Abstract
Objective
Despite growing consensus about the clinical value of preconception care (PCC), gaps and disparities remain in its delivery. This study aimed to examine the factors influencing behavior of health care providers around PCC in outpatient clinical settings in the United States.
Methods
Twenty health care providers who serve people of reproductive age were interviewed using semi-structured interviews. Data was coded based on a modified Theoretical Domains Framework and analyzed using deductive content analysis.
Results
We interviewed eight family medicine physicians, four obstetricians/gynecologists, seven nurse practitioners, and one nurse midwife. Overall, we found a wide variety in practices and attitudes towards PCC. Barriers and challenges to delivering PCC were shared across sites. We identified six themes that influenced provider behavior around PCC: (1) lack of knowledge of PCC guidelines, (2) perception of lack of preconception patient contact, (3) pessimism around patient “compliance,” (4) opinion about scope of practice, (5) clinical site structure, and (6) reliance on the patient/provider relationship.
Conclusions for Practice
Overall, our findings call for improved provider understanding of PCC and creative incorporation into current health care culture and practice. Given that PCC-specific visits are perceived by some as outside the norm of clinical offerings, providers may need to incorporate PCC into other encounters, as many in this study reported doing. We amplify the call for providers to understand how structural inequities may influence patient behavior and the value of standardized screening, within and beyond PCC, as well as examination of implicit and explicit provider bias.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Significance
What is already known on this subject? Despite consensus on its clinical value, preconception care (PCC) is not consistently delivered. In previous studies outside the United States (US), providers cited lack of PCC programming, lack of knowledge, poor coordination of care, and lack of contact in the preconception period as barriers to PCC delivery.
What this study adds? We use an established framework to elucidate factors influencing US provider behavior around PCC. The intention to provide patient-centered care, perception of strong patient-provider relationships, and assumptions regarding patient “compliance” emerged as barriers and must be reconciled with implementation goals. Our findings call for improved understanding of PCC, creative incorporation into practice, and examination of provider bias in care delivery.
Introduction
The preconception period has been identified as a promising target for interventions to improve maternal and child health (Dean et al., 2014; Kroelinger et al., 2018). Preconception care (also preconception health care, or PCC) involves a continuum of care before or between pregnancies that aims to address risk factors related to reproductive health and pregnancy outcomes (Posner et al., 2006; van der Zee et al., 2011). PCC statements from leading public health and medical organizations underscore the potential impact of PCC (American College of Obstetricians & Gynecologists, 2019; Farahi & Zolotor, 2013; Johnson et al., 2006; World Health Organization, 2013). PCC recommendations include medical interventions such as contraceptive counseling, genetic screening, and mental health management as well as screening for social and environmental risk factors like intimate partner violence (IPV) and workplace exposures (Johnson et al., 2006; Temel et al., 2014). Recent calls have been made to reframe PCC as quality primary and preventive care, regardless of future pregnancy intention (Frayne, 2017). Despite these guidelines and growing consensus about the value of PCC, gaps remain in its delivery (Robbins et al., 2018).
Implementation of practices in health care, such as PCC, requires individual and collective behavior change, which in turn requires understanding factors that influence behavior (Atkins et al., 2017). Previous studies have investigated providers’ PCC-related behavior; however, the majority of these studies have occurred outside the United States (US). These predominantly European studies show a lack of knowledge about PCC among both providers and patients and disagreement regarding where responsibility for PCC lies (Heyes, 2004; M’hamdi et al., 2017; Steel et al., 2016). One survey of US obstetrician-gynecologists (OBGYNs) found that most were willing to provide PCC but felt challenged by limited contact with patients in the preconception period (Morgan et al., 2006). Beyond this study, data on US providers’ approaches to PCC is lacking. Given the unique structure of the US health care system, further study within the US is needed to provide guidance for implementation efforts.
This analysis aimed to characterize factors influencing providers’ PCC-related behavior in outpatient clinical settings. We focus on the concept of PCC as well as the specific elements of contraception counseling, IPV screening, and depression screening. These three components of PCC are supported by strong recommendations from professional organizations and are achievable by most providers offering pregnancy or well-woman care (American College of Obstetricians & Gynecologists, 2019; Farahi & Zolotor, 2013; Johnson et al., 2006; World Health Organization, 2013). To achieve this aim, we use the Theoretical Domains Framework (TDF), a framework that explains determinants of evidence-based practice behavior (Atkins et al., 2017; Michie, 2005). The TDF consists of 12 domains that impact behavior change and has been employed in similar studies of PCC in Europe (M’hamdi et al., 2017).
Methods
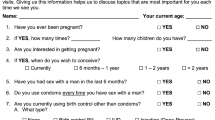
For this qualitative study, two authors (MT and EN) conducted semi-structured interviews with health care providers serving people of reproductive age about their PCC beliefs and practices from June through August 2017. A sample of providers was selected purposively to represent diversity in geography (urban and rural) and clinical setting (Table 1) across Wisconsin. Participants were approached via email.
Interviews were conducted in person at the health care site or via telephone and lasted from 12 to 52 min, with an average length of 24 min. The structured interview guide was developed using national recommendations regarding PCC (Siu et al., 2016; US Preventive Services Task Force et al., 2018) and focused on knowledge of and perceived barriers to implementing PCC (Online Resource 1). Additional questions focused on contraceptive counseling, depression screening, and IPV screening (Farahi & Zolotor, 2013; Lassi et al., 2014). All participants were asked the same questions with further probing by interviewers. Participants were asked their age, gender, and time in current position. Interviews were audio-recorded and transcribed verbatim.
Transcriptions were coded using deductive content analysis guided by the TDF (Michie, 2005). The domains were applied as codes to transcripts through line-by-line coding. Three authors (MG, EN, MT) coded the first three transcripts to refine code definitions and to establish consistency. Subsequently, two coders independently coded each transcript and discussed coding decisions until reaching 100% agreement.
Code reports were generated based on each TDF domain (code). Each code report and its interview responses were read in their entirety by each author. To generate themes, authors first identified reoccurring or strongly expressed ideas related to provider behavior within each code report. Those ideas were then compared across code reports for similarity and grouped into themes. Table 2 displays the themes and the TDF domains, or codes, which contributed data to those themes. The entire analysis was completed with consensus by all study team members (Braun & Clarke, 2012) and was facilitated by NVIVO 12.0 software. The study was deemed exempt by the University of Wisconsin-Madison Institutional Review Board.
Results
Twenty providers from 14 clinics were interviewed: eight family medicine physicians, four OBGYNs, seven nurse practitioners, and one nurse midwife. These providers worked in diverse settings including private practices (n = 6), Federally Qualified Health Centers or Rural Health Centers (henceforth “FQHCs,” n = 3), a public health clinic (n = 1), and family planning clinics (n = 4). Twenty-eight clinics were originally approached for interviews; 2 sites declined to participate (2 urban), and 12 did not respond (6 rural and 6 urban). Providers’ average age was 46 years (range 32–65 years), and average time in current position was 10 years (range 1–31 years). The sample was 70% women and 30% men.
There was general agreement among participants that, if implemented, PCC “is extremely valuable,” and could have positive impact on health. Providers expressed confidence in their skills to implement PCC. However, they described barriers preventing successful implementation. Six themes emerged that describe factors limiting PCC provision (Table 2).
Lack of Knowledge About PCC Guidelines
Emerging from data coded within TDF domains “Knowledge” and “Skills,” there was a lack of awareness of published PCC guidelines. Few providers could name an organization that had published recommendations for such care. For example, one provider admitted, “I’m not sure what official [PCC] guidelines you’re talking about.” Those who were aware of guidelines almost exclusively worked at family planning clinics, where care more strongly relied on guidelines. These providers cited recommendations from the Quality Family Planning Guidelines, American College of Obstetricians and Gynecologists, and Centers for Disease Control and Prevention.
However, when providers were asked more broadly about care they delivered to “all women of reproductive age,” they often named individual elements of PCC, including contraceptive counseling, diabetes screening, and others.
I don’t think I’m aware of any specific guidelines, but there are certain things like um... if a woman has prediabetes or is a diabetic, you’re obviously going to counsel her…—Family Medicine physician, FQHC, Urban County.
There was awareness that specific elements of PCC should be delivered to patients of reproductive age. However, awareness of guidelines was low, which likely contributes to gaps in implementation of full recommendations.
Limited Preconception Patient Contact
Even when providers had confidence in their personal capability to provide PCC, they cited that patients often did not plan pregnancies or seek PCC per se, and thus felt less able to consistently deliver such care. Data contributing to this theme emerged from the codes “Beliefs about Capabilities” and “Memory, Attention, and Decision-Making.”
The greatest [barrier] probably would be on the patient side, the regularity with which they come in.”—Nurse practitioner, family planning clinic, Urban County.
However, providers did report providing elements of PCC when patients presented for well-woman visits or other preventive health care.
I would say that most of my patients do not come in for a visit specifically for preconception care, so I will catch this part of their care if they’re coming in for an annual exam.—Family Medicine physician, Private Practice, Rural County.
In other words, when discussing PCC abstractly, providers felt that patients not seeking care during the preconception period created a barrier, but they acknowledged that they did deliver PCC at annual or preventive visits.
Providers also perceived unplanned pregnancy as a barrier to PCC, citing that they often see patients after they become pregnant. When asked about PCC’s effectiveness, multiple providers cited that 50% of pregnancies are unplanned, implying that they are not able to provide PCC to patients who do not plan their pregnancies.
I’ve seen benefits from preconception planning, yes, but with some people, the only time you see them is already after the fact—then you’re already planning preconception planning for the next time they’re pregnant.—OBGYN, private practice, Urban County.
Some providers tried to elicit patients’ future pregnancy plans even when they presented for another type of visit so that PCC could be incorporated early.
…if somebody’s thinking about having a baby in the future—and this is something ongoing for me, because I see gynecology exams who then go ahead and get pregnant—so I do mention [PCC] a year or two ahead of time, if I can.—OBGYN, private practice, Urban County.
Despite feeling that PCC was challenging to implement as a discrete set of recommendations, the same providers found times to conduct screenings or counseling considered part of PCC. In other words, they provided elements of PCC without necessarily considering this to be PCC provision. This discordance contributed to pessimism around PCC feasibility and was consistent across clinical sites.
Pessimism About Patient “Compliance”
Despite expressing confidence in their ability to provide elements of PCC, providers perceived the effectiveness of PCC as dependent on patient follow-through; this often manifested as pessimism. Providers were concerned about (1) patient knowledge, (2) patient willingness to change behavior, and (3) patient ability to make changes amidst broader structural factors. TDF domains that generated this theme included “Beliefs about Consequences” and “Memory, Attention, and Decision-Making.”
Patient knowledge around reproductive health was seen as a challenge to providing PCC. Some perceived that PCC was a “foreign concept” to patients. Some believed that patients lacked an even broader understanding of pregnancy and reproduction.
…people [are] resistant to the idea cause they’re kind of in denial that they could get pregnant OBGYN physician, private practice, Dane County.
Additionally, some providers (though a minority of our sample) expressed paternalistic and damaging views about some patients.
Interviewer: What problems have you encountered when delivering preconception care in general?
Interviewee: Some of the tragedies of life, you know: uneducated, uninformed, poor individuals, lack of resources, lack of family support… the preconceptual planning is just so out of touch… the lives they’re living are so simplistic and basic and somewhat—for some people—almost animalistic, and the concept of preconception care, talking about birth control in general to them, is just very foreign. OBGYN physician, private practice, Urban County.
The OBGYN above is an extreme example, in which the provider frames some patients’ lifestyles as “animalistic.” Most providers in the sample did not use such language but many did imply that poor education or lack of knowledge affected their patients’ “compliance” with PCC recommendations. These assumptions—that some women will be noncompliant or are unable to manage their own health—perpetuates negative stereotypes about women of color, poor women, and others.
In addition, providers felt that some patients were simply unwilling to change their behavior. A lack of “motivation” to make lifestyle changes or “apathy” were cited as barriers to the success of PCC, or, as one provider said, “they just ignore you.” This was connected to examples of tobacco, alcohol, and weight loss.
We definitely can give patients information and advise them on what they should and shouldn’t be doing. However, once they leave the office, I’m not sure if they do all those things.—Nurse Practitioner, family planning clinic, Urban County.
I think probably the biggest problem would be an unwillingness to change a behavior.—Nurse Practitioner, family planning clinic, Urban County.
One provider related this to the concept of physician burnout, and thus to further pessimism about the impact of PCC:
[Providers] give recommendations but they may not be followed… I think the thing that most providers suffer the most from is, ‘if I really reach out and help, how do I know that that information or that help is going to actually be applied?’ Family medicine physician, private practice, Urban County
Many providers also acknowledged structural factors related to patients’ ability to change behavior, rather than their willingness alone. Providers felt that PCC effectiveness depended on patients’ socioeconomic situation and psychosocial stressors they faced, such as poverty and immigration status. For example, one provider acknowledged that the “time constraints pulled [patients] in many different directions with jobs and family” all constituted “roadblocks” for PCC. Lack of insurance coverage for PCC was mentioned by multiple providers. Together, these three related perceptions of patients and their knowledge, willingness, and structural context made providers feel pessimistic about PCC’s impact on health even when implemented in a clinical setting.
Scope and Style of Practice
Providers generally saw PCC as within their professional scope of practice; data related to this theme were coded with the TDF domain “Social Professional Role.” However, there was variability in how providers prioritized PCC and elements therein.
Within PCC, most providers expressed motivation to talk to all women of reproductive age about contraception. However, depression and IPV screening were generally spoken about as lower priorities, without the same motivation to implement them universally.
I do try to do [contraceptive counseling at] all of my visits where a woman is of childbearing age…. I try really, really hard at that.—Family medicine physician, FQHC, Urban County.
I think in theory [depression screening] sounds good, I think in practicality…I don’t know in a practical sense how well it’d work.—Family medicine physician, private practice, Urban County.
These examples demonstrate the tone many providers used when discussing these elements of PCC; providers were motivated to work toward universal contraceptive counseling but time constraints and other clinical priorities were cited as barriers to universal depression and IPV screenings.
Providers also framed PCC provision as antithetical to providing patient-centered care. Focusing on the patient’s goals was often raised as a reason that providers did not discuss aspects of PCC, given limited time and the desire to address the patient’s concerns. Providers were more likely to discuss aspects of PCC if patients presented for annual exams or other preventive care.
Sometimes you’re limited, you know, somebody comes in just for a cough, they don’t really want to have everything addressed Family medicine physician, FQHC, Urban County.
In these cases, the decision of whether to provide PCC was considered up to provider discretion and style. For these providers, focusing on patient goals was considered more important than provision of consistent PCC.
Clinical Site Policies
Some providers reported not delivering PCC due to clinic policies or structure, a theme that emerged from the TDF domain “Environmental Context.” At these sites, either (1) PCC services were not offered at all or (2) the services were offered to only a subset of patients. For example, one provider at a private practice said, “we just don’t really do [contraceptive counseling] here,” and another at a public health clinic said, “we don’t do screening for depression here.” Both were providers at clinical locations where patients of reproductive age seek primary or reproductive care, but elements of PCC were considered outside their scope of services.
In addition, providers who offered prenatal care tended to emphasize depression and IPV screening more with pregnant patients than non-pregnant patients, if not entirely limiting these screenings to pregnant patients. This practice was sometimes attributed to time constraints and the characterization of pregnant patients as more “high-risk.”
New OB visits are screened for depression as well, postpartum visits are screened, but somebody who comes in because they’re having burning with urination? No. OBGYN physician, private practice, Urban County.
I think—not quite sure—but I think it’s part of the questions that my nursing staff go through with my pregnant patients. And then, really I don’t screen anybody else routinely [for IPV]. Family medicine physician, private practice, Urban County.
In these cases, the barriers to PCC delivery were attributed to the policies of the clinic or established norms of practice and not the individual provider’s scope.
Patient-Provider Relationships
Within the TDF domain “Social Influences,” providers’ relationships with patients were often cited as reasons that depression and IPV screening were not necessary. Some providers felt that they knew their patients so well that they would be able to perceive if a patient was experiencing depression or violence.
A lot of it is more of an art. I don’t have—don’t know of a questionnaire specifically for [IPV screening], necessarily. But a lot of times with just talking to the patient you can kind of gauge. Family medicine physician, FQHC, Urban County.
Other providers explained that they look for physical or verbal signs of depression, violence, or trauma. For example, one provider said they listened for “hesitancy” in patients’ answers. Others noted a certain way they expected a patient experiencing IPV would respond to a physical exam.
I cannot tell you how many times I’ve found sexual abuse… watching them go off the table, just jumping off the table... in terror. So, I definitely don’t do a formalized [screening for IPV] but I think I do something even better... OBGYN physician, private practice, Urban County.
Like this provider, others supported their claims that they detected IPV through skills developed over many years of experience. In general, these “signs” were considered stand-ins for screenings and were relied on in the place of standardized protocols.
Some providers felt that they knew their patients well enough that they did not need to ask whether they were experiencing depression or violence:
Clearly after 30 years and having all the same patients, I know who are the at risk people [for depression]. Family medicine physician, private practice, Dane County.
I am not talking to my patient of 30 years about how often she’s being beaten by her husband. OBGYN physician, private practice, Urban County.
Another element of this reasoning was a feeling that patients would disclose this information without prompting.
I’m under the assumption, I suppose—and this is perhaps wrong—that my patients would tell me. Because I do have a very close relationship with most of my patients, and I feel like they tell me a lot of things… Family medicine physician, private practice, Rural County.
Generally, these providers used their perceived relationships with patients as reason to not conduct universal screening for depression or IPV, either because they expected to discern signs on their own, or because they expected patients to disclose without prompting.
Discussion
In this study of health care providers in diverse settings across Wisconsin, we found that despite perceived value and confidence in skills surrounding PCC, providers experienced numerous barriers to PCC implementation and its impact. Many of these barriers were common across outpatient clinical settings.
Our results echo previous findings within and outside the US, in which providers cite a lack of comprehensive programming, knowledge, and contact in the preconception period as barriers to PCC delivery (Heyes, 2004; M’hamdi et al., 2017), in addition to persistent ambiguity regarding which health care providers are responsible for PCC (Steel et al., 2016). Our findings shed light on this debate, with most in our sample considering PCC within their scope but varying in how much they prioritized actually delivering PCC services. Further, many included elements of PCC in their practice without considering this to be PCC provision, a discordance that may have contributed to the pessimism we observed around PCC feasibility.
In addition to themes that echo previous research, our findings elucidate additional factors. The intention to provide patient-centered care and perception of strong patient-provider relationships—both typically viewed positively—were characterized as reasons why PCC was not consistently provided. This was especially salient with regard to screenings for depression and IPV. Contrary to our participants’ perceptions, though, patients often do not disclose traumatic experiences without being prompted, and clinician reluctance to inquire about violence may in fact decrease likeliness of disclosure (Rodriguez et al., 1996; Halpern-Meekin et al., 2019).
Finally, this study demonstrated that many providers hold problematic assumptions regarding the patients they serve, their motivations, and “compliance”—a concept that in itself implies a paternalistic relationship between provider and patient and ignores the role of social and structural determinants of health and health-related behavior. These assumptions, likely rooted in biases, were often cited as challenges to PCC implementation. This finding is consistent with research that demonstrates that implicit bias shapes provider behavior and affects delivery of care (Chapman et al., 2013).
Limitations
This study has several limitations that should be noted. While our sample did include a variety of provider types in diverse clinical settings, the size does not allow us to draw thorough comparisons between these groups. We also had a high nonresponse rate. The relatively small number of rural participants likely resulted in findings biased towards perspectives of urban providers. Additionally, the scope and aim of this study represents only provider perspectives on PCC implementation; we did not evaluate patient perspectives, which are crucial to providing effective and patient-centered PCC.
Conclusions for Practice
There have been calls to improve practical guidance for PCC implementation, to which this study can contribute. In particular, our findings underscore the need for clarity about which health professionals should deliver PCC (Steel et al., 2016). Providers may benefit from expanding their understanding of what constitutes PCC and when PCC can and should be introduced. Given that PCC-specific visits are perceived by some as outside the norm of clinical offerings, providers may need to incorporate PCC into other encounters, as many in this study reported doing. We also identify a need for providers to examine their clinical skills around depression and violence screening. Further, we amplify the call for providers to understand how structural inequities may influence patient behavior, and to examine their own implicit and explicit biases and take action to address them within and outside of direct care provision. Providers should also reconsider the value of standardized screening, both within and beyond PCC. Given this constellation of challenges and barriers, expanding the care team and establishing or strengthening relationships with community organizations could be critical actions to improve PCC and support.
Data Availability
Upon request and with appropriate IRB approval.
Code Availability
Not applicable.
References
American College of Obstetricians and Gynecologists. (2019). ACOG Committee opinion No. 762: Prepregnancy counseling. Obstetrics and Gynecology, 133(1), e78–e89. https://doi.org/10.1097/AOG.0000000000003013
Atkins, L., Francis, J., Islam, R., O’Connor, D., Patey, A., Ivers, N., Foy, R., Duncan, E. M., Colquhoun, H., Grimshaw, J. M., Lawton, R., & Michie, S. (2017). A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implementation Science, 12(1), 77. https://doi.org/10.1186/s13012-017-0605-9
Braun, V., & Clarke, V. (2012). Thematic analysis. In H. Cooper, P. M. Camic, D. L. Long, A. T. Panter, D. Rindskopf, & K. J. Sher (Eds.), APA handbook of research methods in psychology, Vol 2: Research designs: Quantitative, qualitative, neuropsychological, and biological (pp. 57–71). American Psychological Association. https://doi.org/10.1037/13620-004
Chapman, E. N., Kaatz, A., & Carnes, M. (2013). Physicians and implicit bias: How doctors may unwittingly perpetuate health care disparities. Journal of General Internal Medicine, 28(11), 1504–1510. https://doi.org/10.1007/s11606-013-2441-1
Dean, S. V., Lassi, Z. S., Imam, A. M., & Bhutta, Z. A. (2014). Preconception care: Closing the gap in the continuum of care to accelerate improvements in maternal, newborn and child health. Reproductive Health, 11(Suppl 3), S1. https://doi.org/10.1186/1742-4755-11-S3-S1
Farahi, N., & Zolotor, A. (2013). Recommendations for preconception counseling and care. American Family Physician, 88(8), 499–506.
Frayne, D. J. (2017). Preconception care is primary care: A call to action. American Family Physician, 96(8), 3.
Halpern-Meekin, S., Costanzo, M., Ehrenthal, D., & Rhoades, G. (2019). Intimate partner violence screening in the prenatal period: Variation by state, insurance, and patient characteristics. Maternal and Child Health Journal, 23(6), 756–767. https://doi.org/10.1007/s10995-018-2692-x.
Heyes, T. (2004). Preconception care: Practice and beliefs of primary care workers. Family Practice, 21(1), 22–27. https://doi.org/10.1093/fampra/cmh106
Johnson, K., Posner, S. F., Biermann, J., Cordero, J. F., Atrash, H. K., Parker, C. S., Boulet, S., Curtis, M. G., CDC/ATSDR Preconception Care Work Group, & Select Panel on Preconception Care. (2006). Recommendations to improve preconception health and health care—United States. A report of the CDC/ATSDR Preconception Care Work Group and the select panel on preconception care. MMWR. Recommendations and Reports: Morbidity and Mortality Weekly Report. Recommendations and Reports, 55(RR-6), 1–23.
Kroelinger, C. D., Okoroh, E. M., Boulet, S. L., Olson, C. K., & Robbins, C. L. (2018). Making the case: The importance of using 10 key preconception indicators in understanding the health of women of reproductive age. Journal of Women’s Health, 27(6), 739–743. https://doi.org/10.1089/jwh.2018.7034
Lassi, Z. S., Dean, S. V., Mallick, D., & Bhutta, Z. A. (2014). Preconception care: Delivery strategies and packages for care. Reproductive Health, 11(Suppl 3), S7. https://doi.org/10.1186/1742-4755-11-S3-S7
M’hamdi, H. I., van Voorst, S. F., Pinxten, W., Hilhorst, M. T., & Steegers, E. A. P. (2017). Barriers in the uptake and delivery of preconception care: Exploring the views of care providers. Maternal and Child Health Journal, 21(1), 21–28. https://doi.org/10.1007/s10995-016-2089-7
Michie, S. (2005). Making psychological theory useful for implementing evidence based practice: A consensus approach. Quality and Safety in Health Care, 14(1), 26–33. https://doi.org/10.1136/qshc.2004.011155
Morgan, M. A., Hawks, D., Zinberg, S., & Schulkin, J. (2006). What obstetrician–gynecologists think of preconception care. Maternal and Child Health Journal, 10(S1), 59–65. https://doi.org/10.1007/s10995-006-0086-y
Posner, S. F., Johnson, K., Parker, C., Atrash, H., & Biermann, J. (2006). The national summit on preconception care: A summary of concepts and recommendations. Maternal and Child Health Journal, 10(5 Suppl), S197-205. https://doi.org/10.1007/s10995-006-0107-x
Robbins, C., Boulet, S. L., Morgan, I., D’Angelo, D. V., Zapata, L. B., Morrow, B., Sharma, A., & Kroelinger, C. D. (2018). Disparities in preconception health indicators—Behavioral risk factor surveillance system, 2013-2015, and pregnancy risk assessment monitoring system, 2013–2014. Morbidity and Mortality Weekly Report. Surveillance Summaries (Washington, D.C.: 2002), 67(1), 1–16. https://doi.org/10.15585/mmwr.ss6701a1
Rodriguez, M. A., Quiroga, S. S., & Bauer, H. M. (1996). Breaking the silence. Battered women’s perspectives on medical care. Archives of Family Medicine, 5(3), 153–158. https://doi.org/10.1001/archfami.5.3.153
Siu, A. L., US Preventive Services Task Force (USPSTF), Bibbins-Domingo, K., Grossman, D. C., Baumann, L. C., Davidson, K. W., Ebell, M., García, F. A. R., Gillman, M., Herzstein, J., Kemper, A. R., Krist, A. H., Kurth, A. E., Owens, D. K., Phillips, W. R., Phipps, M. G., & Pignone, M. P. (2016). Screening for depression in adults: US preventive services task force recommendation statement. JAMA, 315(4), 380–387. https://doi.org/10.1001/jama.2015.18392
Steel, A., Lucke, J., Reid, R., & Adams, J. (2016). A systematic review of women’s and health professional’s attitudes and experience of preconception care service delivery. Family Practice, 33(6), 588–595. https://doi.org/10.1093/fampra/cmw094
Temel, S., van Voorst, S. F., Jack, B. W., Denktaş, S., & Steegers, E. A. P. (2014). Evidence-based preconceptional lifestyle interventions. Epidemiologic Reviews, 36(1), 19–30. https://doi.org/10.1093/epirev/mxt003
US Preventive Services Task Force, Curry, S. J., Krist, A. H., Owens, D. K., Barry, M. J., Caughey, A. B., Davidson, K. W., Doubeni, C. A., Epling, J. W., Grossman, D. C., Kemper, A. R., Kubik, M., Kurth, A., Landefeld, C. S., Mangione, C. M., Silverstein, M., Simon, M. A., Tseng, C.-W., & Wong, J. B. (2018). Screening for intimate partner violence, elder abuse, and abuse of vulnerable adults: US preventive services task force final recommendation statement. JAMA, 320(16), 1678–1687. https://doi.org/10.1001/jama.2018.14741
van der Zee, B., de Beaufort, I., Temel, S., de Wert, G., Denktas, S., & Steegers, E. (2011). Preconception care: An essential preventive strategy to improve children’s and women’s health. Journal of Public Health Policy, 32(3), 367–379. https://doi.org/10.1057/jphp.2011.13
World Health Organization. (2013). Meeting to develop a global consensus on preconception care to reduce maternal and childhood mortality and morbidity: World Health Organization Headquarters, Geneva, 6–7 February 2012: Meeting report. World Health Organization.
Acknowledgements
Funding for this work was provided by the Herman and Gwendolyn Shapiro Foundation and the Population Research Infrastructure grant from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (P2C HD047873). The Social Sciences Computing Cooperative at the University of Wisconsin-Madison provided technological support. The authors thank Ann Vitous of the Center for Healthcare Outcomes and Policy at the University of Michigan for providing guidance on the Theoretical Domains Framework used in this analysis.
Funding
This research was supported by the Herman and Gwendolyn Shapiro Foundation at the University of Wisconsin-Madison and the Population Research Infrastructure grant from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (P2C HD047873).
Author information
Authors and Affiliations
Contributions
Dr. ECN recruited participants, conducted interviews, coded transcripts, drafted the initial manuscript, and reviewed and revised the final manuscript. Dr. MZG advised on the design of the analysis, coded transcripts, reviewed and contributed to themes, critically reviewed the manuscript for important intellectual content, and reviewed and revised the manuscript. Dr. MPT recruited participants, conducted interviews, coded transcripts, reviewed and contributed to themes, and reviewed and revised the final manuscript. Dr. DBE conceptualized the study, critically reviewed the manuscript for important intellectual content, and reviewed the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to disclose.
Ethical Approval
The study was deemed exempt by the University of Wisconsin–Madison Institutional Review Board.
Consent to Participate
All persons gave their informed consent prior to their inclusion in the study. Details that might disclose the identity of the subjects were omitted.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nacev, E.C., Greene, M.Z., Taboada, M.P. et al. Factors Influencing Provider Behavior Around Delivery of Preconception Care. Matern Child Health J 26, 1567–1575 (2022). https://doi.org/10.1007/s10995-022-03411-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-022-03411-8