Abstract
Duchenne muscular dystrophy (DMD) is a degenerative skeletal muscle disease that makes walking and breathing difficult. DMD is caused by an X-linked (Xp21) mutation in the dystrophin gene. Dystrophin is a scaffolding protein located in the sarcolemmal cytoskeleton, important in maintaining structural integrity and regulating muscle cell (muscle fiber) growth and repair. Dystrophin deficiency in mouse models (e.g., mdx mouse) destabilizes the interface between muscle fibers and the extracellular matrix, resulting in profound damage, inflammation, and weakness in diaphragm and limb muscles. While the link between dystrophin deficiency with inflammation and pathology is multi-factorial, elevated oxidative stress has been proposed as a central mediator. Unfortunately, the use of non-specific antioxidant scavengers in mouse and human studies has led to inconsistent results, obscuring our understanding of the importance of redox signaling in pathology of muscular dystrophy. However, recent studies with more mechanistic approaches in mdx mice suggest that NAD(P)H oxidase and nuclear factor-kappaB are important in amplifying dystrophin-deficient muscle pathology. Therefore, more targeted antioxidant therapeutics may ameliorate damage and weakness in human population, thus promoting better muscle function and quality of life. This review will focus upon the pathobiology of dystrophin deficiency in diaphragm and limb muscle primarily in mouse models, with a rationale for development of targeted therapeutic antioxidants in DMD patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Pathophysiological significance of dystrophin deficiency
Duchenne muscular dystrophy (DMD) is a severe, genetically-linked pathological disorder that imparts damage, necrosis, fibrosis, and weakness while impeding repair. DMD is caused by an X-linked genetic mutation or deletion of the scaffolding protein dystrophin, which is part of the sarcolemmal dystrophin-glycoprotein complex (DGC). Dystrophin is particularly susceptible to mutations due to its large size (2.5 Mb), and thus the incidence of DMD is high, affecting over 1 in every 3,500 males. The mutated dystrophin protein may result in compromised attachment to the DGC, limited attachment, or complete absence of the protein. In humans, the mutation that prevents the production of any functional dystrophin leads to a severe and highly morbid myopathy, DMD, whereas reductions or truncations of dystrophin protein that retains some function usually lead to a more benign myopathy, Becker muscular dystrophy, where expected lifespan is a nearly normal, but this varies from individual to individual.
Myopathy in patients suffering from DMD is especially critical for respiratory (e.g., diaphragm) and limb muscles. The symptoms of DMD first develop between 2–5 years of age, particularly in lower limb muscles, contributing to problems with balance and ambulation. Limb muscles show marked pseudo-hypertrophies in the early stage of DMD while muscles become highly susceptible to contraction-induced damage and progressively weaker (Lynch 2004). In addition, respiratory muscles, including the diaphragm, become fibrotic and weak. Patients typically need mechanical ventilator assistance and are no longer able to walk on their own in more advanced stage of DMD (Escolar and Scacheri 2001). The progression of DMD is severe and catastrophic, whereby respiratory or cardiovascular failure leads to premature mortality by the early to mid-twenties (Yiu and Kornberg 2008; Escolar and Scacheri 2001).
The murine X-linked muscular dystrophy (mdx) mouse strain is the most widely used animal model for DMD. Although both mdx and DMD are genetically homologous and characterized by a complete absence of dystrophin, the mdx mice show less severe muscular dystrophy than DMD in humans. Typically, limb muscles in mdx mice undergo a series of necrosis, inflammation, and degeneration starting postnatal at 2–3 weeks, with a substantial inflammatory and necrotic phase peaking at 4 weeks of age (Spencer et al. 2000; Grounds and Torrisi 2004). However, most of necrotic fibers in mdx mice are compensated for by a vigorous regeneration from 3–12 months of age (Pastoret and Sebille 1995). A second, progressive necrotic phase in limb muscles where the necrotic process persisted, but regeneration declined begins around 13 months (Pastoret and Sebille 1995). Moreover, muscle function is compromised. For example, specific force of skeletal muscles of the mdx mice is about average 25 % less than that of the age-matched control and normalized power output is about average 33 % less (Lynch et al. 2001).
In contrast, the diaphragm muscle in mdx mice displays progressive degeneration and ineffective regeneration resulting in muscle fiber loss, inflammation and fibrosis throughout the lifespan. The diaphragm muscle in mdx mice fails to restore muscle structure and function comparable to the clinical symptoms observed in DMD limb muscle (Stedman et al. 1991; Dupont-Versteegden and McCarter 1992; Lynch et al. 1997). The normalized force and power generation of diaphragm in adult mdx mice (4–6 month old) is decreased by 40 and 54 %, and old mdx (24-month old) mice is reduced by 52 and 69 % compared with age-matched wild type mice (Lynch et al. 1997). The degree of dystrophic pathology in mdx mice eventually leads to early mortality. The average mortality in mdx mice is about 21.5 months for male and 22.5 months for female, representing a 19 (male) and 17 % (female) reduction compared with wild type mice, respectively (Chamberlain et al. 2007). The mechanisms underlying inflammation and impaired muscle function during the necrotic and fibrotic phases have been a focus of research in dystrophin deficient mice in the diaphragm muscle with some relevance to human DMD patients (Stedman et al. 1991).
Skeletal muscles in mdx mice display a lower threshold for material fatigue and Ca2+-mediated injury in response to repeated stretch or eccentric contraction (Childers et al. 2002; Warren et al. 1993). As immune cell invasion and muscle injury result in massive inflammation, apoptosis, necrosis, and damage (Spencer and Tidball 2001; Sussman 2002), repeated damage and repair cycling, coupled with inflammatory mediators (TNF-α, NF-κB, TGF-ß), elicit accumulation of connective tissue or “fibrosis” (Spencer and Tidball 2001; Sussman 2002; Hartel et al. 2001). As a result stiffness and thus internal work are elevated (Hartel et al. 2001; Disatnik and Rando 1999; Matsumura and Campbell 1994; Rando 2001a; Sandri and Carraro 1999). Muscle degeneration with dystrophin deficiency in mdx mice is primarily a function of muscle protein breakdown and muscle fiber loss, and less a result of impaired protein production (Badalamente and Stracher 2000).
Dystrophin deficiency and dystrophin-glycoprotein complex (DGC)
Dystrophin deficiency leads to a marked reduction in expression of dystrophin, sarcolemmal, and subsarcolemmal proteins in the dystrophin-glycoprotein complex (DGC) (Grady et al. 1999; Matsumura and Campbell 1994; Chang et al. 1996; Brenman et al. 1995). The DGC plays a major role in linking the actin cytoskeleton to the extracellular matrix, thus stabilizing the sarcolemma during contraction and relaxation (Kosek and Bamman 2008). The DGC transmits forces or “loads” generated in the muscle sarcomeres to extracellular matrix and integrates cell signaling in response to mechanical strain (Kosek and Bamman 2008). The DGC includes α-, ß-dystroglycan, α-, ß-, γ-, ∂-sarcoglycan subunits, biglycan, the scaffolding proteins dystrophin, dystrobrevin, utrophin, syncoilin, Grb2, dysferlin, α-, ß-syntrophin, and the mu-splice variant of neuronal nitric oxide synthase (nNOS). The DGC is also associated with structural caveolae domain proteins including caveolin-3, and dysferlin in the sarcolemma. The DGC is anchored by α-dystroglycan binding to laminin-2, while β-dystroglycan attaches to α-dystroglycan and the C-terminal of dystrophin. Indeed, targeted deletion of ß-dystroglycan in mice results in embryonic death rather than progressive muscle damage, indicating that ß-dystroglycan is indispensable for early embryonic development (Williamson et al. 1997).
The cytoplasmic portion of the DGC includes α- and ß-syntrophin, dystrobrevins, nNOS, and dystrophin. Syntrophins bind directly to dystrophin, utrophin, and dystrobrevin, with their interaction mediated by cooperative action of the PH2 and SU COOH-terminal binding domains (Adams et al. 2000). The α1-syntrophin, localized on the sarcolemma and neuromuscular junction with dystrophin, is predominantly expressed in skeletal and cardiac muscle, whereas β1- and β2-syntrophin are expressed in wide variety of tissues (Kameya et al. 1999; Peters et al. 1997). The α1-syntrophin also binds to voltage-gated sodium channels and nNOS via the PDZ domain. Syntrophin-null mice have selective loss of nNOS, but not muscular dystrophy (Miyagoe-Suzuki and Takeda 2001). Thus, α1-syntrophin is of major importance in anchoring nNOS to the sarcolemma via dystrophin or dystrobrevin.
Dystrobrevins are also important components of DGC and form an intracellular subcomplex in the vicinity of the sarcolemma, with two dystrobrevin isoforms α and β encoded by different genes. Dystrobrevins are thought to serve as a scaffold for signaling proteins, and, like dystrophin, bind to nNOS through α- and ß-syntrophins. The α-dystrobrevin, localized near the sarcolemma and neuromuscular junction, is the predominant isoform in skeletal muscle (Jones et al. 2003). The β-dystrobrevin is expressed in brain, liver, lung and kidney, but not in skeletal muscle (Hoshino et al. 2002). The N-terminal half of α-dystrobrevin participates in association with the sarcoglycan-sarcospan complex (Yoshida et al. 2000). The α-dystrobrevin isoform also binds both dystrophin and syntrophin in skeletal muscle. Lack of dystrobrevin results in milder muscle pathology compared to the DMD patients (Jones et al. 2003; Grady et al. 1999).
Nitric oxide (NO•), generated from l-arginine by nitric oxide synthase (NOS), is an important and highly versatile signaling modulator involved in regulation of numerous cellular physiological and pathological processes: muscle contractility, metabolism, glucose uptake, satellite cell activation, hypertrophy, atrophy, injury, and repair (Kaminski and Andrade 2001; Chen et al. 2008). In mammals, three isoforms of NOS, neuronal (nNOS, NOS1), inducible (iNOS, NOS2), and endothelial (eNOS, NOS3), are expressed under normal conditions. The mu (μ)-splice variant of nNOS is a predominant isoform and key signaling protein expressed in muscle, where nNOSμ is normally co-localized at the sarcolemma within the DGC (Brenman et al. 1996; Wakayama et al. 1997). nNOSμ is anchored to the sarcolemmal cytoskeleton by binding of a PDZ motif at its N-terminus to α-syntrophin or ß-syntrophin, which in turn are bound to dystrophin or dystrobrevin (Rando 2001a; Jones et al. 2003). nNOSμ may be thus associated with dystrophin indirectly through its interaction with α1-syntrophin (Wakayama et al. 1997). However, recent evidence indicates that dystrophin carrying spectrin-like repeats 16 and 17 plays a direct role in nNOS recruitment to the sarcolemma (Lai et al. 2009). Further studies of the molecular mechanisms by which dystrophin, syntrophin, and nNOS are regulated are required.
In the absence of dystrophin in both DMD humans and mdx mice, nNOS is absent from sarcolemma and partially accumulates in the cytosol where it maintains its enzymatic activity (Chang et al. 1996; Brenman et al. 1995). Dislocation or translocation of nNOS from the dystroglycan complex may enhance myopathy via (a) elevation of NAD(P)H oxidase activity, (b) increased inflammation, (c) increased protein degradation via activation of ubiquitin ligases, and (d) impaired satellite cell activation (Nguyen and Tidball 2003; Tidball and Wehling-Henricks 2007). Reduction in nNOS coupled with increased susceptibility to material fatigue injury exacerbates damage and inflammation (Tidball and Wehling-Henricks 2007). While the loss of nNOS from the sarcolemma is not requisite in rendering a dystrophic phenotype, it is contributory to tissue damage (Rando 2001b).
Wehling et al. (Wehling et al. 2001) found that a muscle-specific nNOS transgene in mdx mice attenuated muscular dystrophy. They suggested that the loss of nNOS from sarcolemma in dystrophin-deficient muscles exacerbates membrane damage and inflammation. Although enhancing NO• production in muscle suffering from DMD can ameliorate muscle pathology (Wehling et al. 2001) and nNOS deficiency can lead to recurrent ischemia–reperfusion injury (Rando 2001b), the relationship between NO• and dystrophic pathology is complex. Previous studies demonstrated that mice lacking NO• production (Chao et al. 1998; Crosbie et al. 1998) or α-1 syntrophin (Kameya et al. 1999) do not develop a muscular dystrophy. However, these findings are consistent with Rando’s “two-hit hypothesis”, where the lack of nNOS exacerbates pathology in the presence of other defects associated with dystrophin-deficiency (Rando 2001b).
Caveolin-3 is a small sarcolemmal protein located in caveolae, invaginations central to growth and insulin signaling (Fecchi et al. 2006). Caveolin-3 binds to DGC proteins including ß-dystroglycan and nNOS, and inhibits nNOS via distinct scaffolding domains (Whitehead et al. 2008; Sunada et al. 2001). Caveolin-3 also binds to transient receptor potential channel 1 (TRPC1), a stretch-activated Ca2+ channel (Gervasio et al. 2008). Either upregulation or suppression via genetic ablation of caveolin-3 exacerbates DMD or causes limb-girdle muscular dystrophy (LGMD-1C) (Galbiati et al. 2001). Caveolin-3 may regulate DGC assembly and thus can contribute to loss of DGC proteins from the sarcolemma with dystrophin deficiency (Allen et al. 2010; Galbiati et al. 2001; Venema et al. 1997).
Dystrophin deficiency and inflammation
Mounting evidence indicates that inflammatory processes are highly integrated into the pathologies of dystrophin-deficient muscle (Hnia et al. 2008; Spencer and Tidball 2001). Indeed, the complex pathology of dystrophin deficiency is strongly related to infiltration of immune cells in response to the damage and degeneration (Hodgetts et al. 2006; Spencer et al. 2001). The inflammatory process in dystrophic-deficient muscle involves a unique invasion of autoreactive immune cells into damaged sites, characteristic of chronic damage and repair cycling (Spencer and Tidball 2001).
The major constituents of the inflammatory cell infiltration of muscle with dystrophin deficiency include macrophages, T-cells, and eosinophils (Spencer et al. 2001). Macrophages, CD4+ cells (helper lymphocytes) and CD8+ cells (cytotoxic lymphocytes) commonly infiltrate perimysial and endomysial sites of muscles. Macrophages and T-cells are believed to play significant roles in muscle degeneration, necrosis, apoptosis, and fibrosis in mdx mice (Morrison et al. 2000; Spencer et al. 1997). The depletion of macrophages, CD4+ and CD8+ cells, or impairment of their cytotoxicity by removal of perforin, ameliorated muscle histopathology and increased repair and regeneration in 3–4 week old mdx mice (Wehling et al. 2001; Spencer et al. 1997; Spencer et al. 2001). Moreover, antibody depletion of T-cells in mdx mice also reduced other inflammatory cells such as eosinophils, which have the capacity to promote cell membrane lysis and cell death by surrounding the degenerative muscle fibers (Wehling-Henricks et al. 2008; Cai et al. 2000). Morrison and colleagues (Morrison et al. 2000) suggested that T-cells also play a role in the onset of the fibrosis, which compromises the ability of dystrophic muscle to regenerate.
Inflammation is an early event in the pathological process with dystrophin deficiency. Inflammation and muscle cell death are first apparent at 3–4 weeks of age in mdx mice, with regenerative muscle replacing pathology by 14 weeks of age (Spencer and Tidball 2001). In human DMD, inflammation is mild but histologically discernable at birth, but it is not easy to diagnose the symptoms during first few years of life (Partridge 1991; Spencer and Tidball 2001). The mechanisms by which inflammatory cells promote the dystrophic pathology remain unknown. However, activation of nuclear factor-kappaB (NF-κB), oxidative stress, and pro-inflammatory cytokines (e.g., TNF-α, IL-1ß, TGF-ß) appear to be inflammatory-mediated processes integrated into the progression of muscular dystrophy (Peterson and Guttridge 2008; Kumar et al. 2004).
Evidence indicates that activation of NF-κB is an important mediator of muscle damage and pathology with dystrophin deficiency in both humans (Monici et al. 2003) and mdx mice (Kumar and Boriek 2003; Monici et al. 2003; Acharyya et al. 2007). Monici et al. (Monici et al. 2003) reported that NF-κB immunoreactivity was 20–40 % greater in necrotic fibers and the cytoplasm of regenerating fibers in DMD patients. Kumar and colleagues (Kumar and Boriek 2003) demonstrated that NF-κB DNA binding activity, and downstream inflammatory cytokines such as TNF-α and IL-1β, were significantly higher in diaphragms of 15-day-old mdx mice compared with wild-types. This was linked to lower protein levels of inhibitory IkBα in the mdx diaphragm. Acharyya et al. (Acharyya et al. 2007) reported that NF-κB DNA binding activity was elevated in mdx diaphragm, tibialis anterior (TA), and gastrocnemius muscles. Localization of NF-κB is greater in the nuclear fraction in mdx skeletal muscle than wild-type muscle (Whitehead et al. 2008). Further, immunohistochemical analysis of muscles expressing a dystrophin mutation indicated that NF-κB p65 subunit was localized in infiltrating immune cells (Peterson and Guttridge 2008). NF-κB activation as well as p65 and p50 subunits are elevated in immune cells and muscle fibers of mdx mice (Acharyya et al. 2007; Kumar and Boriek 2003). Indeed, NF-κB subunit activation is linked to dystrophin-deficient pathology (Acharyya et al. 2007; Kumar and Boriek 2003).
More mechanistic studies inhibiting NF-κB activation support the direct involvement of this transcription factor in pathology of dystrophin-deficient muscles, and thus as a target of therapeutic development. Indeed, genetic manipulation (Acharyya et al. 2007) or pharmacological blockade (Carlson et al. 2005; Pan et al. 2008; Messina et al. 2006b) of NF-κB alleviates the severity of the pathological phenotype limb muscles of mdx mice. Genetic ablation of the NF-κB subunit p65 or IKKβ reduced pathologic phenotype including inflammation, and promoted muscle regeneration. Stabilization of IkB-β by pyrrolidine dithiocarbamate (PDTC) improved muscle fiber survival in passively stretched dystrophic skeletal muscle, reduced necrosis, and enhanced muscle regeneration in mdx mice (Carlson et al. 2005).
Glucocorticoid therapy mitigates elevation of NF-κB and oxidative stress, concomitant with reduced damage and enhanced functional properties (Lim et al. 2004; Messina et al. 2009). The administration of curcumin, derived from the spice turmeric, attenuated NF-κB activation and dystrophic pathology in one study (Pan et al. 2008), but not a second investigation (Durham et al. 2006). More specific approaches have yielded more consistent results. For example, IRFI-042, an inhibitor of lipid peroxidation, reduced NF-κB activation and necrosis (Messina et al. 2006a), suggesting that oxidative stress may be upstream of pro-inflammatory signaling in mdx mice. In addition, treatment with NBD (NEMO-binding domain) peptide, a specific, non-toxic inhibitor of IKK (IkappaB kinase) reduced macrophage accumulation, necrosis, and improved contractile function in dystrophin-deficient muscle (Acharyya et al. 2007). Thus NBD has significant translational potential in treating DMD.
Dystrophin deficiency and oxidative stress
Muscle damage and weakness with dystrophin deficiency are proposed to be a consequence of damage repair cycling mediated via material fatigue injury and inflammation (Childers et al. 2002; Rando 2002; Spencer and Tidball 2001; Warren et al. 1993). Anti-inflammatory corticosteroid drugs reduce oxidative stress, damage, apoptosis, and disease progression with dystrophin deficiency in mdx mice, but have numerous side effects that limit their long-term use (Lim et al. 2004). While the link between material fatigue injury and inflammation with muscle damage and weakness in dystrophin deficiency is unresolved, elevated “oxidative stress” has been proposed as a contributing mechanism (Tidball and Wehling-Henricks 2004; Disatnik et al. 1998; Haycock et al. 1996; Ragusa et al. 1997; Rando 2001b, 2002; Rando et al. 1998; Tidball and Wehling-Henricks 2007; Williams and Allen 2007; Whitehead et al. 2010). Indeed, inflammatory signaling, including NF-κB and cytokine (TNF-α, IL-1β) pathways, may be responsive to oxidative stress (Tidball and Wehling-Henricks 2007; Grounds and Torrisi 2004). In addition, oxidative stress and upregulation of NF-κB are believed to be part of the cause in a variety of myopathies including disuse, cachexia, chronic heart failure, chronic obstructive pulmonary disease, AIDS, and cancer (Adams et al. 1999; Arbogast et al. 2007; Lawler et al. 2003; Dalla Libera et al. 2001; Buck and Chojkier 1996; Powers et al. 2007).
Oxidative stress is the result of (a) increased reactive oxygen species (ROS) and reactive nitrogen species (RNS) and (b) decreased, insufficient, or imbalanced antioxidant enzymes and stress proteins (e.g., heat shock proteins, IGF-1). A deficit of antioxidant defense and elevated ROS/RNS production can lead to cellular dysfunction, damage and tissue degeneration (Rando 2002). The possibility that oxidative stress contributes to muscle pathology in DMD was first proposed by Binder et al. (Binder et al. 1965), who noted the similarities to muscle pathology that occurred in α-tocopherol (e.g., vitamin E) deficiency, which directly increases free radicals and oxidative damage. Subsequently, Mendell et al. (Mendell et al. 1971) suggested that ischemia–reperfusion muscle injury produces oxidative lesions and damage with pathological characteristics, which were argued similar to those found in patients with dystrophinopathies.
Elevation of oxidative stress markers is a consistent finding with dystrophin deficiency in DMD humans (Haycock et al. 1996; Rodriguez and Tarnopolsky 2003) and mdx mice (Kaczor et al. 2007; Hauser et al. 1995; Ragusa et al. 1997). Byproducts of lipid peroxidation (e.g., TBARS, expired pentane), oxidation of proteins and oxidized DNA are increased in human DMD patients or mdx mice. In DMD humans, the protein carbonyl level in the quadriceps muscle was significantly higher (211 %) than in control subjects (Haycock et al. 1996). Rodriguez et al. (Rodriguez and Tarnopolsky 2003) have reported a marked increase in 8-hydroxy-2’-deoxyguqnosine, a marker of oxidative damage to DNA, in DMD patients compared with the healthy control. In mdx mice, Ragusa et al. (Ragusa et al. 1997) demonstrated that the content of TBARS, lipid peroxidation products, was consitantly higher in skeletal muscle than in control mice. The mdx mice also elevated the values for oxidoreductase of NADH O2 and cytochrome C in quadriceps and gastrocnemius compared with controls (Hauser et al. 1995). The dystrophin deficiency in mdx mice is involved with increased oxidative degradation in cell molecules. Nakae et al. (Nakae et al. 2004) suggested that lipofuscin, the so-called ageing pigment, was increased by the oxidative degradation of cellular macromolecules by oxygen-derived free radicals and redox-active metal ions. Disatnik et al. (Disatnik et al. 2000) also reported that the susceptibility of the cell populations to oxidative stress is increased with severity of the phenotype in the respective mdx, and mdx-transgenic strain which expresses full-length or truncated forms of dystrophin.
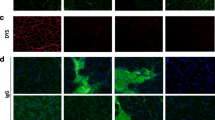
Potential sources of ROS in respiratory and limb muscles with dystrophin deficiency include the inflammatory cells (e.g., myeloperoxidase), NAD(P)H oxidase (NOX), xanthine–xanthine oxidase, mitochondria, and decoupling of NOS (Adams et al. 1999; Whitehead et al. 2008; Williams and Allen 2007; Spurney et al. 2008; Baker and Austin 1989). NAD(P)H oxidase is gathering particular interest as a major source of oxidative stress and contributor to dystrophin deficiency-induced muscle pathology (Whitehead et al. 2006; Whitehead et al. 2008; Whitehead et al. 2010). The NOX2 isoform of NAD(P)H oxidase includes membrane-bound gp91phox, p22phox subunits, and the cytosolic p47phox and p67phox subunits (Nguyen and Tidball 2003). It has been suggested that NOX2 may hyper-respond to stretch in dystrophin deficient muscles, possibly upstream of upregulation of caveolin-3 stretch activated Ca2+ channels (SACs), including TRPC1 (Gervasio et al. 2008; Whitehead et al. 2008). TRPC1 directly binds to caveolin-3 and both are upregulated in dystrophin-deficient muscles, and the activation and localization of TRPC1 are caveolin-3-dependent (Gervasio et al. 2008). Hydrogen peroxide increased TRPC1 protein levels in myoblasts, suggesting that increased TRPC1 via caveolin-3 may be redox dependent (Gervasio et al. 2008).
Metalloproteinase-9 (MMP-9), a member of the family of zinc-containing enzymes involved in degradation of extracellular matrix (ECM) proteins, has also been suggested to contribute to muscle pathogenesis in mdx mice (Lawler et al. 2011; Li et al. 2009). The genetic deletion of MMP-9 significantly inhibited the NF-κB activation in dystrophic muscle of mdx mice (Li et al. 2009), indicating that MMP-9 may be upstream of NF-κB activation. In addition, upregulation of caveolin-3 and MMP-9 is associated with nNOS dislocation from the DGC (Gervasio et al. 2008; Lawler et al. 2011). Downregulation and dislocation of nNOS from the DGC may also elevate oxidative stress, and disrupt DGC proteins, resulting in muscle wasting (Nguyen and Tidball 2003; Wehling et al. 2001; Shiao et al. 2004; Tidball and Wehling-Henricks 2004). Thus model is proposed that oxidative stress amplifies pathology of dystrophin deficient muscles via NAD(P)H oxidase, which triggers a cascade including caveolin-3, TRPC-1, MMP-9, and NF-κB (Fig. 1). This redox signaling pathway may contribute to nNOS dislocation and DGC disruption with dystrophin deficiency.
Redox signaling model for murine dystrophin deficiency-induced myopathy In the model, NAD(P)H oxidase, NOX2, contribute to increased caveolin-3 and MMP-9 protein contents. Subsequent signaling cascades involving transient receptor potential channel 1(TRPC1) and NF-κB activation result in nNOS dislocation and DGC disruption which are associated with dystrophin deficiency-induced myopathy
Muscles deficient of dystrophin from the sarcolemmal region are also more susceptible to oxidative damage than healthy muscle (Disatnik et al. 1998; Rando et al. 1998; Disatnik et al. 2000). For example, Rando et al. (Rando et al. 1998) showed that dystrophin-deficient myotubes are more susceptible to oxidative stress-induced damage compared with normal cells. Rando (Rando 2001b) proposed a “two-hit” hypothesis where the combination of oxidative stress with disturbances in the DGC leads to pathology with DMD. While oxidative stress is elevated and integrated with inflammatory cell invasion (macrophages, T-cells), cause and effect have remained uncertain with dystrophin deficiency (Tidball and Wehling-Henricks 2007). However, only more recently has the tie between oxidative stress and pathology in muscles with dystrophin deficiency moved beyond association (Spurney et al. 2008; Tidball and Wehling-Henricks 2007; Whitehead et al. 2008; Williams and Allen 2007).
Dystrophin deficiency and therapeutics: trials and tribulations
Muscle necrosis, inflammation, and fibrosis are prominent pathological features of dystrophin deficiency in mice (Zhou and Lu 2010; Porter et al. 2002) and humans (De Pasquale et al. 2012; Messina et al. 2011; Abdel-Salam et al. 2009). These pathological changes are a result of muscle damage-repair cycling and contribute to weakness in dystrophin-deficient muscles. Therefore, an important therapeutic goal in improving muscle function and dystrophic phenotype is to ameliorate these pathological changes. While a plethora of therapeutic strategies have been employed with the purpose of ameliorating dystrophin deficiency, including DMD, there remains no successful single treatment for the disease.
Gene therapy or cell therapy to restore the dystrophin missing from the DGC are promising, but one clinical trial has not yet produced convincing benefit in DMD patients (Mendell et al. 2010). In parallel, there is increasing interest in administration of non-invasive mechanical ventilation (NIV) for its longer survival effect for DMD patients (Bach and Martinez 2011; Ishikawa et al. 2011). However, the success of NIV is variable (i.e., depending on the selection of an appropriate patient, interface and ventilator settings, skills of the clinician, and motivation of the patient) and the use of NIV is limited (Hess 2012).
Interventions using corticosteroids, such as prednisone and deflazacort, confer partial benefits by reducing oxidative damage and inflammation. However, glucocorticoids produce significant side effects including impeding growth and maturation, enhancing edema and weight gain, osteopenia, immunosuppression, and susceptibility to infection (Carter and McDonald 2000; Skrabek and Anderson 2001). The NF-κB inhibitors curcumin (Pan et al. 2008) and PDTC (Messina et al. 2006b) attenuate muscle degeneration and enhance muscle regeneration and function in mdx mice, suggesting of the potential of NF-κB blockade on reducing dystrophin deficiency-induced muscle pathology. Imatinib, an anti-fibrotic agent and c-Abl inhibitor, also ameliorates muscle necrosis, inflammation and fibrosis while improving muscle function in mdx mice (Huang et al. 2009). Downregulation of platelet-derived growth factor (PDGF) and c-Abl signaling were proposed as contributory to the improvement of muscle function (Huang et al. 2009).
Prevention of pathology by a host of different antioxidants in dystrophin-deficient muscles have met with inconsistent success (Table 1). For example, green tea extracts including epigallocatechin-3-gallate (Buetler et al. 2002; Nakae et al. 2008; Dorchies et al. 2006), low-iron diet (Bornman et al. 1998), and N-acetylcysteine (Whitehead et al. 2008) all protected against muscle damage. Recently, a 6 week treatment of N-acetylcysteine was found to protect against damage, incidence of internal nuclei, macrophage invasion, and weakness in the EDL muscle of 8 week old mdx mice (Whitehead et al. 2008). N-acetylcysteine also increased protein levels of the ß-dystroglycan and utrophin, while decreasing caveolin-3 and NF-κB activation. In contrast, patient trials using nicotinamide (Vitamin B), tocopherols (Vitamin E), and penicillamine elicited no protection against pathology and muscle dysfunction (Roelofs et al. 1979; Fenichel et al. 1988; Stern et al. 1982; Walton and Nattrass 1954). For examples, Fenichel et al. (Fenichel et al. 1988) demonstrated that penicillamine and vitamin E treatment for 18 months in DMD patients did not change serum creatine kinase level, muscle strength, and cardio-pulmonary function. Walton et al. (Walton and Nattrass 1954) also reported no beneficial or a deteriorative effect of vitamin B3 and vitamin E on muscle function and motor behavior of DMD patients. Specificity of ROS, source of oxidants, timing, and cellular regulation of nutritional supplements must all be considered when determining the role of oxidative stress as an amplifier against damage and weakness in dystrophin-deficient muscles. Indeed, effective antioxidant treatments should arguably be targeted and, initiated early in the course of the disease (Rando 2002).
Part of the inconsistency observed in non-specific antioxidant scavenger interventions in ameliorating dystrophinopathies including DMD may lie within the nature of redox microenvironments of the sarcolemma (Ushio-Fukai 2009; Fisher 2009). Increasing evidence emphasizes the importance of hydrogen peroxide and superoxide anions (O •−2 ) in muscle wasting models (Arbogast et al. 2007; Whitehead et al. 2008; Lawler et al. 2003; Kim and Lawler 2012; Selsby 2011). In dystrophin-deficient muscle xanthine–xanthine oxidase system, NAD(P)H oxidase, and mitochondria may contribute to the generation of O •−2 , which, in turn, is dismutated to hydrogen peroxide by superoxide dismutase (Baker and Austin 1989; Whitehead et al. 2008). NAD(P)H oxidase is a source of oxidative stress that is localized in cell membranes and inflammatory cells (Nguyen and Tidball 2003). While NAD(P)H oxidase releases O •−2 into the interstitial space, O •−2 enters the cell easily via chloride channel-3 (ClC3), while hydrogen peroxide diffuses across cell membranes and is facilitated by aquaporin channels (Fisher 2009).
NAD(P)H oxidase may also be an important contributor of muscle pathology and muscle wasting seen in mechanical ventilation (McClung et al. 2007) and aging (Vasilaki et al. 2006). Furthermore, knockout of the gp91phox, a regulatory subunit of NOX2 reduces membrane and fiber damage during reloading following hindlimb unloading (Nguyen and Tidball 2003). Indeed, NAD(P)H oxidase is elevated in the sarcolemma with both dystrophin deficiency and disuse (Williams and Allen 2007). Evidence indicates that inhibition of NAD(P)H oxidase via apocynin increased anti-apoptotic proteins such as Bcl-2 (B cell lymphoma-2) and BAG-4 (Bcl-2-associated athanogene-4) in the diaphragm of mdx mice (Kim et al. 2008). Moreover, apocynin ameliorates sarcolemmal localization of p47phox subunit and MMP-9 (Lawler et al. 2011). Therefore, NOX2 isoform of NAD(P)H oxidase may be an important regulator affecting dystrophin deficiency-induced muscle pathology, such as activating TRPC1. Whitehead et al. (Whitehead et al. 2006) demonstrated that inhibition of TRPC1 by streptomycin and spider venom GsMTx4 reduced muscle damage and prevented weakness in the EDL muscle following stretch in mdx mice. However, further studies are required.
Li et al. (Li et al. 2009) demonstrated that pharmacological inhibition and genetic deletion of MMP-9 in mdx mice significantly reduced muscle damage, inflammation, and necrosis. Furthermore, genetic ablation of MMP-9 also increased the DGC proteins β-dystroglycan and nNOS (Li et al. 2009). Suppression of MMP-9 also reduced caveolin-3 protein levels (Li et al. 2009), indicating that MMP-9 may be an important regulator of caveolin-3 in dystrophic muscles.
The diaphragm muscle may be at particular risk with dystrophin deficiency because oxidant production is higher in the mdx diaphragm than limb muscles, which could contribute to more profound fibrosis, weakness, and fatigability in that muscle (Hartel et al. 2001; Stevens and Faulkner 2000). In addition, the diaphragm muscle in the mdx mouse model experiences muscle damage and disease progression that resemble more closely human DMD pathology than observed for limb muscles, which tend to recover or adapt after an initial necrotic phase (Tidball and Wehling-Henricks 2007; Tkatchenko et al. 2000). Therefore, the study of the mechanisms by which oxidative stress causes pathology in diaphragm with dystrophin-deficiency, and development of targeted, antioxidant therapeutics are vital in translation to human disease and myopathy.
In conclusion, increasing evidence is showing that oxidative stress could play a vital role in pathology in diaphragm and limb muscles with dystrophin deficiency. While initial antioxidant interventions yielded equivocal results in reducing pathology, more recent evidence suggest that oxidative stress may be initiated via NAD(P)H oxidase, which elicits a downstream cascade involving MMP-9, NF-κB, caveolin-3, and TRPC-1 that further disrupts the DGC, including nNOSμ. While the mechanisms that stimulate NAD(P)H oxidase and by which TRPC1 and Ca2+ homeostasis further compromises integrity of the DGC are unknown in dystrophinopathies, the potential for the development of new, targeted interventions is now possible against respiratory and limb muscle failure.
References
Abdel-Salam E, Abdel-Meguid I, Korraa SS (2009) Markers of degeneration and regeneration in Duchenne muscular dystrophy. Acta Myol 28(3):94–100
Acharyya S, Villalta SA, Bakkar N, Bupha-Intr T, Janssen PM, Carathers M, Li ZW, Beg AA, Ghosh S, Sahenk Z, Weinstein M, Gardner KL, Rafael-Fortney JA, Karin M, Tidball JG, Baldwin AS, Guttridge DC (2007) Interplay of IKK/NF-kappaB signaling in macrophages and myofibers promotes muscle degeneration in Duchenne muscular dystrophy. J Clin Invest 117(4):889–901
Adams V, Jiang H, Yu J, Mobius-Winkler S, Fiehn E, Linke A, Weigl C, Schuler G, Hambrecht R (1999) Apoptosis in skeletal myocytes of patients with chronic heart failure is associated with exercise intolerance. J Am Coll Cardiol 33(4):959–965
Adams ME, Kramarcy N, Krall SP, Rossi SG, Rotundo RL, Sealock R, Froehner SC (2000) Absence of alpha-syntrophin leads to structurally aberrant neuromuscular synapses deficient in utrophin. J Cell Biol 150(6):1385–1398
Allen DG, Gervasio OL, Yeung EW, Whitehead NP (2010) Calcium and the damage pathways in muscular dystrophy. Can J Physiol Pharmacol 88(2):83–91
Arbogast S, Smith J, Matuszczak Y, Hardin BJ, Moylan JS, Smith JD, Ware J, Kennedy AR, Reid MB (2007) Bowman-Birk inhibitor concentrate prevents atrophy, weakness, and oxidative stress in soleus muscle of hindlimb-unloaded mice. J Appl Physiol 102(3):956–964
Bach JR, Martinez D (2011) Duchenne muscular dystrophy: continuous noninvasive ventilatory support prolongs survival. Respir Care 56(6):744–750
Badalamente MA, Stracher A (2000) Delay of muscle degeneration and necrosis in mdx mice by calpain inhibition. Muscle Nerve 23(1):106–111
Baker MS, Austin L (1989) The pathological damage in Duchenne muscular dystrophy may be due to increased intracellular oxy-radical generation caused by the absence of dystrophin and subsequent alterations in Ca2 + metabolism. Med Hypotheses 29(3):187–193
Berneske GM, Butson AR, Gauld EN, Levy D (1960) Clinical trial of high dosage vitamin E in human muscular dystrophy. Can Med Assoc J 82:418–421
Binder HJ, Herting DC, Hurst V, Finch SC, Spiro HM (1965) Tocopherol deficiency in man. N Engl J Med 273(24):1289–1297
Bornman L, Rossouw H, Gericke GS, Polla BS (1998) Effects of iron deprivation on the pathology and stress protein expression in murine X-linked muscular dystrophy. Biochem Pharmacol 56(6):751–757
Brenman JE, Chao DS, Xia H, Aldape K, Bredt DS (1995) Nitric oxide synthase complexed with dystrophin and absent from skeletal muscle sarcolemma in Duchenne muscular dystrophy. Cell 82(5):743–752
Brenman JE, Chao DS, Gee SH, McGee AW, Craven SE, Santillano DR, Wu Z, Huang F, Xia H, Peters MF, Froehner SC, Bredt DS (1996) Interaction of nitric oxide synthase with the postsynaptic density protein PSD-95 and alpha1-syntrophin mediated by PDZ domains. Cell 84(5):757–767
Buck M, Chojkier M (1996) Muscle wasting and dedifferentiation induced by oxidative stress in a murine model of cachexia is prevented by inhibitors of nitric oxide synthesis and antioxidants. EMBO J 15(8):1753–1765
Buetler TM, Renard M, Offord EA, Schneider H, Ruegg UT (2002) Green tea extract decreases muscle necrosis in mdx mice and protects against reactive oxygen species. Am J Clin Nutr 75(4):749–753
Cai B, Spencer MJ, Nakamura G, Tseng-Ong L, Tidball JG (2000) Eosinophilia of dystrophin-deficient muscle is promoted by perforin-mediated cytotoxicity by T cell effectors. Am J Pathol 156(5):1789–1796
Carlson CG, Samadi A, Siegel A (2005) Chronic treatment with agents that stabilize cytosolic IkappaB-alpha enhances survival and improves resting membrane potential in MDX muscle fibers subjected to chronic passive stretch. Neurobiol Dis 20(3):719–730
Carter GT, McDonald CM (2000) Preserving function in Duchenne dystrophy with long-term pulse prednisone therapy. Am J Phys Med Rehabil 79(5):455–458
Chamberlain JS, Metzger J, Reyes M, Townsend D, Faulkner JA (2007) Dystrophin-deficient mdx mice display a reduced life span and are susceptible to spontaneous rhabdomyosarcoma. FASEB J 21(9):2195–2204
Chang WJ, Iannaccone ST, Lau KS, Masters BS, McCabe TJ, McMillan K, Padre RC, Spencer MJ, Tidball JG, Stull JT (1996) Neuronal nitric oxide synthase and dystrophin-deficient muscular dystrophy. Proc Natl Acad Sci U S A 93(17):9142–9147
Chao DS, Silvagno F, Bredt DS (1998) Muscular dystrophy in mdx mice despite lack of neuronal nitric oxide synthase. J Neurochem 71(2):784–789
Chen M, Cheng C, Yan M, Niu S, Gao S, Shi S, Liu H, Qin Y, Shen A (2008) Involvement of CAPON and nitric oxide synthases in rat muscle regeneration after peripheral nerve injury. J Mol Neurosci 34(1):89–100
Childers MK, Okamura CS, Bogan DJ, Bogan JR, Petroski GF, McDonald K, Kornegay JN (2002) Eccentric contraction injury in dystrophic canine muscle. Arch Phys Med Rehabil 83(11):1572–1578
Crosbie RH, Straub V, Yun HY, Lee JC, Rafael JA, Chamberlain JS, Dawson VL, Dawson TM, Campbell KP (1998) mdx muscle pathology is independent of nNOS perturbation. Hum Mol Genet 7(5):823–829
Dalla Libera L, Sabbadini R, Renken C, Ravara B, Sandri M, Betto R, Angelini A, Vescovo G (2001) Apoptosis in the skeletal muscle of rats with heart failure is associated with increased serum levels of TNF-alpha and sphingosine. J Mol Cell Cardiol 33(10):1871–1878
De Pasquale L, D’Amico A, Verardo M, Petrini S, Bertini E, De Benedetti F (2012) Increased muscle expression of interleukin-17 in Duchenne muscular dystrophy. Neurology 78(17):1309–1314
Disatnik MH, Rando TA (1999) Integrin-mediated muscle cell spreading. The role of protein kinase c in outside-in and inside-out signaling and evidence of integrin cross-talk. J Biol Chem 274(45):32486–32492
Disatnik MH, Dhawan J, Yu Y, Beal MF, Whirl MM, Franco AA, Rando TA (1998) Evidence of oxidative stress in mdx mouse muscle: studies of the pre-necrotic state. J Neurol Sci 161(1):77–84
Disatnik MH, Chamberlain JS, Rando TA (2000) Dystrophin mutations predict cellular susceptibility to oxidative stress. Muscle Nerve 23(5):784–792
Dorchies OM, Wagner S, Vuadens O, Waldhauser K, Buetler TM, Kucera P, Ruegg UT (2006) Green tea extract and its major polyphenol (-)-epigallocatechin gallate improve muscle function in a mouse model for Duchenne muscular dystrophy. Am J Physiol Cell Physiol 290(2):C616–C625
Dupont-Versteegden EE, McCarter RJ (1992) Differential expression of muscular dystrophy in diaphragm versus hindlimb muscles of mdx mice. Muscle Nerve 15(10):1105–1110
Durham WJ, Arbogast S, Gerken E, Li YP, Reid MB (2006) Progressive nuclear factor-kappaB activation resistant to inhibition by contraction and curcumin in mdx mice. Muscle Nerve 34(3):298–303
Escolar DM, Scacheri CG (2001) Pharmacologic and genetic therapy for childhood muscular dystrophies. Curr Neurol Neurosci Rep 1(2):168–174
Fecchi K, Volonte D, Hezel MP, Schmeck K, Galbiati F (2006) Spatial and temporal regulation of GLUT4 translocation by flotillin-1 and caveolin-3 in skeletal muscle cells. FASEB J 20(6):705–707
Fenichel GM, Brooke MH, Griggs RC, Mendell JR, Miller JP, Moxley RT 3rd, Park JH, Provine MA, Florence J, Kaiser KK et al (1988) Clinical investigation in Duchenne muscular dystrophy: penicillamine and vitamin E. Muscle Nerve 11(11):1164–1168
Fisher AB (2009) Redox signaling across cell membranes. Antioxid Redox Signal 11(6):1349–1356
Galbiati F, Razani B, Lisanti MP (2001) Caveolae and caveolin-3 in muscular dystrophy. Trends Mol Med 7(10):435–441
Gervasio OL, Whitehead NP, Yeung EW, Phillips WD, Allen DG (2008) TRPC1 binds to caveolin-3 and is regulated by Src kinase - role in Duchenne muscular dystrophy. J Cell Sci 121(Pt 13):2246–2255
Grady RM, Grange RW, Lau KS, Maimone MM, Nichol MC, Stull JT, Sanes JR (1999) Role for alpha-dystrobrevin in the pathogenesis of dystrophin-dependent muscular dystrophies. Nat Cell Biol 1(4):215–220
Grounds MD, Torrisi J (2004) Anti-TNFalpha (Remicade) therapy protects dystrophic skeletal muscle from necrosis. FASEB J 18(6):676–682
Hartel JV, Granchelli JA, Hudecki MS, Pollina CM, Gosselin LE (2001) Impact of prednisone on TGF-beta1 and collagen in diaphragm muscle from mdx mice. Muscle Nerve 24(3):428–432
Hauser E, Hoger H, Bittner R, Widhalm K, Herkner K, Lubec G (1995) Oxyradical damage and mitochondrial enzyme activities in the mdx mouse. Neuropediatrics 26(5):260–262
Haycock JW, MacNeil S, Jones P, Harris JB, Mantle D (1996) Oxidative damage to muscle protein in Duchenne muscular dystrophy. NeuroReport 8(1):357–361
Hess DR (2012) The growing role of noninvasive ventilation in patients requiring prolonged mechanical ventilation. Respir Care 57 (6):900–918; discussion 918–920
Hnia K, Gayraud J, Hugon G, Ramonatxo M, De La Porte S, Matecki S, Mornet D (2008) l-arginine decreases inflammation and modulates the nuclear factor-kappaB/matrix metalloproteinase cascade in mdx muscle fibers. Am J Pathol 172(6):1509–1519
Hodgetts S, Radley H, Davies M, Grounds MD (2006) Reduced necrosis of dystrophic muscle by depletion of host neutrophils, or blocking TNFalpha function with Etanercept in mdx mice. Neuromuscul Disord 16(9–10):591–602
Hoshino S, Ohkoshi N, Ishii A, Shoji S (2002) The expression of alpha-dystrobrevin and dystrophin during skeletal muscle regeneration. J Muscle Res Cell Motil 23(2):131–138
Huang P, Zhao XS, Fields M, Ransohoff RM, Zhou L (2009) Imatinib attenuates skeletal muscle dystrophy in mdx mice. FASEB J 23(8):2539–2548
Ishikawa Y, Miura T, Aoyagi T, Ogata H, Hamada S, Minami R (2011) Duchenne muscular dystrophy: survival by cardio-respiratory interventions. Neuromuscul Disord 21(1):47–51
Jones KJ, Compton AG, Yang N, Mills MA, Peters MF, Mowat D, Kunkel LM, Froehner SC, North KN (2003) Deficiency of the syntrophins and alpha-dystrobrevin in patients with inherited myopathy. Neuromuscul Disord 13(6):456–467
Kaczor JJ, Hall JE, Payne E, Tarnopolsky MA (2007) Low intensity training decreases markers of oxidative stress in skeletal muscle of mdx mice. Free Radic Biol Med 43(1):145–154
Kameya S, Miyagoe Y, Nonaka I, Ikemoto T, Endo M, Hanaoka K, Nabeshima Y, Takeda S (1999) Alpha1-syntrophin gene disruption results in the absence of neuronal-type nitric-oxide synthase at the sarcolemma but does not induce muscle degeneration. J Biol Chem 274(4):2193–2200
Kaminski HJ, Andrade FH (2001) Nitric oxide: biologic effects on muscle and role in muscle diseases. Neuromuscul Disord 11(6–7):517–524
Kim J-H, Lawler JM (2012) Amplification of proinflammatory phenotype, damage, and weakness by oxidative stress in the diaphragm muscle of mdx mice. Free Radic Biol Med 52(9):1597–1606
Kim J-H, Kwak HB, Lawler JM (2008) NAD(P)H oxidase inhibition upregulates anti-apoptotic BAG-4 protein expression in the mdx diaphragm. FASEB J 22(959):8
Kosek DJ, Bamman MM (2008) Modulation of the dystrophin-associated protein complex in response to resistance training in young and older men. J Appl Physiol 104(5):1476–1484
Kumar A, Boriek AM (2003) Mechanical stress activates the nuclear factor-kappaB pathway in skeletal muscle fibers: a possible role in Duchenne muscular dystrophy. FASEB J 17(3):386–396
Kumar A, Takada Y, Boriek AM, Aggarwal BB (2004) Nuclear factor-kappaB: its role in health and disease. J Mol Med 82(7):434–448
Lai Y, Thomas GD, Yue Y, Yang HT, Li D, Long C, Judge L, Bostick B, Chamberlain JS, Terjung RL, Duan D (2009) Dystrophins carrying spectrin-like repeats 16 and 17 anchor nNOS to the sarcolemma and enhance exercise performance in a mouse model of muscular dystrophy. J Clin Invest 119(3):624–635
Lawler JM, Song W, Demaree SR (2003) Hindlimb unloading increases oxidative stress and disrupts antioxidant capacity in skeletal muscle. Free Radic Biol Med 35(1):9–16
Lawler JM, Hord JM, Yang Lee, Kumar Joshi, and Jong-Hee Kim (2011) Redox regulation of caveolin-3 and MMP-9 in the diaphragm of mdx mice. FASEB J LB:519
Li H, Mittal A, Makonchuk DY, Bhatnagar S, Kumar A (2009) Matrix metalloproteinase-9 inhibition ameliorates pathogenesis and improves skeletal muscle regeneration in muscular dystrophy. Hum Mol Genet 18(14):2584–2598
Lim JH, Kim DY, Bang MS (2004) Effects of exercise and steroid on skeletal muscle apoptosis in the mdx mouse. Muscle Nerve 30(4):456–462
Lynch GS (2004) Role of contraction-induced injury in the mechanisms of muscle damage in muscular dystrophy. Clin Exp Pharmacol Physiol 31(8):557–561
Lynch GS, Rafael JA, Hinkle RT, Cole NM, Chamberlain JS, Faulkner JA (1997) Contractile properties of diaphragm muscle segments from old mdx and old transgenic mdx mice. Am J Physiol 272(6 Pt 1):C2063–C2068
Lynch GS, Hinkle RT, Chamberlain JS, Brooks SV, Faulkner JA (2001) Force and power output of fast and slow skeletal muscles from mdx mice 6–28 months old. J Physiol 535(Pt 2):591–600
Matsumura K, Campbell KP (1994) Dystrophin-glycoprotein complex: its role in the molecular pathogenesis of muscular dystrophies. Muscle Nerve 17(1):2–15
McClung JM, Kavazis AN, DeRuisseau KC, Falk DJ, Deering MA, Lee Y, Sugiura T, Powers SK (2007) Caspase-3 regulation of diaphragm myonuclear domain during mechanical ventilation-induced atrophy. Am J Respir Crit Care Med 175(2):150–159
Mendell JR, Engel WK, Derrer EC (1971) Duchenne muscular dystrophy: functional ischemia reproduces its characteristic lesions. Science 172(988):1143–1145
Mendell JR, Campbell K, Rodino-Klapac L, Sahenk Z, Shilling C, Lewis S, Bowles D, Gray S, Li C, Galloway G, Malik V, Coley B, Clark KR, Li J, Xiao X, Samulski J, McPhee SW, Samulski RJ, Walker CM (2010) Dystrophin immunity in Duchenne’s muscular dystrophy. N Engl J Med 363(15):1429–1437
Messina S, Altavilla D, Aguennouz M, Seminara P, Minutoli L, Monici MC, Bitto A, Mazzeo A, Marini H, Squadrito F, Vita G (2006a) Lipid peroxidation inhibition blunts nuclear factor-kappaB activation, reduces skeletal muscle degeneration, and enhances muscle function in mdx mice. Am J Pathol 168(3):918–926
Messina S, Bitto A, Aguennouz M, Minutoli L, Monici MC, Altavilla D, Squadrito F, Vita G (2006b) Nuclear factor kappa-B blockade reduces skeletal muscle degeneration and enhances muscle function in Mdx mice. Exp Neurol 198(1):234–241
Messina S, Bitto A, Aguennouz M, Mazzeo A, Migliorato A, Polito F, Irrera N, Altavilla D, Vita GL, Russo M, Naro A, De Pasquale MG, Rizzuto E, Musaro A, Squadrito F, Vita G (2009) Flavocoxid counteracts muscle necrosis and improves functional properties in mdx mice: a comparison study with methylprednisolone. Exp Neurol 220(2):349–358
Messina S, Vita GL, Aguennouz M, Sframeli M, Romeo S, Rodolico C, Vita G (2011) Activation of NF-kappaB pathway in Duchenne muscular dystrophy: relation to age. Acta Myol 30(1):16–23
Miyagoe-Suzuki Y, Takeda SI (2001) Association of neuronal nitric oxide synthase (nNOS) with alpha1-syntrophin at the sarcolemma. Microsc Res Tech 55(3):164–170
Monici MC, Aguennouz M, Mazzeo A, Messina C, Vita G (2003) Activation of nuclear factor-kappaB in inflammatory myopathies and Duchenne muscular dystrophy. Neurology 60(6):993–997
Morrison J, Lu QL, Pastoret C, Partridge T, Bou-Gharios G (2000) T-cell-dependent fibrosis in the mdx dystrophic mouse. Lab Invest 80(6):881–891
Nakae Y, Stoward PJ, Kashiyama T, Shono M, Akagi A, Matsuzaki T, Nonaka I (2004) Early onset of lipofuscin accumulation in dystrophin-deficient skeletal muscles of DMD patients and mdx mice. J Mol Histol 35(5):489–499
Nakae Y, Hirasaka K, Goto J, Nikawa T, Shono M, Yoshida M, Stoward PJ (2008) Subcutaneous injection, from birth, of epigallocatechin-3-gallate, a component of green tea, limits the onset of muscular dystrophy in mdx mice: a quantitative histological, immunohistochemical and electrophysiological study. Histochem Cell Biol 129(4):489–501
Nguyen HX, Tidball JG (2003) Null mutation of gp91phox reduces muscle membrane lysis during muscle inflammation in mice. J Physiol 553(Pt 3):833–841
Pan Y, Chen C, Shen Y, Zhu CH, Wang G, Wang XC, Chen HQ, Zhu MS (2008) Curcumin alleviates dystrophic muscle pathology in mdx mice. Mol Cells 25(4):531–537
Partridge T (1991) Animal models of muscular dystrophy–what can they teach us? Neuropathol Appl Neurobiol 17(5):353–363
Pastoret C, Sebille A (1995) Age-related differences in regeneration of dystrophic (mdx) and normal muscle in the mouse. Muscle Nerve 18(10):1147–1154
Peters MF, Adams ME, Froehner SC (1997) Differential association of syntrophin pairs with the dystrophin complex. J Cell Biol 138(1):81–93
Peterson JM, Guttridge DC (2008) Skeletal muscle diseases, inflammation, and NF-kappaB signaling: insights and opportunities for therapeutic intervention. Int Rev Immunol 27(5):375–387
Porter JD, Khanna S, Kaminski HJ, Rao JS, Merriam AP, Richmonds CR, Leahy P, Li J, Guo W, Andrade FH (2002) A chronic inflammatory response dominates the skeletal muscle molecular signature in dystrophin-deficient mdx mice. Hum Mol Genet 11(3):263–272
Powers SK, Kavazis AN, McClung JM (2007) Oxidative stress and disuse muscle atrophy. J Appl Physiol 102(6):2389–2397
Ragusa RJ, Chow CK, Porter JD (1997) Oxidative stress as a potential pathogenic mechanism in an animal model of Duchenne muscular dystrophy. Neuromuscul Disord 7(6–7):379–386
Rando TA (2001a) The dystrophin-glycoprotein complex, cellular signaling, and the regulation of cell survival in the muscular dystrophies. Muscle Nerve 24(12):1575–1594
Rando TA (2001b) Role of nitric oxide in the pathogenesis of muscular dystrophies: a “two hit” hypothesis of the cause of muscle necrosis. Microsc Res Tech 55(4):223–235
Rando TA (2002) Oxidative stress and the pathogenesis of muscular dystrophies. Am J Phys Med Rehabil 81(11 Suppl):S175–S186
Rando TA, Disatnik MH, Yu Y, Franco A (1998) Muscle cells from mdx mice have an increased susceptibility to oxidative stress. Neuromuscul Disord 8(1):14–21
Rodriguez MC, Tarnopolsky MA (2003) Patients with dystrophinopathy show evidence of increased oxidative stress. Free Radic Biol Med 34(9):1217–1220
Roelofs RI, de Arango GS, Law PK, Kinsman D, Buchanan DC, Park JH (1979) Treatment of Duchenne’s muscular dystrophy with penicillamine. Results of a double-blind trial. Arch Neurol 36(5):266–268
Sandri M, Carraro U (1999) Apoptosis of skeletal muscles during development and disease. Int J Biochem Cell Biol 31(12):1373–1390
Selsby JT (2011) Increased catalase expression improves muscle function in mdx mice. Exp Physiol 96(2):194–202
Shiao T, Fond A, Deng B, Wehling-Henricks M, Adams ME, Froehner SC, Tidball JG (2004) Defects in neuromuscular junction structure in dystrophic muscle are corrected by expression of a NOS transgene in dystrophin-deficient muscles, but not in muscles lacking alpha- and beta1-syntrophins. Hum Mol Genet 13(17):1873–1884
Skrabek RQ, Anderson JE (2001) Metabolic shifts and myocyte hypertrophy in deflazacort treatment of mdx mouse cardiomyopathy. Muscle Nerve 24(2):192–202
Spencer MJ, Tidball JG (2001) Do immune cells promote the pathology of dystrophin-deficient myopathies? Neuromuscul Disord 11(6–7):556–564
Spencer MJ, Walsh CM, Dorshkind KA, Rodriguez EM, Tidball JG (1997) Myonuclear apoptosis in dystrophic mdx muscle occurs by perforin-mediated cytotoxicity. J Clin Invest 99(11):2745–2751
Spencer MJ, Marino MW, Winckler WM (2000) Altered pathological progression of diaphragm and quadriceps muscle in TNF-deficient, dystrophin-deficient mice. Neuromuscul Disord 10(8):612–619
Spencer MJ, Montecino-Rodriguez E, Dorshkind K, Tidball JG (2001) Helper (CD4(+)) and cytotoxic (CD8(+)) T cells promote the pathology of dystrophin-deficient muscle. Clin Immunol 98(2):235–243
Spurney CF, Knoblach S, Pistilli EE, Nagaraju K, Martin GR, Hoffman EP (2008) Dystrophin-deficient cardiomyopathy in mouse: expression of Nox4 and Lox are associated with fibrosis and altered functional parameters in the heart. Neuromuscul Disord 18(5):371–381
Stedman HH, Sweeney HL, Shrager JB, Maguire HC, Panettieri RA, Petrof B, Narusawa M, Leferovich JM, Sladky JT, Kelly AM (1991) The mdx mouse diaphragm reproduces the degenerative changes of Duchenne muscular dystrophy. Nature 352(6335):536–539
Stern LZ, Ringel SP, Ziter FA, Menander-Huber KB, Ionasescu V, Pellegrino RJ, Snyder RD (1982) Drug trial of superoxide dismutase in Duchenne’s muscular dystrophy. Arch Neurol 39(6):342–346
Stevens ED, Faulkner JA (2000) The capacity of mdx mouse diaphragm muscle to do oscillatory work. J Physiol 522(Pt 3):457–466
Sunada Y, Ohi H, Hase A, Hosono T, Arata S, Higuchi S, Matsumura K, Shimizu T (2001) Transgenic mice expressing mutant caveolin-3 show severe myopathy associated with increased nNOS activity. Hum Mol Genet 10(3):173–178
Sussman M (2002) Duchenne muscular dystrophy. J Am Acad Orthop Surg 10(2):138–151
Tidball JG, Wehling-Henricks M (2004) Expression of a NOS transgene in dystrophin-deficient muscle reduces muscle membrane damage without increasing the expression of membrane-associated cytoskeletal proteins. Mol Genet Metab 82(4):312–320
Tidball JG, Wehling-Henricks M (2007) The role of free radicals in the pathophysiology of muscular dystrophy. J Appl Physiol 102(4):1677–1686
Tkatchenko AV, Le Cam G, Léger JJ, Dechesne CA (2000) Large-scale analysis of differential gene expression in the hindlimb muscles and diaphragm of mdx mouse. Biochim Biophys Acta 1500 (1):17–30
Ushio-Fukai M (2009) Compartmentalization of redox signaling through NADPH oxidase-derived ROS. Antioxid Redox Signal 11(6):1289–1299
Vasilaki A, Mansouri A, Remmen H, van der Meulen JH, Larkin L, Richardson AG, McArdle A, Faulkner JA, Jackson MJ (2006) Free radical generation by skeletal muscle of adult and old mice: effect of contractile activity. Aging Cell 5(2):109–117
Venema VJ, Ju H, Zou R, Venema RC (1997) Interaction of neuronal nitric-oxide synthase with caveolin-3 in skeletal muscle. Identification of a novel caveolin scaffolding/inhibitory domain. J Biol Chem 272(45):28187–28190
Wakayama Y, Inoue M, Murahashi M, Shibuya S, Jimi T, Kojima H, Oniki H (1997) Ultrastructural localization of alpha 1-syntrophin and neuronal nitric oxide synthase in normal skeletal myofiber, and their relation to each other and to dystrophin. Acta Neuropathol 94(5):455–464
Walton JN, Nattrass FJ (1954) On the classification, natural history and treatment of the myopathies. Brain 77(2):169–231
Warren GL, Hayes DA, Lowe DA, Prior BM, Armstrong RB (1993) Materials fatigue initiates eccentric contraction-induced injury in rat soleus muscle. J Physiol 464:477–489
Wehling M, Spencer MJ, Tidball JG (2001) A nitric oxide synthase transgene ameliorates muscular dystrophy in mdx mice. J Cell Biol 155(1):123–131
Wehling-Henricks M, Sokolow S, Lee JJ, Myung KH, Villalta SA, Tidball JG (2008) Major basic protein-1 promotes fibrosis of dystrophic muscle and attenuates the cellular immune response in muscular dystrophy. Hum Mol Genet 17(15):2280–2292
Whitehead NP, Streamer M, Lusambili LI, Sachs F, Allen DG (2006) Streptomycin reduces stretch-induced membrane permeability in muscles from mdx mice. Neuromuscul Disord 16(12):845–854
Whitehead NP, Pham C, Gervasio OL, Allen DG (2008) N-Acetylcysteine ameliorates skeletal muscle pathophysiology in mdx mice. J Physiol 586(7):2003–2014
Whitehead NP, Yeung EW, Froehner SC, Allen DG (2010) Skeletal muscle NADPH oxidase is increased and triggers stretch-induced damage in the mdx mouse. PLoS ONE 5(12):e15354
Williams IA, Allen DG (2007) The role of reactive oxygen species in the hearts of dystrophin-deficient mdx mice. Am J Physiol Heart Circ Physiol 293(3):H1969–H1977
Williamson RA, Henry MD, Daniels KJ, Hrstka RF, Lee JC, Sunada Y, Ibraghimov-Beskrovnaya O, Campbell KP (1997) Dystroglycan is essential for early embryonic development: disruption of Reichert’s membrane in Dag1-null mice. Hum Mol Genet 6(6):831–841
Yiu EM, Kornberg AJ (2008) Duchenne muscular dystrophy. Neurol India 56(3):236–247
Yoshida M, Hama H, Ishikawa-Sakurai M, Imamura M, Mizuno Y, Araishi K, Wakabayashi-Takai E, Noguchi S, Sasaoka T, Ozawa E (2000) Biochemical evidence for association of dystrobrevin with the sarcoglycan-sarcospan complex as a basis for understanding sarcoglycanopathy. Hum Mol Genet 9(7):1033–1040
Zhou L, Lu H (2010) Targeting fibrosis in Duchenne muscular dystrophy. J Neuropathol Exp Neurol 69(8):771–776
Acknowledgments
This work is supported by the Sydney and JL Huffines research grant (JHK, JML) and NIH (AG017768, AR054084) (LVT, JML).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, JH., Kwak, HB., Thompson, L.V. et al. Contribution of oxidative stress to pathology in diaphragm and limb muscles with Duchenne muscular dystrophy. J Muscle Res Cell Motil 34, 1–13 (2013). https://doi.org/10.1007/s10974-012-9330-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10974-012-9330-9