Abstract
We report treatment outcome of eleven patients with pyridoxine-dependent epilepsy caused by pathogenic variants in ALDH7A1 (PDE-ALDH7A1). We developed a clinical severity score to compare phenotype with biochemical features, genotype and delays in the initiation of pyridoxine. Clinical severity score included 1) global developmental delay/ intellectual disability; 2) age of seizure onset prior to pyridoxine; 3) current seizures on treatment. Phenotype scored 1–3 = mild; 4–6 = moderate; and 7–9 = severe. Five patients had mild, four patients had moderate, and two patients had severe phenotype. Phenotype ranged from mild to severe in eight patients (no lysine-restricted diet in the infantile period) with more than 10-fold elevated urine or plasma α-AASA levels. Phenotype ranged from mild to moderate in patients with homozygous truncating variants and from moderate to severe in patients with homozygous missense variants. There was no correlation between severity of the phenotype and the degree of α-AASA elevation in urine or genotype. All patients were on pyridoxine, nine patients were on arginine and five patients were on the lysine-restricted diet. 73% of the patients became seizure free on pyridoxine. 25% of the patients had a mild phenotype on pyridoxine monotherapy. Whereas, 100% of the patients, on the lysine-restricted diet initiated within their first 7 months of life, had a mild phenotype. Early initiation of lysine-restricted diet and/or arginine therapy likely improved neurodevelopmental outcome in young patients with PDE-ALDH7A1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pyridoxine-dependent epilepsy (PDE) (OMIM#266,100) caused by mutations in ALDH7A1 (PDE-ALDH7A1). ALDH7A1 encodes α-aminoadipic-semialdehyde-dehydrogenase (α -AASAD) (EC 1.2.1.31) in the lysine catabolic pathway (Mills et al. 2006). α-AASAD deficiency leads to the accumulation of α-aminoadipic acid semialdehyde (α-AASA) and piperidine 6-carboxylate (P6C), which inactivates pyridoxal-5-phosphate (Mills et al. 2006).
Neonatal or infantile onset refractory seizures are the classical presentation with a dramatic response to pyridoxine (Gospe 2014). In a recent brief communication, 11 patients on pyridoxine monotherapy had normal neurocognitive functions by neuropsychological assessments and 17 patients reported to have normal neurodevelopmental or neurocognitive outcome based on the physician’s subjective assessments (Nasr et al. 2015). Improvements in developmental milestones, cognitive functions and urine and cerebrospinal fluid (CSF) α-AASA levels, sum of AASA and P6C concentrations (AASA-P6C) and urine and plasma pipecolic acid (PA) levels on lysine-restricted diet and/or arginine therapy has been reported in 13 PDE-ALDH7A1 patients (Van Karnebeek et al. 2012; Coughlin et al. 2015; Mahajnah et al. 2016; Yuzyuk et al. 2016). Improvements in cognitive functions and CSF α-AASA levels on arginine was reported in a single PDE-ALDH7A1 patient (Mercimek-Mahmutoglu et al. 2014).
We report treatment outcome of 11 patients with PDE-ALDH7A1 in a retrospective cohort study. We developed a clinical severity score to assess treatment outcome and to compare phenotype and biochemical features and genotype.
Methods
All PDE-ALDH7A1 patients were included. Electronic patient charts were reviewed for clinical features, investigations, neuroimaging and treatment. Institutional Research Ethics Board approved the study (Approval#1000050808).
Clinical severity score
We developed a clinical severity score: A) global developmental delay (GDD) (assessed by physician during their last clinic visit) or intellectual disability (ID) (assessed by psychological assessments): 0 = normal; 1 = mild; 2 = moderate; 3 = severe; B) age of seizure onset prior to pyridoxine: 0 = no seizures; 1 = seizure onset >1 month of age; 2 = seizure onset ≥7 days - < 1 month of age; 3 = seizure onset <7 days of age; C) clinical or electrical seizures on pyridoxine: 0 = no seizures with normal electroencephalography (EEG) on low dose pyridoxine (200 mg/day independent of age and weight of patients); 1 = no seizures with abnormal EEG on low dose pyridoxine (200 mg/day independent of age and weight of patients); 2 = no seizures on high dose pyridoxine (up to 1.5 g/day) and anti-seizure medications with or without normal EEG; 3 = seizures on high dose pyridoxine and anti-seizure medications and/or arginine and/or lysine-restricted diet with or without normal EEG. The sum of all clinical features were given as phenotype, classified as 1–3 = mild; 4–6 = moderate; and 7–9 = severe.
Comparison of phenotype and biochemical features and genotype
Urine, plasma, and CSF α-AASA measurements and molecular genetic investigations were performed in one of the clinical biochemical or molecular genetic laboratories (NM_001182.3) according to their methods. Urine, plasma and CSF α-AASA levels were calculated as an X-fold elevated of normal α-AASA levels. We used the recommendations for mutation nomenclature (www.hgvs.org/mutnomen) to name gene variations.
Treatment outcome
Pyridoxine dose ranged 3–30 mg/kg/day. Pyridoxine dose was increased in patients with ongoing clinical seizures. Lysine-restricted diet was applied and medical formula (Glutarex I, lysine and tryptophan free formula for glutaric aciduria type I diet treatment) was supplemented to prevent protein malnutrition. PDE Consortium Consensus Recommendations were taken as guidelines for the lysine-restricted diet (Van Karnebeek et al. 2014), but modified according to the patients’s tolerance to the medical formula. All patients were supplemented with tryptophan (15–25 mg/kg/day) on the lysine-restricted diet. Arginine dose was 400 mg/kg/day (maximum 15 g/day for patients >40 kg).
Results
Eleven patients (6 males; 5 females) from 9 unrelated families (two affected siblings in two families) were included. Five patients were partially reported (Nasr et al. 2015; Jain-Ghai et al. 2014; Mercimek-Mahmutoglu et al. 2015; Gallagher et al. 2009). The current average age was 8.6 ± 5.62 standard deviation (SD) years (range 7 months-17 years). Demographics, clinical features, brain magnetic resonance imaging (MRI) and EEG results are summarized in Table 1. Biochemical and molecular genetic investigations are summarized in Table 2. All biochemical results were collected on pyridoxine either at the time of initial diagnosis in young patients or at the time of their first clinic visit in older patients seen in our clinic.
Clinical severity score
According to our clinical severity score five patients had mild (in three of them lysine-restricted diet started within their first 7 months of life), four patients had moderate, and two patients had severe phenotype. Seven patients had neonatal onset and 4 patients had infantile onset seizures. The most common seizure type was generalized tonic-clonic seizures. Three patients had myoclonic seizures. Two patients presented with absence seizures. Two patients had complex partial seizures.
Comparison of phenotype and biochemical features and genotype
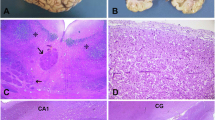
Phenotype compared to urine/plasma α-AASA levels, collected on pyridoxine prior to initiation of lysine-restricted diet or arginine, are depicted in Fig. 1. The highest urine α-AASA was present in a patient with a mild phenotype. Phenotype ranged from mild to severe in all patients with urine or plasma α-AASA levels more than 10-fold elevated of normal. In eight patients with no lysine-restricted diet initiated within their first 7 months of life (except patient ID# 5, 8 and 11) phenotype also ranged from mild to severe with urine or plasma α-AASA levels more than 10-fold elevated of normal (Supplemental Fig. 1). Phenotype compared to CSF α-AASA levels (collected on pyridoxine prior to initiation of lysine-restricted diet) are depicted in Fig. 2.
Clinical severeity score compared to CSF α-AASA levels (collected on pyridoxine prior to initiation of lysine-restricted diet) are depicted in Fig. 2
All patients had likely pathogenic variants (12 known and two novel) identified by direct sequencing in ALDH7A1 (Table 2). None of the novel variants were found in either ESP6500 Exome or dbSNP database as polymorphisms. Missense variants were the most common variant type in 50%. All missense variants involved highly conserved amino acid change across species. Parental testing confirmed carrier status in the parents in all patients except in one father (patient ID# 3). In all patients with novel likely pathogenic variants, urine or plasma α-AASA levels were elevated confirming the pathogenicity. A homozygous missense variant resulted in a moderate phenotype in one and in a severe phenotype in another patient. A mild phenotype in one and a moderate phenotype in another patient caused by a homozygous truncating variant.
Treatment outcome
Treatment of patients are summarized in Table 3. Average duration of follow-up was 6.5 ± 5.3 SD years (range 7 months–17 years). All patients were on pyridoxine (average treatment duration 8.3 ± 5.6 SD years; range 6 months – 16 years). Five patients were on the lysine-restricted diet (average age of initiation 3.51 ± 4.46 SD years; range 1 month–9 years). The average duration of the lysine-restricted diet was 14.2 ± 14 SD months (range 3 months–40 months). Nine patients were on arginine (Table 3), one of those did not comply with treatment due to its unpleasant taste (patient ID# 1).
Eight patients were seizure free on low dose pyridoxine (200 mg/day). Three patients (patient ID# 1, 6,7) had occasional seizures and required high dose pyridoxine and/or anti-seizure medications.
In three out of five patients (patient ID# 5, 8, 11), lysine-restricted diet was started within the first 7 months of life. All these patients had normal cognitive functions and/or neurodevelopment. In one out of five patients with severe phenotype (patient ID# 3), lysine-restricted diet was started at the age of 9 years, who gained vocalization, ability to roll side-to-side and holding her head at one-year of therapy.
Phenotype compared to delays in the initiation of pyridoxine therapy is depicted in Fig. 3. Patient ID# 3 with severe phenotype had a 14-month delay between seizure onset and initiation of pyridoxine. Whereas patient ID# 6 with severe phenotype had her first seizure at the age of three days and on the same day pyridoxine was started. In three patients with moderate phenotype pyridoxine was started between 1 to 6 months after seizure onset.
Psychological assessment results of four patients on the lysine-restricted diet and/or arginine are summarized in Supplemental Table 1. Neurocognitive and/or neurodevelopmental outcomes of three patients on the lysine-restricted diet therapy, initiated within the first 7 months of life, were normal (two of them with age appropriate developmental milestones at the age of 7 and 11 months). Two patients with mild phenotype (patient ID#2 and 4) had normal neurocognitive functions with specific borderline impairments in visual processing speed or verbal memory (reported previously in details in Nasr et al. 2015). Patient ID# 4 showed improvements in general abilities index from 108 to 116 and improvements in verbal and motor functioning at 12th months of arginine therapy reported previously (reported previously in details in Mercimek-Mahmutoglu et al. 2014). Whereas patient 9 demonstrated no improvements in neurocognitive functions on one-year of arginine therapy.
EEG on pyridoxine was normal in seven patients and abnormal in one patient with severe phenotype with no clinical seizures (Table 3). One patient had hemorrhagic changes in the brain MRI (Table 3).
A follow-up urine α-AASA level was available in 4 patients on lysine-restricted diet or arginine therapy and improved between 11 to 87% from the baseline (Table 3). In two patients on arginine therapy, CSF α-AASA decreased between 28 to 57% from baseline. One patient on lysine-restricted diet did not show any improvements in CSF α-AASA levels from the baseline at 7 months of age to 33 months of lysine-restricted diet and arginine therapy (reported previously in details in Mahajnah et al. 2016).
Discussion
We report treatment outcome of 11 PDE-ALDH7A1 patients in a retrospective cohort study from a single Epilepsy Genetics Clinic. All patients had elevated urine α-AASA levels on pyridoxine, which is a good biomarker to identify patients even on long-term pyridoxine. We applied a clinical severity score to compare phenotype with biochemical features and genotype for the first time. In eight patients, who were not treated with lysine-restricted diet in the infantile period, phenotype ranged from mild to severe with moderate to marked elevations of urine or plasma α-AASA levels and the highest urine α-AASA level was present in a patient with a mild phenotype. There seems to be no correlation between the severity of phenotype and degree of urine α-AASA elevation; genotype based on the variant type; and delays in the initiation of pyridoxine. All patients with CSF α-AASA measurements had a mild phenotype. We do not know if higher CSF α-AASA levels would have caused a severe phenotype. It is interesting that only two out of eight patients (25%) had a mild phenotype on pyridoxine monotherapy. Whereas, three patients (100%) on the lysine-restricted diet initiated within their first 7 months of life had a mild phenotype. Therefore, lysine-restricted diet had likely a major impact on their mild phenotype and normal neurodevelopmental outcome. We think that early initiation of lysine-restricted diet and/or arginine therapy improved neurodevelopmental outcome in our small number of patient cohort on different treatment regimens.
Thirteen patients on the lysine-restricted diet and/or arginine showed improvements in developmental milestones or neurodevelopmental outcome, seizures, urine and CSF α-AASA levels, sum of AASA and P6C concentrations (AASA-P6C) and urine and plasma pipecolic acid (PA) levels in limited studies (Van Karnebeek et al. 2012; Coughlin et al. 2015; Mahajnah et al. 2016; Yuzyuk et al. 2016). Asymptomatic mild central nervous system serotonin deficiency was reported in one patient on the strict lysine-restricted diet, which was improved by tryptophan supplementation (Mahajnah et al. 2016). Short-term arginine therapy (one of our current study patients) resulted in improvements in general abilities index and 57% decrease in CSF α-AASA (Mercimek-Mahmutoglu et al. 2014). In our current study, three additional patients on arginine showed no improvements in cognitive functions or general abilities index, but mild improvement in CSF α-AASA level (28% decrease from baseline). It is not clear if the outcome of arginine therapy was compromised by unpleasant taste and compliance problems. More patients, who do not want lysine-restricted diet, should be treated with long-term arginine to assess its effectiveness. An older sibling had moderate GDD within the first 6–12 months of age (6-month delay in the initiation of pyridoxine), whereas his younger sibling, treated with lysine-restricted diet and arginine from the age of 2 months, had normal development at the age of 7 months. In our current study, two of 8 patients (25%) on long-term pyridoxine achieved normal neurocognitive functions with specific borderline impairments in visual processing speed. Whereas, three patients (100%), received lysine-restricted diet within 7 months of their life, had normal neurodevelopmental or neurocognitive functions. Long-term neurodevelopmental outcome of patients treated with lysine-restricted diet and arginine within the first year of life would be necessary to arrive at a decision, if PDE-ALDH7A1 should be included into newborn screening programs in the near future.
Seizure freedom was reported in 71% of PDE-ALDH7A1 patients on pyridoxine (Bok et al. 2012). In our retrospective cohort study, 8 patients (73%) became seizure free on pyridoxine, which is similar to previous report. Three patients with clinical seizures were neither on the lysine-restricted diet despite it was recommended. Only one of those three patients was on arginine with compliance problems. Lysine-restricted diet and/or arginine therapies are likely necessary to achieve better seizure control as well as improve neurodevelopmental outcome in addition to pyridoxine therapy.
Normal EEG with clinical seizures have been rarely reported in patients with PDE-ALDH7A1 prior to pyridoxine therapy (Mikati et al. 1991; Mills et al. 2010; Stockler et al. 2011). In our retrospective cohort study, two patients had a normal initial EEG with clinical seizures. One patient was diagnosed early with PDE-ALDH7A1 due to the positive family history. It is important to note that a normal EEG or no correlation of clinical seizures on EEG do not exclude PDE-ALDH7A1.
Intracerebral or subdural hemorrhages have been reported in few patients with PDE-ALDH7A1 (Bok et al. 2012; Mills et al. 2010; Mercimek-Mahmutoglu et al. 2012). In our retrospective cohort study, we also identified subdural or posterior fossa hemorrhage in two patients (18%) in neuroimaging. In patients with intracerebral or subdural hemorrhage and drug resistant seizures, PDE-ALDH7A1 should be included in the differential diagnosis.
In summary, we report eleven patients with PDE-ALDH7A1. Based on our clinical severity score, there is no correlation between phenotype and the degree of α-AASA elevation in urine, genotype and delays in the initiation of pyridoxine therapy. Early initiation of lysine-restricted diet resulted in mild phenotype and normal neurodevelopmental outcome. Our clinical severity score might aid comparison of phenotype with degree of α-AASA elevation in urine and genotype in larger patient population studies.
References
Bok LA, Halbertsma FJ, Houterman S et al (2012) Long-term outcome in pyridoxine-dependent epilepsy. Dev Med Child Neurol 54:849–854
Coughlin CR 2nd, van Karnebeek CD, Al-Hertani W et al (2015) Triple therapy with pyridoxine, arginine supplementation and dietary lysine restriction in pyridoxine-dependent epilepsy: neurodevelopmental outcome. Mol Genet Metab 116:35–43
Gallagher RC, Van Hove JL, Scharer G et al (2009) Folinic acid-responsive seizures are identical to pyridoxine-dependent epilepsy. Ann Neurol 65:550–556
Gospe SM Jr (2014) Pyridoxine-dependent epilepsy. In: Pagon RA, Adam MP, Ardinger HH, Wallace SE, Amemiya A, Bean LJH, Bird TD, Fong CT, Mefford HC, Smith RJH, Stephens K (eds) GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–2015. 2001 [updated 2014]
Jain-Ghai S, Mishra N, Hahn C, Blaser S, Mercimek-Mahmutoglu S (2014) Fetal onset ventriculomegaly and subependymal cysts in a pyridoxine dependent epilepsy patient. Pediatrics 133:e1092–e1096
Kanno J, Kure S, Narisawa A et al (2007) Allelic and non-allelic heterogeneities in pyridoxine dependent seizures revealed by ALDH7A1 mutational analysis. Mol Genet Metab 91:384–389
Mahajnah M, Cordeiro D, Austin V et al (2016) A prospective case study of the safety and efficacy of lysine restricted diet and arginine supplementation therapy in a patient with pyridoxine-dependent epilepsy caused by mutations in ALDH7A1. Pediatr Neurol. doi:10.1016/j.pediatrneurol.2016.03.008
Mercimek-Mahmutoglu S, Horvath GA, Coulter-Mackie M et al (2012) Profound neonatal hypoglycemia and lactic acidosis caused by pyridoxine-dependent epilepsy. Pediatrics 129:e1368–e1372
Mercimek-Mahmutoglu S, Cordeiro D, Cruz V et al (2014) Novel therapy for pyridoxine dependent epilepsy due to ALDH7A1 genetic defect: Larginine supplementation alternative to lysine-restricted diet. Eur J Paediatr Neruol 18:741–746
Mercimek-Mahmutoglu S, Sidky S, Hyland K et al (2015) Prevalence of inherited neurotransmitter disorders in patients with movement disorders and epilepsy: a retrospective cohort study. Orphanet J Rare Dis 10:12
Mikati MA, Trevathan E, Krishnamoorthy KS, Lombroso CT (1991) Pyridoxine-dependent epilepsy: EEG investigations and long-term follow-up. Electroencephalogr Clin Neurophysiol 78:215–221
Mills PB, Struys E, Jakobs C et al (2006) Mutations in antiquitin in individuals with pyridoxine-dependent seizures. Nat Med 12:307–309
Mills PB, Footitt EJ, Mills KA et al (2010) Genotypic and phenotypic spectrum of pyridoxine-dependent epilepsy (ALDH7A1 deficiency). Brain 133:2148–2159
Nasr E, Mamak E, Feigenbaum A, Donner EJ, Mercimek-Mahmutoglu S (2015) Long-term treatment outcome of two patients with pyridoxine-dependent epilepsy caused by ALDH7A1 mutations: normal neurocognitive outcome. J Child Neurol 30:648–653
Plecko B, Paul K, Paschke E et al (2007) Biochemical and molecular characterization of 18 patients with pyridoxine-dependent epilepsy and mutations of the antiquitin (ALDH7A1) gene. Hum Mutat 28:19–26
Salomons GS, Bok LA, Struys EA, Pope LL, Darmin PS, Mills PB, Clayton PT, Willemsen MA, Jakobs C (2007) An intriguing “silent” mutation and a founder effect in antiquitin (ALDH7A1). Ann Neurol 62:414–418
Stockler S, Plecko B, Gospe SM Jr et al (2011) Pyridoxine dependent epilepsy and antiquitin deficiency: clinical and molecular characteristics and recommendations for diagnosis, treatment and follow-up. Mol Genet Metab 104:48–60
Van Karnebeek CD, Hartmann H, Jaggumantri S et al (2012) Lysine restricted diet for pyridoxine-dependent epilepsy: first evidence and future trials. Mol Genet Metab 107:335–344
Van Karnebeek CD, Stockler-Ipsiroglu S, Jaggumantri S et al (2014) Lysine-restricted diet as adjunct therapy for pyridoxine-dependent epilepsy: the PDE consortium consensus recommendations. JIMD Rep 15:1–11
Yuzyuk T, Thomas A, Viau K, Liu A, De Biase I, Botto LD, Pasquali M, Longo N (2016) Effect of dietary lysine restriction and arginine supplementation in two patients with pyridoxine-dependent epilepsy. Mol Genet Metab 118:167–172
Acknowledgements
We would like to thank to parents and patients. We would like to thank to Mrs. L. Nagy, metabolic dietician and Mrs. S. Herd, metabolic dietician for the application of lysine-restricted diet. We would like to thank to Dr. G. Salomons for performing mutation analysis of ALDH7A1. We would like to thank to Dr. Siriwardena, Dr. Donner, Dr. Raiman and Dr. Peter Humphreys referring their patients. We would like to thank to Stacy Hewson for genetic counseling of families for molecular genetic test results.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Institutional Research Ethics Board approved the study (Approval#1000050808).
Electronic supplementary material
Supplemental Figure 1
Clinical severity score compared to the X-fold elevated in the upper limit of normal urine and plasma α-AASA levels in eight patients with no lysine-restricted diet initiated within their first 7 months of life (except patient ID# 5, 8 and 11) with PDE-ALDH7A1. *Values for these patients are from plasma α-AASA level. (JPEG 46 kb)
Supplemental Table 1
Neuropsychological assessment results on treatment in patients with PDE-ALDH7A1. (DOCX 30 kb)
Rights and permissions
About this article
Cite this article
Al Teneiji, A., Bruun, T.U.J., Cordeiro, D. et al. Phenotype, biochemical features, genotype and treatment outcome of pyridoxine-dependent epilepsy. Metab Brain Dis 32, 443–451 (2017). https://doi.org/10.1007/s11011-016-9933-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11011-016-9933-8