Abstract
We recently identified leptin as a downstream factor mediating the hypertrophic effects of both angiotensin II and endothelin-1 in cardiomyocytes, an effect dependent on increased leptin biosynthesis, however, the mechanism for such increased leptin production is not known. This study was designed to elucidate the mechanisms underlying angiotensin II- and endothelin-1-stimulated synthesis in cultured ventricular myocytes. The hypertrophic effects of both angiotensin II (100 nM) and endothelin-1 (10 nM) were associated with increased leptin secretion and gene expression by 40 and 50 %, and 86 and 68 %, respectively. These effects were associated with significantly increased nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) phosphorylation by 34 and 52 %, as well as enhanced translocation of NF-κB into nuclei and also the NF-κB-DNA binding activity by 35 and 31 % induced by angiotensin II and endothelin-1, respectively. On their own, 24 h treatment with either angiotensin II or endothelin-1 increased cell surface area by 30 and 40 %, protein synthesis by 30 % and the α-skeletal actin gene by 53 and 68 %, respectively, indicating a robust hypertrophic effect whereas this was completely prevented by NF-κB inhibition. In addition, NF-κB inhibition significantly attenuated angiotensin II and endothelin-1-induced p38 MAPK activation whereas inhibition of p38 MAPK blocked both angiotensin II- and endothelin-1-induced increases in leptin secretion. The ability of both angiotensin II- and endothelin-1 to increase leptin production in cardiomyocytes and the resultant hypertrophic response are mediated by NF-κB and dependent on p38 MAPK activation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The plasma concentrations of leptin, a 16 kDa peptide which is a product of the obesity gene, are greatly elevated in obesity and to a lesser extent in cardiovascular disease including heart failure [1, 2], independently of obesity. There still remains substantial uncertainty as to the role of leptin in the heart failure process although both leptin and its receptors are upregulated in the failing heart [3, 4] and we and others have shown that inhibition of leptin expression [3] or blocking of leptin receptors [5] attenuates postinfarction ventricular dysfunction. Both angiotensin II (Ang II) and endothelin-1 (ET-1) plasma concentrations are also increased in patients with heart failure [6, 7]. We have previously reported that both Ang II and ET-1 stimulate leptin production in cultured rat ventricular myocytes via de novo synthesis and that leptin likely mediates the pro-hypertrophic effects of these compounds since leptin receptor blockade inhibited the hypertrophic effects of both Ang II and ET-1 [8]. However, the mechanisms underlying the stimulation of leptin production and secretion in cardiac cells are not known.
A number of signaling pathways has been implicated in the hypertrophic program initiated by Ang II and ET-1. One pathway which has attracted substantial attention is nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) which has been shown to participate in the hypertrophic response to both Ang II and ET-1 [9–11] as well as Ang II-induced left-ventricular remodeling [12]. Moreover, NF-κB inhibition has been shown to prevent cardiac hypertrophy and heart failure [13]. However, it appears that the hypertrophic response to Ang II and ET-1 is complex and also involves activation of mitogen-activated protein kinases (MAPKs) [14, 15]. Leptin also activates MAPKs in cardiomyocytes [16]. In view of the apparent role of leptin in mediating the pro-hypertrophic effect of both Ang II and ET-1, we hypothesized that activation of NF-κB and MAPKs could be potential mechanisms involved in the stimulation of leptin synthesis induced by Ang II and ET-1. Accordingly, this study was performed to determine the relative contributions of NF-κB and MAPKs toward Ang II and ET-1-induced increase in leptin production in cardiomyocytes and the relationship between these effects and the hypertrophic responses to both agonists.
Materials and methods
Materials
One-day old Sprague–Dawley neonatal rat pups were purchased from Charles River (St. Constant, QC, Canada). Trizol and superscript II RNase H-reverse transcriptase were from Invitrogen (Carlsbad, CA, USA). ELISA assay kit for leptin determination was purchased from assay designs (Ann Arbor, MI, USA). Antibodies for Western blotting were either from Cell Signaling Technology (Beverly, MA, USA) (P-p38, P-ERK1/2, P-NF-κB, NF-κB, and GAPDH) or Santa Cruz Biotechnology (Santa Cruz, CA, USA) (p38, ERK1/2, and PCNA). Reagents for protein assays were from Bio-Rad Laboratories (Mississauga, ON, Canada). The NF-κB inhibitor 6-Amino-4-(4-phenoxyphenylethylamino) quinazoline was purchased from EMD Chemicals (Gibbstown, NJ, USA). The l-leucine [3,4,5-3H] was purchased from MP Biomedicals (Solon, OH). Penicillin and streptomycin used for culture medium were purchased from Invitrogen Canada Inc. (Burlington, ON, Canada). All other chemicals and drugs were purchased from Sigma-Aldrich Canada (Oakville, ON, Canada).
Primary culture of cardiomyocytes
The procedures followed are in accordance with the University of Western Ontario animal care guidelines, which conform to the guidelines of the Canadian Council on Animal Care (Ottawa, ON, Canada). Primary cultures of cardiomyocytes were prepared from 1-day old Sprague–Dawley neonatal rat heart ventricles as described previously [17]. Rats were sacrificed by decapitation and hearts were excised and rinsed in buffer containing 1× Hank’s balanced salt solution (HBSS), 20 mM HEPES, and 1 % Penicillin Streptomycin. Ventricles were then minced with a scalpel mounted with a surgical blade and the minced tissue was transferred to a water-jacketed Erlenmyer flask maintained at 37 °C. The tissue was subjected to six sequential digestions using a solution containing 0.4 % type 2 collagenase, 1× HBSS, 20 mM HEPES, 100 U/ml penicillin, and 100 μg/ml streptomycin. After each extraction, the supernatant was added to a tube having an equal volume of 1× HBSS, 20 % fetal bovine serum, and 1 % Penicillin Streptomycin to stop collagenase activity. All extractions were then pooled, filtered using a 70 μm cell strainer and centrifuged at 500× g for 5 min at 4 °C. The pellet was resuspended in cell culture medium containing Dulbecco’s-modified Eagle’s medium and Ham’s F-12 supplemented with 10 % fetal bovine serum, 10 μg/ml transferrin, 10 μg/ml insulin, 10 ng/ml selenium, 100 units/ml penicillin, 100 μg/ml streptomycin, 2 mg/ml bovine serum albumin BSA), 5 μg/ml linoleic acid, 3 mM pyruvic acid, 1 % minimum essential medium (MEM) non-essential amino acids, 0.1 % MEM vitamin, 0.1 mM bromodeoxyuridine, 100 μM l-ascorbic acid, and 30 mM HEPES (pH 7.14) and two 30 min periods of preplating were carried out to enrich the cardiomyocyte population. Myocytes were then plated on Primaria dishes and cultured for 48 h. The cells were washed with phosphate-buffered saline (PBS) and cultured for 24 h in cell culture medium devoid of fetal bovine serum before starting treatment. Based on the percentage of cells demonstrating myosin staining, there was <5 % contamination by non-cardiomyocytes in our preparation.
Cell surface area analysis of cardiomyocytes
Cells were cultured for 24 h in serum-containing medium after which they were serum-starved for 24 h before treatments. Cells were treated with vehicle (control), Ang II (100 nM) or ET-1 (10 nM) in the presence or absence of NF-κB activation inhibitor peptide (1 μM), p38 MAPK inhibitor SB203580 (10 μM), or ERK1/2 MAPK inhibitor PD 98059 (10 μM) for 24 h. Cell surface area was analyzed using a Leica inverted microscope equipped with an infinity 1 camera at 200× magnification. Cell area was measured using SigmaScan Software (Systat, Richmond, CA, USA).
Leucine incorporation
Cardiomyocytes (5 × 105) were plated into 24-well primaria culture plates and cultured for 48 h in serum-containing media followed by incubation in serum-free media for 24 h. Following the appropriate treatments, 2 μCi of [3H] leucine was added to each well and incubated for 24 h. At the end of labeling, cells were washed three times with ice-cold PBS and incubated with 5 % trichloroacetic acid (TCA) on ice for 30 min. The cells were washed two more times with ice-cold 5 % TCA and solubilized in 0.5 N sodium hydroxide. After neutralizing with 0.5 N hydrochloric acid, the entire cell suspension was used to determine the incorporated radioactivity by liquid scintillation counting.
RNA isolation, reverse transcription, and real-time PCR analysis for leptin, OBRb, and 18S rRNA
Following the treatments, total RNA from cells was extracted using Trizol according to the manufacturer’s instructions. Five microgram RNA were used to synthesize first strand of cDNA using SuperScript™ II RNase H-reverse transcriptase according to the manufacturer’s protocol and was used as template in the following PCR reactions. The expression of the above genes was performed in 10 μl reaction volumes using EvaGreen qPCR Mastermix (Applied Biological Materials Inc., Richmond, BC, Canada) and fluorescence was measured and quantified using DNA Engine Opticon 2 System (MJ Research, Waltham, MA, USA). The primer sequences for leptin, OBRb, and 18S rRNA and the PCR cycle conditions to amplify the genes were as described previously [8]. 18S rRNA gene expression was used as a control.
ELISA analysis for leptin content
Cardiomyocytes (2 × 106) were plated into six-well primaria culture plates and cultured for 48 h in serum-containing media followed by incubation in serum-free media for 24 h. The cultures (cells in 0.5 ml of serum-free medium) were treated with vehicle, Ang II (100 nM) or ET-1 (10 nM) in the presence or absence of p38 MAPK inhibitor SB203580 (10 μM), ERK1/2 MAPK inhibitor PD 98059 (10 μM), or NF-κB activation inhibitor (1 μM) for 24 h. A 300 μl aliquot of cell culture media was taken for assaying leptin release using a Rat Leptin Enzyme Immunometric Assay Kit (Enzo Life Sciences, Plymouth Meeting, PA, USA) according to the manufacturer’s instructions. The developed color was measured at 540 nm in a Molecular Devices (Sunnyvale, CA, USA) Spectramax M5 plate reader.
SDS-PAGE and Western blotting
Following the treatments, cells were washed twice with cold PBS and protein lysates were prepared as described previously [8]. Protein (30 μg) was resolved on 10 % acrylamide gels and transferred on to 0.45 μm nitrocellulose membrane. After blocking the membranes with 5 % skim dry milk they were probed with P-p38, P-ERK1/2, P-NF-κB, PCNA, or glyceraldehyde-3-phosphate dehydrogenase (GAPDH) antibodies. Following incubation with horseradish peroxidase-coupled to the secondary antibody, the signal was detected with ECL Western blotting detection reagents.
Immunofluorescence microscopy
Cells were grown on round cover slips coated with collagen. Cells were treated with Ang II (100 nM) or ET-1 (10 nM) for 3 h. After the treatment, myocytes were fixed in ice-cold mixture of acetone and methanol (20:80) for 1 h at 4 °C. Fixation was followed by permeabilization with 0.1 % Triton and blocking with 1 % BSA for 1 h. Cells were incubated with an antibody against total NF-κB (1:100 dilution) overnight at 4 °C. This was followed by incubation in alexa fluor 594 goat anti-rabbit IgG (1:250 dilution) for 1 h at room temperature in the dark. The cells were mounted on a glass slide using Dako cytomation fluorescent mounting medium and visualized using a Zeiss Observer D1 microscope (Carl Zeiss, Oberkochen, Germany).
Preparation of cytosolic and nuclear fractions
Following appropriate treatments myocytes were rinsed with ice-cold PBS and scraped into 1 ml of PBS followed by centrifugation at 800 × g for 5 min. The cell pellet was resuspended by gently vortexing in 200 μl of buffer A containing 10 mM HEPES (pH 7.9), 1 mM EDTA, 1 mM EGTA, 10 mM KCl, 1 mM DTT, 5 mM NaF, 1 mM Sodium vanadate, and 0.5 % NP-40 supplemented with cocktail of protease inhibitors followed by centrifugation at 8,000× g for 15 min at 4 °C. The supernatant was used as a cytosolic extract and the cell pellet is resuspended in 50 μl of buffer B (buffer A supplemented with 20 % glycerol and 0.4 M KCl) and incubated at 4 °C for 30 min. The nuclear suspension was centrifuged at 13,000× g for 15 min at 4 °C and the supernatant was collected and used as the nuclear extract.
NF-κB transcription factor activity
Cells were treated with Ang II (100 nM) or ET-1 (10 nM) in the presence or absence of NF-κB activation inhibitor peptide (1 μM) for 3 h. Nuclear fractions from these cells were prepared as noted above, and 10 μg of nuclear protein was used to measure the NF-κB transcription factor activity using a NF-κB (p65) transcription factor assay ELISA kit (Rockland Immunochemicals, Inc., Gilbertsville, PA, USA) according to manufacturer’s instructions. The developed color was measured at 450 nm in a Molecular Devices, Spectramax M5 plate reader.
Statistical analysis
The data were analysed with ANOVA and post ANOVA analysis with Dunnets test. P values of <0.05 were considered as significant.
Results
Ang II and ET-1-induced NF-κB activation and nuclear translocation
Our initial studies determined the activation of NF-κB by either Ang II or ET-1. As shown in Fig. 1a, both Ang II- and ET-1-treatment for 10 min induced the activation of NF-κB by 34 and 52 %, respectively, compared to control. We next determined the effect of Ang II or ET-1 on the translocation of NF-κB from cytosol into the nucleus. Treatment with either Ang II or ET-1 for 3 h resulted in translocation of NF-κB from cytosol into nucleus as determined by Western blotting (Fig. 1b), immunofluorescence detection (Fig. 1c), and NF-κB-DNA binding activity (Fig. 1d). The NF-κB activity stimulated by Ang II or ET-1 was blocked by NF-κB inhibitor peptide, confirming the NF-κB inhibitor specificity.
Ang II and ET-1 administration results in activation and translocation of NF-κB into nuclei. a Demonstrates activation and quantification of NF-κB as determined by the degree of phosphorylation after treatment with Ang II or ET-1 for 10 min. b The expression and quantification of total NF-κB in cytosol (Cyt) and nuclear (Nuc) fractions isolated from myocytes treated with Ang II or ET-1 for 3 h. GAPDH and PCNA were used as loading controls for cytosol and nuclear fractions, respectively. c Immunofluorescent images of NF-κB localization in cytosol in control (Ctrl) and in nuclei in myocytes treated with Ang II or ET-1 for 3 h. d Quantification of NF-κB-DNA binding activity in nuclear lysates of control (Ctrl) and treated with Ang II or ET-1 for 3 h in the presence or absence of NF-κB-activation inhibitor, 6-amino-4-(4-phenoxyphenylethylamino) quinazoline (NFI). Values indicate means ± SEM (n = 6). *P < 0.05 from untreated myocytes (Ctrl)
NF-κB inhibition prevents Ang II and ET-1-induced cardiomyocyte hypertrophy
Figure 2 summarizes results of experiments aimed at determining the potential contribution of NF-κB to cardiomyocyte hypertrophy. Treatment with either Ang II or ET-1 for 24 h increased the cell surface area by ~30 and 40 %, respectively (Fig. 2a, b), rate of protein synthesis by 30 % (Fig. 2c, d), and α-skeletal actin gene expression by 53 and 68 %, respectively (Fig. 2e, f). The hypertrophic responses to both Ang II and ET-1 were completely abrogated by the NF-κB inhibitor.
Ang II- and ET-1-induced cardiomyocyte hypertrophy is prevented by a NF-κB inhibitor (NFI). Panels show cell surface area (a, b), [3H] leucine incorporation (c, d), and expression of α-skeletal actin (e, f). Myocytes were treated for 24 h in the presence or absence of the NF-κB inhibitor (NFI). Values indicate means ± SEM (n = 6–9). *P < 0.05 from untreated myocytes (Ctrl), # P < 0.05 from Ang II group, $ P < 0.05 from ET-1 group
NF-κB inhibition prevents Ang II and ET-1-induced elevations in leptin secretion and gene expression but not OBRb upregulation
Based on results presented previously (see Discussion) and those reported here suggesting that leptin and NF-κB mediate Ang II- and ET-1-initiated hypertrophic signaling, we hypothesized that these two factors may be linked, such that NF-κB may be one of the potential signaling mechanisms involved in leptin production. As expected, treatment of myocytes with Ang II or ET-1 for 24 h resulted in increased leptin secretion by 40 and 50 %, respectively (Fig. 3a, b). Moreover, as shown in Fig. 3c, d these effects were associated with significantly increased leptin gene expression by 86 and 68 % for Ang II and ET-1, respectively. The ability of both agonists to increase secretion or expression of leptin was completely prevented by NF-κB inhibition.
NF-κB inhibition attenuates Ang II- and ET-1-induced leptin secretion and expression but not leptin receptor b isoform (OBRb) expression in cardiomyocytes. Panels demonstrate quantification of secretion (a, b) and gene expression (c, d) of leptin as well as expression of OBRb (e, f). Cells were treated with Ang II or ET-1 in the presence or absence of the NF-κB inhibitor (NFI) for 24 h. Values indicate means ± SEM (n = 7–9). *P < 0.05 from untreated myocytes (Ctrl), # P < 0.05 from Ang II group, $ P < 0.05 from ET-1 group. The control medium leptin concentration before initiation of any treatment was 457 ± 35 pg/ml
Both Ang II and ET-1 produced a nearly two-fold increase in cardiomyocyte OBRb expression after 24 h treatment. However, as shown in Fig. 3e, f, this response was unaffected by NF-κB inhibition.
Effect of NF-κB inhibition on Ang II- and ET-1-induced activation of P38 and ERK1/2 MAPKs
We next determined whether NF-κB inhibition can modify the ability of either agonist to activate either p38 or ERK1/2 MAPKs. As shown in Fig. 4a, b, both Ang II and ET-1 significantly increased p38 phosphorylation which was completely prevented by NF-κB inhibition. Similarly, ERK1/2 phosphorylation was significantly enhanced by both agents (Fig. 4c, d). However, in contrast to the effect seen with p38, NF-κB inhibition significantly attenuated only the response to Ang II, although values in the presence of the inhibitor were significantly higher from control, whereas the nearly two-fold increase in ERK phosphorylation in response to ET-1 was unaffected.
NF-κB inhibition attenuates MAPK activation in myocytes treated for 10 min with either Ang II or ET-1. Panels demonstrate quantification of phosphorylated p38 (P-p38, a, b) and phosphorylated ERK1/2 (P-ER1/2, c, d) in the presence or absence of the NF-κB inhibitor (NFI). Values indicate means ± SEM (n = 6). *P < 0.05 from untreated myocytes (Ctrl), # P < 0.05 from Ang II group, $ P < 0.05 from ET-1 group
P38 MAPK inhibition blunts Ang II and ET-1-induced leptin secretion
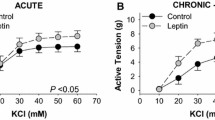
We next determined the effect of p38 and ERK1/2 MAPKs inhibition on Ang II- or ET-1-induced leptin secretion. As shown in Fig. 5a, b, the p38 inhibitor SB203580 significantly inhibited the stimulation in leptin secretion induced by both hypertrophic factors although the effect was more pronounced against ET-1. The ERK inhibitor PD98059 was without any significant effect. Moreover, the hypertrophic responses to either Ang II or ET-1 paralleled the effects seen on leptin secretion in that the hypertrophic response was abrogated by p38 inhibition with no effect seen with the ERK inhibitor PD98059 (Fig. 5c, d).
Inhibition of p38 MAPK but not ERK1/2 blocks the stimulation of leptin secretion and hypertrophic responses in myocytes treated for 24 h with Ang II or ET-1. Panels show leptin secretion (a, b) and myocyte surface areas (c, d) in the presence or absence of the p38 inhibitor SB 203580 (SB) or the ERK1/2 inhibitor PD 98059 (PD). Values indicate means ± SEM (n = 6). *P < 0.05 from untreated myocytes (Ctrl), # P < 0.05 from Ang II group, $ P < 0.05 from ET-1 group
Discussion
Although, the direct cardiac hypertrophic effects of leptin have been extensively documented [16, 18–20] there is also evidence that leptin mediates the effect of other pro-hypertrophic factors in a paracrine or autocrine manner. In particular, work from our laboratory has shown that both Ang II and ET-1 have the ability to potently increase the release of leptin from cultured ventricular myocytes, a phenomenon which we have previously shown reflects de novo protein synthesis [8]. Moreover, blockade of leptin receptors prevented the hypertrophic effect of both Ang II and ET-1. When taken together, the data suggest the leptin may serve as an endogenous paracrine or autocrine factor in mediating the hypertrophic effect of Ang II and ET-1. Since plasma levels of leptin [1, 2], as well as both Ang II and ET-1 [6, 7] are elevated in patients with heart failure it is important to understand the possible interaction between these factors especially. Moreover, leptin has recently been demonstrated to be closely associated with the development of heart failure in obese men [21] and both ET-1 and Ang II have been implicated in the increased cardiovascular risk in obese individuals [22, 23].
We hypothesize that both Ang II and ET-1 represent important endogenous stimulants for leptin secretion, especially under pathological conditions. Accordingly, in this study we sought to understand the mechanistic basis for increased leptin production seen following Ang II or ET-1 administration and to further show whether these mechanisms underlie or contribute to the hypertrophic effect of either Ang II or ET-1. Our study focussed primarily on the transcriptional factor NF-κB which regulates a large number of intracellular processes in the cardiovascular system associated with both physiology and pathology [24, 25]. Moreover, NF-κB has been shown to be involved in the development of cardiomyocyte hypertrophy [26, 27] and myocardial NF-κB has been shown to be activated in patients with heart failure [28, 29]. Of particular relevance to this report, NF-κB ablation has been shown to prevent the hypertrophic effect of chronic (4 week) Ang II infusion in mice [30] and NF-κB has been reported to mediate a number of cardiovascular effects produced by Ang II [31–33] and ET-1 [34]. When taken together NF-κB emerges as an important mediator for the effects produced by both Ang II and ET-1, however, whether this transcriptional factor contributes to the ability of either agonist to upregulate the leptin system has not been studied.
These results provide strong evidence for a key role of NF-κB in mediating the ability of both Ang II and ET-1 to stimulate leptin production resulting in the hypertrophic response in cultured neonatal rat ventricular myocytes. This is based on a number of lines of evidence. First, both Ang II and ET-1 potently activated NF-κB as shown by increased NF-κB phosphorylation and enhanced translocation into nuclei coupled with elevated NF-κB transcription factor activity. Second, inhibition of NF-κB activation with 6-Amino-4-(4-phenoxyphenylethylamino) quinazoline completely abrogated the hypertrophic response to both agonists. Third, these effects were associated with prevention in the increased expression and production of leptin. In view of the fact that the hypertrophic effect of both Ang II and ET-1 can be prevented by a specific OBR antagonist as well as an antibody directed against leptin [8], it is reasonable to propose that NF-κB plays a critical role in mediating the hypertrophic effect of Ang II and ET-1 by preventing leptin upregulation. Interestingly, NF-κB inhibition failed to exert any effect on the ability of either Ang II or ET-1 to enhance OBRb expression, thus suggesting that with respect to the leptin system the role of this transcriptional factor is restricted to the regulation of leptin production. Our study implicating NF-κB as a key regulator of the hypertrophic response to both Ang II and ET-1 further supports the contention that NF-κB is a key component of the hypertrophic program: indeed overexpression of NF-κB per se in the absence of other prohypertrophic stimuli results in the hypertrophic phenotype in cardiomyocytes [9]. Overall, those findings as well as those reported here suggest some commonality with respect to mechanisms underlying the effects of Ang II and ET-1 following activation of their respective receptors.
Previously, we have extensively demonstrated that the hypertrophic effect of leptin is mediated by MAPK activation, or more specifically by phosphorylation followed by selective translocation of p38 MAPK, but not ERK1/2, into nuclei following cardiomyocyte stimulation with leptin [35]. Interestingly, MAPK inhibition has been to shown to attenuate the hypertrophic effect of both Ang II and ET-1 [14, 15, 18]. The question then arises as to whether MAPK is also involved in the NF-κB-dependent stimulation of leptin production induced by either Ang II or ET-1 and whether this is related to the hypertrophic influence of either agent. Our results suggest that this is a potentially likely scenario as both agonists increased p38 as well as ERK1/2 phosphorylation. Although NF-κB inhibition effectively inhibited the increased p38 phosphorylation induced by both And II as well as ET-1 diverse effects were seen with respect to ERK1/2 phosphorylation. In this regard, NF-κB inhibition only partially reduced the Ang II-induced increased ERK1/2 phosphorylation whereas ET-1-induced changes in ERK1/2 were unaffected. The reasons for these differences are not known but the results suggest that NF-κB plays a less pivotal role in mediating the activation of ERK1/2 by Ang II whereas the effect of ET-1 on ERK1/2 is likely independent of NF-κB. The robust ability of NF-κB inhibition to selectively prevent p38 activation agrees with our finding that only p38 MAPK inhibition significantly attenuated the ability of either Ang II or ET-1 to augment leptin secretion. Based on the fact that only p38 is translocated into nuclei following leptin administration [35], our results, when taken together, support our contention that the hypertrophic effect of leptin is dependent on p38 but not ERK1/2 MAPK activation. Moreover, the hypertrophic effect of leptin is abrogated by p38 but not by ERK1/2 inhibition [16]. It is interesting to point out that Ang II-induced leptin production has also been demonstrated in human adipocytes, however, in that study this phenomenon was found to be ERK1/2-dependent [36]. Thus, the results presented in this report may be specific for the cardiac myocyte. Although p38 MAPK has been suggested to be involved in NF-κB activation [37] we are unaware of any study suggesting a NF-κB-dependent p38 activation. It is, however, interesting that the α1-adrenoceptor-induced increased production of interleukin-6 by cardiomyocytes has also been shown to be both NF-κB and p38 MAPK-dependent [38].
Summary and conclusion
Based on these results we propose that Ang II and ET-1 by binding to their respective sarcolemmal receptors upregulate the synthesis of leptin in cardiomyocytes through NF-κB-dependent mechanisms which involves the translocation of NF-κB into nuclei as well as the phosphorylation and translocation of p38 MAPK (Fig. 6). Although not illustrated in Fig. 6, it is important to point out that both Ang II and ET-1 receptors have also been identified on nuclear membranes in cardiac cells [39, 40] and thus, the role of these receptors in the regulation of leptin production needs to be determined with further studies. Irrespective of the nature of the receptor involved, our hypothesis is that the increased intracellular production of leptin and its subsequent efflux from cardiomyocytes leads to OBR activation and the resulting hypertrophic response. Moreover, Ang II and ET-1 likely induce hypertrophy via NF-κB and p38 activation independently of leptin upregulation. Thus, administration of an NF-κB inhibitor (NFI) or p38 inhibitor (SB) can effectively abrogate both the elevation in leptin synthesis as well as the hypertrophic response to both Ang II and ET-1. The concept of Ang II and ET-1-dependent leptin upregulation needs to be studied further especially under in vivo conditions. However, given the fact that Ang II, ET-1, and leptin are all upregulated in obesity as well as heart failure, our findings could be of importance in understanding the mechanisms of regulation of leptin production in pathology as well as its potential role in mediating the increased risk in cardiovascular morbidity.
Proposed mechanism for increased leptin production in cardiomyocytes produced by either Ang II and ET-1 and the subsequent hypertrophic response. See Discussion for details
References
Toth MJ, Gottlieb SS, Fisher ML, Ryan AS, Nicklas BJ, Poehlman ET (1997) Plasma leptin concentrations and energy expenditure in heart failure patients. Metabolism 46:450–453
Leyva F, Anker SD, Egerer K, Stevenson JC, Kox WJ, Coats AJ (1998) Hyperleptinaemia in chronic heart failure. Relationships with insulin. Eur Heart J 19:1547–1551
Moro C, Grauzam S, Ormezzano O, Toufektsian MC, Tanguy S, Calabrese P, Coll JL, Bak I, Juhasz B, Tosaki A, de Leiris J, Boucher F (2011) Inhibition of cardiac leptin expression after infarction reduces subsequent dysfunction. J Cell Mol Med 15:1688–1694
McGaffin KR, Moravec CS, McTiernan CF (2009) Leptin signaling in the failing and mechanically unloaded human heart. Circ Heart Fail 2:676–683
Purdham DM, Rajapurohitam V, Zeidan A, Huang C, Gross GJ, Karmazyn M (2008) A neutralizing leptin receptor antibody mitigates hypertrophy and hemodynamic dysfunction in the postinfarcted rat heart. Am J Physiol Heart Circ Physiol 295:H441–H446
Pedersen EB, Danielsen H, Jensen T, Madsen M, Sorensen SS, Thomsen OO (1986) Angiotensin II, aldosterone and arginine vasopressin in plasma in congestive heart failure. Eur J Clin Invest 16:56–60
Kinugawa T, Kato M, Ogino K, Osaki S, Igawa O, Hisatome I, Shigemasa C (2003) Plasma endothelin-1 levels and clinical correlates in patients with chronic heart failure. J Card Fail 9:318–324
Rajapurohitam V, Javadov S, Purdham DM, Kirshenbaum LA, Karmazyn M (2006) An autocrine role for leptin in mediating the cardiomyocyte hypertrophic effects of angiotensin II and endothelin-1. J Mol Cell Cardiol 41:265–274
Purcell NH, Tang G, Yu C, Mercurio F, DiDonato JA, Lin A (2001) Activation of NF-kappa B is required for hypertrophic growth of primary rat neonatal ventricular cardiomyocytes. Proc Natl Acad Sci USA 98:6668–6673
Hirotani S, Otsu K, Nishida K, Higuchi Y, Morita T, Nakayama H, Yamaguchi O, Mano T, Matsumura Y, Ueno H, Tada M, Hori M (2002) Involvement of nuclear factor-kappaB and apoptosis signal-regulating kinase 1 in G-protein-coupled receptor agonist-induced cardiomyocyte hypertrophy. Circulation 105:509–515
Doi T, Sakoda T, Akagami T, Naka T, Mori Y, Tsujino T, Masuyama T, Ohyanagi M (2008) Aldosterone induces interleukin-18 through endothelin-1, angiotensin II, Rho/Rho-kinase, and PPARs in cardiomyocytes. Am J Physiol Heart Circ Physiol 295:H1279–H1287
Sarman B, Skoumal R, Leskinen H, Rysa J, Ilves M, Soini Y, Tuukkanen J, Pikkarainen S, Lako-Futo Z, Papp L, deChatel R, Toth M, Ruskoaho H, Szokodi I (2007) Nuclear factor-kappaB signaling contributes to severe, but not moderate, angiotensin II-induced left ventricular remodeling. J Hypertens 25:1927–1939
Gupta S, Young D, Maitra RK, Gupta A, Popovic ZB, Yong SL, Mahajan A, Wang Q, Sen S (2008) Prevention of cardiac hypertrophy and heart failure by silencing of NF-kappaB. J Mol Biol 375:637–649
Li H, Shi S, Sun YH, Zhao YJ, Li QF, Li HZ, Wang R, Xu CQ (2009) Dopamine D2 receptor stimulation inhibits angiotensin II-induced hypertrophy in cultured neonatal rat ventricular myocytes. Clin Exp Pharmacol Physiol 36:312–318
Xia Y, Karmazyn M (2004) Obligatory role for endogenous endothelin in mediating the hypertrophic effects of phenylephrine and angiotensin II in neonatal rat ventricular myocytes: evidence for two distinct mechanisms for endothelin regulation. J Pharmacol Exp Ther 310:43–51
Rajapurohitam V, Gan XT, Kirshenbaum LA, Karmazyn M (2003) The obesity-associated peptide leptin induces hypertrophy in neonatal rat ventricular myocytes. Circ Res 93:277–279
Gan XT, Chakrabarti S, Karmazyn M (2003) Increased endothelin-1 and endothelin receptor expression in myocytes of ischemic and reperfused rat hearts and ventricular myocytes exposed to ischemic conditions and its inhibition by nitric oxide generation. Can J Physiol Pharmacol 81:105–113
Xu FP, Chen MS, Wang YZ, Yi Q, Lin SB, Chen AF, Luo JD (2004) Leptin induces hypertrophy via endothelin-1-reactive oxygen species pathway in cultured neonatal rat cardiomyocytes. Circulation 110:1269–1275
Abe Y, Ono K, Kawamura T, Wada H, Kita T, Shimatsu A, Hasegawa K (2007) Leptin induces elongation of cardiac myocytes and causes eccentric left ventricular dilatation with compensation. Am J Physiol Heart Circ Physiol 292:H2387–H2396
Madani S, De Girolamo S, Munoz DM, Li RK, Sweeney G (2006) Direct effects of leptin on size and extracellular matrix components of human pediatric ventricular myocytes. Cardiovasc Res 69:716–725
Wannamethee SG, Shaper AG, Whincup PH, Lennon L, Sattar N (2011) Obesity and risk of incident heart failure in older men with and without pre-existing coronary heart disease: does leptin have a role? J Am Coll Cardiol 58:1870–1877
Parrinello G, Scaglione R, Pinto A, Corrao S, Cecala M, Di Silvestre G, Amato P, Licata A, Licata G (1996) Central obesity and hypertension: the role of plasma endothelin. Am J Hypertens 9:1186–1191
Zalesin KC, Franklin BA, Miller WM, Peterson ED, McCullough PA (2008) Impact of obesity on cardiovascular disease. Endocrinol Metab Clin North Am 37:663–684
Van der Heiden K, Cuhlmann S, le Luong A, Zakkar M, Evans (2010) PC Role of nuclear factor kappaB in cardiovascular health and disease. Clin Sci (Lond) 118:593–605
Gutierrez SH, Kuri MR, del Castillo ER (2008) Cardiac role of the transcription factor NF-kappaB. Cardiovasc Hematol Disord 8:153–160
Freund C, Schmidt-Ullrich R, Baurand A, Dunger S, Schneider W, Loser P, El-Jamali A, Dietz R, Scheidereit C, Bergmann MW (2005) Requirement of nuclear factor-kappaB in angiotensin II- and isoproterenol-induced cardiac hypertrophy in vivo. Circulation 111:2319–2325
Gupta S, Purcell NH, Lin A, d Sen S (2002) Activation of nuclear factor-kappaB is necessary for myotrophin-induced cardiac hypertrophy. J Cell Biol 159:1019–1028
Frantz S, Fraccarollo D, Wagner H, Behr TM, Jung P, Angermann CE, Ertl G, Bauersachs J (2003) Sustained activation of nuclear factor kappa B and activator protein 1 in chronic heart failure. Cardiovasc Res 57:749–756
Wong SC, Fukuchi M, Melnyk P, Rodger I, Giaid A (1998) Induction of cyclooxygenase-2 and activation of nuclear factor-kappaB in myocardium of patients with congestive heart failure. Circulation 98:100–103
Kawano S, Kubota T, Monden Y, Tsutsumi T, Inoue T, Kawamura N, Tsutsui H, Sunagawa K (2006) Blockade of NF-kappaB improves cardiac function and survival after myocardial infarction. Am J Physiol Heart Circ Physiol 291:H1337–H1344
Brasier AR, Jamaluddin M, Han Y, Patterson C, Runge MS (2000) Angiotensin II induces gene transcription through cell-type-dependent effects on the nuclear factor-kappaB (NF-kappaB) transcription factor. Mol Cell Biochem 212:155–169
Li XC, Zhuo JL (2008) Nuclear factor-kappaB as a hormonal intracellular signaling molecule: focus on angiotensin II-induced cardiovascular and renal injury. Curr Opin Nephrol Hypertens 17:37–43
Celi A, Del Fiorentino A, Cianchetti S, Pedrinelli R (2008) Tissue factor modulation by Angiotensin II: a clue to a better understanding of the cardiovascular effects of renin-angiotensin system blockade? Endocr Metab Immune Disord Drug Targets 8:308–313
Schorlemmer A, Matter ML, Shohet RV (2008) Cardioprotective signaling by endothelin. Trends Cardiovasc Med 18:233–239
Zeidan A, Javadov S, Chakrabarti S, Karmazyn M (2008) Leptin-induced cardiomyocyte hypertrophy involves selective caveolae and RhoA/ROCK-dependent p38 MAPK translocation to nuclei. Cardiovasc Res 77:64–72
Skurk T, van Harmelen V, Blum WF, Hauner H (2005) Angiotensin II promotes leptin production in cultured human fat cells by an ERK1/2-dependent pathway. Obes Res 13:969–973
Chandrasekar B, Valente AJ, Freeman GL, Mahimainathan L, Mummidi S (2006) Interleukin-18 induces human cardiac endothelial cell death via a novel signaling pathway involving NF-kappaB-dependent PTEN activation. Biochem Biophys Res Commun 339:956–963
Perez DM, Papay RS, Shi T (2009) α1-Adrenergic receptor stimulates interleukin-6 expression and secretion through both mRNA stability and transcriptional regulation: involvement of p38 mitogen-activated protein kinase and nuclear factor-kappaB. Mol Pharmacol 76:144–152
Bkaily G, Avedanian L, Jacques D (2009) Nuclear membrane receptors and channels as targets for drug development in cardiovascular diseases. Can J Physiol Pharmacol 87:108–119
Bkaily G, Avedanian L, Al-Khoury J, Provost C, Nader M, D’Orleans-Juste P, Jacques D (2011) Nuclear membrane receptors for ET-1 in cardiovascular function. Am J Physiol Regul Integr Comp Physiol 300:R251–R263
Acknowledgments
This study was supported by a grant (MOP62764) from the Canadian Institutes of Health Research. AK held a Postdoctoral Research Award from the Heart and Stroke Foundation of Canada during the course of these studies. MK is a Canada Research Chair in Experimental Cardiology.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rajapurohitam, V., Kilic, A., Javadov, S. et al. Role of NF-κB and p38 MAPK activation in mediating angiotensin II and endothelin-1-induced stimulation in leptin production and cardiomyocyte hypertrophy. Mol Cell Biochem 366, 287–297 (2012). https://doi.org/10.1007/s11010-012-1307-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-012-1307-x