Abstract
Background
The c-myc oncogene, which causes glutamine dependence in triple negative breast cancers (TNBC), is also the target of one of the signaling pathways affected by β-Escin.
Methods and results
We sought to determine how c-myc protein affects glutamine metabolism and the proteins, glutamine transporter alanine-serine-cysteine 2 (ASCT2) and glutaminase (GLS1), in β-Escin-treated MDA-MB-231 cells using glutamine uptake and western blot analysis. Cell viability, colony formation, migration and apoptosis were also evaluated in MDA-MB-231 cells in response to β-Escin treatment using MTS, colony forming, wound healing, and Annexin-V assay. We determined that β-Escin decreased glutamine uptake and reduced c-myc and GLS1 protein expressions and increased the expression of ASCT2. In addition, this inhibition of glutamine metabolism decreased cell proliferation, colony formation and migration, and induced apoptosis.
Conclusions
In this study, it was suggested that β-Escin inhibits glutamine metabolism via c-myc in MDA-MB-231 cells, and it is thought that as a result of interrupting the energy supply in these cells via c-myc, it results in a decrease in the carcinogenic properties of the cells. Consequently, β-Escin may be promising as a therapeutic agent for glutamine-dependent cancers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer, which is complex, multifactorial and highly heterogeneous, is one of the most common cancers worldwide. Breast cancer displays clinical heterogeneity in the expression of genes related to energy metabolism [1, 2]. Breast cancer subtypes are also quite heterogeneous in terms of intake and use of glutamine, which is the second most important energy source for some cancer types [1, 3, 4]. Compared to other breast cancer subtypes, triple negative breast cancer (TNBC), which metastasizes to distant tissue, has very poor prognosis, is aggressive, and has exogenous glutamine dependence [3, 5, 6]. Extracellular glutamine is taken into the cell with the Na+ associated glutamine transporter alanine-serine-cysteine 2 (ASCT2) protein, upregulated by myc [7]. Glutamine taken into the cell is converted into glutamate by the glutaminase (GLS) enzyme, which is in the first step of metabolism [8]. There are two different forms of the GLS enzyme; kidney type glutaminase (GLS1, KGA or GAC) encoded by GLS1 [9] and liver type glutaminase (LGA or GAB) encoded by GLS2 [10]. GLS2 is regulated by p53 tumor suppressor and exhibits tumor suppressive effects [8], while GLS1 expression is upregulated in manycancer types such as breast, colon, pancreas, glioma and lung cancer [1112, 13, 14]. Suppression of glutamine metabolism, which contributes to the progression of glutamine-dependent tumors, is important in reducing the aggressiveness of these tumors and determining therapeutic approaches [15].
Escin is a natural triterpene compound obtained from the seeds of Aesculus hippocastanum. Escin has been used in traditional medicine treatments for centuries [16] and in clinical practice in cases of venous insufficiency in hemorrhoids [17], hematoma, trauma or postoperative to surgery [18, 19]. It was also shown to have anti-proliferative and apoptosis-inducing properties in many types of cancer such as renal cancers [20], leukemia [21,22,23], breast cancer [21], cervical cancer [21], glioma and lung cancer [24]. It was noticed that β-Escin induced apoptosis through the ATM/H2AX pathway in colorectal cancer cells [25], and through the ROS/P38 MAPK pathway in osteosarcoma cells [26]. It inhibited metastasis and angiogenesis through the NF-κB/IκB signaling pathway in melanoma cells [27], and had anti-proliferative effects in hepatocellular carcinoma with STAT3 inhibition [28]. Furthermore, β-Escin decreased c-myc expression, a regulator of glutamine metabolism, one of the disrupted energy metabolisms which is a fundamental feature of cancer progression in various cancer cells [29, 30].
Therefore, the effects of β-Escin were investigated on expression of c-myc, GLS1, ASCT2 and cell proliferation, migration, apoptotic cell death and glutamine metabolism in aggressive TNBC MDA-MB-231 breast cancer cells. Our findings demonstrated that β-Escin treatment suppressed the expression of c-myc, GLS1 and ASCT2, suggesting reduced glutamine metabolism in TNBC cells. Overall, the results demonstrated that β-Escin treatment leads to reduced cell proliferation, migration/invasion and induced apoptotic cell death through suppression of c-myc expression and glutamine metabolism in these cells.
Materials and methods
Cell culture and drug treatment
MDA-MB-231 cell line was obtained from American Type Culture Collection (Manassas, VA, USA). The cells were cultured as described in previous studies [31, 32]. β-Escin was purchased from USP Reference Standard (Cat no: 1,249,202) and dissolved in dimethyl sulfoxide (DMSO; Merck).
Detection of cell viability and proliferation
To detect the effect of β-Escin on cell proliferation of MDA-MB-231 cells, we performed MTS(3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2 H-tetrazolium) analysis. MTS analysis was done as described in previous studies in cells treated with different doses of β-Escin at 24, 48 and 72 h intervals [31, 32]. β-Escin stock solution was dissolved to 1 mM in DMSO and stored at − 80 °C. In the study, the DMSO solvent group was used as the control group and evaluations were made according to the control group.
Western blot analysis and antibodies
MDA-MB-231 cells were treated with β-Escin at 48 h and 16–18 µM concentrations, and western blot analysis was done to define the expression levels of the targeted proteins (c-myc, ASCT2 and GLS1). Lysis of cell samples, total protein extraction and measurement, separation of proteins in SDS-Page and transfer to the membrane, antibody treatment and imaging of target proteins with chemiluminescence were carried out to determine target protein expressions, as stated in previous studies [33].
Glutamine uptake
To detect the effect of β-Escin on glutamine uptake of MDA-MB-231 cells, breast cancer cells, glutamine uptake analyses were performed. Cells were seeded at a density of 1500 cells/well in 96-well plates and β-Escin treatment was administered at the indicated times and concentrations. After 96 h incubation, 2 µl of cell medium was removed and assay steps were followed according to the manufacturer’s protocol (Glutamine/Glutamate-Glo™ assay; Promega). Luminescence measurement was determined using a microculture plate reader (Promega, Glomax-Multi Detection System).
Colony forming assay
To detect the effect of β-Escin on colony formation of MDA-MB-231 cells, clonogenic assay was performed. MDA-MB-231 cells were seeded in 6-well plates and treated with β-Escin at the determined concentrations at 48 h of culture and incubated for 14 days. After incubation, cells were washed with PBS and stained with crystal violet to count visible colonies [31].
Apoptosis analysis
Muse Annexin V apoptosis and dead cell assay reagent were used for apoptosis analysis (Millipore; MCH100115). MDA-MB-231 cells were seeded in 25 cm2 flasks (3.5 × 105 cells/4 ml medium) and treated with β-Escin concentrations for 48 h. Then cells were harvested by removing with trypsin. Afterward, the cells were stained with annexin V and dead cell reagent according to the manufacturer’s protocols (Millipore Corporation) and analyzed using Muse Cell Analyzer (Millipore Corporation).
Scratch wound healing assay
To detect the effect of β-Escin on migration of MDA-MB-231 cells, we performed wound-healing scratch assay. MDA-MB-231 cells were seeded in a 6 well plate (3 × 105 cells/wells), and treated with β-Escin at the indicated concentrations (16–18 µM) for 48 h. Then the cell monolayer was wounded using a 100 µl sterile pipette tip and the cell medium was replaced with fresh medium. Wound areas forming in the cell monolayer were imaged at 0, 24 and 48 h with a phase-contrast microscope and multiple images of the wound areas were measured using Image J program [31].
Statistical analysis
All experiments were performed with at least three repetitions. Statistical analyses were evaluated using GraphPad Prism 6. Data were expressed as mean ± SD and evaluated using the unpaired t test. p < 0.05 was considered statistically significant.
Results
β-Escin treatment suppresses proliferation and colony formation in MDA-MB-231 cells
To determine the effects of β-Escin on MDA-MB-231 cell proliferation and viability, MTS assay was performed after 48 h treatment with increasing doses of β-Escin (16–18µM). The MTS analysis revealed that β-Escin treatment significantly reduced cell proliferation of MDA-MB-231 (Fig. 1a) compared to DMSO-treated control cells. We then investigated the effects of β-Escin on colony formation of MDA-MB-231 cells. β-Escin treatment (10–14 µM) led to a significant reduction in the number of colonies compared to DMSO-treated cells (Control) (Fig. 1b and c).
β-Escin inhibits cell proliferation and colony formation of MDA-MB-231 cells. (a) MDA-MB-231 cells were seeded at a density of 1.5 × 103 cells/well into 96-well plates and treated with a series of concentrations of β-Escin (16, 17, and 18 µM) or a vehicle only control for 48 h and cell viability was measured by MTS assay. (b) A total of 1000 cells were seeded in six-well plates and cultured for 10–14 days. Colony formation was detected. (c) Quantitative analysis of the colony numbers of MDA-MB-231 cells after β-Escin treatment. The values are mean ± SD from three independent experiments. ***p < 0.001, **p < 0.01 vs. the control group
β-Escin treatment inhibits the migration of MDA-MB-231 cells
To determine the effect of β-Escin on cell motility and migration of MDA-MB-231 cells, wound healing analysis was performed. β-Escin treatment (16–18 µM) significantly reduced motility or migration of MDA-MB-231cells (Fig. 2a-b) compared to control cells.
β-Escin inhibits cell motility and migration in MDA-MB-231 cells. Cell migration in cells treated with β-Escin at concentrations of 16, 17, and 18 µM was determined by scratch wound healing analysis. (a) Cells treated with β-Escin for 48 h were wounded with a 100 µl pipette tip. Microscopic images were taken at 0, 24 and 48 h to determine the cell migration in the created wound areas. (b) Quantitative analyses of wound areas in β-Escin-treated cells were compared with the control group treated with DMSO. ***p < 0.001, ns; not significant
β-Escin treatment induces apoptotic cell death in MDA-MB-231 cells
In order to determine the effect of β-Escin on apoptosis in MDA-MB-231 cells, concentrations of β-Escin from 16 to 18 µM, which were identified to reduce cell viability by 50% in MDA-MB-231 cells, were used for treatment for 48 h. Control and β-Escin-treated cells were measured with annexin V staining in flow cytometry. The rate of apoptosis was significantly increased in β-Escin-treated cells compared to controls (Fig. 3a-b). As a result, the treatment of β-Escin on MDA-MB-231 cells induced apoptosis in these cells.
β-Escin induces apoptosis in MDA-MB-231 cells. Cell death by apoptosis in cells treated with β-Escin at concentrations of 16, 17, and 18 µM for 48 h was determined by Muse Cell Analyzer using Annexin V/PI staining. (a) Histogram of apoptotic cells in β-Escin-treated cells after measurement. (b) Analysis of apoptotic cell numbers in β-Escin-treated cells compared to control group. ***p < 0.001, **p < 0.01, *p < 0.05
β-Escin treatment inhibits expression of c-myc and molecules associated with glutamine metabolism, and glutamine metabolism in MDA-MB-231 cells
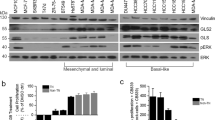
In cancer cells, c-myc plays a role as an important regulator of energy metabolism. It specifically induces mitochondrial biogenesis and regulates GLS1 protein levels via miR-23a/b [29]. Therefore, we analyzed the expression of c-myc in β-Escin-treated MDA-MB-231 cells using western blot. As shown in Fig. 4a-b, β-Escin treatment led to decreased expression of c-myc. Furthermore, we investigated expressions of GLS1 and ASCT2 proteins, which are associated with glutamine metabolism, in β-Escin-treated cells. We found that β-Escin treatment also inhibited expression of GLS1 (Fig. 4a-c), but ASCT2 expression increased compared to controls (Fig. 4d).
β-Escin suppresses glutamine metabolism by downregulating c-myc protein expression. MDA-MB-231 cells were treated with 16, 17, and 18 µM concentrations of β-Escin for 48 h. (a) c-myc and glutamine metabolism-associated GLS1 and ASCT2 protein expression in MDA-MB-231 cells treated with the concentrations of 16, 17 and 18 µM β-Escin were determined by western blot analysis. (b) Quantitative analysis of the optical density ratio of c-myc compared with the loading control (tubulin) in MDA-MB-231 cells. (c) Quantitative analysis of the optical density ratio of GLS1 compared with the loading control (tubulin) in MDA-MB-231 cells. (d) Quantitative analysis of the optical density ratio of ASCT2 compared with the loading control (tubulin) in MDA-MB-231 cells. (e) Glutamine uptake in MDA-MB-231 cells after β-Escin treatment was determined by measuring the relative light unit (RLU) by luminescent imaging. The values are mean ± SD from three independent experiments. ***p < 0.001 vs. the control group
Next, glutamine uptake analysis was performed to determine if glutamine uptake was altered by inhibition of c-myc expression in β-Escin-treated cells. The amount of glutamine in the culture medium of β-Escin-treated cells and control cells was determined with the relative light unit (RLU) values obtained as a result of luminescence measurements. The RLU values showed that the amount of glutamine in culture medium of the β-Escin-treated cells was higher than the controls (Fig. 4e). Our results indicate that the glutamine uptake decreased in β-Escin-treated cells compared to control cells.
Discussion
Glutamine dependence is due to mutations that result in activation of the c-myc oncogene or loss of tumor suppressors such as Rb, which triggers glutamine uptake and utilization through up-regulation of enzymes and cellular transporters that support replication in tumors, causing an aggressive cancer phenotype [34, 35]. Breast cancer, with heterogeneous tumor character, is also heterogeneous in terms of glutamine metabolism. The c-myc oncogene, which is associated with reprogramming in tumorigenesis, is overexpressed in 40% of TNBCs, making these cells glutamine dependent [36]. The glutamine-dependent phenotype of TNBC tumors provides an opportunity to offer effective therapies targeting c-myc and glutamine metabolism-related enzymes as the main susceptibility of these tumors. In this respect, β-Escin has anti-proliferative properties through the pathways it affects in many cancers.
Escin induced DNA disease and apoptosis via the ATM/H2AX pathway at large amounts in HCT116 colorectal cancer [25]. Wang et al. [37] stated that Escin Ia suppressed the metastasis of TNBC cells by inhibiting epithelial mesenchymal transformation. During in vivo and in vitro studies with human osteosarcoma cells, autophagy and caspase-dependent apoptosis were induced via the ROS/P38 MAPK pathway. In B16F10 and SK-MEL5 melanoma cells, β-Escin was suggested to inhibit anti-tumorigenic properties such as metastasis and angiogenesis via NF-κB/IκB signaling [38]. It was reported that β-Escin inhibits ECM production in omental tumors and blocks the production of proteins such as HIF1α-targeted lactate dehydrogenase A and hexokinase 2 in these tumors. β-Escin was reported to have therapeutic potential in the OvCa tumor microenvironment due to its ability to inhibit OvCa spread by targeting both cancer and stromal cells [39]. Wang et al. [27] showed that β-Escin inhibited NF-kB and NF-kB-regulated gene products such as c-myc, Cyclin D1, COX2, Survivin, and Bcl-2 in pancreatic cancer. β-Escin treated to hepatocellular carcinoma cells inhibited signal transducer and activator of transcription 3 (STAT3) and down regulated the expression of STAT3-regulated gene products; thus, suppressing cellular proliferation and providing chemotherapy sensitivity [28]. Omi et al. [40] showed that Escin inhibited angiogenesis by blocking NF-kB activity in pancreatic cancer cell PaCa and decreasing IL-8 and VEGF secretion. It was stated that β-Escin treatment prevents metastasis in A549 cells through the inhibition of reactive oxygen species in hypoxia-induced metastasis caused by HIF-lα activation, transforming growth factor-β and matrix metalloproteinases [41]. Huang et al. [42] stated that β-Escin administration to cholangiocarcinoma cells reversed P-gp-dependent multidrug resistance by inhibition of the GSK3β/β-catenin pathway, and they stated that the use of β-Escin in combination for the treatment of these cancers is promising. In this study, we determined that β-Escin decreased the protein expression of c-myc, which is regulated to amino acid metabolism in MDA-MB-231 cells. In addition, we showed that GLS1, one of the glutamine metabolism proteins, also reduced protein expression. We also showed that β-Escin reduces glutamine uptake of glutamine-dependent MDA-MB-231 cells, inhibits proliferation, colony formation and migration, and also induces apoptosis.
Glutamine metabolism-related proteins show heterogeneity in breast cancer subtypes. van Geldermalsen et al. [43] stated that ASCT2 has high expression in most breast cancers, but ASCT2-mediated glutamine uptake is required for maintenance of cancer progression and mTORC1 signaling only in TNBC. In this study, which was performed with MDA-MB-231 cells, it is understood that the amount of glutamine taken into the cells decreased in cells treated with β-Escin, but this situation was not related to the protein levels of ASCT2. It was thought that the only reason for the reduction in the amount of glutamine uptake into cells without reduction in ASCT2 protein levels was the GLS1 levels in β-Escin-treated cells.
In conclusion, in this study, we think that β-Escin exerts anti-carcinogenic effects through c-myc in MDA-MB-231 cells and may be promising as a therapeutic agent for glutamine-dependent cancers. Because c-myc is a regulator of amino acid metabolism and can achieve these effects by inhibition of c-myc. However, further analysis is required to prove that β-Escin mediates these effects through downregulation of c-myc. We plan to conduct these analyzes in future studies to be show that c-myc is directly affected by β-Escin.
Code availability
Not applicable.
References
Cappelletti V, Iorio E, Miodini P, Silvestri M, Dugo M, Daidone MG (2017) Metabolic Footprints and Molecular Subtypes in Breast Cancer. Disease markers 7687851
El Ansari R, McIntyre A, Craze ML, Ellis IO, Rakha EA, Green AR (2018) Altered glutamine metabolism in breast cancer; subtype dependencies and alternative adaptations. Histopathology 72:183–190
Kim S, Kim DH, Jung WH, Koo JS (2013) Expression of glutamine metabolism-related proteins according to molecular subtype of breast cancer. Endocrine-related Cancer 20:339–348
Delgir S, Bastami M, Ilkhani K, Safi A, Seif F, Alivand MR (2021) The pathways related to glutamine metabolism, glutamine inhibitors and their implication for improving the efficiency of chemotherapy in triple-negative breast cancer. Mutat Res Reviews Mutat Res 787:108366
Lampa M, Arlt H, He T, Ospina B, Reeves J et al (2017) Glutaminase is essential for the growth of triple-negative breast cancer cells with a deregulated glutamine metabolism pathway and its suppression synergizes with mTOR inhibition. PLoS ONE 12:e0185092
Edwards DN, Ngwa VM, Raybuck AL, Wang S, Hwang Y et al (2021) Selective glutamine metabolism inhibition in tumor cells improves antitumor T lymphocyte activity in triple-negative breast cancer. The Journal of clinical investigation 131
Masisi BK, El Ansari R, Alfarsi L, Rakha EA, Green AR, Craze ML (2020) The role of glutaminase in cancer. Histopathology 76:498–508
Mates JM, Segura JA, Martin-Rufian M et al (2013) Glutaminase isoenzymes as key regulators in metabolic and oxidative stress against cancer. Curr Mol Med 13:514–534
Katt WP, Lukey MJ, Cerione RA (2017) A tale of two glutaminases: homologous enzymes with distinct roles in tumorigenesis. Future Med Chem 9:223–243
Martín-Rufián M, Tosina M, Campos-Sandoval JA, Manzanares E, Lobo C et al (2012) Mammalian glutaminase Gls2 gene encodes two functional alternative transcripts by a surrogate promoter usage mechanism. PLoS ONE 7:e38380
Gao P, Tchernyshyov I, Chang T-C, Lee Y-S, Kita K et al (2009) c-Myc suppression of miR-23a/b enhances mitochondrial glutaminase expression and glutamine metabolism. Nature 458:762–765
Shukla SK, Purohit V, Mehla K, Gunda V, Chaika NV et al (2017) MUC1 and HIF-1alpha signaling crosstalk induces anabolic glucose metabolism to impart gemcitabine resistance to pancreatic cancer. Cancer Cell 32:71–87 e7
Anso E, Mullen AR, Felsher DW, Matés JM, DeBerardinis RJ, Chandel NS (2013) Metabolic changes in cancer cells upon suppression of MYC. Cancer & metabolism 1:7
Yuneva MO, Fan TW, Allen TD, Higashi RM, Ferraris DV et al (2012) The metabolic profile of tumors depends on both the responsible genetic lesion and tissue type. Cell Metabol 15:157–170
Martinez-Outschoorn UE, Peiris-Pages M, Pestell RG, Sotgia F, Lisanti MP (2017) Cancer metabolism: a therapeutic perspective. Nat Rev Clin Oncol 14:11–31
Ezberci F, Unal E (2018) Aesculus Hippocastanum (Aescin, Horse Chestnut) in the Management of Hemorrhoidal Disease. Turk J Colorectal Dis 28:54–57
Raafat M, Kamel AA, Shehata AH, Ahmed AF, Bayoumi AMA et al (2022) Aescin Protects against Experimental Benign Prostatic Hyperplasia and Preserves Prostate Histomorphology in Rats via Suppression of Inflammatory Cytokines and COX-2. Pharmaceuticals 15
Pittler MH, Ernst E (2012) Horse chestnut seed extract for chronic venous insufficiency. Cochrane Database Syst Rev 11:CD003230
Gallelli L (2019) Escin: a review of its anti-edematous, anti-inflammatory, and venotonic properties. Drug Des Devel Ther 13:3425–3437
Yuan S-Y, Cheng C-L, Wang S-S, Ho H-C, Chiu K-Y et al (2017) Escin induces apoptosis in human renal cancer cells through G2/M arrest and reactive oxygen species-modulated mitochondrial pathways. Oncol Rep 37:1002–1010
Mojžišová G, Kello M, Pilátová M, Tomečková V, Vašková J et al (2016) Antiproliferative effect of β-escin-an in vitro study. Acta Biochim Pol 63:79–87
Zhang Z, Gao J, Cai X, Zhao Y, Wang Y et al (2011) Escin sodium induces apoptosis of human acute leukemia Jurkat T cells. Phytother Res 25:1747–1755
Niu Y-P, Li L-D, Wu L-M (2008) Beta-aescin: a potent natural inhibitor of proliferation and inducer of apoptosis in human chronic myeloid leukemia K562 cells in vitro. Leuk Lymphoma 49:1384–1391
Çiftçi GA, Işcan A, Kutlu M (2015) Escin reduces cell proliferation and induces apoptosis on glioma and lung adenocarcinoma cell lines. Cytotechnology 67:893–904
Wang Z, Chen Q, Li B, Xie JM, Yang XD et al (2018) Escin-induced DNA damage promotes escin-induced apoptosis in human colorectal cancer cells via p62 regulation of the ATM/gammaH2AX pathway. Acta Pharmacol Sin 39:1645–1660
Zhu J, Yu W, Liu B, Wang Y, Shao J et al (2017) Escin induces caspase-dependent apoptosis and autophagy through the ROS/p38 MAPK signalling pathway in human osteosarcoma cells in vitro and in vivo. Cell Death Dis 8:e3113
Wang YW, Wang SJ, Zhou YN, Pan SH, Sun B (2012) Escin augments the efficacy of gemcitabine through down-regulation of nuclear factor-kappaB and nuclear factor-kappaB-regulated gene products in pancreatic cancer both in vitro and in vivo. J Cancer Res Clin Oncol 138:785–797
Tan SM, Li F, Rajendran P, Kumar AP, Hui KM, Sethi G (2010) Identification of beta-escin as a novel inhibitor of signal transducer and activator of transcription 3/Janus-activated kinase 2 signaling pathway that suppresses proliferation and induces apoptosis in human hepatocellular carcinoma cells. J Pharmacol Exp Ther 334:285–293
Dang CV, Le A, Gao P (2009) MYC-induced cancer cell energy metabolism and therapeutic opportunities. Clin cancer research: official J Am Association Cancer Res 15:6479–6483
Liu W, Le A, Hancock C, Lane AN, Dang CV et al (2012) Reprogramming of proline and glutamine metabolism contributes to the proliferative and metabolic responses regulated by oncogenic transcription factor c-MYC. Proc Natl Acad Sci USA 109:8983–8988
Hamurcu Z, Delibasi N, Gecene S, Sener EF, Donmez-Altuntas H et al (2018) Targeting LC3 and Beclin-1 autophagy genes suppresses proliferation, survival, migration and invasion by inhibition of Cyclin-D1 and uPAR/Integrin beta1/ Src signaling in triple negative breast cancer cells. J Cancer Res Clin Oncol 144:415–430
Hamurcu Z, Delibasi N, Nalbantoglu U, Sener EF, Nurdinov N et al (2019) FOXM1 plays a role in autophagy by transcriptionally regulating Beclin-1 and LC3 genes in human triple-negative breast cancer cells. J Mol Med 97:491–508
Unal TD, Hamurcu Z, Delibasi N, Cinar V, Guler A et al (2021) Thymoquinone Inhibits Proliferation and Migration of MDA-MB-231 Triple Negative Breast Cancer Cells by Suppressing Autophagy, Beclin-1 and LC3. Anticancer Agents Med Chem 21:355–364
Deberardinis RJ, Sayed N, Ditsworth D, Thompson CB (2008) Brick by brick: metabolism and tumor cell growth. Curr Opin Genet Dev 18:54–61
Chang CF, Diers AR, Hogg N (2015) Cancer cell metabolism and the modulating effects of nitric oxide. Free Radic Biol Med 79:324–336
Timmerman LA, Holton T, Yuneva M, Louie RJ, Padro M et al (2013) Glutamine sensitivity analysis identifies the xCT antiporter as a common triple-negative breast tumor therapeutic target. Cancer Cell 24:450–465
Wang Y, Xu X, Zhao P, Tong B, Wei Z, Dai Y (2016) Escin Ia suppresses the metastasis of triple-negative breast cancer by inhibiting epithelial-mesenchymal transition via down-regulating LOXL2 expression. Oncotarget 7:23684–23699
Kwak H, An H, Alam MB, Choi WS, Lee SY, Lee SH (2018) Inhibition of Migration and Invasion in Melanoma Cells by beta-Escin via the ERK/NF-kappaB Signaling Pathway. Biol Pharm Bull 41:1606–1610
Kenny HA, Hart PC, Kordylewicz K, Lal M, Shen M et al (2021) The Natural Product beta-Escin Targets Cancer and Stromal Cells of the Tumor Microenvironment to Inhibit Ovarian Cancer Metastasis. Cancers 13
Omi K, Matsuo Y, Ueda G, Aoyama Y, Kato T et al (2021) Escin inhibits angiogenesis by suppressing interleukin8 and vascular endothelial growth factor production by blocking nuclear factor kappaB activation in pancreatic cancer cell lines. Oncology reports 45
Paneerselvam C, Ganapasam S (2020) beta-Escin alleviates cobalt chloride-induced hypoxia-mediated apoptotic resistance and invasion via ROS-dependent HIF-1alpha/TGF-beta/MMPs in A549 cells. Toxicol Res 9:191–201
Huang GL, Shen DY, Cai CF, Zhang QY, Ren HY, Chen QX (2015) beta-escin reverses multidrug resistance through inhibition of the GSK3beta/beta-catenin pathway in cholangiocarcinoma. World J Gastroenterol 21:1148–1157
van Geldermalsen M, Wang Q, Nagarajah R, Marshall AD, Thoeng A et al (2016) ASCT2/SLC1A5 controls glutamine uptake and tumour growth in triple-negative basal-like breast cancer. Oncogene 35:3201–3208
Acknowledgements
This work was financially supported by the Scientific and Technological Research Council of Turkey (TUBITAK). Research Grant (Grant number: 119S227).
Author information
Authors and Affiliations
Contributions
All authors contributed equally to this work.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest or other disclosures to report.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
AKAR, S., DONMEZ-ALTUNTAS, H. & HAMURCU, Z. β-Escin reduces cancer progression in aggressive MDA-MB-231 cells by inhibiting glutamine metabolism through downregulation of c-myc oncogene. Mol Biol Rep 49, 7409–7415 (2022). https://doi.org/10.1007/s11033-022-07536-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07536-5