Abstract
Background
Mitochondria are known to be involved in mediating the calorigenic effects of thyroid hormones. With an abundance of these hormones, alterations in energy metabolism and cellular respiration take place, leading to the development of cardiac hypertrophy. Vitamin D has recently gained attention due to its involvement in the regulation of mitochondrial function, demonstrating promising potential in preserving the integrity and functionality of the mitochondrial network. The present study aimed to investigate the therapeutic potential of Vitamin D on cardiac hypertrophy induced by hyperthyroidism, with a focus on the contributions of mitophagy and apoptosis as possible underlying molecular mechanisms.
Methods and results
The rats were divided into three groups: control; hyperthyroid; hyperthyroid + Vitamin D. Hyperthyroidism was induced by Levothyroxine administration for four weeks. Serum thyroid hormones levels, myocardial damage markers, cardiac hypertrophy indices, and histological examination were assessed. The assessment of Malondialdehyde (MDA) levels and the expression of the related genes were conducted using heart tissue samples. Vitamin D pretreatment exhibited a significant improvement in the hyperthyroidism-induced decline in markers indicative of myocardial damage, oxidative stress, and indices of cardiac hypertrophy. Vitamin D pretreatment also improved the downregulation observed in myocardial expression levels of genes involved in the regulation of mitophagy and apoptosis, including PTEN putative kinase 1 (PINK1), Mitofusin-2 (MFN2), Dynamin-related Protein 1 (DRP1), and B cell lymphoma-2 (Bcl-2), induced by hyperthyroidism.
Conclusions
These results suggest that supplementation with Vitamin D could be advantageous in preventing the progression of cardiac hypertrophy and myocardial damage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is well known that thyroid hormones are essentially involved in the regulation of numerous metabolic processes in nearly all body organs. Hence any disturbances in thyroid hormone levels have detrimental impacts on the whole body, particularly in the cardiovascular system [1]. Hyperthyroidism is a pathological condition characterized by the persistent overproduction of thyroid hormones by the thyroid gland [2], which, apart from its direct effects on altering cardiac function, has been shown to be associated with derangement of certain molecular pathways that could underlie the structural and functional changes of the heart leading to cardiac remodeling [3].
Cardiac hypertrophy is a clinical abnormality defined by an enlargement of myocardial mass that has been considered to be one of the most lethal consequences of hyperthyroidism, which consists of chronic maladaptive changes in cellular metabolic processes that eventually leading to heart failure [4]. Despite several possible mechanisms having been suggested over the past decades to explain the cardiac hypertrophy induced by hyperthyroidism, the leading cause of this pathogenesis remains controversial.
In recent studies taking into account the intensification of metabolism caused by hyperthyroidism, impaired energy homeostasis has been considered as a new aspect in the possibility of developing cardiac hypertrophy. Therefore, mitochondria as organelles in which most of the metabolic transformations and energy production take place, have emerged as the target of studying the pathogenesis of hyperthyroidism [5, 6]. The high-volume density of the cardiac functional mitochondria, besides supplying energy for the continuous contraction activity, is involved in the coordination of metabolic transduction, calcium buffering, and cell survival and death pathways. Accordingly, maintaining a normal population of functional mitochondria is essential for cardiomyocytes viability and their responsiveness to physiological and pathological stimuli [7]. There is significant evidence that impaired mitochondrial homeostasis is intimately linked to the onset of hypertrophic responses and transition to heart failure [8].
Normally, the homeostasis of the mitochondrial network is preserved by a set of mechanisms known as mitochondrial quality control (MQC) comprising recognition and targeting the damaged mitochondria to the clearance system through the mitophagy process and their replacement with healthy ones via mitochondrial biogenesis [9]. Deficiency of these processes during cardiac disorders affects virtually all functional aspects of mitochondria, including respiration, energy production, and apoptosis, and predisposes the heart to energy crisis and failure progression [10]. Recent reports have characterized insufficient or impaired mitophagy as a major contributor to the development of cardiovascular disease [11]. Mitophagy refers to a specific subtype of autophagy that directs dysfunctional mitochondria to be eliminated or recycled by autophagosomes. Interrupted mitophagy, following the accumulation of defective mitochondria, exposes cardiomyocytes to oxidative stress and eventually cell death, which could favor the progression of cardiac hypertrophy [12].
The most studied mechanism of mitophagy involves the interplay between PTEN putative kinase 1 (PINK1) and the mitochondrial fusion protein (MFN2). In fact the PINK1/MFN2 signaling pathway is upstream of events that recognize defective mitochondria to autophagy adapter proteins through the Parkin-dependent pathway [13]. Previous investigations have shown that the inhibition of either PINK1 or MFN2 is associated with the development of pathological cardiac hypertrophy and left ventricular dysfunction [14, 15]. Hyperthyroidism results in a reduction in the expression of PINK1 within cardiac tissue [10], the restoration of mitophagy could be ameliorated cardiac hypertrophy induced by hyperthyroidism. Furthermore, the efficient removal of damaged mitochondria through mitophagy is primarily dependent on the consistent occurrence of mitochondrial fission process to separate defective mitochondria from the intact population, which is mainly driven by Dynamin related protein 1 (DRP1) [16]. It has been documented in prior studies that DRP1-deficient animals exhibited a deterioration in mitophagy, along with progressive development of cardiac hypertrophy and dysfunction [17, 18].
On the other hand, cardiomyocyte apoptosis is known as an important contributory factor in hypertrophic remodeling and heart failure [19]. Apoptosis could be triggered by mitophagy impairment, reactive oxygen species (ROS) production, and an imbalance between Bcl-2-associated X-protein (Bax) and B cell lymphoma-2 (Bcl-2), the key regulators of apoptosis [20]. The presence of hyperthyroidism leads to an imbalance in the pro-survival/pro-apoptotic equilibrium through the elevation of the Bax/Bcl2 ratio, signifying the activation of a mitochondrial apoptotic pathway [21]. Hence, the investigation of the apoptosis pathway activation in conjunction with mitophagy dysfunction is being studied as a potential mechanism in the development of cardiac hypertrophy and injury.
Vitamin D is a vital pro-steroid hormone that is engaged in a multitude of physiological and pathological processes [22]. Vitamin D receptor is expressed in normal and malignant thyroid tissue [23]. Low levels of Vitamin D are associated with autoimmune thyroid diseases. Impaired Vitamin D signaling has been shown to promote overgrowth of the thyroid gland [24, 25]. Bozcourt et al. showed that the serum level of Vitamin D in hyperthyroid patients was significantly lower than the control group, and the severity of Vitamin D deficiency was related to the duration of hyperthyroidism [26].
Recently, Vitamin D has been increasingly acknowledged as a key component in signaling pathways that govern the function of cardiomyocytes, and its deficiency has been extensively shown to be linked with the progression of various cardiovascular diseases, including cardiac hypertrophic remodeling, suggesting its crucial involvement in regulating heart function [27, 28]. The therapeutic effects of Vitamin D supplementation are classically attributed to its antioxidant properties. However, recent findings indicate that Vitamin D, by modulating mitochondrial function alongside the suppression of oxidative stress, is effective in improving cellular energy status and respiration [29]. Many studies have demonstrated the cardioprotective effect of Vitamin D in various experimental models, including aging-induced cardiac hypertrophy with D-galactose, ovarian-induced cardiac alterations, myocardial infarction, doxorubicin-induced cardiotoxicity, and hyperthyroid-induced cardiomyopathy in rats [30,31,32,33,34]. The present study aims to investigate the effect of Vitamin D supplementation on ameliorating cardiac hypertrophy caused by hyperthyroidism via modulating the regulatory pathways associated with mitophagy and apoptosis processes.
Materials and methods
Animals
The study was conducted on a group of fifteen adult male Wistar rats weighing ~ 250–300 g. The animals were obtained from the animal house of the Hamadan University of Medical Science and were placed in plastic cages (5 rats per cage) under controlled laboratory settings (25 °C ± 5 °C with 12/12-hour light/ dark cycles and air conditioning) with unrestricted access to standard rodent feed and water throughout the duration of the experiment. All experiments were carried out following the National Institutes of Health guidelines and approved by the Hamadan Animal Experiment Committee (Ethics Committee permission No. IR.UMSHA.REC.1402.008).
Experimental protocol
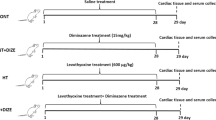
After being weighed, the animals were randomly assigned to three groups consisting of five rats as follows: control (CONT), hyperthyroid (HT) and hyperthyroid + Vitamin D (HT + VID). Hyperthyroidism was induced through the daily oral administration of 600 µg/kg of Levothyroxine (Iran Hormone Pharmaceutical Company) for a duration of 28 days [35]. The rats in the control group were solely given normal saline and the HT + VID group underwent simultaneous pretreatment with LT4 (600 µg/kg/day) and 400IU/kg/day of Vitamin D (OSVE pharmaceutical company, Iran) dissolved in olive oil by gavage for 28 days [36]. The weight of rats was monitored on a weekly basis to assess changes during the pretreatment period. After the pretreatment period had ended, following an overnight period of fasting, the rats were assessed for their weight and euthanized through the administration of intraperitoneal sodium pentobarbital (Sigma Chemical Company, Germany) injection (60 mg/kg) [37].
Specimens’ preparation
Once the rats were euthanized under deep anesthesia, blood samples (~ 5 mL per rat) were collected from the inferior vena cava. Subsequently after 30 min of clotting at ambient temperature, the samples were centrifuged at 3000 rpm for 15 min to separate the serum. The obtained serum was preserved at − 40 °C for subsequent assessments. The isolated heart was swiftly placed in liquid nitrogen and then stored at -80 °C. Heart tissue samples underwent homogenization in a PBS solution under ice cold conditions, after which the homogenates were centrifuged at 4000–6000 rpm for 10 min at 4 °C using a refrigerated centrifuge and the resultant supernatants were then stored at -80 °C.
Cardiac hypertrophy indices
The presence of cardiac hypertrophy was evaluated by applying the conventional established ratios, including the heart weight (g) to body weight (g) ratio (HW/BW), heart weight (g) to tibia length (cm) ratio (HW/TBL), and heart weight (g) to tail length (cm) ratio (HW/TAL) [38, 39].
Histological examination
The heart tissues were isolated from the animals and then fixed in 10% neutral buffered formalin for structural evaluation. The fixed tissues were sectioned (4 μm slices) and stained with hematoxylin and eosin (H&E). The samples were histologically analyzed through photomicroscope imaging. The size of cardiomyocytes were measured by Image J software.
Biochemical assays
Assessment of serum TSH and T4 levels
The diagnosis of hyperthyroidism induction was conducted by measuring the serum levels of thyroid-stimulating hormone (TSH) and thyroxine (T4). The values additionally demonstrate the pretreatment results regarding alterations in thyroid hormone levels. The serum levels of T4 were detected using the VIDAS kit (France) via the enzyme-linked fluorescent immunoassay (ELFA) method and the estimation of TSH concentration in serum samples was performed using an enzyme-linked immunosorbent assay (ELISA) kit from Zell Bio (Germany). Following the completion of the preparation steps in accordance with the kit’s instructions, the concentrations were calculated by measuring the optical absorbance at the wavelength of 420 nm and 450 nm, respectively.
Measurement of lipid peroxidation
Lipid peroxidation refers to the free-radical-mediated oxidative degradation of polyunsaturated fatty acids and malondialdehyde (MDA) as a byproduct of this process is commonly used as a reliable marker to measure the state of lipid peroxidation as well as oxidative stress [40]. The measurement of MDA concentration in the heart tissue was carried out using the ELISA kit provided by Zell Bio GmbH (Germany) which relies on a colorimetric approach and the interaction between MDA and Thiobarbituric acid (TBA) at elevated temperatures. Upon following the manufacturer’s protocol, the prepared mixture was subjected to centrifugation at 3000–4000 rpm for 10 min. The final values were derived by measuring the optical density of the resultant pink-colored supernatant at a wavelength of 535 nm and its compliance with the standard OD curve with µM units.
Measurement of myocardial damage markers
The levels of serum lactate dehydrogenase (LDH) and creatine kinase myocardial band (CKMB) were measured as enzymatic biomarkers for diagnosing myocardial damage. The estimation was carried out using commercial kits obtained from Pars Azmun (Iran) based on the photometric method by measuring the optical density of the mixture prepared according to the kit’s instructions at 340 nm in consecutive minutes and calculating the final values with the provided formula.
Quantitative real-time PCR-based gene expression analysis
The evaluation of mRNA expression levels for the examined genes was conducted using the Sina Cyber Blue NO ROX HS-qPCR (*2)100T.1 ml-MM2171 kit. RNA was extracted from the heart tissues using RNXTM-PLUS by following the manufacturer’s procedure. Gene-specific primer sequences employed in the reverse transcription process for RNA to cDNA conversion were determined based on published sequences from relevant studies (Table 1). Quantification of obtained results was performed using the comparative threshold cycle (CT) method with beta-actin as the housekeeping gene for normalization.
Statistical analyses
Data analysis was conducted using SPSS 16.0 software, and values were expressed as a mean ± standard error of the mean (SEM). One way ANOVA (analysis of variance) was applied to determine statistical differences among the experimental groups, followed by the least-significant difference (LSD) post-hoc test. Statistical significance was attributed to differences at a significance level of p < 0.05.
Results
Validation of experimental induction of hyperthyroidism
Hyperthyroid status in the experimental model groups was confirmed through the measurement of TSH and T4 serum concentrations. In Consistence with successful modeling, our results demonstrated that the serum TSH level was significantly decreased in the HT group compared to the control group (3.8 ± 0.08mIU/mL vs. 5.3 ± 0.05mIU/mL, P < 0.001) and the serum T4 level of the HT group was significantly increased in comparison with the control group (4.06 ± 0.25 µg/dL vs. 1.62 ± 0.79 µg/dL, P < 0.001) (Fig. 1).
TSH (A) and T4 (B) levels in animals groups. Data have been expressed as mean ± SEM in CONT; control, HT; hyperthyroid, HT + VD; hyperthyroid plus Vitamin D, TSH; Thyroid stimulating hormone, T4; Thyroxine. n = 5, ### p < 0.001 compared with control group, ** p < 0.001, *** p < 0.001 compared to the HT group
Body weight and cardiac hypertrophy indices
Throughout the four-week pretreatment period, there were no significant changes in the total body weight between the experimental groups. The HT group displayed a significant increment in all three indices of cardiac hypertrophy HW/BW, HW/TBL, and HW/TAL ratios in comparison with the CONT group respectively, which verify the successful modeling of cardiac hypertrophy induced by hyperthyroidism in the corresponding groups. There was a significant decrease observed in the values of both the HW/BW, HW/TBL and HW/TAL ratios in the group receiving both thyroxine and Vitamin D supplementation, as compared to the HT group respectively (Table 2).
Effect of vitamin D on cardiac histology
The tissue sections prepared from the control group (A) show the morphology of cardiomyocytes with oval and bright central nuclei in normal physiologic conditions. Examination of different fields of samples from the HT group (B) indicates an irregularity in the arrangement of cardiomyocytes, an increase in the intracellular distance, and also importantly the cardiac hypertrophy in HT group. However, the administration of Vitamin D into the hyperthyroid rats (C) was able to reduce the irregularity of myofibers, and other pathological conditions related Levothyroxine -induced hyperthyroidism (Fig. 2). Moreover, the size of cardiomyocytes were significantly (P < 0.001) increased in the hyperthyroid animals compared to the control animals. Also, Vitamin D treatment significantly (P < 0.001) improved the size of cardiomyocytes in the HT + VD rats versus the HT rats (Fig. 3).
Quantization of cardiomyocyte size. The findings have been presented as mean ± SEM in in CONT; control, HT; hyperthyroid, HT + VD; hyperthyroid plus Vitamin D. For each animal (n = 3 per group), a total of three slices were analyzed. ### p < 0.001 compared with control group, *** p < 0.001 compared to the D-GAL group
Effect of vitamin D on the serum concentrations of T4 and TSH
The simultaneous administration of LT4 and Vitamin D in the HT + VD group resulted in a significant elevation in TSH serum levels compared to the HT group. In contrast, rats in the HT + VD group exhibited a significant decrease in the serum level of T4 in comparison to the HT group of rats. Accordingly, these findings suggest that Vitamin D supplementation is efficient in improving alterations in TSH and T4 concentrations brought about by prolonged exposure to elevated thyroid hormone levels (Fig. 1).
Effect of vitamin D on cardiac MDA levels
The HT group animals demonstrated a significant elevation of cardiac MDA levels compared to the control group. Pretreatment with Vitamin D significantly reduced the cardiac MDA levels compared to the HT group. Indeed, the administration of Vitamin D brought the cardiac MDA concentration back to normal levels, as observed in the control group (Fig. 4).
Effect of vitamin D on cardiac damage markers
The results of the serum LDH and CK-MB concentration analysis showed that the values of these biomarkers in the HT group were more two times higher than the CONT group, and both of these serum level changes were significantly reversed by Vitamin D pretreatment (Table 3).
Expression profile of mitophagy-related genes in heart tissue
RT-qPCR analysis of Cardiac tissue from the HT group rats displayed a significant downregulation of all three aforementioned mitophagy related genes including PINK1, MFN2, and DRP1 compared to the CONT group respectively. Hyperthyroid rats treated with Vitamin D exhibited a significant up-regulation in the cardiac expression levels of PINK1, MFN2, and DRP1 compared to the HT group. The results signify the effectiveness of Vitamin D supplementation on the modulation of hyperthyroidism-driven changes in mitophagy-related gene expression(Table 4).
Effect of vitamin D on the expression of mitochondrial dependent apoptosis related genes
The cardiac expression level of key mitochondria-dependent apoptosis regulators, Bax and Bcl-2 was measured to evaluate the apoptosis status of the experimental groups. Analysis of real-time PCR data revealed a significant increase in cardiac Bax levels and, in contrast, a significant decrease in cardiac Bcl-2 levels in the hyperthyroid group compared to the control group. Vitamin D administration in hyperthyroid rats significantly reversed Bcl-2 downregulation, while the expression of Bax remained relatively unchanged compared to the control group. (Whereas the expression of Bax did not exhibit significant changes when compared to the control group) (Table 4).
Discussion
Heart disease caused by hyperthyroidism is a serious complication associated with hyperthyroidism. The use of cardioprotective drugs can be useful for patients with hyperthyroidism. The aim of the present study was to validate the effectiveness of Vitamin D as a therapeutic option for the pretreatment of cardiac hypertrophy induced by hyperthyroidism, with a focus on mitochondria-related mechanisms, including the contribution of mitophagy and apoptosis, as possible molecular mechanisms that underlie the progression of this pathogenesis. In this study, the confirmation of the induction of hyperthyroidism in rats was shown by a significant increase in T4 and a significant decrease in TSH in rats with hyperthyroidism compared to the control group. Simultaneous consumption of Vitamin D led to a significant improvement in the thyroid profile of rats with hyperthyroidism. This content is in agreement with the results of Kaplan et al. [41]. , who confirmed the improvement of thyroid profile in Levothyroxine-induced hyperthyroidism in rats. Experimental studies have reported that Vitamin D has a direct role on Dio2, an enzyme essential for the conversion of T4 to T3 in target organs [42]. The effect of Vitamin D on the cultured thyroid cells of rats indicates the direct anti-thyroid effect of Vitamin D, which is consistent with the findings of the present study [43].
Hyperthyroidism induction in these animals was accompanied by a significant rise in cardiac hypertrophy indices, including the ratio of HW/BW, HW/TBL, and HW/TAL, demonstrating the evident presence of cardiac hypertrophy. Additionally, hyperthyroid rats exhibited a significant elevation in the serum levels of LDH and CK-MB, markers of myocardial damage, signifying the damage inflicted upon the cellular structure of cardiomyocytes. Moreover, Shokri et al. indicated cardiac hypertrophy and a significant increase in serum LDH and CK-MB in hyperthyroidism rat model indicating that hyperthyroidism resulted in with cardiac hypertrophy and cardiac damage [38]. All changes in these markers were effectively reversed following a four-week course of Vitamin D pretreatment, suggesting the comparative efficacy of Vitamin D therapy in ameliorating cardiac hypertrophy and myocardial damage induced by hyperthyroidism. This is consistent with a previous study that showed Vitamin D supplementation reduced cardiac marker enzymes in rats with doxorubicin-induced cardiotoxicity [30]. In addition, administration of Vitamin D significantly reduced the ratio of heart weight to body weight in a mouse model of aging-induced cardiac hypertrophy, which is consistent with our results [33].
The results of our study, consistent with recent findings, demonstrated a significant reduction in the cardiac expression levels of aforementioned components involved in the regulation of mitophagy process, i.e. PINK1, MFN2, and DRP1, in experimentally hyperthyroid rats compared to the control group [38]. Recent studies have demonstrated that the knockout or suppression of PINK1 results in abnormal functioning of cardiac mitochondria, heightened levels of oxidative stress, impaired left ventricular function, and pathological cardiac hypertrophy [14, 44]. Moreover, the decline in cardiac MFN2 expression, given its crucial role in maintaining quality control mechanisms, has been reported to be associated with impaired mitochondrial function, elevated production of ROS as well as the disruption of PINK1-dependent mitophagy activation [45]. Disruption of the mitochondrial fission mechanism due to repressed DRP1 expression has been found to be linked with mitochondrial dysfunction and perturbation of mitophagy, favoring cardiac dysfunction and the onset of cardiac hypertrophy [18, 46]. Pretreatment with Vitamin D significantly up-regulated the expression of all three of these genes. The findings not only support the involvement of Vitamin D signaling in modulating mitophagy but also highlight its possible potential in optimizing the regulatory pathways involved in this biological process. There is evidence that the improvement of cardiac function in individuals receiving Vitamin D pretreatment is partially attributed to the enhancement of mitochondrial function and density, which is reflected in an increase in ATP production capacity and overall energy homeostasis [47]. It has also been documented that Vitamin D receptor knockout is associated with increased ROS production following the disruption of mitochondrial integrity and normal functionality of respiratory chain, which highlights the importance of nuclear and mitochondrial transcription coordination for cell survival [48].
In the present study, oxidative stress in hyperthyroidism induced by Levothyroxine was shown by a significant increase of cardiac MDA in the hyperthyroid group compared to the control group. Hyperthyroidism causes lipid peroxidation in heart tissue. MDA is a reliable biomarker for investigating oxidative stress in various pathological conditions [49]. This increase in oxidative stress marker, was significantly revered by Vitamin D. Besides its antioxidant properties, it is postulated that this might be a result of normalizing the autophagy process and subsequently averting additional ROS production by defective mitochondria.
Experimental hyperthyroidism increases apoptosis in heart tissue [34]. This study indicated a significant upregulation of Bax expression and significant downregulation of Bcl-2 in cardiac tissue of hyperthyroid group rats. The resulting oxidative damage, gradually spreads to intact mitochondria and other intracellular organelles, giving rise to a vicious cycle called ROS-induced ROS. Ultimately, as a result of either direct damage caused by ROS or the increased permeability brought about by intracellular damage signals, mitochondrial apoptotic inducing factors are released, culminating in cell death [50]. Additionally, the regulation of mitochondrial-dependent apoptosis is primarily governed by the interplay between pro-apoptotic (Bax) and anti-apoptotic (Bcl-2) proteins from the Bcl-2 protein family. Upregulation of Bax is induced upon exposure to a range of detrimental events within or outside the cell, such as those seen in hyperthyroidism [20]. The group treated with Vitamin D did not exhibit any notable alterations in the expression of Bax. However, there was a significant enhancement in the expression of Bcl2, suggesting the partial effectiveness of this pretreatment in inhibiting apoptosis induced by hyperthyroidism. The anti-apoptotic role of Vitamin D was previously reported in experimental models of diabetic cardiomyopathy and myocardial infarction [51].
Cardiac changes were confirmed by histological study of heart in rats with hyperthyroidism. Light microscopic examination of the heart of hyperthyroid rats indicated irregularity of myofibers, and increased cardiomyocytes diameter. Administration of Vitamin D to animals with hyperthyroidism improved these alterations.
Conclusion
Collectively, the findings presented in this study provide evidence supporting the beneficial effects of Vitamin D in improving cardiac hypertrophy and ameliorating myocardial damage caused by hyperthyroidism. The results suggest that the potential mechanism implicated in the favorable impacts of Vitamin D in mitigating the progression of cardiac hypertrophy might be associated with its efficiency in counteracting the changes brought about by hyperthyroidism in the dysregulation of pathways governing mitophagy and mitochondrial-dependent apoptosis. Taken together, these findings not only support the effectiveness of Vitamin D therapy in improving cardiovascular events but also provide additional evidence in the growing body of Vitamin D therapeutic approaches, backing the therapeutic value of Vitamin D in addressing pathogenesis linked to mitochondrial dysfunction. Whether Vitamin D exerts protective effects on cardiac hypertrophy caused by hyperthyroidism through a direct effect on cardiac and mitochondrial function or whether secondary effects occur to improve hyperthyroidism and alter these pathways is not known. Therefore, more clinical and experimental research is needed in the future on Vitamin D and the role of hyperthyroidism.
Data availability
The data used and analyzed in this study are avail¬able from the Corresponding author on reasonable request.
Abbreviations
- ANOVA:
-
Analysis of variance
- ACTB:
-
Beta-actin
- Bax:
-
(Bcl-2)-associated X
- Bcl2:
-
B-cell lymphoma protein 2
- BW:
-
Body Weight
- CK-MB:
-
Creatine kinase
- CONT:
-
Control
- CT:
-
Threshold cycle
- Drp1:
-
Dynamin related protein 1
- ELISA:
-
Enzyme-linked immunosorbent assay
- HT:
-
Hyperthyroid
- HW:
-
Heart Weight
- LDH:
-
Lactate dehydrogenase
- LSD:
-
Least-significant difference
- MDA:
-
Malondialdehyde
- Mfn2:
-
Mitofusin-2
- MQC:
-
Mitochondrial quality control
- OMM:
-
Outer mitochondrial membrane
- PINK:
-
PTEN induced putative kinase 1
- qRT-PCR:
-
Quantitative Real-Time Polymerase chain reaction
- ROS:
-
Reactive oxygen species
- SEM:
-
Standard error of the mean
- TAL:
-
Tail length
- TBA:
-
Thiobarbituric acid
- TBL:
-
Tibia length
- T4:
-
Thyroxine
- TSH:
-
Thyroid-stimulating hormone
References
Kanda V, Sathyamurthy P, Narayanan L (2016) Cardiovascular manifestations in hyperthyroidism. Int j res med sci 4(7):3032. https://doi.org/10.18203/2320-6012.ijrms20161992
Sheng CX, Zhang CJ, Li YZ, Sun YM (2020) Effect of β-casomorphin-7 on myocardial hypertrophy in hyperthyroidism-induced cardiomyopathy. Eur Rev Med Pharmacol Sci 24(11):6380–6389. https://doi.org/10.26355/eurrev_202006_21536
Ojamaa K (2010) Signaling mechanisms in thyroid hormone-induced cardiac hypertrophy. Vascul Pharmacol 52(3–4):113–119. https://doi.org/10.1016/j.vph.2009.11.008
Khamis T, Alsemeh AE, Abdullah DM (2022) Sacubitril/valsartan (LCZ696) ameliorates hyperthyroid-induced cardiac hypertrophy in male rats through modulation of miR-377, let-7 b, autophagy, and fibrotic signaling pathways. Sci Rep 12(1):1–13. https://doi.org/10.1038/s41598-022-18860-y
Venediktova N, Solomadin I, Nikiforova A, Starinets V, Mironova G (2021) Functional state of Rat Heart Mitochondria in experimental hyperthyroidism. Int J Mol Sci 22(21):11744. https://doi.org/10.3390/ijms222111744
Yang D, Liu HQ, Liu FY, Guo Z, An P, Wang MY et al (2022) Mitochondria in pathological cardiac hypertrophy research and therapy. Front Cardiovasc Med 8:2190. https://doi.org/10.3389/fcvm.2021.822969
Moyzis AG, Sadoshima J, Gustafsson ÅB (2015) Mending a broken heart: the role of mitophagy in cardioprotection. Am J Physiol Heart Circ Physiol 308(3):183–192. https://doi.org/10.1152/ajpheart.00708
Abel ED, Doenst T (2011) Mitochondrial adaptations to physiological vs. pathological cardiac hypertrophy. Cardiovasc Res 90(2):234–242. https://doi.org/10.1093/cvr/cvr015
Suliman HB, Piantadosi CA (2016) Mitochondrial quality control as a therapeutic target. Pharmacol Rev 68(1):20–48. https://doi.org/10.1124/pr.115.011502
Venediktova N, Solomadin I, Starinets V (2023) Effect of Thyroxine on the structural and dynamic features of Cardiac Mitochondria and Mitophagy in rats. Cells 12(3):396. https://doi.org/10.3390/cells12030396
Forte M, D’Ambrosio L, Schiattarella GG, Salerno N, Perrone MA, Loffredo FS, Bertero E, Pilichou K, Manno G, Valenti V, Spadafora L, Bernardi M, Simeone B, Sarto G, Frati G, Perrino C, Sciarretta S, Italian Society of Cardiology Working Group on Cellular and Molecular Biology of the Heart (2024) Mitophagy modulation for the treatment of cardiovascular diseases. Eur J Clin Invest 54(8):e14199. https://doi.org/10.1111/eci.14199Epub 2024 Mar 26. PMID: 38530070
Morales PE, Arias-Durán C, Ávalos-Guajardo Y, Aedo G, Verdejo HE, Parra V et al (2020) Emerging role of mitophagy in cardiovascular physiology and pathology. Mol Aspects Med 71:100822. https://doi.org/10.1016/j.mam.2019.09.006
Dorn GW (2019) Evolving concepts of mitochondrial dynamics. Annu Rev Physiol 81:1–17. https://doi.org/10.1146/annurev-physiol-020518-114358
Billia F, Hauck L, Konecny F, Rao V, Shen J, Mak TW (2011) PTEN-inducible kinase 1 (PINK1)/Park6 is indispensable for normal heart function. Proc Natl Acad Sci 108(23):9572–9577. https://doi.org/10.1073/pnas.1106291108
Chen Y, Dorn GW (2013) PINK1-phosphorylated mitofusin 2 is a parkin receptor for culling damaged mitochondria. Science 340(6131):471–475. https://doi.org/10.1126/science
Tong T, Zablocki M, Sadoshima D J (2020) The role of Drp1 in mitophagy and cell death in the heart. J Mol Cell Cardiol 142:138–145. https://doi.org/10.1016/j.yjmcc.2020.04.015
Jin JY, Wei XX, Zhi XL, Wang XH, Meng D (2021) Drp1-dependent mitochondrial fission in cardiovascular disease. Acta Pharmacol Sin 42(5):655–664. https://doi.org/10.1038/s41401-020-00518-y
Ikeda Y, Shirakabe A, Maejima Y, Zhai P, Sciarretta S, Toli J et al (2015) Endogenous Drp1 mediates mitochondrial autophagy and protects the heart against energy stress. Circ Res 116(2):264–278. https://doi.org/10.1161/CIRCRESAHA.116.303356
Wollert KC, Drexler H (2002) Regulation of cardiac remodeling by nitric oxide: focus on cardiac myocyte hypertrophy and apoptosis. Heart Fail Rev 7(4):317–325. https://doi.org/10.1023/a:1020706316429
Hardwick JM, Soane L (2013) Multiple functions of BCL-2 family proteins. Cold Spring Harb Perspect Biol 5(2):a008722. https://doi.org/10.1101/cshperspect.a008722
Fernandes RO, Dreher GJ, Schenkel PC, Fernandes TR, Ribeiro MF, Araujo AS et al (2011) Redox status and pro-survival/pro‐apoptotic protein expression in the early cardiac hypertrophy induced by experimental hyperthyroidism. Cell Biochem Funct 29(7):617–623. https://doi.org/10.1002/cbf.1796
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357(3):266–281. https://doi.org/10.1056/NEJMra070553
Clinckspoor I, Verlinden L, Mathieu C, Bouillon R, Verstuyf A, Decallonne B (2013) Vitamin D in thyroid tumorigenesis and development. Prog Histochem Cytochem 48(2):65–98. https://doi.org/10.1016/j.proghi.2013.07.001
Muscogiuri G, Tirabassi G, Bizzaro G, Orio F, Paschou SA, Vryonidou A, Balercia G, Shoenfeld Y, Colao A (2015) Vitamin D and thyroid disease: to D or not to D? Eur J Clin Nutr 69(3):291–296. https://doi.org/10.1038/ejcn.2014.265
Kmieć P, Sworczak K (2015) Vitamin D in thyroid disorders. Exp Clin Endocrinol Diabetes 123(7):386–393. https://doi.org/10.1055/s-0035-1554714
Bozkurt NC, Karbek B, Ucan B, Sahin M, Cakal E, Ozbek M, Delibasi T (2013) The association between severity of vitamin D deficiency and Hashimoto’s thyroiditis. Endocr Pract 19(3):479–484. https://doi.org/10.4158/EP12376.OR
Bae S, Singh SS, Yu H, Lee JY, Cho BR, Kang PM (2013) Vitamin D signaling pathway plays an important role in the development of heart failure after myocardial infarction. J Appl Physiol 114(8):979–987. https://doi.org/10.1152/japplphysiol.01506.2012
Condoleo V, Pelaia C, Armentaro G, Severini G, Clausi E, Cassano V et al (2021) Role of vitamin D in cardiovascular diseases. Endocr 2(4):417–426. https://doi.org/10.3390/endocrines2040037
Reddy AM, Iqbal M, Chopra H, Urmi S, Junapudi S, Bibi S et al (2022) Pivotal role of vitamin D in mitochondrial health, cardiac function, and human reproduction. EXCLI J 21:967–990. https://doi.org/10.17179/excli2022-4935
Aygun H, Gul SS (2019) Cardioprotective effect of melatonin and agomelatine on doxorubicin-induced cardiotoxicity in a rat model: an electrocardiographic, scintigraphic and biochemical study. Bratisl Lek Listy 120(4):249–255. https://doi.org/10.4149/BLL_2019_045
El Agaty SM (2019) Cardioprotective effect of vitamin D2 on isoproterenol-induced myocardial infarction in diabetic rats. Arch Physiol Biochem 125(3):210–219. https://doi.org/10.1080/13813455.2018.1448423
Mohammed NA, El-Malkey NF, Ibrahim AA, Abdullah DM (2019) Vitamin D3 supplementation ameliorates ovariectomy-induced cardiac apoptotic and structural changes in adult albino rats. Can J Physiol Pharmacol 97(7):647–654. https://doi.org/10.1139/cjpp-2018-0674
Shahidi S, Ramezani-Aliakbari K, Komaki A, Salehi I, Hashemi S, Asl SS, Habibi P, Ramezani-Aliakbari F (2023) Effect of vitamin D on cardiac hypertrophy in D-galactose-induced aging model through cardiac mitophagy. Mol Biol Rep 50(12):10147–10155. https://doi.org/10.1007/s11033-023-08875-7
Salem HR, Hegazy GA, Abdallah R, Abo-Elsoud RA (2023) Protective role of vitamin D3 in a rat model of hyperthyroid-induced cardiomyopathy. J Tradit Complement Med 13(3):277–284. https://doi.org/10.1016/j.jtcme.2023.02.007
Hashem H, Saad S (2020) Comparative study of the effect of experimentally induced hyperthyroidism and hypothyroidism on the parotid gland in adult male albino rats. EJH 43(3):791–807. https://doi.org/10.21608/ejh.2019.17411.1174
Jeremy M, Gurusubramanian G, Roy VK (2019) Vitamin D3 regulates apoptosis and proliferation in the testis of D-galactose-induced aged rat model. Sci Rep 9(1):14103. https://doi.org/10.1038/s41598-019-50679-y
Shackebaei D, Hesari M, Ramezani-Aliakbari S, Hoseinkhani Z, Ramezani-Aliakbari F (2022) Gallic acid protects against isoproterenol-induced cardiotoxicity in rats. Hum Exp Toxicol 41:09603271211064532. https://doi.org/10.1177/09603271211064532
Shokri F, Zarei M, Komaki A, Raoufi S, Ramezani-Aliakbari F (2024) Effect of diminazene on cardiac hypertrophy through mitophagy in rat models with hyperthyroidism induced by levothyroxine. Naunyn Schmiedebergs Arch Pharmacol 397(2):1151–1162. https://doi.org/10.1007/s00210-023-02680-6
Ryu Y, Jin L, Kee HJ, Piao ZH, Cho JY, Kim GR, Choi SY, Lin MQ, Jeong MH (2016) Gallic acid prevents isoproterenol-induced cardiac hypertrophy and fibrosis through regulation of JNK2 signaling and Smad3 binding activity. Sci Rep 6:34790. https://doi.org/10.1038/srep34790
Grotto D, Maria LS, Valentini J, Paniz C, Schmitt G, Garcia SC et al (2009) Importance of the lipid peroxidation biomarkers and methodological aspects for malondialdehyde quantification. Quim Nova 32:169–174. https://doi.org/10.1590/S0100-40422009000100032
Kaplan S, Türk A, Aydın H, Erten M, Kırıcı P (2021) Vitamin D improves oxidative stress and histopathological damage in rat ovaries caused by hyperthyroidism. J Obstet Gynaecol Res 47(10):3551–3560. https://doi.org/10.1111/jog.14948
Alrefaie Z, Awad H (2015) Effect of vitamin D3 on thyroid function and de-iodinase 2 expression in diabetic rats. Arch Physiol Biochem 121(5):206–209. https://doi.org/10.3109/13813455.2015.1107101
Berg JP, Sandvik JA, Ree AH, Sørnes G, Bjøro T, Torjesen PA, Gordeladze JO, Haug E (1994) 1,25-Dihydroxyvitamin D3 attenuates adenylyl cyclase activity in rat thyroid cells: reduction of thyrotropin receptor number and increase in guanine nucleotide-binding protein Gi-2 alpha. Endocrinology 135(2):595–602. https://doi.org/10.1210/endo.135.2.8033808
Abudureyimu M, Yu W, Cao RY, Zhang Y, Liu H, Zheng H (2020) Berberine promotes cardiac function by upregulating PINK1/Parkin-Mediated Mitophagy in Heart failure. Front Physiol 25:11:565751. https://doi.org/10.3389/fphys.2020.565751
Song M, Dorn GW 2nd (2015) Mitoconfusion: noncanonical functioning of dynamism factors in static mitochondria of the heart. Cell Metab 21(2):195–205. https://doi.org/10.1016/j.cmet.2014.12.019
Song M, Mihara K, Chen Y, Scorrano L, Dorn GW 2nd (2015) Mitochondrial fission and fusion factors reciprocally orchestrate mitophagic culling in mouse hearts and cultured fibroblasts. Cell Metab 21(2):273–286. https://doi.org/10.1016/j.cmet.2014.12.011
Hussien NI, El-Wakeel HS, Souror SM, Ahmed IA (2019) Alleviation of cardiac mitochondrial dysfunction and oxidative stress underlies the protective effect of vitamin D in chronic stress-induced cardiac dysfunction in rats. Gen Physiol Biophys 38(1):51–61. https://doi.org/10.4149/gpb_2018036
Ricca C, Aillon A, Bergandi L, Alotto D, Castagnoli C, Silvagno F (2018) Vitamin D receptor is necessary for mitochondrial function and cell health. Int J Mol Sci 19(6):1672. https://doi.org/10.3390/ijms19061672
Mogulkoc R, Baltaci AK, Oztekin E, Sivrikaya A, Aydin L (2006) Effects of hyperthyroidism induced by L-thyroxin administration on lipid peroxidation in various rat tissues. Acta Biol Hung 57(2):157–163. https://doi.org/10.1556/ABiol.57.2006.2.3
Zorov DB, Juhaszova M, Sollott SJ (2014) Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release. Physiol Rev 94(3):909–950. https://doi.org/10.1152/physrev.00026.2013
Guler G, Dasdelen D, Baltaci SB, Sivrikaya A, Baltaci AK, Mogulkoc R (2021) The effects of thyroid dysfunction on DNA damage and apoptosis in liver and heart tissues of rats. Horm Mol Biol Clin Investig 43(1):47–53. https://doi.org/10.1515/hmbci-2021-0059
Acknowledgements
The authors would like to thank the Hamadan University of Medical Sciences for funding.
Funding
The study was funded by Vice-chancellor for Research and Technology, Hamadan University of Medical Sciences (No. 140207045341).
Author information
Authors and Affiliations
Contributions
FSh: Investigation, Supervision, Project admin¬istration. KhR-A: Investigation, Supervision, Project admin¬istration. MZ: Conceptualization, Formal analysis, Writing - Review & Editing. AK: Formal analysis, Writing - Review & Editing. SR: Inves¬tigation. HN: Writing - Review & Editing. FRA: Conceptualization, Formal analysis, Investigation, Writing - Original Draft, Funding ac¬quisition. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was granted by the Ethics Committee of Hamadan University of Medical Sciences (Ethics Committee permission No. IR.UMSHA.REC.1400.008).
Consent for publication
None.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shokri, F., Ramezani-Aliakbari, K., Zarei, M. et al. Cardioprotective effect of Vitamin D on cardiac hypertrophy through improvement of mitophagy and apoptosis in an experimental rat model of levothyroxine -induced hyperthyroidism. Mol Biol Rep 51, 969 (2024). https://doi.org/10.1007/s11033-024-09897-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11033-024-09897-5