Abstract
Background
Hepatitis B virus (HBV) infection is a severe global health problem, and there has been no effective method to eliminate HBV. This study was designed to explore the pharmacological mechanism of Dihydromyricetin (DHM) treatment on HBV replication in vitro.
Methods and Results
DHM is a flavonoid compound from Ampelopsis grossedentata. Using HepG2.2.15 cells, which can stably express HBV in vitro, we demonstrated that DHM treatment dramatically reduced HBV replication and secretions of HBsAg and HBeAg. Meanwhile, DHM inhibited mRNA expression of HBV RNAs in HepG2.2.15 cells, including Total HBV RNA, HBV pregenomic RNA (pgRNA), and HBV precore mRNA (pcRNA). Also, DHM elevated the mRNA expressions of inflammatory cytokines and antiviral effectors. In contrast, DHM decreased the mRNA level of HNF4α, which positively correlated with HBV replication. Further studies show that the activation of nuclear factor-kappa B (NF-κB) and mitogen-activated protein kinase (MAPK) signaling pathway played a critical role in DHM-initiated inhibition of HBV replication in HepG2.2.15 cells. Besides, activated autophagy was another contributor that may accelerate the clearance of HBV components.
Conclusion
In summary, DHM could suppress HBV replication by activating NF-κB, MAPKs, and autophagy in HepG2.2.15 cells. Our studies shed light on the future application of DHM for the clinical treatment of HBV infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis B virus (HBV) infection is a severe global health problem. According to the World Health Organization (WHO), approximately two billion people worldwide have been infected with HBV, and more than 350 million are suffering from chronic HBV infection [1]. Infections caused by HBV are responsible for a substantial proportion of liver diseases globally, including liver fibrosis, cirrhosis, liver failure, and hepatocellular carcinoma. And this results in nearly one million deaths annually [2].
HBV is a small double-stranded DNA virus belonging to the Hepadnaviridae family. Upon infection, the double-stranded relaxed circular DNA (rcDNA) bound with the viral polymerase is released from the capsid, enters the nucleoplasm, and then converts into a covalently closed circular DNA (cccDNA) in the nucleus [3]. The persistence of cccDNA in the nuclei of infected hepatocytes leads to persistent HBV infection. Currently, there has been no effective method to eliminate HBV from patients [4].
Antiviral drugs and immunomodulatory agents are the current major treatments for patients with chronic HBV infection [1]. As the main antiviral drugs, nucleotide Analogs (NAs) can inhibit viral replication by targeting the DNA polymerase of HBV, such as adefovir, lamivudine, and entecavir. However, long-term administration of these drugs usually leads to serious side effects [5]. Although HBV infection has no direct toxic effect on the target cells, the suppression of immune responses in HBV infection is considered a significant cause of liver diseases[6]. The immunomodulatory agents seem to be another HBV infection treatment drug like interferon (IFN). IFN has been widely applied to clinical immunotherapy to activate host immune repressed by HBV. It was reported that IFN could reduce the expressions of HBsAg and HBeAg in the liver[7]. And IFN treatment displayed an inhibitory effect on the activation of HBV promoter [8]. However, the therapeutic effect of IFN is limited and only effective for a few people. Long-term use of IFN will also produce adverse reactions like a liver failure[9]. So far, it has still been urgent to search for new antiviral drugs for HBV treatment.
Dihydromyricetin (DHM), also known as ampelopsis, is a natural flavonol compound isolated from Ampelopsis grossedentata (Hand-Mazz.) plants. In previous studies, DHM had a variety of pharmacological activities, including anti-inflammation [10], anti-oxidation [11], cardioprotective effect [12], neuroprotection [13], and anti-tumor [14]. Noticeably, DHM was revealed to possess liver-protective properties against acute liver injury, fatty liver, liver regeneration, and hepatocyte deterioration [11, 13]. Further, a recent study reported that DHM obliterated the proliferation of Herpes simplex virus 1 (HSV-1) in a toll-like receptor 9 (TLR9)-dependent manner [14]. TLR agonists are known for their promotive effects on immune system activation in HBV-infected cells, indicative of the viral clearance in HBV-specific immune responses [15]. For example, the oral administration of Vesatolimod (GS-9620), a TLR7 agonist, resulted in the suppression of HBV-DNA synthesis, loss of HBsAg, and a reduced occurrence rate of hepatocellular carcinoma (HCC) [16]. Nevertheless, no evidence illustrated whether DHM could block HBV replication of hepatocytes in a viral-special immune response mediated by TLRs.
In this study, we aim to investigate the repression of DHM on HBV infection in hepatocytes. Using HepG2.2.15 cells, a cellular model that can stably express HBV in vitro, we explored the regulatory effect of DHM on HBV replication, pro-inflammatory cytokine activation, and antiviral gene expression. To reveal the potential molecular mechanism, we detected the changes of TLRs and their downstream signals, such as nuclear factor-kappa B (NF-κB), mitogen-activated protein kinase (MAPK) pathway in HepG2.2.15 cells with DHM treatment. Further, we studied the role of autophagy activation in DHM-initiated anti-HBV reaction in hepatocytes.
Materials and methods
Reagents
DHM, with a purity of 98%, was purchased from Yuanye Bio-Technology Co., Ltd (Shanghai, China). Dulbecco’s Modified Eagle’s Medium-F12 (DMEM/F12), G418, Penicillin, Streptomycin, and fetal bovine serum (FBS) were obtained from Gibco (Grand Island, NY, USA), and 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) was purchased from Amresco (Solon, Ohio, USA). Nuclear and Cytoplasmic Protein Extraction Kit was supplied by Beyotime Biotechnology (Shanghai, China). Antibodies against TLR4 (sc-293,072), p-ERK1/2 (sc-7383), ERK1/2 (sc-514,302), p-p38 (sc-166,182), p38 (sc-7972), and Actin (sc-81,178) were bought from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Antibodies against p-JNK (#9251), JNK (#9252), p-PI3K (#4228), PI3K (#4228), p-Akt (Ser 473) (#5315), Akt (#9272), p-NF-κB/p65(#3033), NF-κB/p65(#4764), p-IKKα/β (#2697), IKKα/β (#8943), IκBα (#4812), SQSTM1/p62 (#5114), LC3B (#2775), Beclin-1 (#3738), and mTOR (#2983) were obtained from Cell Signaling Technologies (Beverly, MA, USA). ECL (Enhanced chemiluminescence) detection kit was purchased from Summer Biotechnology Co., Ltd (Beijing, China). All the other chemicals used were of analytical grade unless otherwise stated.
Cell Culture
HepG2 and HepG2.2.15 cells were obtained from China Center for Type Culture Collection in Wuhan. All used cell lines were cultured in a humidified atmosphere containing 95% air and 5% CO2 at 37 °C. The HBV-producing HepG2.2.15 hepatoma cell line, containing the integrated HBV genomic dimers, was routinely cultured in the DMEM/F12 media. The medium was supplemented with 10% FBS, penicillin (100 U/mL), streptomycin (100 U/mL), and G418 (400 µg/mL). HepG2 cells were cultured with the same treatment as HepG2.2.15 cells apart from the addition of G418 (400 µg/mL).
Cell viability
HepG2.2.15 cells were seeded in a 96-well plate at 37 °C after the cell density reached 70%. Then, the culture medium was removed and substituted with a fresh medium containing different concentrations of DHM (30, 60, 90, and 120 µM) for 24 h. Next, the medium was removed, and 100 µL of MTT (1 mg/mL) was added to each well. After the incubation for an additional 4 h, the medium was removed. The formazan crystals formed in cells were dissolved with 100 µL of dimethylsulfoxide (DMSO) (Solarbio science & technology co., ltd, Beijing, China). Subsequently, the cytotoxicity was determined by analyzing MTT absorbance at 490 nm.
For the cytotoxicity analysis of Lamivudine (3-TC) on HepG2.2.15 cells, we prepared the 3-TC solution by dissolving it in water. After the filtration through a 0.45 μm filter, different concentrations of 3-TC (12.5, 25, 50, and 100 µg/mL) were added to the culture medium, and the cells were incubated for 24 h. Then, we performed the MTT analysis as before.
Measurement of HBV antigens
The HBsAg and HBeAg kits (Shanghai Kehua Bio-Engineering Co., Ltd.) were used to detect the levels of secreted HBsAg and HBeAg viral proteins in the medium. Briefly, HepG2.2.15 cells were seeded in a 24-well plate and incubated overnight. Then, the culture medium was replaced with different concentrations of DHM (30, 60, and 120 µM) or 3-TC (50 µg/mL). The medium was harvested at 6 h, 12 h, and 24 h, respectively. After the centrifugation to remove cell debris, the supernatant was collected for the detection of secreted HBsAg and HBeAg. The experiment was performed using an enzyme-linked immunosorbent assay (ELISA) according to the manufacturer’s instructions.
RNA extraction and quantitative RT-PCR (qRT-PCR)
Total RNA of HepG2 Cells or HepG2.2.15 Cells was extracted using Trizol reagent (Summer Biotechnology Co., Ltd, Beijing, China). And 1 µg of RNA was reversely transcribed to cDNA with a first-strand cDNA synthesis kit according to the manufacturer’s protocol (Summer Biotechnology Co., Ltd, Beijing, China). The mRNA levels of target genes were measured by qRT-PCR using a SYBR QPCR mixture (Summer Biotechnology Co., Ltd, Beijing, China) at the CFX Connect Real-time system (Bio-Rad, Hercules, CA, USA). The primers for qRT-PCR were detailed in Supplementary Table 1. The thermal cycle condition was as follows: pre-denaturation at 94 °C for 10 min; 40 cycles of denaturation at 95 °C for 15 s, annealing/extension at 60 °C for 60 s. After that, we normalized the expression levels of target genes against that of β-actin. The fold changes were calculated using a 2−ΔΔCT method.
Detection of HBV-DNA expression
After the DHM treatment, the medium was collected to determine HBV-DNA level using a Hepatitis B Virus Nucleic Acid Quantitative Detection Kit according to the manufacturer’s instructions (KHB, Shanghai, China). In brief, HepG2.2.15 Cells were seeded in a six-well plate. After the cell density reached 80%, cells were treated with different concentrations of DHM (30, 60, and 120 µM) or 3-TC (50 µg/mL) for 24 h. After the treatment, the medium was collected and centrifuged at 13,000× g for 2 min. Next, 100 µL of the supernatant was mixed with 100 µL of sample treatment solution A (mainly containing NaCl). The mixture was centrifuged at 13,000× g for 10 min, and the supernatant was discarded, followed by adding 25 µL of sample treatment Solution B (mainly containing Tris, NP40). After the shaking for seconds with subsequent incubation at 100 °C for 10 min, the mixture was centrifuged as before. And 2 µL of the supernatant was used as a reaction template for RT-PCR analysis.
Western blot analysis
The cell lysate was prepared using IP lysis buffer (Beyotime Biotechnology, Shanghai, China) supplemented with a protease inhibitor cocktail (Merck, Darmstadt, Germany). The concentration of sample lysate was determined using a bicinchoninic acid (BCA) protein assay kit (Beyotime Biotechnology, Shanghai, China). After the boiling with loading buffer, samples were separated by 10−15% SDS-PAGE. And the proteins were transferred onto polyvinylidene difluoride membranes (PVDF) (Millipore, Billerica, MA, USA). Then, the membranes were blocked with 5% non-fat milk in Tris-buffered saline Tween-20 (TBST) for 1 h. After the washing with TBST, membranes were incubated with primary antibodies at 4 °C overnight. Next, After the washing, membranes were incubated with horseradish peroxidase (HRP)-conjugated secondary antibodies (Cell Signaling Technology, MA, USA) for 1 h at room temperature. Finally, we visualized the protein signals with ECL (Sigma Aldrich, MO, USA), and the relative band intensity was quantified using software Image J (NIH, Bethesda, MD, USA).
Immunofluorescence staining
HepG2.2.15 cells seeded on sterile coverslips were treated with different concentrations of DHM (30, 60, and 120 µM) for 12 h. Then, cells were fixed with 4% paraformaldehyde in PBS for 20 min, washed three times with PBS, and permeabilized with PBS containing 0.5% Triton X-100 for 20 min. Next, cells were washed and blocked with PBS containing 1% BSA for 30 min, followed by the incubation with anti-Flag overnight at 4 °C. After the washing with PBS, cells were incubated with secondary Fluor488-conjugated Goat anti-IgG (H + R) (Summer Biotechnology Co., Ltd, Beijing, China) for 1 h. And DAPI was used for the nucleus staining. Finally, the immunofluorescence images were photographed and analyzed using a Nikon Intensilight C-HGFI microscope (Nikon, Melville, NY, USA). The accumulation of nuclear p65 was measured by calculating three random fields of view per slide, and the data were indicated as a percentage of nuclear p65 positive cells.
Nuclear and cytoplasmic extraction assay
After the treatment with DHM for 24h, HepG2.2.15 cells in 35 mm dishes were collected and washed twice with cold PBS. Then, 200 µL of Cytoplasmic Extraction Reagent I was added to each dish, which was left on ice for 15 min. Next, 10 µL of Cytoplasmic Extraction Reagent II was added, followed by incubation on ice for 1 min. The cell lysates were collected into tubes for centrifugation at 12,000× g for 5 min. After the collection of supernatants (Cytoplasmic extract), 50 µL of Nuclear Extraction Reagent was added to each tube. The samples were mixed and placed on ice for 30 min. After the centrifugation at 12,000× g for 15 min, the supernatants were collected as a nuclear extract.
Statistical analysis
All quantitative data were shown as mean ± standard deviation (SD) and compared by the student’s t-test and one-way Analysis of Variance (ANOVA) followed by Turkey’s post-hoc analysis. A value of P < 0.05 was considered significant.
Results
DHM inhibited HBV replication in HepG2.2.15 cells
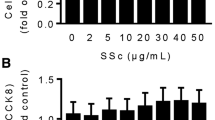
Using HPLC-MS/MS, we first analyzed the structure of DHM with a high purity (Supplementary Fig. 1), which was qualified for the following experiments. Firstly, we assessed the viability of HepG2.2.15 cells treated with different concentrations of DHM (30 − 120 µM) or 3-TC (an antiviral drug) (12.5 − 100 µg/mL) by MTT assay. As shown in Fig. 1a, compared with the Ctrl group, there had no significant differences in cell viability between DHM treatment groups after 24 h co-culturing, suggesting that DHM was non-toxic to HepG2.2.15 cells at the experimental doses. However, 100 µg/mL of 3-TC had a significant toxic effect on HepG2.2.15 cells (Supplementary Fig. 2a).
Effect of DHM on HBV replication in HepG2.2.15 cells. (a) Cell viability was measured by MTT to assess the cytotoxic effect of DHM on HepG2.2.15 cells. (b) Cells were treated with DHM (30 − 120 µM) or 3-TC (50 µg/mL) for 24 h. Then, the secretion of HBV DNA particles in the culture medium was examined by qRT-PCR. (c-d) HBsAg (c) and HBeAg (d) levels in the culture medium were evaluated by ELISA. (e-f) HepG2.2.15 cells were treated with DHM (30 − 120 µM) or 3-TC (50 µg/mL) for 6 h. Then, cells were harvested for detections of total HBV RNA (e), HBV pgRNA (f), and HBV pcRNA (g) at RNA levels by qRT-PCR. Data were presented as mean ± SD. *P < 0.05, **P < 0.01, vs. Ctrl group
Since HBV DNA reflects the level of HBV replication in hepatocytes, it is regarded as an indicator of the efficacy of antiviral drugs. Thus, we measured the concentration of HBV-DNA in the culture medium among experimental groups using a Hepatitis B Virus Nucleic Acid Quantitative Detection Kit. The result showed that both DHM (30 − 120 µM) and 3-TC (12.5 − 50 µg/mL) remarkably reduced HBV-DNA levels in HepG2.2.15 cells (P < 0.01, vs. Ctrl group) (Fig. 1b and Supplementary Fig. 2b). Also, HBsAg and HBeAg were used to indicate HBV replication. The ELISA assay suggested that DHM treatment (30 − 120 µM) for 6 − 24 h statistically reduced the secretion of HBeAg and HBsAg in the culture medium of HepG2.2.15 cells in a dose- and time-dependent manner (P < 0.05 or 0.01, vs. Ctrl group) (Fig. 1c and 1d). However, 3-TC (12.5 − 50 µg/mL) failed to suppress the production of both HBV antigens (Supplementary Fig. 2c and 2d). Further, DHM treatment (30 − 120 µM) significantly inhibited the mRNA levels of HBV RNAs dose-dependently, including total HBV RNA, HBV pregenomic RNA (pgRNA), and HBV precore mRNA (pcRNA) (P < 0.05 or 0.01, vs. Ctrl group) (Fig. 1e -1g). The co-administration of DHM and 3-TC did not display a synergistic effect on the suppressions of three HBVs in HepG2.2.15 cells.
DHM altered mRNA expressions of inflammatory cytokines and antiviral genes in HepG2.2.15 cells
To determine whether the inhibitory effect of DHM on HBV replication is associated with the activated innate immune responses, we evaluated the expressions of inflammatory cytokines and their downstream antiviral regulators. It was suggested that DHM treatment (30 − 120 µM) for 6 h remarkably increased the mRNA levels of inflammatory cytokines in HepG2.2.15 cells in a dose-dependent manner, including IL-6, IL-8, TNF-α (P < 0.05 or 0.01, vs. Ctrl group) (Fig. 2a − 2c). DHM (120 µM) also significantly elevated the mRNA expression of IFN-α, an important anti-virus cytokine (P < 0.05, vs. Ctrl group) (Fig. 2d).
Effect of DHM treatment on mRNA expressions of inflammatory cytokines and antiviral genes in HepG2.2.15 cells. Cells were treated with DHM (30, 60, 120 µM), 3-TC (50 µg/mL), or DHM (60 µM) plus 3-TC (50 µg/mL) for 6 h. After that, the RNA was extracted and amplified by qRT-PCR to detect the levels of IL-6 (a), IL-8 (b), TNF-α (c), IFN-α (d), HNF4α (e), MxA (f), PKR (g), and OAS (h). Data were presented as mean ± SD. *P < 0.01, **P < 0.05, vs. Ctrl group
HNF4α is a member of the hepatocyte nuclear factor (HNF) family and plays a crucial role in the transcriptional regulation of HBV. Therefore, we investigated whether DHM treatment affected the expression of HNF in HepG2.2.15 cells. As shown in Fig. 2e, DHM (30 − 120 µM) markedly downregulated the mRNA level of HNF4α than that of the Ctrl group (P < 0.05 or 0.01). Next, we detected the transcriptional changes of three interferon-inducible antiviral proteins in HepG2.2.15 cells after DHM treatment, i.e., 2’,5’-oligoadenylate synthetase (OAS), myxovirus resistance A protein (MxA), and protein kinase R(PKR). As expected, the mRNA levels of all three proteins were elevated in DHM-treated HepG2.2.15 cells to certain extents (P < 0.05 or 0.01, vs. Ctrl group) (Fig. 2f−2 h), providing a basis for the antiviral effect of DHM. Overall, the anti-HBV activity of DHM was comparable to that of 3-TC, and the combination of both compounds led to more robust biological activities in promoting the expressions of IL-8, TNF-α, MxA, and PKR compared with DHM or 3-TC treatment alone (Fig. 2b, 2c 2f, and 2 g). Next, we performed the same treatment on the HepG2 cell line, the parental cells of HepG2.2.15. On the contrary, DHM treatment decreased the mRNA levels of inflammatory cytokines and antiviral genes in HepG2 cells (P < 0.05 or 0.01, vs. Ctrl group) (Supplementary Fig. 3), suggesting a specific effect of DHM on HBV replication.
DHM promoted activation of NF-κB and MAPKs signaling pathways in HepG2.2.15 cells
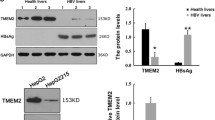
NF-κB is an essential transcriptional regulator responsible for pro-inflammatory gene expression in immune responses. We examined the promotive effect of DHM on activating the NF-κB signaling pathway in HepG2.2.15 cells by Western Blot. As suggested in Fig. 3a, DHM treatment (30 − 120 µM) for 24 h slightly increased the protein level of TLR4 (no significance), a membrane receptor mediated by inflammatory inducers. Meanwhile, DHM treatment (120 µM) elevated the phosphorylation of p65 (a key subunit of NF-κB) but down-regulated the protein expression of IκBα (a negative controller of NF-κB) (P < 0.05 or 0.01, vs. Ctrl group) (Fig. 3b and 3c).
Promotive effect of DHM treatment on activation of NF-κB and MAPK signaling pathways in HepG2.2.15 cells. After the treatment with DHM (30, 60, 120 µM) for 24 h, cells were collected for Western blot analysis. (a − c) Protein levels of the NF-κB pathway, including TLR4 (a), p-P65 (b), and IκBα (c). (d − f) Protein levels of the MAPK signaling pathway, including p-P38 (d), p-ERK (e), and p-JNK (f). Data were presented as mean ± SD. **P < 0.01, *P < 0.05, vs. Ctrl group
The MAPKs are an important type of phosphorylation kinases involved in inflammatory reaction-associated signal transduction [15]. Using Western blot assay, we obtained a similar result as the above (Fig. 3d − 3f). Briefly, DHM treatment for 24 h significantly activated the phosphorylated levels of P38, ERK, and JNK in HepG2.2.15 cells (P < 0.05 or 0.01, vs. Ctrl group). However, DHM did not affected the activation of NF-κB and MPAK pathways in HepG2 cells (Supplementary Fig. 4a and 4b).
DHM facilitated p65 nuclear translocation in HepG2.2.15 cells
To confirm the effect of DHM on NF-κB pathway activation, we performed immunofluorescence staining to check the distribution of p65 subunit in HepG2.2.15 cells. The result indicates that DHM treatment (30 − 120 µM) for 12 h led to the translocation of p65 from the cytoplasm into the nucleus. And the fluorescence intensity of P65 in the nucleus was enhanced with the increased DHM concentration, indicating the NF-κB activation induced by DHM treatment (Fig. 4a). This was further validated by the nuclear and cytoplasmic extraction assay of p65, in which DHM treatment for 24 h elevated the P65 protein accumulation in the nucleus but reduced its distribution in the cytoplasm (Fig. 4b).
Boosted translocation of NF-κB/p65 from cytoplasm into nucleus of HepG2.2.15 cells by DHM treatment. (a) Immunofluorescence assay of HepG2.2.15 cells treated with DHM (30, 60, 120 µM). Green fluorescence, p65 staining; Blue fluorescence, nuclear staining. Red arrow, p65 location in the nucleus. (b) Protein levels of p65 in the cytoplasm and nucleus of HepG2.2.15 cells treated with DHM (30, 60, 120 µM) for 24 h using a nuclear and cytoplasmic extraction kit. Histone H3 and β-actin were separately used as the internal standards of cytoplasm and nucleus. Data were presented as mean ± SD. *P < 0.05, **P < 0.01, vs. Ctrl group
DHM induced autophagy via regulation of PI3K-Akt-mTOR pathway in HepG2.2.15 cells
To assess whether autophagy was involved in DHM-initiated inhibition of HBV replication, we detected the expressions of autophagy-related proteins like Beclin-1, p62, and LC3B in HepG2.2.15 cells treated with DHM (30 − 120 µM) for 24 h. It was revealed that the expression of adopter protein p62 was increased in a dose-dependent manner after DHM treatment, so did the protein levels of Beclin-1 and LC3 II (P < 0.05 or 0.01, vs. Ctrl group) (Fig. 5a). Additionally, DHM treatment had no effect on the protein levels of mTOR, Beclin-1, p62, and LC3B in HepG2 cells (Supplementary Fig. 4c).
Activation of DHM on autophagy via regulation of PI3K-Akt-mTOR signaling pathway in HepG2.2.15 cells. Cells were treated with DHM (30, 60, 120 µM) for 24 h, and the protein was extracted for further experiments. (a) Protein expression analysis of mTOR, Beclin-1, p62, and LC3 I/II by western blot assay. (b) Protein expression analysis of p-PI3K, PI3K, p-Akt473, and Akt. Data were presented as mean ± SD. **P < 0.01, *P < 0.05, vs. Ctrl group
Extensive molecular interactions occur in the early stages of autophagosome formation, and the PI3K-Akt-mTOR pathway is one of the most studied ones[17]. We first studied the change of mTOR, a suppressor of autophagy [18]. The result showed that high doses of DHM significantly reduced the protein level of mTOR in HepG2.2.15 cells (P < 0.05, vs. Ctrl group) (Fig. 5a). Next, we analyzed the effect of DHM on the phosphorylation of PI3K and Akt, which initiated the upstream signaling cascade to regulate the activity of mTOR. However, DHM treatment did not affect the activation of both phosphorylated kinases, suggesting that PI3K and Akt were not the direct targets of DHM (Fig. 5b).
Discussion
In the past decade, viral hepatitis has been the seventh leading cause of death globally, and the mortality is higher than those of AIDS, diabetes, and tuberculosis [19]. Due to the limited clinical efficacy of present chemical drugs and immunosuppressors, researchers made efforts to discover new natural compounds for HBV treatment. So far, various medical plants have been demonstrated to display antiviral activities. For example, Catechins and epigallocatechin gallate (EGCG) in green tea were shown to block the cellular entry of HBV, reduce HBV DNA proliferation, and decrease HBsAg level in HBV-infected mice [20]. Curcumin suppressed internalization, attachment, and final viral load of HBV [21]. The anti-HBV activity of luteolin in vitro and in vivo was dependent on the repressed HNF4α and its binding to HBV promoters[22]. This study found that DHM could hamper HBV replication by activating NF-κB, MAPKs, and autophagy in HepG2.2.15 cells.
During the process of HBV invasion into hepatocytes, the cccDNA that forms in the nucleus serves as a transcription template for all viral transcripts, including the 3.5 kb pcRNA and pgRNA, the 2.4 kb and 2.1 kb surface mRNAs, and a 0.7 kb X mRNA. Then the viral mRNA was translated into viral protein in the cytoplasm. Among the viral transcripts, pcRNA encodes HBeAg protein, and pgRNA translates viral HBc and Pol proteins. Also, pgRNA acts as a template for the replication of HBV genome. The surface mRNAs encode LS, MS, and S proteins. In addition, the X mRNA translates HBx protein [19]. After that, the progeny viral capsids will assemble, incorporating viral genome and DNA polymerase to form viral core particles [4]. HepG2.2.15 cells are derived from the human hepatoma cell line HepG2 and are characterized by having stable HBV expression and replication in the culture system. Though researchers have reported that HBV components such as HBx can affect the cell cycle and apoptosis in HepG2 cells via regulating intracellular signaling[23], it is reasonable that specific differences exist between the two cell lines due to the additional part of the HBV genome. To determine the relationship between DHM and HBV replication, we chose HepG2.2.15 cells as our in vitro experimental model, which was derived from hepatocellular carcinoma cells HepG2 and was characterized by stable HBV expression and replication in the culture system[24]. Chronic HBV-infected patients with high levels of HBV DNA and HBsAg will more frequently develop into HCC [25]. Therefore, the simultaneous inhibition of viral DNA and antigens should be an ideal approach for anti-HBV therapy. In our study, DHM potently reduced a load of HBV DNA (Fig. 1b). Meanwhile, DHM-treated HepG2.2.15 cells for 6 − 24 h resulted in a significant reduction of HBsAg and HBeAg secretion (Fig. 1c). These results revealed that DHM might be a promising candidate for inhibiting HBV replication and viral antigen expression.
Since cccDNA functions as the template for viral RNAs, the durable existence of cccDNA in infected hepatocytes was the primary reason for the failed HBV eradication. Due to the inaccessibility of cccDNA and the lack of reliable detection methods, viral RNA has recently been used as a biomarker for the transcriptional activity of cccDNA to monitor the treatment effect of patients with chronic HBV infection [26]. In this study, DHM treatment prominently reduced the levels of HBV RNA in HepG2.2.15 cells, including Total HBV RNA, HBV pcRNA, and HBV pgRNA (Fig. 1d). Based on the above, DHM displayed potential in dampening down the replication of HBV at mRNA and protein levels.
During HBV infection, the virus recruits several cellular regulators to regulate multiple steps of the HBV replication cycle[19]. Moreover, HBV could selectively and specifically alter the expression of intracellular cytokines involved in the host immune response, ultimately interfering persistent viral infection[27]. In our study, DHM and 3TC can differentially upregulate the expressions of intracellular cytokines (such as IL-6, IL-8, TNF-α, and IFN-α), which play important roles in viral clearance (Fig. 2a - 2d) [28]. Among them, IFNs triggers antiviral effects by inducing the production of related regulators, such as OAS, MxA, and PKR [29]. Our results indicate that DHM promoted interferon production and activated the release of above antiviral proteins (Fig. 2f h). HNF4α, a member of the nuclear receptor superfamily, controls up to 60% of hepatic gene expression. The expression level of HNF4α was positively correlated with HBV replication and HBV DNA production [30]. In parallel, our studies found that DHM treatment significantly suppressed the expression of HNF4α RNA in HepG2.2.15 cells (Fig. 2e). Next, we explored whether the combination of DHM and 3-TC had a synergistic effect. The 3-TC is a nucleotide analog and inhibits viral replication by targeting the DNA polymerase of HBV. Indeed, the combination of both drugs further promoted the expressions of some cytokines and antiviral proteins, such as IL-8, TNF-α, MxA, and PKR (Fig. 2). Collectively, the anti-HBV effect of DHM might be related to the increments of inflammatory cytokines or regulators produced form HepG2.2.15 cells.
Host immune response to HBV infection has long been recognized as a clinical reaction to acute infection [31]. It is proposed that the innate immune cells identify viral particles through several families of pattern-recognition receptors (PRRs) expressed on the cell membrane. Among these PRRs, TLRs are the most prominent ones [32]. Upon activation, TLRs will recruit adaptor proteins, which initiate the transduction of downstream pathways (like NF-κB and MAPKs) and the final expression of inflammatory cytokines to resist pathogen infection [33]. In the present study, DHM increased TLR4 protein expression in HepG2.2.15 cells, suggesting that the TLR4-mediated signaling pathway may be a critical mechanism of DHM against HBV. Besides, DHM enhanced the activity of NF-κB signaling by facilitating the IκBα degradation, p65 phosphorylation, and its subsequent translocation from the cytoplasm to the nucleus (Figs. 3b and 3c, Fig.4). Meanwhile, DHM dramatically upregulated the MAPK phosphorylation, including p38, ERK, and JNK (Fig. 3d − 3f). MAPKs are classical kinases involved in multiple cellular events such as immune defense and inflammatory response [34]. Therefore, we presume that DHM can elevate the expressions of inflammatory cytokines by activating NF-κB and MAPK signaling pathways.
Autophagy is a highly conserved catabolic process. It is vital to maintain the internal environment stability by removing damaged organelles, long-lived proteins, and misfolded peptides from the cellular microenvironment [35]. Besides the target materials of “self” origin, autophagy also eliminates intracellular pathogens and acts as a defense mechanism to repress infections [36]. Autophagy was activated upon viral or bacterial infection, subsequently exerting a protective function by restricting the replication of intracellular pathogens [1]. For instance, autophagy was critical for regulating the immune response to viral infections like HCV [37]. Hence, activating intracellular autophagy was an important therapeutic strategy to resist pathogen invasion [38]. Consistent with these studies, we observed that DHM activated autophagy in HepG2.2.15 cells indicated by the increases of autophagy biomarkers, including p62, Beclin-1, and LC3 II (Fig. 5a). To explore the molecular mechanism of DHM in activating autophagy, we detected the activation of PI3K-Akt-mTOR pathway that occurred in the early stage of autophagy [39]. The mTOR is a member of the PI3K-associated kinase family and induces the occurrence of autophagy [40]. In this study, we observed that DHM had no effect on the phosphorylation of PI3K and AKT. Still, DHM significantly decreased the mTOR protein level, suggesting the significance of mTOR in DHM-induced autophagy (Fig. 5). Noticeably, studies have demonstrated the contribution of NF-κB to autophagic activation by upregulating Beclin-1 expression [41]. Moreover, NF-κB can induce autophagy by transactivating the inflammatory genes, such as IL-1β, TNF-α, and TGF-β[42,43,44]. Hence, we presume that DHM might activate autophagy through the NF-κB-medicated signal transduction.
Conclusion
In summary, we demonstrated that DHM effectively inhibited HBV replication in HepG2.2.15 cells. Further studies show that DHM promoted the expressions of inflammatory cytokines, IFN-α, and IFN-α-mediated antiviral effectors. Meanwhile, DHM reduced the mRNA level of the nuclear receptor HNF4α. The molecular mechanism of DHM was related to the activation of NF-κB and MAPK signaling pathways in HepG2.2.15 cells. Also, activated autophagy was another contributor that may accelerate the clearance of HBV components in DHM-treated HepG2.2.15 cells (Supplementary Fig. 5). Taken together, this study shed light on the application of DHM for the clinical treatment of HBV infection in the future.
Abbreviations
- HBV:
-
Hepatitis B virus.
- DHM:
-
Dihydromyricetin.
- rcDNA:
-
double-stranded relaxed circular DNA.
- cccDNA:
-
covalently closed circular DNA.
- pgRNA:
-
HBV pregenomic RNA.
- pcRNA:
-
HBV precore mRNA.
- NF-κB:
-
Nuclear factor-kappa B.
- MAPK:
-
Mitogen-activated protein kinase.
- IFN:
-
Interferon.
- OAS:
-
2’,5’-oligoadenylate synthetase.
- MxA:
-
Myxovirus resistance A protein.
- PKR:
-
Protein kinase R.
References
Yang Y, Liu Y, Xue J et al (2017) MicroRNA-141 Targets Sirt1 and Inhibits Autophagy to Reduce HBV Replication. Cell Physiol Biochem 41:310–322. https://doi.org/10.1159/000456162
Li X, Wu S, Du Y et al (2020) Entecavir therapy reverses gut microbiota dysbiosis induced by hepatitis B virus infection in a mouse model. Int J Antimicrob Agents 56:106000. https://doi.org/10.1016/j.ijantimicag.2020.106000
Yang H, Zhou Y, Mo J et al (2020) SOX9 represses hepatitis B virus replication through binding to HBV EnhII/Cp and inhibiting the promoter activity. Antiviral Res 177:104761. https://doi.org/10.1016/j.antiviral.2020.104761
Liu S, Zhou B, Valdes JD et al (2019) Serum Hepatitis B Virus RNA: A New Potential Biomarker for Chronic Hepatitis B Virus Infection. Hepatology 69:1816–1827. https://doi.org/10.1002/hep.30325
Pant K, Yadav AK, Gupta P et al (2016) Humic acid inhibits HBV-induced autophagosome formation and induces apoptosis in HBV-transfected Hep G2 cells. Sci Rep 6:34496. https://doi.org/10.1038/srep34496
Wu LL, Peng WH, Wu HL et al (2019) Lymphocyte Antigen 6 Complex, Locus C(+) Monocytes and Kupffer Cells Orchestrate Liver Immune Responses Against Hepatitis B Virus in Mice. Hepatology 69:2364–2380. https://doi.org/10.1002/hep.30510
De Ridder F, Sonneveld MJ, Lenz O et al (2021) Mean HBsAg decline at week 24 of PEG-IFN-based treatment predicts subsequent rate of HBsAg clearance - suggesting a valuable endpoint for early development HBV trials. J Viral Hepat 28:1563–1569. https://doi.org/10.1111/jvh.13599
Park YK, Lee SY, Lee AR et al (2020) Antiviral activity of interferon-stimulated gene 20, as a putative repressor binding to hepatitis B virus enhancer II and core promoter. J Gastroenterol Hepatol 35:1426–1436. https://doi.org/10.1111/jgh.14986
Wang YX, Niklasch M, Liu T et al (2020) Interferon-inducible MX2 is a host restriction factor of hepatitis B virus replication. J Hepatol 72:865–876. https://doi.org/10.1016/j.jhep.2019.12.009
Sun Z, Lu W, Lin N et al (2020) Dihydromyricetin alleviates doxorubicin-induced cardiotoxicity by inhibiting NLRP3 inflammasome through activation of SIRT1. Biochem Pharmacol 175:113888. https://doi.org/10.1016/j.bcp.2020.113888
Tong H, Zhang X, Tan L et al (2020) Multitarget and promising role of dihydromyricetin in the treatment of metabolic diseases. Eur J Pharmacol 870:172888. https://doi.org/10.1016/j.ejphar.2019.172888
Liu TT, Zeng Y, Tang K et al (2017) Dihydromyricetin ameliorates atherosclerosis in LDL receptor deficient mice. Atherosclerosis 262:39–50. https://doi.org/10.1016/j.atherosclerosis.2017.05.003
Li H, Li Q, Liu Z et al (2017) ; 2017: 1053617. https://doi.org/10.1155/2017/1053617
Zhou HY, Gao SQ, Gong YS et al (2020) Anti-HSV-1 effect of dihydromyricetin from Ampelopsis grossedentata via the TLR9-dependent anti-inflammatory pathway. J Glob Antimicrob Resist 23:370–376. https://doi.org/10.1016/j.jgar.2020.10.003
Zhang E, Lu M (2015) Toll-like receptor (TLR)-mediated innate immune responses in the control of hepatitis B virus (HBV) infection. Med Microbiol Immunol 204:11–20. https://doi.org/10.1007/s00430-014-0370-1
Nguyen MH, Wong G, Gane E et al (2020) Hepatitis B Virus, Advances in Prevention, Diagnosis, and Therapy. Clin Microbiol Reviews 33:e00046–e00019. https://doi.org/10.1128/CMR.00046-19
Yang J, Pi C, Wang G (2018) Inhibition of PI3K/Akt/mTOR pathway by apigenin induces apoptosis and autophagy in hepatocellular carcinoma cells. Biomed Pharmacother 103:699–707. https://doi.org/10.1016/j.biopha.2018.04.072
Wang H, Liu Y, Wang D et al (2019) The Upstream Pathway of mTOR-Mediated Autophagy in Liver Diseases. Cells 8. https://doi.org/10.3390/cells8121597
Qu B, Brown RJP (2021) Strategies to Inhibit Hepatitis B Virus at the Transcript Level. Viruses 13. https://doi.org/10.3390/v13071327
Lai YH, Sun CP, Huang HC et al (2018) Epigallocatechin gallate inhibits hepatitis B virus infection in human liver chimeric mice. BMC Complement Altern Med 18:248. https://doi.org/10.1186/s12906-018-2316-4
Thongsri P, Pewkliang Y, Borwornpinyo S et al (2021) Curcumin inhibited hepatitis B viral entry through NTCP binding. Sci Rep 11:19125. https://doi.org/10.1038/s41598-021-98243-x
Bai L, Nong Y, Shi Y et al (2016) Luteolin Inhibits Hepatitis B Virus Replication through Extracellular Signal-Regulated Kinase-Mediated Down-Regulation of Hepatocyte Nuclear Factor 4alpha Expression. Mol Pharm 13:568–577. https://doi.org/10.1021/acs.molpharmaceut.5b00789
Zhong LH, Zhu LY, Zhao YY et al (2018) Apoptosis of hepatocarcinoma cells Hepg2 induced by Huaier extract through regulation of HBx and CEACAM1 gene expression. J Biol Regul Homeost Agents 32:1389–1398
Wang B, Zhao XP, Fan YC et al (2013) IL-17A but not IL-22 suppresses the replication of hepatitis B virus mediated by over-expression of MxA and OAS mRNA in the HepG2.2.15 cell line. Antiviral Res 97:285–292. https://doi.org/10.1016/j.antiviral.2012.12.018
Mueller H, Wildum S, Luangsay S et al (2018) A novel orally available small molecule that inhibits hepatitis B virus expression. J Hepatol 68:412–420. https://doi.org/10.1016/j.jhep.2017.10.014
Jansen L, Kootstra NA, van Dort KA et al (2016) Hepatitis B Virus Pregenomic RNA Is Present in Virions in Plasma and Is Associated With a Response to Pegylated Interferon Alfa-2a and Nucleos(t)ide Analogues. J Infect Dis 213:224–232. https://doi.org/10.1093/infdis/jiv397
Kong F, You H, Kong D et al (2019) The interaction of hepatitis B virus with the ubiquitin proteasome system in viral replication and associated pathogenesis. Virol J 16:73. https://doi.org/10.1186/s12985-019-1183-z
Das D, Sengupta I, Sarkar N et al (2017) Anti-hepatitis B virus (HBV) response of imiquimod based toll like receptor 7 ligand in hbv-positive human hepatocelluar carcinoma cell line. BMC Infect Dis 17:76. https://doi.org/10.1186/s12879-017-2189-z
Wan Y, Cao W, Han T et al (2017) Inducible Rubicon facilitates viral replication by antagonizing interferon production. Cell Mol Immunol 14:607–620. https://doi.org/10.1038/cmi.2017.1
Pan Y, Ke Z, Ye H et al (2019) Saikosaponin C exerts anti-HBV effects by attenuating HNF1alpha and HNF4alpha expression to suppress HBV pgRNA synthesis. Inflamm Res 68:1025–1034. https://doi.org/10.1007/s00011-019-01284-2
Boni C, Vecchi A, Rossi M et al (2018) TLR7 Agonist Increases Responses of Hepatitis B Virus-Specific T Cells and Natural Killer Cells in Patients With Chronic Hepatitis B Treated With Nucleos(T)Ide Analogues. Gastroenterology 154:1764–1777e1767. https://doi.org/10.1053/j.gastro.2018.01.030
Min Y, Lee S, Kim MJ et al (2017) Ubiquitin-Specific Protease 14 Negatively Regulates Toll-Like Receptor 4-Mediated Signaling and Autophagy Induction by Inhibiting Ubiquitination of TAK1-Binding Protein 2 and Beclin 1. Front Immunol 8:1827. https://doi.org/10.3389/fimmu.2017.01827
Pandey S, Kawai T, Akira S (2015) Microbial Sensing by Toll-Like Receptors and Intracellular Nucleic Acid Sensors. Cold Spring Harb Perspect Biol. https://doi.org/10.1101/cshperspect.a016246
Wang QQ, Gao H, Yuan R et al (2020) Procyanidin A2, a polyphenolic compound, exerts anti-inflammatory and anti-oxidative activity in lipopolysaccharide-stimulated RAW264.7 cells. PLoS ONE 15:e0237017. https://doi.org/10.1371/journal.pone.0237017
Wu WKK, Zhang L, Chan MTV, Autophagy NAFLD, NAFLD-Related HCC (2018) Adv Exp Med Biol 1061:127–138. https://doi.org/10.1007/978-981-10-8684-7_10
Khan M, Imam H, Siddiqui A (2018) Subversion of cellular autophagy during virus infection: Insights from hepatitis B and hepatitis C viruses. Liver Res 2:146–156. https://doi.org/10.1016/j.livres.2018.09.002
Chan ST, Ou JJ, Hepatitis C (2017) Virus-Induced Autophagy and Host Innate Immune Response. Viruses 9. https://doi.org/10.3390/v9080224
Zhou M, Xu W, Wang J et al (2018) Boosting mTOR-dependent autophagy via upstream TLR4-MyD88-MAPK signalling and downstream NF-kappaB pathway quenches intestinal inflammation and oxidative stress injury. EBioMedicine 35:345–360. https://doi.org/10.1016/j.ebiom.2018.08.035
Xu Z, Han X, Ou D et al (2020) Targeting PI3K/AKT/mTOR-mediated autophagy for tumor therapy. Appl Microbiol Biotechnol 104:575–587. https://doi.org/10.1007/s00253-019-10257-8
Xia J, Guo S, Fang T et al (2014) Dihydromyricetin induces autophagy in HepG2 cells involved in inhibition of mTOR and regulating its upstream pathways. Food Chem Toxicol 66:7–13. https://doi.org/10.1016/j.fct.2014.01.014
Cao S, Huang Y, Zhang Q et al (2019) Molecular mechanisms of apoptosis and autophagy elicited by combined treatment with oridonin and cetuximab in laryngeal squamous cell carcinoma. Apoptosis 24:33–45. https://doi.org/10.1007/s10495-018-1497-0
Zhang P, Xin X, Fang L et al (2017) HMGB1 mediates Aspergillus fumigatus-induced inflammatory response in alveolar macrophages of COPD mice via activating MyD88/NF-kappaB and syk/PI3K signalings. Int Immunopharmacol 53:125–132. https://doi.org/10.1016/j.intimp.2017.10.007
Le Y, Wang Y, Zhou L et al (2020) Cigarette smoke-induced HMGB1 translocation and release contribute to migration and NF-kappaB activation through inducing autophagy in lung macrophages. J Cell Mol Med 24:1319–1331. https://doi.org/10.1111/jcmm.14789
Man S, Li M, Zhou J et al (2020) Polyethyleneimine coated Fe3O4 magnetic nanoparticles induce autophagy, NF-kappaB and TGF-beta signaling pathway activation in HeLa cervical carcinoma cells via reactive oxygen species generation. Biomater Sci 8:201–211. https://doi.org/10.1039/c9bm01563a
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethical approval:
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, X., Hu, H., Hu, B. et al. Dihydromyricetin inhibits Hepatitis B virus replication by activating NF-κB, MAPKs, and autophagy in HepG2.2.15 cells. Mol Biol Rep 50, 1403–1414 (2023). https://doi.org/10.1007/s11033-022-07971-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07971-4