, 14, 35, 36].
Several factors associated with fatal outcome, most related to low CD4 count, high intra-cranial pressure, and occurrence of concomitant diseases, among others, have been studied [1, 2, 16, 18, 35, 36]. In the present study, the median CD4 cells count was 37 (range 4–601). Interestingly, eight patients had CD4 cell count >200 cells/mL, and among them, only four survived. Although our findings were comparable to those reported in the literature [35, 36], it is important to remark that we only analyzed the CD4 count at the first and relapsed episodes, and no CD4 count over time was analyzed.
Regarding the occurrence of other diseases, tuberculosis plus meningitis was more associated with Died event than the other diseases. On the contrary, a lower association between cytomegalovirus plus meningitis and Survived event was observed.
Susceptibility Tests
All strains tested had MIC-RM and MIC-Etest values for amphotericin B ≤1 and ≤0.064 mg/L, respectively, indicating that all strains were susceptible to the antifungal drug tested. When compared to both the methods, the exact concordance of MIC-Etest with the reference method was of 12.2 %. Similar results were found by Dias et al. who communicated a low agreement of 5 % between Etest strips and the EDef 7.1 reference method [34]. Dannaoui et al. [38] compared the behavior of 659 strains of Candida spp. and 31 strains of C. neoformans against amphotericin B, flucytosine, fluconazole, itraconazole, voriconazole, and caspofungin by using Etest strips and EDef 7.1. They found that the C. neoformans strains showed 73.1 % of agreement ±2 dilutions with amphotericin B MIC in disagreement with our results of 25.7 % of agreement ±2 dilutions. Our results are also in disagreement with those reported by Mawell et al. and Ochiuzzi et al. who used Etest strips and the M27-A2 reference method [32, 37]. Maxwell et al. evaluated 162 strains of C. neoformans against amphotericin B and voriconazole and found 99 and 94 % of agreement, respectively, between both methods [32]. Ochiuzzi et al. [37] evaluated 266 isolates of C. neoformans by using the M27-A2 reference method and Etest strips and observed 33.5 % of exact concordance between both methods. To note, for the Etest strips, Ochiuzzi et al. used Mueller–Hinton agar instead of RPMI agar as recommended by the manufacturers. In addition, for MIC determination, Maxwell et al. and Ochiuzzi et al. used an inoculum of 0.5–2.5 × 103 CFU/mL, incubation in static condition at 35 °C, and final reading at 72 h, as recommended by the CLSI method [4]. Thus, comparison between these studies and our study is difficult, taking into account that the methods and technical conditions were different.
In the present study, the MIC-RM and MIC-Etest did no correlate with clinical outcome (p = 0.146), and thus the clinical relevance of these determinations is questionable and could limit the usefulness of this in vitro test for guiding therapy. Similar findings have been reported by other authors [13–15].
Minimal Fungicidal Concentration
In our study, MFC determination showed that several strains exhibited high values for amphotericin B (≥2 mg/L). Although MFC showed a better approximation to the clinical evolution, we observed no significant correlation between the value of MFC and MIC-RM for amphotericin B (p = 0.146). In a previous study, Rodero et al. [18] observed a better correlation with clinical evolution when MIC versus MFC and TKC were tested in a group of 16 AIDS patients.
It is possible that the technical factors that influence the results are still insufficiently known because only few studies have been developed for fungi. This leads to difficulties in interpreting the information provided by such determinations [21].
Time–Kill Curves
We evaluated the cidal activity of amphotericin B at 1 mg/L concentration that represents 2–5 times the MIC of the tested isolates by using TKC.
Burgess et al. [25] reported that amphotericin B has a fungistatic activity at concentrations ≤1 × MIC and that concentrations >1 × MIC are fungicidal for C. neoformans strains. Similar findings were also communicated for Klepser et al. [23] when Candida albicans was tested against amphotericin B. In the present study, in disagreement with Burgess’s and Klepser’s findings, the cidal activity was not observed in 50 % of the strains tested. Also, these strains were isolated from 26 patients, 25 (96.1 %) of whom died. Patients whose strains showed to be susceptible within the first 48 h had higher chance of survival; the opposite occurred with most patients whose strains were not susceptible to the antifungal drug. A significant correlation with outcome (p < 0.05) was observed.
We observed that the strains that were not inhibited with amphotericin B 1 mg/L were killed with ≥2 mg/L (data not shown). This means that we cannot consider these isolates as resistant, but we should rather consider the term tolerant, i.e., microorganisms that can tolerate high concentrations of antimicrobial fungicides without causing their death.
The tolerance phenomenon has been described for some species of bacteria, but little is known for fungi [20, 21]. In vitro tolerance could be related to the organism’s growth stage at the time of contact with the antimicrobial agent. It is possible that this tolerance reaction is present in the host in conditions in which microbial growth is slowed, for example, in patients suffering meningitis, osteomyelitis, or endocarditis. Thus, though antifungal therapeutic concentrations are available and suitable, the cell is refractory to them [20, 21].
Presumably if this phenomenon occurs in vivo, given the state of immunodeficiency of HIV/AIDS patients, it is not difficult to imagine that when the peak plasma concentration of the antimicrobial decreases, tolerant strains can regain their metabolic activity and further develop until a fungal mass is hardly eradicated by the host. It is important to note that when a strain is inhibited, but not killed by concentrations of 1 mg/L amphotericin B within the first 48 h, other treatment options should be considered.
It is important to point out that, in our study, the largest number of survivors (n = 15) was found among patients whose strains were completely inhibited within the first 24 h of in vitro exposure to amphotericin B. This situation could be of benefit to the host, since by dramatically reducing the fungal mass; the patient is given the possibility of a better clinical outcome. This finding is comparable to what happens with bacteria, since the prognosis for cure is higher when the bactericidal effect is evident within the first 24 h of exposure to the organism against antibacterial drugs [20]. A controversial finding was the fact that nine of 13 patients whose isolates met these criteria also died. According to data base records, among them, seven discontinued the antiretroviral treatment and fluconazole ambulatory treatment. Perhaps this situation contributed to fatal outcome.
Similar results were observed by Rodero et al. [18] in a previous study of 16 strains of C. neoformans obtained from 16 AIDS patients. In that study, the isolates that were inhibited at 12–48 h against amphotericin B were obtained mostly from the group of patients that survived.
Pappalardo et al. [28] conducted a TKC study of 40 strains of C. neoformans obtained from 20 AIDS patients and found that seven (17.5 %) strains showed tolerance to amphotericin B, and regrowth of these strains was observed within 6–24 h after the fungicidal end point. However, in contrast with that found in the present study, they observed no correlation between the outcome (death or survival) and the occurrence of tolerant isolates. Furthermore, in our study, no regrowth was observed.
As discussed above, we observed a low correlation between the reference and commercial methods and outcome, perhaps due to the characteristics of C. neoformans growth, which makes the microorganism express differently depending on the culture medium in which it is developing. We also emphasized the difficulties interpreting results obtained from the susceptibility tests against C. neoformans and their real meaning when trying to correlate them with the outcome. Regardless of the technique used, we believe that, to date, the methods available do not ensure that results could correlate in vitro–in vivo and that they lead to less effective treatments.
To remark, the present study was subject to limitations. First, it was a retrospective laboratory-based study, thus, some clinical data were uncompleted or missing, and it was the reason because the sample size was small. Second, TKC assay is not a standardized method; it is time consuming and requires trained personnel, limiting their application to reference laboratories or research institutions. Despite these limitations, we believe that our contribution could be useful to study the behavior of C. neoformans against amphotericin B, although it is necessary to continue the development of new and better in vitro techniques.
Conclusions
The reference method EDef 7.2, the Etest strips, and the Neo-Sensitabs™ tablets failed to detect C. neoformans as not susceptible to amphotericin B. As previously reported, we found that TKC might be a useful tool to detect C. neoformans not susceptible to amphotericin B, better than standard in vitro susceptibility testing. In this group of patients, TKC seemed to correlate better with clinical outcome.
References
Negroni R, Helou SH, Lopez Daneri G, Robles AM, Arechavala A, Bianchi MH. Interrupción exitosa de la profilaxis secundaria antifúngica en la criptococosis asociada al SIDA. Rev Argent Microbiol. 2004;36:113–7.
Negroni R. Criptococosis. In: Benetucci J, editor. SIDA y enfermedades asociadas. Diagnóstico, clínica y tratamiento. 3rd ed. Buenos Aires: FUNDAI; 2008. p. 332–6.
Perfect JR, Dismukes WE, Dromer F, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:291–322.
Clinical and Laboratory Standards Institute. Reference method for broth dilution antifungal susceptibility testing of yeasts. Approved standard. CLSI document M27-A3. 3rd ed. Wayne: Clinical and Laboratory Standards Institute; 2008. p. 19087–1898.
Arendrup MC, Cuenca-Estrella M, Lass-Flörl C, Hope W and the Subcommittee on Antifungal Susceptibility Testing (AFST) of the ESCMID European Committee for Antimicrobial Susceptibility Testing (EUCAST). Eucast Definitive Document EDef 7.2 Revision. Method for the determination of broth dilution minimum Inhibitory concentrations of antifungal agents for yeasts. www.eucast.org (2012).
Rodríguez-Tudela JL, Martín-Diez F, Cuenca-Estrella M, Rodero L, Carpintero Y, Gorgojo B. Influence of shaking of antifungal susceptibility testing of Cryptococcus neoformans: a comparison of NCCLS Standard M27-A medium, buffered yeast nitrogen base, and RPMI-2 % glucose. Antimicrob Agent Chemoter. 2000;44:400–4.
Zaragoza O, Mesa-Arango AC, Gómez-López A, Bernal-Martínez L, Rodríguez-Tudela JL, Cuenca-Estrella M. Process analysis of variables for standardization of antifungal susceptibility testing of nonfermentative yeasts. Antimicrob Agents Chemother. 2011;55:1563–70.
Govender N, Patel J, van Wyk M, Chiller T, Lockhart SR, GERMS-AS. Trends in antifungal drug susceptibility of cryptococcus neoformans isolates obtained through population-based surveillance in South Africa in 2002–2003 and 2007–2008. Antimicrob Agents Chemother. 2011;55:2606–11.
Pfaller MA, Castanheira M, Diekema DJ, Messer SA, Jones RN. Wild-type MIC distributions and epidemiologic cutoff values for fluconazole, posaconazole, and voriconazole when testing Cryptococcus neoformans as determined by the CLSI broth microdilution method. Diagn Microbiol Infect Dis. 2011;71:252–9.
Espinel-Ingroff A, Aller AI, Canton E, et al. Cryptococcus neoformans–Cryptococcus gattii species complex: an international study of wild-type susceptibility endpoint distributions and epidemiological cutoff values for fluconazole, itraconazole, posaconazole and voriconazole. Antimicrob Agents Chemother. 2012;56:5898–906.
Espinel-Ingroff A, Chowdhary A, Cuenca-Estrella M, et al. Cryptococcus neoformans–Cryptococcus gattii species complex: an international study of wild-type susceptibility endpoint distributions and epidemiological cutoff values for amphotericin B and flucytosine. Antimicrob Agents Chemother. 2012;56:3107–13.
Li M, Liao Y, Chen M, Pan W, Weng L. Antifungal susceptibilities of Cryptococcus species complex isolates form AIDS and non-AIDS patients in southeast China. Braz Infect Dis. 2012;16:175–9.
Dannaoui E, Abdul M, Arpin M, et al. Results obtained with various antifungal susceptibility testing methods do not predict early clinical outcome in patients with cryptococcosis. Antimicrob Agents Chemother. 2006;50:2464–70.
Arechavala AI, Ochiuzzi ME, Borgnia MD, Santiso GM. Fluconazole and amphotericin B susceptibility testing of Cryptococcus neoformans: results of minimal inhibitory concentrations against 265 isolates from HIV-positive patients before and after two or more months of antifungal therapy. Rev Iberoam Micol. 2009;26:194–7.
Larsen RA, Bauer M, Pitisuttithum P, et al. Correlation of susceptibility of Cryptococcus neoformans to amphotericin B with clinical outcome. Antimicrob Agents Chemother. 2011;55:5624–30.
Lee Ch, Chang TY, Liu JW, et al. Correlation of anti-fungal susceptibility with clinical outcomes in patients with cryptococcal meningitis. BMC Infect Dis. 2012;12:361.
Rex JH, Chester R, Cooper JR, et al. Detection of amphotericin B-resistant candida isolates in a broth-based system. Antimicrob Agents Chemother. 1995;39:906–9.
Rodero L, Córdoba S, Cahn P, et al. Timed-kill curves for Cryptococcus neoformans isolated from patients with AIDS. Med Mycol. 2000;38:201–7.
Córdoba S, Afeltra J, Vitale RG. Evaluation of the in vitro activity of amphotericin B by time kill curves methodology against Cryptococcus neoformans encapsulated and capsulate-deficient strains. Diagn Microbiol Infect Dis. 2011;71:260–2.
National Committee for Clinical Laboratory Standards. Methods for determining bactericidal activity of antimicrobial agents: approved guideline. NCCLS document M26-A. Wayne, 1999.
Pfaller MA, Sheehan DJ, Rex JH. Determination of fungicidal activities against yeasts and molds: lessons learned from bactericidal testing and the need for standardization. Clin Microbiol Rev. 2004;17:268–80.
Mouton JW, Vinks AA. Pharmacokinetic/pharmacodynamic modelling of antibacterials in vitro and in vivo using bacterial growth and kill kinetics: the minimum inhibitory concentration versus stationary concentration. Clin Pharmacokinet. 2005;44:201–10.
Klepser MA, Wolfe EJ, Jones RN, Nightingale CH, Pfaller MA. Antifungal pharmacodynamic characteristics of fluconazole and amphotericin B tested against Candida albicans. Antimicrob Agents Chemother. 1997;42:1207–12.
Klepser ME, Ernst EJ, Lewis RE, Ernst ME, Pfaller MA. Influence of test conditions on antifungal time-kill curve results: proposal for standardized methods. Antimicrob Agents Chemother. 1998;42:1207–12.
Burgess DS, Hastings RW. A comparison of dynamic characteristics of fluconazole, itraconazole, and amphotericin B against Cryptococcus neoformans using time-kill methodology. Diagn Microbiol Infect Dis. 2000;38:87–93.
Ernst EJ, Yodoi K, Roling EE, Klepser ME. Rates and extents of antifungal activities of amphotericin B, flucytosine, fluconazole, and voriconazole against Candida lusitaniae determined by microdilution, Etest, and time-kill methods. Antimicrob Agents Chemother. 2002;46:578–81.
Sandoval-Denis M, Pastor FJ, Capilla J, Sutton DA, Fothergill AW, Guarro J. In Vitro pharmacodynamics and in vivo efficacy of fluconazole, amphotericin B and caspofungina in a murine infection by Candida lusitaniae. Int J Antimicrob Agents. 2014;43:161–4.
Pappalardo MCSM, Szeszs MW, Martins MA, et al. Susceptibility of clinical isolates of Cryptococcus neoformans to amphotericin B using time-kill methodology. Diagn Microbiol Infect Dis. 2009;64:146–51.
Kurtzman CP, Fell JW. The yeast, a taxonomic study. 5th ed. Amsterdam: Elsevier; 2011.
Ikeda R, Shinoda T, Fukazawa Y, Kaufman L. Antigenic characterization of Cryptococcus neoformans serotypes and its application to serotyping of clinical isolates. J Clin Microbiol. 1982;16:22–9.
Neo-Sensitabs user’s guide; A/S Rosco Diagnostica, Taastrup, Denmark. 2007. http://www.rosco.uk.
Maxwell MJ, Messer SA, Hollis RJ, Diekema DJ, Pfaller MA. Evaluation of Etest method for determining voriconazole and amphotericin B MICs for 162 clinical isolates of Cryptococcus neoformans. J Clin Microbiol. 2003;41:97–9.
Cuenca-Estrella M, Gomez-Lopez A, Alastruey-Izquierdo A, et al. Comparison of the Vitek 2 antifungal susceptibility system with the Clinical and Laboratory Standards Institute (CLSI) and European Committee on Antimicrobial Susceptibility Testing (EUCAST) broth microdilution reference methods and with the Sensititre YeastOne and Etest techniques for in vitro detection of antifungal resistance in yeast isolates. J Clin Microbiol. 2010;48:1782–6.
Dias ALT, Matsumoto FE, Melhem MSC, et al. Comparative anlysis of Etest and broth microdilution method (AFST-EUCAST) for trends in antifungal drug susceptibility testing of Brazilian Cryptococcus neoformans isolates. J Med Microbiol. 2006;55:1693–9.
Sow D, Clement Tine R, Sylla K, et al. Cryptococcal meningitis in Senegal: epidemiology, laboratory findings, therapeutic and outcome of cases diagnosed from 2004 to 2011. Mycopathologia. 2013;176:443–9.
Meda J, Kalluvya S, Downs JA, et al. Cryptococcal meningitis management in Tanzania with strict schedule of serial lumber punctures using intravenous tubing sets: an operational research study. J Acquir Immune Defic Syndr. 2014;66(2):e31–6. doi:10.1097/QAI.0000000000000147.
Ochiuzzi ME, Santiso GM, Arechavala AI. Correlation of Etest and neo-sensitabs diffusion assays on Mueller–Hinton-methylene blue agar with broth microdilution reference method (CLSI-M27-A2) for testing susceptibilities of Cryptococcus neoformans to amphotericin B and fluconazole. Med Mycol. 2010;48:893–6.
Dannaoui E, Paugam A, Develoux M, et al. Comparison of antifungal MICs for yeasts obtained using the EUCAST method in a reference laboratory and the Etest in nine different hospital laboratories. Clin Microbiol Infect. 2010;16:863–9.
Acknowledgements
We thank Alicia Trovero from the Instituto Nacional de Producción de Biológicos, ANLIS “Dr. C. G Malbrán” (Buenos Aires, Argentina), for her collaboration with serotype determinations.
Conflict of interest
None.
Ethical standard
This study did not need an ethics committee approval because it did not include direct contact, personal information, or clinical samples of patients, just isolates.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Córdoba, S., Vivot, W., Szusz, W. et al. Comparison of Different In Vitro Tests to Detect Cryptococcus neoformans Not Susceptible to Amphotericin B. Mycopathologia 179, 359–371 (2015). https://doi.org/10.1007/s11046-015-9871-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-015-9871-8