Abstract
To describe the characteristics of infants with bilateral Stage 4b or 5 ROP (i.e. with subtotal or total retinal detachment) who presented to eye departments in two major cities in Mexico, to identify reasons why they may have become blind in order to recommend how programs could be improved. A large case-series of infants with Stage 4b or 5 ROP in both eyes confirmed by ultrasound who attended the ROP Clinic, Hospital Civil de Guadalajara from September 2010 to November 2012, and the Department of Ophthalmology, Hospital Infantil de Mexico Federico Gomez from December 2011 to December 2012 were identified from the diagnostic databases of each hospital. Mothers of infants in Guadalajara had a telephone interview. 89/94 eligible infants were included in the study, 48 in Guadalajara and 41 in Mexico City. Cases came from 22 of the 32 states in Mexico. Half of the infants attending Guadalajara 24/48 (50 %) had been cared for in NICUs without ROP screening programs and were not examined. Among the 24 infants cared for in NICUs with ROP programs, 7/24 (29.1 %) mothers reported that their infant had not been examined while in the NICU, and a further 9/24 (37.5 %) were either not referred for screening after discharge or they did not attend. Two infants had failed laser treatment. Strategies and resources to prevent end stage ROP have not been firmly established in Mexico. There is an urgent need to expand the coverage and quality of ROP programs, to ensure that existing screening guidelines are better adhered to, and to improve communication with parents.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Retinopathy of prematurity (ROP) is an important cause of potentially avoidable blindness in children, particularly in Latin America, Eastern Europe and the emerging economies of Asia [1]. Recent estimates suggest that 20,000 (15,500–27,200) survivors of preterm birth become blind from ROP each year with the largest number being in Asia [2]. Rates of ROP blindness per million live births are 2.5 times greater in Latin America than in high income countries, suggesting that much can be done to prevent visual impairment from ROP through interventions to reduce preterm birth [3], by improving neonatal care [4, 5] and by increasing the coverage and quality of programs for detecting and treating infants with severe acute ROP [6, 7]. In Mexico ROP is the commonest cause of avoidable blindness in children, having great economic and social impact [8], as it compromises the individual´s development and participation in productive life.
Progression to Stage 4b (subtotal retinal detachment) or Stage 5 ROP (total retinal detachment) can occur if infants are not screened or treated, or if peripheral laser treatment fails to control progression. To avoid these cases, high coverage with high quality ROP programs in units caring for preterm infants at risk is required. This entails the following steps in each unit: identifying all infants who need to be examined, using locally agreed, evidence based criteria, and timely examination of infants by an experienced ophthalmologist while they are still in the unit and after discharge, if required. Infants with severe ROP need urgent treatment with laser photocoagulation, or cryotherapy if laser is not available, with follow up and retreatment, if necessary. Evidence of the extent to which each of these steps is being implemented is often not monitored or reported, but there is some evidence that not all eligible infants have a first eye examination [9], and a relatively high proportion of infants fail to complete all examinations after discharge [7, 10]. Data from the clinical trials of treatment of severe ROP demonstrate that although treatment significantly improves structural and function outcomes, visual impairment cannot always be prevented [11, 12].
The Mexican national ROP guidelines recommend that infants with birth weight (BW) ≤1,750 gs or gestational age (GA) ≤34 weeks be examined [13] taking account of the risk in bigger, more mature infants in middle income settings [14]. Sicker, more mature infants should also be examined, at the discretion of the attending physician. A law has recently been passed in Mexico which makes eye examination of preterm infants mandatory [15].
A recent study undertaken in 32 neonatal units in five states in Mexico showed that a third of units had no program for detecting or treating ROP, and less than 20 % had programs which followed international norms. (Zepeda-Romero LC, Gilbert CE. Prevention of blindness from retinopathy of prematurity in Mexico. Quality of the neonatal care and characteristics of the ROP programs. London School of Hygiene and Tropical Medicine. Unpublished data, available at www.lshtm.ac.uk/library/MSc_CEH2010-11/100865.pdf). Almost half of the units had suboptimal programs i.e., infants were referred to eye clinics for examination or treatment, or were treated with anti-VEGF agents which are not yet of proven safety or long term efficacy [16, 17].
Mexico has a very complex medical insurance system. Approximately a third of the population is insured by the Mexican Institute of Social Security which is available to those in formal employment. A relatively small proportion is insured by schemes for civil servants, the Navy, the Army and people working in the oil industry. Only 0.4 % has private health insurance. Almost 40 % of the population are covered by the Popular Health Insurance which covers health care in government hospitals [18]. The latter includes the care of newborn babies but the scheme is not automatic as parents have to register their child. Neonatal care and treatment for severe ROP were included in this insurance scheme in 2007, resulting in a marked improvement in the survival of preterm infants [19]. Data from the 2012 census showed that 21.4 % of the population did not have access to any insurance [18].
The purpose of this study was to describe the characteristics of infants with bilateral Stage 4b or 5 disease who presented to two government eye departments in two major cities in Mexico, Guadalajara and Mexico City, to identify reasons why they may have become blind and to identify contributing factors in order to recommend how programs could be improved. Both hospitals are tertiary level referral hospitals for paediatric ophthalmology.
Materials and Methods
Infants with Stage 4b or 5 ROP in both eyes confirmed by ultrasound who attended the ROP Clinic of the Hospital Civil de Guadalajara from September 2010 to November 2012, or the Department of Ophthalmology Hospital Infantil de Mexico Federico Gomez in Mexico City from December 2011 to December 2012 were identified from the diagnostic databases of each hospital. The following information was extracted from the databases in both hospitals, which included details extracted from neonatal care discharge summaries: referral method and diagnosis at referral; the hospital the infant was born in and the level of services available; the neonatal intensive care unit (NICU) the infant attended prior to discharge, and length of stay in the NICU. The time interval between the mother first presenting to medical services because she had noticed a problem and age at the first consultation in the eye department were noted. The following data were collected in relation to the child: GA, BW, gender and singleton or multiple birth.
Contact information was not available for infants attending the clinic in Mexico City and the following additional information was collected by telephone interview with mothers of infants attending the Guadalajara ROP clinic and by reviewing hospital medical records: mother’s age, marital status, education and employment; number of pregnancies and whether the pregnancy with the study child was planned, whether the infant had an eye examination or was treated for ROP, what the mother was told about ROP and whether she was asked to bring her child back for examination after discharge from the NICU. Additional information for infants attending the Guadalajara clinic was also obtained from the neonatologist in charge of the NICU where the child had received care. The neonatologist was asked about the policies and practices in relation to ROP in their unit.
All data were recorded on a standard form, and entered into a database created in Microsoft Office Excel 2010. Data were analysed using SPSS version 21 for windows.
Ethical Considerations
The study abided by the principles of the Declaration of Helsinki. The protocol was approved by the hospitals’ Ethics Committees who did not require full ethical approval. Verbal consent to participate was obtained prior to interviews.
Results
A total of 94 infants with Stage 4b or 5 ROP in both eyes were identified: 53 attended the Guadalajara clinic and 41 were recruited in Mexico City. Five infants attending the Guadalajara clinic were excluded as they had incomplete histories and their families could not be contacted for interview. Data from the databases were therefore available for 89 infants, 48 of whom had additional information from interviews with mothers.
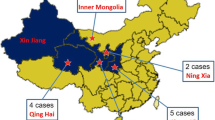
All Study Infants
The majority of the 89 infants were born in government maternity units, the remainder being born in private units (7.9 %). 19 % were twins. In the Mexico City sample, 49 % of infants lived outside the Federal District where Mexico City is located, and in the Guadalajara sample 87.5 % lived outside Jalisco state where Guadalajara is located. Infants came from 22 of the 32 states in Mexico (Fig. 1). There were more male infants in both hospitals, 70.8 % in Guadalajara and 65.9 % Mexico City. The median BW of the 89 infants was 1,232 ± 325 g and the median GA was 29.5 ± 2.5 weeks (Table 1). The majority of infants had BWs ≤1,500 g (85.3 %) or GAs ≤32 weeks (87.6 %). Only one infant born at 36 weeks with a BW of 2,000 g fell outside Mexican screening criteria. This infant had pulmonary hypertension, was treated with high frequency ventilation and was discharged on day 20. However, eight (8.9 %) weighed >1,750 g at birth and four (4.5 %) had a GA of more than 34 weeks.
Infants Attending the Eye Department in Guadalajara
Additional information about the mothers was only available from the 48 infants who attended the clinic in Guadalajara where mothers were interviewed (Table 2). The median age of mothers was 24 ± 7 years (15–39 years), 31 % were adolescents, 54 % were not married, 67 % had primary or middle school education and 90 % were unemployed. 19 % of mothers admitted that the pregnancy was not planned or desired.
Forty percent of infants in Guadalajara were discharged from a NICU unit classified by Mexico’s Health Department as tertiary level (Table 3) and the median stay in the NICU was 51 ± 25 days (9–120 days), with 17 % being discharged before 28 days of life. Most infants (45.8 %) were referred to the Guadalajara ROP clinic by a paediatrician but 27 % were self-referred by the parents who had noticed a problem i.e. their child did not smile in response to a smile. A total of 35 infants had been referred by clinicians. Twelve of the 13 referring ophthalmologists had diagnosed Stage 4 (subtotal detachment, extent not defined) or Stage 5 ROP. Diagnoses were less accurate by the 22 referring paediatricians: three diagnosed Stage 4 (as above) or Stage 5 ROP and two had a diagnosis of retinal detachment. Other diagnoses/reasons for referral were for ROP screening (two infants), Stage 1 ROP (two infants), congenital glaucoma (four infants) and microphthalmos (two infants). In a further four cases ROP was suspected and two were referred without a diagnosis. Overall, Stage 4 (as above) or 5 ROP were correctly diagnosed in 13/35 (37 %) of the infants referred by clinicians.
Half the infants in Guadalajara (24, 50 %) had received care in NICUs without ROP programs and were not examined (Fig. 2). The majority of the infants admitted to secondary level facilities (14/15) were not examined as these NICUs did not have a program. Among the 24 infants cared for in NICUs with ROP programs, 7/24 (29.1 %) mothers reported that their infant had not been examined while an inpatient, and a further 9 (37.5 %) were either not referred for screening after discharge or they did not attend follow up appointments. Seven infants had been treated for ROP: two (8.3 %) had undergone laser photocoagulation and failure of treatment had been documented; two (8.3 %) had late laser photocoagulation because treatment was not available in the city where they lived and they had been referred to different cities before treatment could be provided. Three infants (12.5 %) had been inappropriately treated with topical beta blockers or steroids (Table 4).
During the NICU stay, less than a quarter (23 %) of mothers said they received any information about the risk of blindness due to ROP.
Discussion
In this study 94 infants with end stage ROP presented to two eye units in tertiary referral hospitals in two cities in Mexico over a total recruitment period of 40 months i.e. an average of more than two infants per month. Many had been born and cared for in other States in Mexico, particularly infants attending the Guadalajara ROP clinic where almost 90 % had been born outside Jalisco State. Some of these mothers had travelled by bus for more than 24 h. The low number presenting from Jalisco State probably reflects the fact the Guadalajara city, where the majority of level 3 neonatal units are located, has a very good ROP program. In both hospitals boys outnumbered girls, which may reflect gender differences in rates of preterm birth as well as in the incidence and severity of ROP, but differences in health seeking behaviour may also be a factor [20].
The BW and GA of the 91 infants with adequate data for inclusion in this study are similar to those with end-stage ROP in studies from other middle income countries, where larger, more mature infants are affected than in industrialized countries i.e., in Russia [21] and India [22]. However, our cases were more mature than a large case series from the USA [23].
Focussing on the 48 infants recruited in Guadalajara, despite regulations making examination of preterm infants mandatory in Mexico, 50 % of infants had been cared for in NICUs without ROP programs, over half of whom had been cared for in secondary level NICUs. These findings are supported by the earlier study undertaken in 32 NICUs across Mexico (Zepeda-Romero LC, Gilbert CE. Prevention of blindness from retinopathy of prematurity in Mexico. Quality of the neonatal care and characteristics of the ROP programs. London School of Hygiene & Tropical Medicine. Unpublished data, available at www.lshtm.ac.uk/library/MSc_CEH2010-11/100865.pdf). More needs to be done to improve the coverage of programs in Mexico, including secondary level units. Barriers to the expansion of programs include the concentration of ophthalmologists in large cities and screening for and treating ROP is time consuming, entailing opportunity costs. An additional factor is that residency programs in Mexico do not include training in ROP which means junior ophthalmologists do not develop skills or interest in ROP. For ophthalmologists willing to screen and treat, accessing financial support for equipment and salaries through insurance schemes is also challenging. Although treatment of ROP is included in the federal Ministry of Health’s budget designed to reduce catastrophic health expenditure, reimbursement can be slow and disbursement within the hospital is discretionary. As a consequence programs are often run on a voluntary basis, with lack of continuity, or neonatologists hire ophthalmologists to run programs to reduce the risk of medico-legal action.
Almost a third of the infants in Guadalajara (17/48; 35.4 %) were cared for in NICUs with ROP programs but they were either not examined despite being eligible, or mothers did not bring their child back for examination after discharge, or the infant fell outside the Mexican screening criteria. In this study eight infants with BWs >1,750 g were not examined despite having GAs within the screening criteria. The finding that eligible infants slip through the net has been reported in other studies [9, 24]. To reduce this risk, clear protocols are required for staff who identify infants requiring examination, delineating who is responsible for documenting and communicating information to the examining ophthalmologist and to mothers/other carers.
In this study a high proportion of mothers were unmarried, poorly educated and had higher levels of unemployment than the national average for Mexico (5 %) [25]. Similar characteristics were found among 277 mothers of infants who were screened in the NICU in Hospital Civil de Guadalajara: mean age 24.7 ± 7.2 years; 64 % were not married; 81.4 % had attended primary school but had not completed middle school and 93 % were unemployed (Garnica-Garcia E, Zepeda-Romero LC. Factores de riesgo para retinopatia quirurgica del prematuro en el OPD Hospital Civil de Guadalajara 2005–2009. Unpublished data). These characteristics reflect the population attending this government hospital. Communication strategies need to take this vulnerable group of mothers into account. Discharge summary forms should include whether an eye examination is required after discharge, and this information needs to be communicated verbally and in writing to mothers/carers. Another approach is to ensure that infants are examined prior to discharge from the NICU even is this means the first examination is before 28 days of life, allowing infants with mature retinal vasculature to be discharged.
Only one infant with a difficult clinical course and early discharge receiving care in a secondary level NICU was not examined as it fell outside the BW/GA Mexican screening criteria. However, the guidelines recommend that more mature infants are examined at the discretion of the paediatrician if they have had an unstable clinical course. Although no conclusions can be drawn from this one case, screening criteria may need to be revised for secondary level facilities where levels of care are likely to be lower than in tertiary level NICUs, putting more mature infants at risk. However, having different criteria for different levels of care may cause confusion. Paediatricians and neonatologists need to be made more aware of these additional “sickness” criteria.
Four infants had been treated with laser but had poor outcomes. In two infants this was because treatment had been given too late as the infants were transferred to hospitals in different cities before treatment could be provided. To avoid these delays, a register is required of hospitals which can treat ROP until this care becomes more widely available. As a means of addressing the shortfall of ophthalmologists skilled in laser treatment for ROP in India, some States Ministries of Health support treatment by private practitioners, which is endorsed by the National Program for the Control of Blindness. This approach has the potential to increase the number of infants who can be treated.
Three infants had been given inappropriate treatment by ophthalmologists, and levels of awareness of ROP was low amongst referring paediatricians. More needs to be done to improve awareness of ROP amongst paediatricians in Mexico, through publications, presentations and engaging professional societies. To improve knowledge and skills amongst ophthalmologists, ROP should be included in all ophthalmology residency programs.
Despite being a major cause of avoidable blindness in children, control of ROP is not yet a priority in Mexico [15]. The circumstances of the cases reported in this paper reflect a fragmented health system and disorganized institutions and programs. A way forward would be to support the development of more regional ROP centres of excellence across Mexico, to provide local leadership for program development and to ensure quality control. Advocacy is required so that ophthalmologists receive salary support for screening and treating ROP within government services rather than depending on unreliable reimbursement. Indeed, there are powerful economic arguments for preventing blindness from ROP. In Peru, for example, the societal life time cost of blindness avoided has been estimated at almost $200,000 per child. Other studies have demonstrated that screening and treatment of ROP is highly cost effective [26–29], and in Brazil it has been estimated that including ROP programs in Ministry of Health services for neonatal care would only increases the cost of care of preterm infants by 10 % [30].
The ideal approach is for ROP programs to become embedded within national health systems but this can be challenging in countries where there is an absolute lack of ophthalmologists, or an inadequate number skilled in laser treatment. An alternative approach which has led to expansion of programs in India entails screening by trained technicians who transport a portable wide-field digital imaging system (RetCam, Clarity) to the neonatal unit. The technicians are trained to take and interpret the images, and to make management decisions, or they upload images for remote reading by ROP experts. Ophthalmologists are only request to visit the NICU to examine infants when high risk ROP is detected. In this program in Karnataka State 80 neonatal unis are visited every week by four teams (KID-ROP, http://www.kidrop.org). The program has a competency based training program for technicians, who require 30–90 training days to reach the minimum and maximum levels of competency [31]. Retinal imaging with or without telemedicine is becoming widespread, and a recent study in the United States of America confirms that trained non-clinical personnel can detected ROP requiring referral by remote reading of digital images with high degrees of validity [32]. High levels of skill and competency are possible [33, 34]. However, a current limitation to screening using digital cameras is the lack of a high quality, wide field system which is affordable as the only available camera (RetCam) is very expensive [35].
Limitations of this study are the possibility of recall bias by mothers who were interviewed, but the period of recall was not long as the median interval between discharge and consultation was 3 months. It is possible that some infants receiving care in units with ROP programs were examined but the mother did not know either because she was not told, or she did not understand what was being communicated or its importance. All facility based studies are prone to selection bias as not all infants developing end stage ROP will present to government facilities as some may present to private ophthalmologists. However, the characteristics of the mothers in this study were very similar to those of an earlier study, reflecting the population of mothers whose infants receive care in the government system in Mexico.
References
Gilbert, C. E., Fielder, A., Gordillo, L., Quinn, G., Semiglia, R., Vinsintin, P., et al. (2005). International No-ROP group characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: implications for screening programs. Pediatrics, 115, 518–525.
Blencowe, H., Lawn, J. E., Vazquez, T., Fielder, A., & Gilbert, C. (2013). Preterm-associated visual impairment and estimates of retinopathy of prematurity at regional and global levels for 2010. Pediatric Research, 74(Suppl 1), 35–49.
Born too soon: The global action report on preterm birth. Available at: http://www.who.int/pmnch/media/news/2012/borntoosoon_chapter2.pdf. Accessed 30 Sep 2013.
Gordillo, L., Villanueva, A. M., & Quinn, G. E. (2012). A practical method for reducing blindness due to retinopathy of prematurity in a developing country. Journal of Perinatal Medicine, 40, 577–582.
Quinn, G. E., Gilbert, C. E., Darlow, B. A., & Zin, A. (2010). Retinopathy of prematurity: An epidemic in the making. Chinese Medical Journal (England), 123, 2929–2937.
Darlow, B. A., Gilbert, C. E., & Quiroga, A. M. (2013). Setting up and improving retinopathy of prematurity programs: Interaction of neonatology, nursing, and ophthalmology. Clinics in Perinatology, 40, 215–227.
Jalali, S., Anand, R., Kumar, H., Dogra, M. R., Azad, R., & Gopal, L. (2003). Programme planning and screening strategy in retinopathy of prematurity. Indian Journal of Ophthalmology, 51, 89–99.
Zepeda-Romero, L. C., Barrera de Leon, J. C., Camacho-Choza, C., Gonzalez Bernal, C., Camarena-Garcia, E., Diaz-Alatorre, C., et al. (2011). Retinopathy of prematurity as a major cause of severe visual impairment and blindness in children in schools for the blind in Guadalajara city, Mexico. The British Journal of Ophthalmology, 95(11), 1502–1505.
Zin, A. A., Moreira, M. E., Bunce, C., Darlow, B. A., Gilbert, C. E., et al. (2010). Retinopathy of prematurity in 7 neonatal units in Rio de Janeiro: Screening criteria and workload implications. Pediatrics, 126, e410–e417.
Henderson, M. T., Wang, S. K., & Moshfeghi, D. M. (2013). A new paradigm for incorporating the joint statement screening guidelines for retinopathy of prematurity into clinical practice: Outcomes from a quaternary referral program. Ophthalmic Surgery Lasers and Imaging Retina, 44, 442–447.
Good, W. V. (2004). Early treatment for retinopathy of prematurity cooperative group. Final results of the early treatment for retinopathy of prematurity (ETROP) randomized trial. Transactions of the American Ophthalmological Society, 102, 233–250.
Palmer, E. A., Hardy, R. J., Dobson, V., Phelps, D. L., Quinn, G. E., & Summer, C. G. (2005). 15-year outcomes following threshold retinopathy of prematurity: Final results from the multicenter trial of cryotherapy for retinopathy of prematurity. Archives of Ophthalmology, 123, 311–318.
Manejo de la Retinopatía del Recién Nacido Prematuro. Lineamiento Técnico. México 2010. ISBN - 978-970-721-441-5. Available at: http://www.v2020la.org/docs/lineamiento/Lineamiento-ROP-SSA-2007.pdf. Data Accessed 2 July 2014.
Gilbert, C. E., Fielder, A., Gordillo, L., Quinn, G. E., Semiglia, R., Vinsintin, P., et al. (2005). Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: implications for screening programs. Pediatrics, 115, e518–e525.
Diario Oficial de la Federación, Available at: http://www.dof.gob.mx/nota_detalle.php?codigo=5285817&fecha=25/01/2013. Data Accessed 15 June 2014.
Darlow, B. A., Ells, A. L., Gilbert, C. E., Gole, G. A., Quinn, G. E., et al. (2013). Are we there yet? Bevacizumab therapy for retinopathy of prematurity. Archives of Disease in Childhood. Fetal and Neonatal Edition, 98, F170–F174.
Zepeda-Romero, L. C., Liera-Garcia, J. A., Gutiérrez-Padilla, J. A., Valtierra-Santiago, C. I., & Avila-Gómez, C. D. (2010). Paradoxical vascular-fibrotic reaction after intravitreal bevacizumab for retinopathy of prematurity. Eye (London), 24, 931–933.
Gutiérrez, J. P., & Hernández-Ávila, M. (2013). Cobertura de protección en salud y perfil de la población sin protección en México, 2000–2012. Salud Publica de Mexico, 55(2), S83–S90.
Profit, J., Lee, D., Zupancic, J. A., Papile, L., Gutierrez, C., Goldie, S. J., et al. (2010). Clinical benefits, costs, and cost-effectiveness of neonatal intensive care in Mexico. PLoS Medicine, 7(12), e1000379.
Yang, M. B., Donovan, E. F., & Wagge, J. R. (2006). Race, gender, and clinical risk index for babies (CRIB) score as predictors of severe retinopathy of prematurity. Journal of American Association for Pediatric Ophthalmology and Strabismus, 10, 253–261.
Shah, P. K., Narendran, V., Kalpana, N., & Tawansy, K. A. (2009). Anatomical and visual outcome of stages 4 and 5 retinopathy of prematurity. Eye (London), 23, 176–180.
Bhende, P., Gopal, L., Sharma, T., Verma, A., & Biswas, R. K. (2009). Functional and anatomical outcomes after primary lens-sparing pars plana vitrectomy for Stage 4 retinopathy of prematurity. Indian Journal of Ophthalmology, 57, 267–271.
Cusick, M., Charles, M. K., Agrón, E., Sangiovanni, J. P., Ferris, F. L, 3rd, & Charles, S. (2006). Anatomical and visual results of vitreoretinal surgery for stage 5 retinopathy of prematurity. Retina, 26, 729–735.
Urrets-Zavalia, J. A., Crim, N., Knoll, E. G., Esposito, F. A., Collino, E., Urrets-Zavalia, M. E., et al. (2012). Impact of changing oxygenation policies on retinopathy of prematurity in a neonatal unit in Argentina. British Journal of Ophthalmology, 96, 1456–1461.
INEGI resultados de encuesta nacional de ocupacion y empleo. www.inegi.org.mx/inegi/contenidos/espanol/prensa/comunicados/estrucbo/pdf.
Yanovitch, T. L., Siatkowski, R. M., McCaffree, M., & Corff, K. E. (2006). Retinopathy of prematurity in infants with birth weight > or = 1250 grams-incidence, severity, and screening guideline cost-analysis. Journal of American Association for Pediatric Ophthalmology and Strabismus, 10(2), 128–134.
Kamholz, K. L., Cole, C. H., Gray, J. E., & Zupancic, J. A. (2009). Cost-effectiveness of early treatment for retinopathy of prematurity. Pediatrics, 123(1), 262–269.
Brown, G. C., Brown, M. M., Sharma, S., Tasman, W., & Brown, H. C. (1999). Cost-effectiveness of treatment for threshold retinopathy of prematurity. Pediatrics, 104(4), e47.
Dunbar, J. A., Hsu, V., Christensen, M., Black, B., Williams, P., & Beauchamp, G. (2009). Cost-utility analysis of screening and laser treatment of retinopathy of prematurity. Journal of American Association for Pediatric Ophthalmology and Strabismus, 13(2), 186–190.
Zin, A., Magluta, C., Pinto, M., Entringer, A., de Sousa Mendes Gomes, M., Lopes Moreira, M., & Gilbert, C. (2014). Retinopathy of prematurity screening and treatment cost in Brazil. Revista Panamericana de Salud Pública = Pan American Journal of Public Health, 36(1), 37–43.
Vinekar, A., Gilbert, C. E., Dogra, M., Kurian, M., Shainesh, G., Shetty, B., et al. (2014). The KIDROP model of combining strategies for providing retinopathy of prematurity screening in underserved areas in India using wide-field imaging, tele-medicine, non-physician graders and smart phone reporting. Indian Journal of Ophthalmology, 62, 41–49.
Quinn, G. E., Ying, G. S., Daniel, E., Hildebrand, P. L., Ells, A., Baumritter, A., et al. (2014). Validity of a telemedicine system for the evaluation of acute-phase retinopathy of prematurity. JAMA Ophthalmology,. doi:10.1001/jamaophthalmol.2014.1604.
Fijalkowski, N., Zheng, L. L., Henderson, M. T., Wallenstein, M. B., Leng, T., Moshfeghi, D. M., et al. (2013). Stanford university network for diagnosis of retinopathy of prematurity (SUNDROP): Four-years of screening with telemedicine. Current Eye Research, 38, 283–291.
Photographic Screening for Retinopathy of Prematurity (Photo-ROP) Cooperative Group, Balasubramanian, M., Capone, A, Jr, et al. (2006). The photographic screening for retinopathy of prematurity study (Photo-ROP): Study design and baseline characteristics of enrolled patients. Retina, 26, S4–S10.
Trese, M. T. (2008). What is the real gold standard for ROP screening? Retina, 28, S1–S2.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zepeda-Romero, L.C., Meza-Anguiano, A., Barrera-de León, J.C. et al. Case Series of Infants Presenting with End Stage Retinopathy of Prematurity to Two Tertiary Eye Care Facilities in Mexico: Underlying Reasons for Late Presentation. Matern Child Health J 19, 1417–1425 (2015). https://doi.org/10.1007/s10995-014-1648-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-014-1648-z