Abstract
The emergence of antifungal resistance among Cryptococcus neoformans isolates is a matter of great concern. The Clinical and Laboratory Standards Institute (CLSI) broth microdilution reference method (BMD) for antifungal susceptibility testing of C. neoformans is tedious and time-consuming. Consequently, there is a greater need for a reproducible in vitro susceptibility testing method for use in clinical microbiology laboratories. By random amplified polymorphic DNA analysis, the 62 Indian clinical isolates were characterized as Cryptococcus neoformans var. grubii. We evaluated the susceptibilities of these isolates for amphotericin B (AMB) and fluconazole (FLC) by two commercial techniques, i.e., Vitek 2 and E-test against the CLSI M27-A3 BMD. The essential agreement (EA) between the Vitek 2 and E-test with the reference procedure for FLC was similar (82.2%). For AMB, EA of 92 and 76% was obtained with E-test and Vitek 2. Excellent categorical agreement (CA) (98.3% and 100% by Vitek 2 and E-test, respectively) was obtained for AMB. The CA for FLC was 81 and 77.4% by Vitek 2 and E-test. We conclude that both E-test and Vitek 2 system have acceptable levels of accuracy for susceptibility testing of both the drugs. Both of them could identify fluconazole-resistant strains. Vitek 2 could be used for testing susceptibility of voriconazole and 5-flucytosine also at the same time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There has been a dramatic rise in the incidence of cryptococcal infections during the past three decades, with the advent of acquired immunodeficiency syndrome (AIDS) pandemic [1]. Incidence among immunocompetent patients has also reportedly risen over recent years [2]. Even after the introduction of highly active anti-retroviral therapy (HAART), cryptococcal meningitis remains the most common life-threatening fungal infection among AIDS patients with reported mortality rate of 2.5–15% [3]. Emergence of fluconazole resistance during long-term therapy has been reported in several cases of AIDS-associated cryptococcal meningitis [4]. Along with it, recent reports of expression of heteroresistance to fluconazole demonstrated in few clinical isolates of Cryptococcus neoformans invite the risk of therapeutic failure and relapse which is inevitably fatal [5]. Reports of treatment failure attributable to the development of amphotericin B resistance by C. neoformans further necessitate validating simple alternative antifungal susceptibility testing methods for use in clinical microbiology laboratories [6, 7].
The standard document of reference procedures for antifungal susceptibility testing of yeasts and molds is available from the CLSI and the European Committee on Antimicrobial Susceptibility Testing (EUCAST). There are difference between the two methods in inoculum, test medium, microtitre wells, end-point reading, and breakpoints [7]. The Vitek 2 antifungal susceptibility test system (BioMe′rieux, Hazelwood, France) is a fully automated commercial system that determines yeast growth spectrophotometrically and thus enables simultaneous fungal identification and MIC determination. E-test (BioMe′rieux, Hazelwood, France), an agar-based predefined concentration gradient method for determining the MICs of various agents, is also available for antifungal susceptibility testing [7, 8]. Earlier studies, which have evaluated VITEK 2 or E-test with CLSI and the EUCAST, have shown them to be reliable techniques to determine antifungal susceptibility testing of yeast species and more rapid and easier alternative for clinical laboratories than the procedures developed by either the CLSI or the EUCAST. Although these two commercial systems have been extensively studied for various Candida spp., there are few reports of performance of these systems for antifungal susceptibility testing of C. neoformans [7, 9, 10].
The purpose of the present study was to do the molecular characterization of the clinical isolates of Cryptococcus from India and to evaluate the two commercial techniques, Vitek 2 and E-test, for antifungal susceptibility testing against those isolates by comparing the results with the CLSI reference procedures.
Materials and Methods
Isolates
A total of 62 clinical isolates of C. neoformans were included (12 from HIV-positive patients and 50 from non-HIV patients). Out of 62 isolates, 57 were isolates from cerebrospinal fluid (CSF), 3 were from tracheal aspirate, and 1 each were isolated from blood and sputum, respectively. Isolates from CSF were inclusive of nine serial isolates of the same patient from different clinical episodes of meningitis. All the isolates in the study were obtained from immunosuppressed patients. C. neoformans ATCC 14116, Candida parapsilosis ATCC 22019, and Candida Krusei ATCC 6258 were also included as control strains.
Variety Differentiation
In our laboratory, we used canavanine–glycine–bromthymol blue (CGB) agar, which determines the use of glycine as a carbon source for variety differentiation as recommended by Kwon-Chung et al. [11]. A color change from light yellow green to cobalt blue was considered a positive result for the CGB test, indicating C. neoformans var. gattii (serotype B/C); otherwise, no color change was considered a negative result, indicating C. neoformans (serotype A/D).
Molecular Characterization
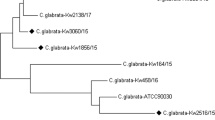
Random amplified polymorphic DNA (RAPD) analysis was the DNA typing technique done for the molecular characterization of the isolates of C. neoformans.
-
(a)
DNA extraction was done by following method of Franzot et al. [12].
-
(b)
PCR high-molecular-weight DNA from C. neoformans strains were subjected to PCR amplification, and analysis was done using the oligonucleotide minisatellite core sequence of wild-type M13 phage (5′GAGGGTGGCGGTTCT3′) and (GACA)4 primers (Meyer et al. [13]. The reactions were performed in a final volume of 50 μl with 30 ng of high-molecular-weight genomic cryptococcal DNA, 0.01 ng primers, 5U Taq polymerase, 10 mM Tris–Hcl, pH 8.3, 50 mM Kcl, 1.5 mM MgCl2, 0.02 mM each of GTP, CTP, ATP, and TTP. The amplification was performed for 40 cycles in a Eppendorf thermal cycler with predwelling at 94°C for 5 min, denaturation at 94°C for 1 min, annealing at 52°C for 1 min, extension at 72°C for 1 min, and a final extension cycle at 72°C for 10 min. The amplification products were separated on 1.4% agarose gel stained by ethidium bromide at a concentration of 10 mg/ml stock to a final concentration of 0.1 μg/ml in 1× TBE(Tri-Borate EDTA) for 72 h at 3 V/cm and observed under UV light.
Antifungal Susceptibility Testing
Broth Microdilution Method
In vitro susceptibility of C. neoformans isolates to fluconazole and amphotericin B was tested using the standard broth microdilution method as recommended by the CLSI M27-A3 protocol [14]. Fluconazole and amphotericin B were obtained as powders from Himedia Laboratories Pvt. Ltd., Mumbai. Stock solutions of amphotericin B and fluconazole were prepared using dimethyl sulphoxide and sterile distilled water, respectively. Stock solutions were diluted with RPMI 1640 (RPMI tissue culture medium supplemented with glutamine) (Himedia Laboratories Pvt. Ltd., Mumbai) with 2% glucose, buffered to pH 7.0 with 0.156 M 3-N-morpholinopropane-sulphonic acid (MOPS; Sisco Research Laboratories Pvt Ltd Mumbai). The final concentrations were 0.12–64 mg/l for fluconazole and 0.03–16 mg/l for amphotericin B. The final inoculum concentration ranged from 0.5 × 103 to 2.5 × 103 for CLSI broth microdilution method. Testing was performed in 96-well round-bottomed microtitre plates, and the plates were incubated at 35°C for 48–72 h. The MICs of fluconazole were read as the lowest concentration of the agent, which inhibited growth by 50%. For amphotericin B, the MIC was the lowest concentration of drug that completely inhibited growth.
E-test Method
Fluconazole and amphotericin B E-test strips were purchased from BioMe′rieux (BioMe′rieux, Hazelwood, France). The concentration gradient for fluconazole ranged from 0.16 to 256 μg/ml and that for amphotericin B ranged from 0.002 to 32 μg/ml [E-test package insert]. The strips were stored at −20°C until use. The agar formulation used was RPMI 1640 (Himedia Laboratories Pvt. Ltd., Mumbai), supplemented with 1.5 agar and 2% glucose, and buffered with MOPS [15]. A plate of 90 mm diameter containing RPMI 1640 and 2% glucose with 1.5% agar to a depth of 4.0 mm was used. The inoculated suspensions of C. neoformans isolates in 0.85% saline were matched with the turbidity of no. 1 McFarland standard by adjusting to the appropriate turbidity via a spectrophotometer (530 nm wavelength). The agar surface was inoculated using a non-toxic sterile swab. After the excess moisture was absorbed into the agar and the surface was completely dry, E-test strip was applied to each plate. The plates were incubated at 35°C and read at 48–72 h. The MIC was read, where the border of the elliptical inhibition zone intersected the scale on the antifungal strip. The fluconazole MICs were read at the lowest concentration at which the border of the elliptical inhibition zone intersected the scale on the strip. The amphotericin B MICs were read at the point at which a zone of almost complete inhibition intersected the strip. Illustrations for the interpretation of the results, as provided by the manufacturer, were consulted [E-test package insert].
Vitek 2
Susceptibility testing with the Vitek 2 system was performed according to the manufacturer’s instructions. Briefly, the inoculum suspensions were prepared from 48-h-old cultures of C. neoformans and adjusted to a turbidity equivalent to 2 McFarland units. This suspension was placed into the provided Vitek 2 cassette along with a sterile polystyrene test tube and a yeast susceptibility test card [AST-YS01, Ref 22108]. The drug concentrations in the AST-YS01 yeast susceptibility test card ranged from 0.25 to 16 μg/ml for amphotericin B, from 1 to 64 μg/ml for fluconazole, from 0.125 to 16 μg/ml for voriconazole, and from 1 to 64 μg/ml for 5-flucytosine. The loaded cassettes were then placed into Vitek 2 instrument. MIC end-points were determined spectrophotometrically by automated equipments. The results were expressed as MICs in μg/ml.
Analysis of Results
Comparison between the test methods (E-test vs. CLSI M27-A3 and Vitek 2 card test vs. CLSI M27-A3) was made on the basis of the MIC results and categorical results. CLSI M27-A3 was referred for MIC interpretative guidelines [14]. For fluconazole, C. neoformans isolates with MIC ≤8 μg/ml were considered sensitive, those with MIC 16–32 μg/ml were considered susceptible dose dependent (SDD), and isolates with MIC ≥64 μg/ml were considered resistant [14]. Although the interpretative breakpoints for amphotericin B have not been defined by the CLSI, it has been suggested that isolates for which MICs are ≥1 μg/ml are considered as resistant [15].
As the E-test strips have a continuous gradient of concentration, the MICs in between twofold dilutions were raised to the closest upper twofold dilution value [16]. The essential agreement (EA) between the methods was defined when the MIC results were within a two dilution ranges. Categorical agreement (CA) was defined when the two methods agreed with respect to the MIC categories.
Very major errors were defined when the isolate was resistant by the reference method but susceptible by the other method. Major errors occurred when the isolate was susceptible by the reference method but resistant by the other method, and minor errors were identified when the isolate identified by one of the methods was susceptible or resistant and by the other method was susceptible dose dependent.
The reproducibility of Vitek 2 was evaluated by testing 11 of the 62 isolates at least twice on different days. Reproducibility was defined when MIC results were within a plus or minus two dilution ranges [10].
Results
All the 62 isolates could not change the yellow color of CGB medium, indicating that they were C. neoformans (serotype A/D). By RAPD analyses, all the isolates examined were VN1 (C. neo var. grubii, serotype A). The RAPD fingerprinting pattern was similar in sequential isolates from a patient. Both primary and relapse isolates of another patient also showed similar fingerprinting patterns.
The in vitro susceptibilities of the isolates of C. neo var. grubii to FLC and AMB were determined. The MIC values were same in 3 sequential isolates of 1 patient with one log2 dilution decrease in the first isolate. In 2 other patients, there was no difference in MIC values of 1st isolate and the relapse isolate.
In vitro susceptibility testing of 62 clinical isolates was done by the three methods, i.e., CLSI M27-A3, E- test, and Vitek 2 system. The MIC range and MIC90 (the MICs at which 90% of the isolates tested were inhibited for each drug) recorded at 72 h for the two drugs tested by three methods are given in Table 1. For FLC, MIC90 determined by E-test and CLSI was similar, but the MIC90 determined by Vitek 2 (8 μg/ml) was less in comparison. The MIC range of E-test and Vitek 2 was more when compared to CLSI method. For AMB, there was difference of only one dilution in MIC90 by E-test (0.25 μg/ml) and Vitek 2 (1 μg/ml) when compared with CLSI (0.5 μg/ml) method.
The percentage MICs by different categories for the two drugs as determined by the three methods are given in Table 2. The overall percentage of sensitive and SDD strains determined by CLSI and E-test was almost similar, but Vitek 2 determined more sensitive and less SDD strains when compared to CLSI method. Both E-test and Vitek 2 were able to detect a fluconazole-resistant strain of a HIV patient, showing MIC of >256 and >64 μg/ml, respectively. By CLSI method, also, a higher MIC of 16 μg/ml was detected for this strain. For AMB, the categorical MICs were similar for the three methods except in one strain that showed a little higher MIC (2 μg/ml) by Vitek 2 system on repeat testing.
Table 3 shows the essential agreement and the categorical agreement along with the categorical errors when the two tests were compared with the CLSI reference method. The essential agreements by the two tests were similar (82.2%) for FLC, but the categorical agreement of Vitek 2 with CLSI was slightly higher (80.7%) when compared to E-test (77.4%) with CLSI. No very major error or major error occurred but minor errors by E-test were slightly more (22.5%) when compared to Vitek 2 test (19.3%). Both CA (100%) and EA (91.9%) of E-test were higher for AMB when compared to the Vitek 2 system, which detected CA (98.39%) and EA (75.8%), respectively.
The Vitek 2 system provided the antifungal data for all the four drugs within a mean time of 24.25 h. Almost all the isolates were sensitive to voriconazole with MIC <0.12 μg/ml. Among all isolates, five were analyzed as intermediate with MICs (8–16 μg/ml) to 5-flucytosine, and rest of all were sensitive with MIC ≤4 μg/ml. The intralaboratory reproducibility of Vitek 2 system for the four agents was 100% for voriconazole, 90.9% for fluconazole and 5-flucytosine, and 63.6% for amphotericin B.
Discussion
Cryptococcus neoformans is a most important opportunistic fungal pathogen that causes localized and/or disseminated life-threatening infection in humans. All the patients included in our study were infected with serotype A (C.neo var. grubii) by RAPD method, which is similar to the predominant serotype earlier isolated in India by Jain et al. [17] and in most countries by Mitchell and Perfect [18].This is also consistent with reports that C.neo var. grubii is prevalent among immunosuppressed and healthy patients that are afflicted with cryptococcosis [19].
There was no significant difference in MIC values of serial isolates obtained from the same patient. This is similar to a surveillance study, where no significant shift in MICs of AMB for C. neoformans has been determined when serial isolates of C. neoformans were obtained from patients in a span of 6 years despite the widespread use of antifungal agents in persons with AIDS by Brandt et al. [20]. Both the primary and relapse isolate of patients showed similar fingerprinting patterns revealing persistence of the same strain despite antifungal therapy as has been found earlier by Brandt et al. [21] and Spitzeret et al. [22].
The use of antifungal agents particularly in long-term suppressive regimens has raised concern about the development of drug resistance in C. neoformans. Although the resistance is rare among clinical isolates of C. neoformans but has been reported by Pfaller et al. [23] and Franzot and Hamdan [24], in our study, we have documented absence of resistance among C. neoformans isolates from India, which is consistent with earlier data published by Klepser and Pfaller [25].
The objective of the present study was to validate the performance of two commercially available systems for antifungal susceptibility testing in our laboratory before implementing the test systems for clinical use. In this study by CLSI M27-A3 method, none of the C. neoformans isolates were resistant to amphotericin B and fluconazole. Our MIC90 of FLC is higher than other studies [10, 26] but similar to a study by Datta et al. [27] and for AMB is similar to a study by Gonzalez Cejudo et al. [10] but lower than a study by Capoor et al. [26].
The MIC90 and MIC range of fluconazole and amphotericin B by E-test are almost similar to the previous studies, but our study had similar CA for amphotericin B and 77.4% for fluconazole, contrary to the study by Capoor et al. which had reported almost similar CA of E-test with CLSI reference method for both the drugs [26].
In our study, the EA between E-test and CLSI method for fluconazole was 81.1%, which is similar to that obtained by Aller et al. but lower than that reported by Colombo et al. (96%) and higher than that reported by Espinel-Ingroff et al. (70%) [16, 28, 29]. The EA between E-test and CLSI method for amphotericin B was very low in previously published studies [16]. In a study by Aller et al., amphotericin B had the lowest agreement (8.1% when tested on antibiotic medium 3, 13.5% on RPMI) [16]. Similar findings (5% essential agreement) were reported by Dias et al. [30]. However, we found very good essential agreement (92%) between E-test and CLSI method for AMB.
Our MIC90 (8 μg/ml) and MIC range (≤1–≥64 μg/ml) for FLC obtained by Vitek 2 system were slightly higher than the study by Gonzalez Cejudo et al. (MIC90 4 μg/ml, MIC range (≤1–≥32 μg/ml); however, MIC90 and MIC range for AMB were comparable in both studies [10]. Our CA was almost similar for AMB (98.4%) but less for FLC (80.7%) when compared to a study by Gonzalez Cejudo et al. [10]. Regarding the CA between the Vitek 2 and reference procedures, there were no very major errors, and most errors detected were minor errors (for fluconazole). Only one major error was detected for amphotericin B. This occurred due to one isolate that showed slightly higher MIC (2 μg/ml) by Vitek 2. In Vitek 2, MICs of all four antifungal agents amphotericin B, fluconazole, voriconazole, and 5-flucytosine were obtained simultaneously for all isolates in this study. Voriconazole susceptibility could be tested in only 13.5% isolates in a study by Cejudo et al. [10].
There are not many published reports that have evaluated E-test along with Vitek 2 system with CLSI for Cryptococcus isolates except a recent report by Cuenca-Estrella et al., which compared these methods for in vitro detection of antifungal resistance in yeast isolates [7]. This is one of the first studies that have compared E-test, Vitek 2 system with CLSI against Cryptococcus isolates. Despite our slightly lower levels of concordance in MIC results for fluconazole by Vitek 2 system, we conclude that both E-test and Vitek 2 system have acceptable levels of accuracy for susceptibility testing of FLC and AMB. Both of them were able to identify fluconazole-resistant strains. Vitek 2 could be used for testing susceptibility of 5-flucytosine and voriconazole also at the same time.
References
Banerjee U, Datta K, Majumdar T, Gupta K. Cryptococcosis in India: the awakening of a giant? Med Mycol. 2001;39:51–67.
Shih CC, Chen YC, Chang SC, Luh KT, Hsieh WC. Cryptococcal meningitis in non-HIV-infected patients. Q J Med. 2000;93:245–51.
Antinori S, Ridolfo A, Fasan M, Magni C, Galimberti L, Milazzo L, Sollima S, Adorni F, Giuliani G, Galli M, Corbellino M, Parravicini C. AIDS-associated cryptococcosis: a comparison of epidemiology, clinical features and outcome in the pre- and post-HAART eras. Experience of a single centre in Italy. 2009. HIV Med. 2009;10:6–11.
Friese G, Discher T, Fussle R, Schmalreck A, Lohmeyer J. Development of azole resistance during fluconazole maintenance therapy for AIDS associated cryptococcal disease. AIDS. 2001;15:2344–5.
Mondon P, Petter R, Amalfitano G, Luzzati R, Concia E, Polacheck I, Kwon-Chung KJ. Heteroresistance to fluconazole and voriconazole in Cryptococcus neoformans. Antimicrob Agents Chemother. 1999;49:1856–61.
Silva PR, Rabelo RA, Terra AP, Teixeira DN. Susceptibility to antifungal agents among Cryptococcus neoformans varieties isolated from patients at a university hospital. Rev Soc Bras Med Trop. 2008;41:158–62.
Cuenca-Estrella M, Gomez-Lopez A, Alastruey-Izquierdo A, Bernal-Martinez L, Cuesta I, Buitrago MJ, Rodriguez-Tudela JL. Comparison of the Vitek 2 Antifungal susceptibility system with the Clinical and Laboratory Standards Institute (CLSI) and European Committee on Antimicrobial susceptibility testing (EUCAST) broth microdilution reference methods and with the sensititre yeast one and Etest techniques for in vitro detection of antifungal resistance in yeast isolates. J Clin Microbiol. 2010;48:1782–6.
Chryssanthou E, Grönfors C, Khanna N. Comparison of broth macrodilution, broth microdilution and E-test susceptibility tests of Cryptococcus neoformans for fluconazole. Mycoses. 1997;40:423–7.
Bourgeois N, Dehandschoewercker L, Bertout S, et al. Antifungal susceptibility of 205 Candida spp. isolated primarily during invasive Candidiasis and comparison of the Vitek 2 system with the CLSI broth microdilution and Etest methods. J Clin Microbiol. 2010;48:154–61.
González MT, González A, Cantón E, Aller AI, Romero A, Pemán J, Quindós G, Martín-Mazuelos E. Evaluation of the VITEK 2 system to test the susceptibility of Candida spp., Trichosporon asahii and Cryptococcus neoformans to amphotericin B, flucytosine, fluconazole and voriconazole: a comparison with the M27–A3 reference method. Med Mycol. 2010;48:710–9.
Kwon-Chung KJ, Polacheck I, Popkin TJ. Melanin lacking mutants of Cryptococcus neoformans and their virulence for mice. J Bacteriol. 1982;150:1414–21.
Franzot SP, Hamdan JS, Currie BP, Casadevall A. Molecular epidemiology of Cryptococcus neoformans in Brazil and the United States evidence for both local genetic difference and a global clonal population structure. J Clin Microbiol. 1997;35:2243–51.
Meyer W, Mitchell TG, Freedman EZ, Vilgalys R. Hybridization probes for conventional DNA fingerprinting used as single primers in the polymerase chain reaction to distinguish strains of Cryptococcus neoformans. J Clin Microbiol. 1993;31:2274–80.
Clinical and Laboratory Standards Institute. Reference method for broth dilution antifungal susceptibility testing of yeasts. Approved Standard third edition, M27-A3.Wayne, PA; 2008.
Lozano-Chiu M, Paetznick VL, Ghannoum MA, Rex JH. Detection of resistance to amphotericin B among Cryptococcus neoformans clinical isolates: performances of three different media assessed by using E-test and National Committee for Clinical Laboratory Standards M27-A methodologies. J Clin Microbiol. 1998;36:2817–22.
Aller AI, Martín-Mazuelos E, Gutiérrez MJ, Bernal S, Chávez M, Recio FJ. Comparison of the Etest and microdilution method for antifungal susceptibility testing of Cryptococcus neoformans to four antifungal agents. J Antimicrob Chemother. 2000;46:997–1000.
Jain N, Wickes BL, Keller SM, Casadevall A, Jain P, Ragan MA, Banerjee U, Fries BC. Molecular epidemiology of clinical Cryptococcus neoformans strains from India. J Clin Microbiol. 2005;43:5733–42.
Mitchell TG, Perfect JR. Cryptococcosis in the era of AIDS-100 years after the discovery of Cryptococcus neoformans. Clin Microbiol Rev. 1995;8:515–48.
Clark RA, Greer DL, Atkinson W, Valainis GT, Hyslop N. Spectrum of Cryptococcus neoformans infection in 68 patients infected with human immunodeficiency virus. Rev Infect Dis. 1990;12:768–77.
Brandt ME, Pfaller MA, Hajjeh RA, Hajjeh RA, Hamill RJ, Pappas PG, Reingold AL, et al. Trends in antifungal drug susceptibility of Cryptococcus neoformans isolates in the United States: 1992 to 1994 and 1996 to 1998. Antimicrob Agents Chemother. 2001;45:3065–9.
Brandt ME, Pfaller MA, Hajjeh RA, Graviss EA, Rees J, Spitzer ED, Pinner RW, Mayer LW, Cryptococcal Disease Active Surveillance Group. Molecular subtypes and antifungal susceptibilities of serial Cryptococcus neoformans isolates in human immunodeficiency virus associated Cryptococcosis. J Infect Dis. 1996;174:812–20.
Spitzer ED, Spitzer SG, Freundlich LF, Casadevall A. Persistence of initial infection in recurrent Cryptococcus neoformans meningitis. Lancet. 1993;341:595–6.
Pfaller M, Zhang J, Messer S, Tumberland M, Mbidde E, Jessup C, Ghannoum M. Molecular epidemiology and antifungal susceptibility of Cryptococcus neoformans isolates from Ugandan AIDS patients. Diagn Microbiol Infect Dis. 1998;32:191–9.
Franzot SP, Hamdan JS. In vitro susceptibilities of clinical and environmental isolates of Cryptococcus neoformans to five antifungal drugs. Antimicrob Agents Chemother. 1996;40:822–4.
Klepser ME, Pfaller MA. Variation in electrophoretic karyotype and antifungal susceptibility of clinical isolates of Cryptococcus neoformans at a university affiliated teaching hospital from 1987 to 1994. J Clin Microbiol. 1998;36:3653–6.
Capoor MR, Mandal P, Deb M, Aggarwal P, Banerjee U. Current scenario of cryptococcosis and antifungal susceptibility pattern in India: a cause for reappraisal. Mycoses. 2008;51:258–65.
Datta K, Jain N, Sethi S, Rattan A, Casadevall A, Banerjee U. Fluconazole and itraconazole susceptibility of clinical isolates of Cryptococcus neoformans at a tertiary care centre in India: a need for care. J Antimicrob Chemother. 2003;52:683–6.
Colombo AL, Barchiesi F, McGough DA, Rinaldi MG. Comparison of E-test and National Committee for Clinical Laboratory Standards broth macrodilution method for azole antifungal susceptibility testing. J Clin Microbiol. 1995;33:535–40.
Espinel-Ingroff A, Pfaller M, Erwin ME, Jones RN. Interlaboratory evaluation of E-test method for testing antifungal susceptibilities of pathogenic yeasts to five antifungal agents by using Casitone agar and solidified RPMI 1640 medium with 2% glucose. J Clin Microbiol. 1996;34:848–52.
Dias AL, Matsumoto FE, Melhem MS, da Silva EG, Auler ME, de Siqueira AM, Paula CR. Comparative analysis of Etest and broth microdilution method (AFST-EUCAST) for trends in antifungal drug susceptibility testing of Brazilian Cryptococcus neoformans isolates. J Med Microbiol. 2006;55:1693–9.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tewari, A., Behera, B., Mathur, P. et al. Comparative Analysis of the Vitek 2 Antifungal Susceptibility System and E-test with the CLSI M27-A3 Broth Microdilution Method for Susceptibility Testing of Indian Clinical Isolates of Cryptococcus neoformans . Mycopathologia 173, 427–433 (2012). https://doi.org/10.1007/s11046-012-9528-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-012-9528-9