Abstract
The objective of the current study is to investigate whether ginsenoside Rb1, a major pharmacological extract of ginseng that could attenuate myocardial ischemia reperfusion (MI/R) injury in non-diabetic myocardium, can attenuate MI/R injury in diabetes that are more vulnerable to ischemic insult. Rats were divided into seven groups: (i) diabetic sham, (ii) diabetic, (iii) normal, (iv) diabetic + ginsenoside Rb1, (v) diabetic + wortmannin, (vi) diabetic + wortmannin + ginsenoside Rb1, (vii) diabetic sham + wortmannin. Ginsenoside Rb1 and/or wortmannin were administered prior to inducing MI/R (30 min of coronary artery occlusion followed by 120 min reperfusion). At the end of the experiment, postischemic myocardial infarct size was significantly higher in the diabetic untreated group as compared to normal (P < 0.05), accompanied with increased myocardial apoptosis, elevated plasma CK-MB and LDH release and reduced blood pressure. Ginsenoside Rb1 reduced infarct size, cardiomyocyte apoptosis and caspase-3 activity compared to the diabetic group. The cardioprotective effects of ginsenoside Rb1 were cancelled by wortmannin. Ginsenoside Rb1 significantly upregulated phosphorylated Akt expression, which was attenuated by wortmannin. Ginsenoside Rb1 exerts cardioprotective effects against MI/R injury in diabetic rats, which is partly through activation of phosphatidylinositol 3-kinase (PI3 K)/Akt pathway. Thus this study shows a novel pharmacological preconditioning with ginsenoside Rb1 in the diabetic myocardium.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease is the leading cause of death in patients with diabetes [1]. The mortality rate in diabetic patients with acute coronary syndromes is higher than their nondiabetic counterparts [2]. As diabetic population is expected to double by the year 2030 worldwide, the burden of cardiovascular disease attributable to epidemic of diabetes will be increasing [3, 4].
Diabetes mellitus has deleterious effects not only on cellular integrity and functions but also on signal transductions [5]. Some pharmacological agents can reduce myocardial injury in nondiabetic animal models but their cardio protective effects were abrogated in diabetic animal models. The potential mechanism of how diabetes abrogates cardio protection is unclear [6, 7].
Ginseng as an important herbal drug has been worldwide used in oriental countries for thousands of years and is also one of the most extensively botanical products used in the Western society [8–10]. Ginsenosides, the triterpene saponins, is one of the major components of ginseng [11, 12]. Today more than 30 kinds of ginsenosides have been identified [13]. Ginsenoside Rb1, the major pharmacological extracts (accounting for 0.37–0.5% of ginseng), possesses a variety of biological activities in the cardiovascular, endocrine, immune, and central nervous systems [14–16].
Ginsenoside Rb1 preconditioning has been shown to limit myocardial ischemia reperfusion (MI/R) injury in rat hearts via a mechanism involving the phosphatidylinositol 3-kinase (PI3 K)–Akt signaling cascade [17]. Given that PI3 K–Akt signaling plays an important role in cardio protection mediated by a variety of treatment interventions and that hyperglycemia alters PI3 K–Akt signaling, it is necessary to study whether ginsenoside Rb1 can also afford similar cardio protection in hearts from diabetic subjects.
In the present study, we therefore examined the cardio protective effects of ginsenoside Rb1 against ischemia/reperfusion injury on streptozotocin (STZ)-induced diabetic rats and explored the underlying mechanism.
Materials and methods
Experimental animals
Male Sprague–Dawley rats weighing 250–300 g were purchased from Tongji Medical School, Huazhong University of Science and Technology (HUST), China. All rats were housed maintained under standard laboratory conditions at 22–24°C, relative humidity of 50 ± 15%, and kept on a 12-h:12-h light–dark cycle. All animals had free access to standard rat chow and water. The experimental protocol used in this study was reviewed and approved by the Animal Care and Use Committee of HUST, and in accordance with the Guide for the Care and Use of Laboratory Animals by the National Institutes of Health (NIH Publication No. 80-23).
Chemicals
STZ, triphenyl tetrazolium chloride (TTC) and Evans blue (EB) were purchased from Sigma (St Louis, MO, USA). Ginsenoside Rb1 (purity >98%) was purchased from the National Institute for the Control of Pharmaceutical and Biological Products (Beijing, China).
Induction of diabetes
Experimental diabetes was induced in the animals by a single intraperitoneal administration of STZ dissolved in 0.1 mol/L citrate buffer (pH 4.5) at a dose of 65 mg/kg. Normal rats received an equal volume of citrate buffer. Three days post-STZ injection, tail vein blood glucose samples were collected and measured with Onetouch glucometer (Johnson & Johnson, USA). The rats were considered diabetic and used for the study only if their glucose levels were greater than 15 mmol/L [18]. Rats were housed 8 weeks after vehicle or STZ injection.
Experimental protocol
Rats were randomly divided into seven groups: (1) diabetic rats subjected to sham MI/R (Dia Sham); (2) diabetic rats subjected to MI/R without treatment (Dia I/R); (3) normal rats subjected to MI/R without treatment (Nor I/R); (4) diabetic rats subjected to MI/R and treated with ginsenoside Rb1 at doses of 40 mg/kg (Dia I/R + Rb1); (5) diabetic groups subjected to MI/R and treated with wortmannin (Dia I/R + Wor); (6) diabetic groups subjected to MI/R and treated with wortmannin and ginsenoside Rb1 (Dia I/R + Wor + Rb1); (7) diabetic rats subjected to sham MI/R and treated with wortmannin (Dia Sham + Wor). All groups were subjected to ischemia–reperfusion except group 1 and 7. Wortmannin (15 ug/kg) [19] was administered 20 min before coronary ischemia and reperfusion, 10 min before the administration of ginsenoside Rb1 (40 mg/kg). Rats in groups without treatment received vehicle (normal saline, 3 mL) injected into the left femoral vein 10 min before coronary ischemia and reperfusion. The dose of ginsenoside Rb1 was chosen based on previous studies which have demonstrated that ginsenoside Rb1 attenuates I/R injury in rats [17, 20]. The time course of the experiments is depicted in Fig. 1.
Surgical preparation
Animals were anesthetized intraperitoneally with pentobarbital sodium (50 mg/kg) [21] followed by a tracheotomy and an artificial ventilation. Blood pressure was recorded from the left femoral artery using a pressure transducer with heart rate monitored by an electrocardiogram (ECG) throughout the procedure. The left femoral vein was cannulated for administration of drugs. A fourth-intercostal space thoracotomy was performed, and the pericardium was excised to expose the heart. The left anterior descending coronary artery (LAD) was ligated 2 mm above the left auricle by a 6–0 silk suture. A small polypropylene tube was placed between the ligature and the LAD. The artery was occluded for 30 min by tightening the ligature. After 30 min ischemia, the ligature was loosened to allow reperfusion for 2 h. The sham group underwent the same surgical procedures, apart from tying the 6–0 silk suture. After 2 h reperfusion rats were killed, and parts of the anterior wall of the left ventricular myocardium near the cardiac apex and blood samples were obtained for further analysis.
Plasma creatine kinase isoenzyme MB and lactate dehydrogenase assay
Blood samples were collected at the end of reperfusion and centrifuged at 3,000 rpm, for 10 min at 4°C. Serum was separated and stored at –20°C. Two specific marker enzymes, including the creatine kinase isoenzyme MB (CK-MB), and lactate dehydrogenase (LDH), were measured by using commercial kits (Beijing Kemeidongya Biotechnology Ltd., China). All these marker enzymes were expressed as U/L.
Determination of infarct size
In each group six rats were sacrificed for the assessment of infarct area (IA) and area at risk (AAR). At the end of the 2 h reperfusion period, the rats were given heparin (1U/g), then the ligature around the coronary artery was retied again and 2 mL of 2% Evans blue dye was injected into the left femoral vein. The presence of Evans blue was used to identify the area that was not subjected to the ischemia. Rat hearts were rapidly excised and frozen at –20°C, and then sliced into 2 mm thick sections parallel to the atrioventricular groove using a heart slice chamber. The slices were incubated in 1% TTC in pH 7.4 buffer for 15 min at 37°C. The viable tissue was stained red by TTC while the infarct portion not taking up TTC stain remained pale. Morphometric measurements of the AAR and IA in each slice were performed with a scanner (Epson, v30, Japan) and an image analysis system (Image-Pro plus 3.0; Media Cybernetics, Silver Spring, MD). The percentage of ratios of AAR versus left ventricle (LV) (AAR/LV) and IA versus AAR (IA/AAR) were calculated.
Caspase-3 activity assay
Cardiac caspase-3 activity was measured by using caspase-3 activity assay kits (Beyotime institute of biotechnology, Shanghai, China). Myocardial tissue from risk area was homogenized in ice-cold lysis buffer. The homogenates were centrifuged for 15 min at 16,000 rpm at 4°C. Supernatants were collected and protein concentrations were measured by bicinchoninic acid method. A volume of 10 μL of protein were incubated with 10 μL caspase-3 substrate acetyl-Asp-Glu-Val-Asp p-nitroanilide (AcDEVD-pNA) at 37°C for 1.5 h. The colorimetric release of pNA (p-nitroaniline) from the AcDEVD-pNA substrate was record at 405 nm. Caspase-3 activity was expressed as the fold of enzyme activity compared to that of sham tissue.
Determination of myocardial apoptosis
A TUNEL assay was used to assess myocardial apoptosis with an apoptosis detection kit (Roche, Basel, Switzerland). After reperfusion, the heart was quickly removed and incubated with 4% paraformaldehyde overnight at room temperature. The sections were treated according to the protocol provided by the manufacturer. For each slide ten fields were randomly chosen, TUNEL-positive cells displayed brown staining within the nucleus of apoptotic cells. Apoptotic cells were quantified under high-power magnification by an investigator in a blinded manner and apoptotic index was calculated (i.e., number of apoptotic myocytes/total number of myocytes counted × 100).
Western blot analysis
Myocardial phosphorylated-Akt (p-Akt) and total Akt protein expression were determined by western blot analysis. At the completion of 2 h reperfusion, part of the myocardial tissue was sampled (100 mg) and homogenized with 1,000 µL lysis buffer. The lysates was centrifuged at 10,000 rpm at 4°C for 15 min; equivalent amounts (50 µg/lane) of protein extracts were separated by electrophoresis on a 10% SDS gels and transferred onto a nitrocellulose membrane. The membrane was blocked with 5% fat free dry milk in TBST buffer and then incubated with the rabbit monoclonal anti-phospho Akt (at Ser473) (1:2,000; Cell Signaling Technology, Beverly, MA) diluted in 5% w/v Bovine Serum Albumin (BSA), and the rabbit monoclonal anti-Akt (1:1,000; Cell Signaling Technology, Beverly, MA) diluted in 5% w/v BSA overnight at 4°C, respectively. After washing with TBST buffer three times, the membrane was incubated with appropriate HRP-conjugated secondary antibody (1:2,000; Cell Signaling Technology, Beverly, MA) 1 h at room temperature followed by additional washing. The protein bands were visualized with the use of enhanced chemiluminescence system (ECL kit; Pierce Biotechnology Inc, Rockford, IL). The intensities of each band were analysis with Quantity one software (Bio-Rad, Hercules, CA).
Statistical analysis
All data were presented as means ± SEM. Difference between groups were determined by using one-way or two-way ANOVA analysis for repeated measurement followed by Bonferroni’s post hoc test. Analysis was performed with GraphPad Prism version 5.0 for Windows (GraphPad Software, San Diego California USA) and values of P < 0.05 were considered statistically significant.
Results
Effect of ginsenoside Rb1 on systemic hemodynamics
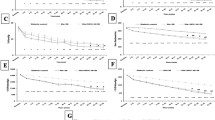
The serial changes in heart rate (HR), mean arterial pressure (MAP) and rate pressure product (RPP) during the experiments were demonstrated in Fig. 2. At baseline, HR and MAP in diabetic groups were lower than those in the nondiabetic group. Accordingly, RPP was lower in those groups. There were no obvious differences among diabetic groups. The values of MAP, HR and RPP were significantly decreased in each groups after ischemia as compared to the baseline values and recovered gradually after reperfusion. At the end of 2 h reperfusion, MAP in Dia I/R + Rb1 group was higher than that in the diabetic untreated group and the wortmannin treated groups. Pretreated with wortmannin markedly blocked ginsenoside Rb1-mediated improvement in cardiac function as evidenced by 20.6% reduction of RPP compared to Dia I/R + Rb1 group (P < 0.05), while wortmannin itself had no effect on hemodynamic parameters in diabetic rats.
a–c Effect of ginsenoside Rb1 on heart rate (HR), mean arterial pressure (MAP), rate-pressure product (RPP) before and during myocardial I/R. Results are expressed as mean ± SEM. Dia diabetic, I/R ischemia/reperfusion, Nor normal, Rb1 ginsenoside Rb1, Wor wortmannin (n = 12, *P < 0.05 vs. Dia I/R group, #P < 0.05 vs. Nor I/R group)
Effects of ginsenoside Rb1 on biochemical markers cellular injury
To examine whether ginsenoside Rb1 altered damage of cardiomyocyte induced by MI/R, the activities of the cardiac enzyme LDH and CK-MB as indices of myocardial cellular injury were measured at the end of reperfusion in different groups. Comparing with diabetic sham group, I/R caused a significant increase in LDH and CK-MB in diabetic I/R group. The damage evoked by I/R were further enhanced in diabetic I/R group comparing with nondiabetic I/R group (both P < 0.05). After pretreatment with ginsenoside Rb1 at a dose of 40 mg/kg, the enzyme levels were found to be attenuated (both P < 0.05 vs. Dia I/R group). Of interest, administration with the PI3 K inhibitor wortmannin partly inhibited ginsenoside Rb1-elicited decrease of LDH and CK-MB to achieve the same level as Dia I/R group (Fig. 3). These results suggest that ginsenoside Rb1 protects the diabetic heart against I/R-induced myocardial injury through activating PI3 K pathway.
Changes of LDH, CK-MB activities after 30 min of myocardial ischemia and 2 h of reperfusion in different experimental groups. Dia diabetic, I/R ischemia/reperfusion, Nor normal, Rb1 ginsenoside Rb1, Wor wortmannin. Results are expressed as mean ± SEM (n = 8, *P < 0.05 vs. Dia I/R group, # P < 0.05 vs. Nor I/R group, $ P < 0.05 vs. Dia I/R + Rb1 group)
Effect of ginsenoside Rb1 on myocardial infarct size
The representative images of AAR and IA from each group were shown in Fig. 4, which expressed as percentage of AAR/LV and IA/AAR. There was no significant difference in area at risk as a percentage to left ventricle (Fig. 4a). Diabetes increased I/R-induced cardiac infarction (51.3 ± 1.7%) compared to nondiabetic group (40.3 ± 1.4%). The infarct size was lower in the Dia I/R + Rb1 group (42.3 ± 2.9%) compared to all other diabetic groups (both P < 0.05). Wortmannin per se did not have significant effect on Dia I/R + Wor rats in infarct size compared with that in Dia I/R group (P > 0.05 vs. Dia I/R). However, wortmannin significantly inhibited ginsenoside Rb1-elicited reduction in infarct size (P < 0.05 vs. Dia I/R + Rb1). This indicates that wortmannin attenuated the protective action of ginsenoside Rb1 against I/R-induced cardiac damage in diabetic rats.
a Area at risk expressed as percent of left ventricle, b infarct size expressed as percent of the area at risk in rats subjected to 30 min ischemia and 2 h of reperfusion. AAR area at risk, LV left ventricle, IA infarct area, Dia diabetic, I/R ischemia/reperfusion, Nor normal, Rb1 ginsenoside Rb1, Wor wortmannin. Results are expressed as mean ± SEM (n = 6, *P < 0.05 vs. Dia I/R group, #P < 0.05 vs. Nor I/R group, $P < 0.05 vs. Dia I/R + Rb1 group)
Effect of ginsenoside Rb1 on cardiomyocyte apoptosis
TUNEL and caspase-3 activity assays were used to evaluate the anti-apoptotic effect of ginsenoside Rb1. Myocardial I/R significantly increased TUNEL-positive cells in both the diabetic and non-diabetic rat hearts (all P < 0.05 vs. sham). Rb1 treatment reduced TUNEL-positive cells in hearts subjected to MI/R (19.6 ± 0.6% in Dia I/R + Rb1 vs. 23.4 ± 0.7% in Dia I/R P < 0.05, Fig. 5).
Representative photomicrographs of TUNEL staining from sham-operated rats or from rats subjected to 30 min of myocardial ischemia and 2 h of reperfusion (×400). Dia diabetic, I/R ischemia/reperfusion, Nor normal, Rb1 ginsenoside Rb1, Wor wortmannin. Results are expressed as mean ± SEM (n = 4, *P < 0.05 vs. Dia I/R group, # P < 0.05 vs. Nor I/R group, $ P < 0.05 vs. Dia I/R + Rb1 group)
Caspase-3 activity in the Dia I/R group was higher compared with the sham-operated group (P < 0.05). Ginsenoside Rb1 attenuated the increase of caspase-3 activity compared with that in the Dia I/R group (P < 0.05, Dia I/R + Rb1 vs. Dia I/R) (Fig. 6).
Effect of ginsenoside Rb1 on myocardial caspase-3 activity after 30 min of myocardial ischemia and 2 h of reperfusion. Dia diabetic, I/R ischemia/reperfusion, Nor normal, Rb1 ginsenoside Rb1, Wor wortmannin. Results are expressed as mean ± SEM (n = 6, *P < 0.05 vs. Dia I/R group, # P < 0.05 vs. Nor I/R group, $ P < 0.05 vs. Dia I/R + Rb1 group)
Pretreatment with wortmannin reverted the effects of Rb1 in reducing TUNEL-positive cells and caspase-3 activity (P > 0.05, Dia I/R vs. Dia I/R + Wor + Rb1 group).
Effect of ginsenoside Rb1 on Akt phosphorylation
Myocardial Akt and phosphorylated Akt expression were examined by western blot in diabetic and nondiabetic rats. As showed in Fig. 7, there were no noticeable differences in the expression of total Akt in diabetic and nondiabetic groups. Diabetes reduced the expression of p-Akt protein in Dia I/R group compared with age matched Nor I/R group (P < 0.05, Nor I/R vs. Dia I/R group). The p-Akt level was markedly increased in the ginsenoside Rb1 treated group compared to diabetic groups (P < 0.05, Dia I/R + Rb1 vs. Dia I/R). Ginsenoside Rb1 failed to promote the raise of p-Akt in diabetic rats in the presence of wortmannin pretreatment.
Representative Western blot showing the effect of ginsenoside Rb1 on total and phosphorylated Akt after myocardial I/R. Dia diabetic, I/R ischemia/reperfusion, Nor normal, Rb1 ginsenoside Rb1, Wor wortmannin. Data obtained from quantitative densitometry were presented as mean ± SEM (n = 6, *P < 0.05 vs. Dia I/R group, # P < 0.05 vs. Nor I/R group, $ P < 0.05 vs. Dia I/R + Rb1 group)
Discussion
The main findings of this study are as following: despite the impaired PI3 K/Akt signaling STZ-induced diabetic rat heart, pretreatment with ginsenoside Rb1 was able to enhance Akt phosphorylation in the circumstance of myocardial I/R, and reduce postischemic myocardial infract size and myocardial apoptosis. Further, PI3 K inhibition with wortmannin reverted the cardio protective effects of ginsenoside Rb1, which is indicative that ginsenoside Rb1 confers its cardio protection via PI3 K/Akt signaling in the diabetic hearts.
Recent studies have shown that STZ-induced diabetes mellitus significantly aggravated myocardial I/R injury and the protective effects of ischemic preconditioning (IPC) were blunted [6, 7, 22]. As preconditioning plays a role through a number of signaling pathways, cardio protective effect in diabetes mellitus might be reduced due to impairment in cardio protective signaling pathways such as the PI3 K/Akt pathway [7, 23]. In our study, levels of p-Akt was significantly lower in Dia I/R than in the Nor I/R group, confirming an impairment of PI3 K/Akt signaling in the diabetic hearts following MI/R. Of note, ginsenoside Rb1 enhanced postischemic myocardial levels of p-Akt expression, which might be the major mechanism whereby ginsenoside Rb1 reduced myocardial infarct size and apoptotic cell death.
It is well known that cardiomyocyte damage subsequent to myocardial ischemia and reperfusion can cause a reduction in cardiac function. Ginsenoside Rb1 has been shown to improve cardiac function and raise the survival rate in transgenic mouse suffering from dilated cardiomyopathy [16]. It remains to be determined whether ginsenoside Rb1 can reverse some functional changes brought about by myocardial ischemia in diabetics. In this study, ginsenoside Rb1 treatment resulted in improvement of number of hemodynamic parameters including MAP, HR and RPP at the end of reperfusion. This is an indirect indicator of improved cardiac function. The results in our present study have clearly shown that ginsenoside Rb1 treatment exerts cardio protective effects for diabetic myocardial I/R animals. It has been established that activation of PI3 K/Akt plays an important protective role in myocardial I/R injury [23–25].
To gain insight into the potential mechanisms responsible for ginsenoside Rb1-elicited cardio protection against I/R-induced apoptosis, we further evaluated the role of PI3 K-Akt pathway in ginsenoside Rb1 mediated cardio protection. Our results showed that there were significant increases of p-Akt after reperfusion in the myocardium of ginsenoside Rb1 treated rats. More importantly, pretreatment with wortmannin, a PI3 K inhibitor, blocked Akt phosphorylation and abolished ginsenoside Rb1-cardioprotective effects. Wortmannin reverted the effects of ginsenoside Rb1 in reducing myocardial infarct size and apoptosis as well as in lowering plasma CK-MB and LDH, biochemical markers of myocardial cellular injury. These results indicate that PI3 K-Akt signaling contributes to ginsenoside Rb1-elicited cardio protection against MI/R injury in diabetic rats.
There are many reports dealing with ginseng’s protective effects on the cardiovascular system. Previous studies have shown that ginsenoside Rb1 resembles estrogen structure and is a functional ligand for estrogen receptor (ER) [13, 26]. It is generally agreed that activation of ER can exert protective effects through the activation of a number of signaling pathways such as PI3 K and mitogen-activated protein kinase (MAPK) [27–29]. Recently, Hwang et al. demonstrated that ginsenoside Rb1 directly activates the PI3 K/Akt pathway after binding to ER in vitro [30]. Therefore, it seems plausible to postulate that ginsenoside Rb1 might bind to the ER and then activate PI3 K/Akt pathway in diabetic rats. This hypothesis needs to be tested both in vivo and in vitro in future studies.
The PI3 K-Akt pathway affects cell survival by a variety of substrates, including apoptotic proteins, endothelial nitric oxide synthase (eNOS) and protein kinase C [31–33]. Scott et al. showed that ginsenosides increased nitric oxide (NO) production in cardiomyocyte [34]. NO produced from eNOS has been implicated as an important mediator of protection in myocardial I/R injury [35, 36]. These reports suggest PI3 K–Akt–eNOS plays an important role in ginsenoside Rb1-elicited cardio protection. Therefore, further investigations are necessary to confirm downstream mechanisms of PI3 K-Akt pathway, such as the eNOS and the antiapoptotic effect.
In conclusion, our present study indicates treatment with ginsenoside Rb1 reduces cardiomyocyte apoptosis, and alleviates cardiac dysfunction following MI/R in diabetic heart. Ginsenoside Rb1 may be an ideal agent for diabetic patients present with an acute myocardial infarction.
References
Trichon BH, Roe MT (2004) Acute coronary syndromes and diabetes mellitus. Diab Vasc Dis Res 1:23–32
Paulson DJ (1997) The diabetic heart is more sensitive to ischemic injury. Cardiovasc Res 34:104–112
Donahoe SM, Stewart GC, McCabe CH, Mohanavelu S, Murphy SA, Cannon CP, Antman EM (2007) Diabetes and mortality following acute coronary syndromes. JAMA 298:765–775
Wild S, Roglic G, Green A, Sicree R, King H (2004) Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 27:1047–1053
Zdychova J, Komers R (2005) Emerging role of Akt kinase/protein kinase B signaling in pathophysiology of diabetes and its complications. Physiol Res 54:1–16
Gross ER, Hsu AK, Gross GJ (2007) Diabetes abolishes morphine-induced cardioprotection via multiple pathways upstream of glycogen synthase kinase-3beta. Diabetes 56:127–136
Tanaka K, Kehl F, Gu W, Krolikowski JG, Pagel PS, Warltier DC, Kersten JR (2002) Isoflurane-induced preconditioning is attenuated by diabetes. Am J Physiol Heart Circ Physiol 282:H2018–H2023
Sengupta S, Toh SA, Sellers LA, Skepper JN, Koolwijk P, Leung HW, Yeung HW, Wong RN, Sasisekharan R, Fan TP (2004) Modulating angiogenesis: the yin and the yang in ginseng. Circulation 110:1219–1225
Yu J, Eto M, Akishita M, Kaneko A, Ouchi Y, Okabe T (2007) Signaling pathway of nitric oxide production induced by ginsenoside Rb1 in human aortic endothelial cells: a possible involvement of androgen receptor. Biochem Biophys Res Commun 353:764–769
Wang YL, Wang CY, Zhang BJ, Zhang ZZ (2009) Shenfu injection suppresses apoptosis by regulation of Bcl-2 and caspase-3 during hypoxia/reoxygenation in neonatal rat cardiomyocytes in vitro. Mol Biol Rep 36:365–370
Xia ZY, Liu XY, Zhan LY, He YH, Luo T, Xia Z (2005) Ginsenosides compound (shen-fu) attenuates gastrointestinal injury and inhibits inflammatory response after cardiopulmonary bypass in patients with congenital heart disease. J Thorac Cardiovasc Surg 130:258–264
Zhu S, Zou K, Fushimi H, Cai S, Komatsu K (2004) Comparative study on triterpene saponins of Ginseng drugs. Planta Med 70:666–677
Leung KW, Cheung LW, Pon YL, Wong RN, Mak NK, Fan TP, Au SC, Tombran-Tink J, Wong AS (2007) Ginsenoside Rb1 inhibits tube-like structure formation of endothelial cells by regulating pigment epithelium-derived factor through the oestrogen beta receptor. Br J Pharmacol 152:207–215
Zhang QH, Wu CF, Duan L, Yang JY (2008) Protective effects of total saponins from stem and leaf of Panax ginseng against cyclophosphamide-induced genotoxicity and apoptosis in mouse bone marrow cells and peripheral lymphocyte cells. Food Chem Toxicol 46:293–302
Shang W, Yang Y, Zhou L, Jiang B, Jin H, Chen M (2008) Ginsenoside Rb1 stimulates glucose uptake through insulin-like signaling pathway in 3T3–L1 adipocytes. J Endocrinol 198:561–569
Zhao H, Lv D, Zhang W, Dong W, Feng J, Xiang Z, Huang L, Qin C, Zhang L (2010) Ginsenoside-Rb1 attenuates dilated cardiomyopathy in cTnT(R141 W) transgenic mouse. J Pharmacol Sci 112:214–222
Wang Z, Li M, Wu WK, Tan HM, Geng DF (2008) Ginsenoside Rb1 preconditioning protects against myocardial infarction after regional ischemia and reperfusion by activation of phosphatidylinositol-3-kinase signal transduction. Cardiovasc Drugs Ther 22:443–452
Xia Z, Kuo KH, Nagareddy PR, Wang F, Guo Z, Guo T, Jiang J, McNeill JH (2007) N-acetylcysteine attenuates PKCbeta2 overexpression and myocardial hypertrophy in streptozotocin-induced diabetic rats. Cardiovasc Res 73:770–782
Shinohara T, Takahashi N, Ooie T, Hara M, Shigematsu S, Nakagawa M, Yonemochi H, Saikawa T, Yoshimatsu H (2006) Phosphatidylinositol 3-kinase-dependent activation of akt, an essential signal for hyperthermia-induced heat-shock protein 72, is attenuated in streptozotocin-induced diabetic heart. Diabetes 55:1307–1315
Wang J, Qiao L, Li Y, Yang G (2008) Ginsenoside Rb1 attenuates intestinal ischemia-reperfusion-induced liver injury by inhibiting NF-kappaB activation. Exp Mol Med 40:686–698
Yang J, Yang J, Ding JW, Chen LH, Wang YL, Li S, Wu H (2008) Sequential expression of TLR4 and its effects on the myocardium of rats with myocardial ischemia-reperfusion injury. Inflammation 31:304–312
Hotta H, Miura T, Miki T, Togashi N, Maeda T, Kim SJ, Tanno M, Yano T, Kuno A, Itoh T, Satoh T, Terashima Y, Ishikawa S, Shimamoto K (2010) Angiotensin II type 1 receptor-mediated upregulation of calcineurin activity underlies impairment of cardioprotective signaling in diabetic hearts. Circ Res 106:129–132
Tsang A, Hausenloy DJ, Mocanu MM, Carr RD, Yellon DM (2005) Preconditioning the diabetic heart: the importance of Akt phosphorylation. Diabetes 54:2360–2364
Hausenloy DJ, Yellon DM (2006) Survival kinases in ischemic preconditioning and postconditioning. Cardiovasc Res 70:240–253
Penumathsa SV, Thirunavukkarasu M, Samuel SM, Zhan L, Maulik G, Bagchi M, Bagchi D, Maulik N (2009) Niacin bound chromium treatment induces myocardial Glut-4 translocation and caveolar interaction via Akt, AMPK and eNOS phosphorylation in streptozotocin induced diabetic rats after ischemia-reperfusion injury. Biochim Biophys Acta 1792:39–48
Zhou W, Chai H, Lin PH, Lumsden AB, Yao Q, Chen C (2005) Ginsenoside Rb1 blocks homocysteine-induced endothelial dysfunction in porcine coronary arteries. J Vasc Surg 41:861–868
Lin J, Steenbergen C, Murphy E, Sun J (2009) Estrogen receptor-beta activation results in S-nitrosylation of proteins involved in cardioprotection. Circulation 120:245–254
Hisamoto K, Ohmichi M, Kurachi H, Hayakawa J, Kanda Y, Nishio Y, Adachi K, Tasaka K, Miyoshi E, Fujiwara N, Taniguchi N, Murata Y (2001) Estrogen induces the Akt-dependent activation of endothelial nitric-oxide synthase in vascular endothelial cells. J Biol Chem 276:3459–3467
Simoncini T, Hafezi-Moghadam A, Brazil DP, Ley K, Chin WW, Liao JK (2000) Interaction of oestrogen receptor with the regulatory subunit of phosphatidylinositol-3-OH kinase. Nature 407:538–541
Hwang YP, Jeong HG (2010) Ginsenoside Rb1 protects against 6-hydroxydopamine-induced oxidative stress by increasing heme oxygenase-1 expression through an estrogen receptor-related PI3 K/Akt/Nrf2-dependent pathway in human dopaminergic cells. Toxicol Appl Pharmacol 242:18–28
Gao F, Gao E, Yue TL, Ohlstein EH, Lopez BL, Christopher TA, Ma XL (2002) Nitric oxide mediates the antiapoptotic effect of insulin in myocardial ischemia-reperfusion: the roles of PI3-kinase, Akt, and endothelial nitric oxide synthase phosphorylation. Circulation 105:1497–1502
Hausenloy DJ, Yellon DM (2004) New directions for protecting the heart against ischaemia-reperfusion injury: targeting the reperfusion injury salvage kinase (RISK)-pathway. Cardiovasc Res 61:448–460
Cross TG, Scheel-Toellner D, Henriquez NV, Deacon E, Salmon M, Lord JM (2000) Serine/threonine protein kinases and apoptosis. Exp Cell Res 256:34–41
Scott GI, Colligan PB, Ren BH, Ren J (2001) Ginsenosides Rb1 and Re decrease cardiac contraction in adult rat ventricular myocytes: role of nitric oxide. Br J Pharmacol 134:1159–1165
Schulz R, Kelm M, Heusch G (2004) Nitric oxide in myocardial ischemia/reperfusion injury. Cardiovasc Res 61:402–413
Brunner F, Maier R, Andrew P, Wolkart G, Zechner R, Mayer B (2003) Attenuation of myocardial ischemia/reperfusion injury in mice with myocyte-specific overexpression of endothelial nitric oxide synthase. Cardiovasc Res 57:55–62
Acknowledgments
This work was supported by the National Natural Science Foundation of China (No.30672033).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, Y., Xia, Zy., Dou, J. et al. Protective effect of ginsenoside Rb1 against myocardial ischemia/reperfusion injury in streptozotocin-induced diabetic rats. Mol Biol Rep 38, 4327–4335 (2011). https://doi.org/10.1007/s11033-010-0558-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-010-0558-4