Abstract
Purpose
To study return to work (RTW) at 2-year follow-up in a randomised controlled trial comparing brief intervention (BI) and multidisciplinary intervention (MDI) in employees on sick leave due to low back pain (LBP) stratified for job relations.
Methods
In total 476 employees on sick leave for 4–12 weeks due to LBP were divided into strata with weak or strong job relations, based on perceived risk of losing job and influence on job planning. In each stratum participants were allocated to BI or MDI. All participants received BI, i.e. a clinical examination by a rheumatologist and physiotherapist. In addition, MDI involved a case manager who made a rehabilitation plan in collaboration with the participant. The primary outcome was time to RTW. Secondary outcomes were median weeks in different employment status and selfreported pain, disability and psychological health. Sustained RTW was estimated by work status the last 4 weeks before the 2-year date.
Results
Participants with strong job relations who received BI had a higher RTW rate (hazard ratio = 0.74 (95% CI 0.57; 0.96)) and spent more weeks working than participants who received MDI. In the stratum of weak job relations, no difference was seen regarding RTW and weeks working. For health-related outcomes and sustained RTW no significant results were found in neither stratum.
Conclusions
Employees with strong job relations achieved higher RTW rates when receiving BI compared to MDI, while no difference was found between intervention groups for employees with weak job relations.
Trial Registration
Current Controlled Trials ISRCTN14136384. Registered 4 August.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Worldwide, low back pain (LBP) is a common health problem and a major cause of disability and absence from work [1, 2]. Almost half of the people with LBP do not experience improvement after 1 year [3]. The probability of returning to work declines with long-term absence from work due to LBP. Furthermore, the risk of labour market marginalization has increased within individuals with LBP [4], resulting in major financial implications for individuals with LBP and society [3].
The determinants of sickness absence for employees with LBP are not only related to pain and disability, but can also involve occupational and psychological factors [5, 6], which may lead to the need for interventions to facilitate return to work (RTW) [7]. Multidisciplinary interventions (MDI), including worksite visits or psychotherapy, have been documented to result in a higher RTW rate at1-year follow-up compared to usual care [8, 9]. Likewise, brief interventions (BI) such as a clinical examination and advice provided by a doctor and a physiotherapist have shown positive effects on RTW compared to usual care in studies with up to 5 years of follow-up [10,11,12].
Studies comparing MDI and BI in employees on sick leave due to LBP found similar RTW rates for the two interventions up to 5 years after the interventions [13,14,15,16]. A subgroup analysis of our previous study [14, 17] stratifying participants according to job relations showed differences in RTW regarding job relations: Participants who felt they had no influence on their job and/or felt at risk of losing their job (weak job relation), had higher RTW rates with MDI than BI. Opposite, participants who perceived they had influence on their own job and did not feel at risk of losing their job (strong job relation) had better RTW rates with BI than MDI. These subgroup differences regarding job relations were tested in a randomised controlled trial (RCT) design; at 1 year follow-up, this RCT only partly confirmed the results of the subgroup analysis [18]. Participants with strong job relations achieved higher RTW rates when receiving BI than MDI as expected from the subgroup analysis, but there were no differences in RTW rates between participants receiving BI compared to MDI in participants with weak job relations.
Aim
The aim of this study was to evaluate RTW after 2 years in a Danish RCT comparing BI and MDI in employees on sick leave due to LBP and stratified according to job relations. Based on the 1-year follow-up study [18] it was hypothesized that employees with strong job relations would also RTW faster with a 2-year follow-up period when receiving BI compared to MDI, whereas no significant difference concerning time to RTW was expected within the group with weak job relations.
Methods
Study Design, Recruitment and Study Population
The RCT was conducted at the Spine Center, Silkeborg Regional Hospital in Denmark between March 2011 and August 2016. A total of 476 participants from 13 municipalities with a total of 750,000 citizens were recruited through general practitioners (GPs). Inclusion criteria were employees aged 18 to 60 years, on full or partial sick leave from work for 4–12 weeks because of LBP, with or without radiculopathy and ability to speak and understand Danish.
Employees on sick leave with continuing and progressive signs of radiculopathy indicating plans for surgery, back surgery within the last year, specific back diseases, known abuse problems, pregnancy, or primary psychiatric disorders were excluded [18].
The study was registered at Current Controlled Trials (ISRCTN14136384).
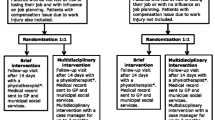
Randomisation and Blinding
All participants with LBP completed a baseline questionnaire before the initial clinical examination. Based on two questions: “Do you have influence on work planning?” and “Do you feel at risk of losing your job due to the present sick leave?” participants were divided into two groups based on either strong or weak job relations. Participants who answered “yes” to the first question and “no” to the second question were allocated to the group of strong job relations, whereas the remaining participants were allocated to the group of weak job relations. In addition, participants with an ongoing compensation claim were allocated to the group of strong job relations, as our previous subgroup analysis showed that participants with a compensation claim and strong job relations returned to work faster when receiving BI [17]. Each group was randomised 1:1 by a computer number generator to receive BI or MDI. The initial clinical examination was double-blinded, but due to the nature of the interventions, both participants and caregivers were aware of which of the two interventions participants received afterwards [19].
Interventions
The interventions have previously been described in detail [19]. In short, all participants underwent a clinical low back examination by a rheumatologist including measurement of range of motion and estimation of tender points. In addition, results from Magnetic Resonance Imaging (MRI) of the lumbar spine were explained to the participant. Furthermore, the participants were informed that exercise and physical activity is the best documented treatment for LBP, and that psychosocial distress can prolong and worsen pain. An examination by a physiotherapist including a mechanical evaluation and advice on exercise was carried out. Participants with radiculopathy were informed about the good prognosis and about the possibility of surgery if case of no improvement. All participants were advised to RTW when possible. Finally, a follow-up visit with the physiotherapist was scheduled 2 weeks later.
In addition to the brief intervention, MDI included a comprehensive interview with a case manager (a social worker, an occupational therapist or a specialist in social medicine) within a week after the first consultation. The interview covered work, private life, psychological pain management and any uncertainties related to RTW. A tailored rehabilitation plan for RTW was made jointly by the participant and the case manager including a time schedule for gradual RTW and a realistic workload. Appointments with individual team members were arranged when relevant. The entire multidisciplinary team including the rheumatologist and the physiotherapist discussed the rehabilitation plan, and a copy of the plan was sent to the municipal job centre. In addition, the case manager arranged a meeting at the workplace or contacted the employer by phone upon agreement with the participant. When the participant had returned to work or this was deemed impossible after 3 months, the intervention was stopped.
Vocational Outcomes
The primary outcome was time to RTW and defined as the period between randomisation and RTW. RTW was operationalised as not receiving any social transfer income except unemployment benefits or flexible job compensation for at least four consecutive weeks.
As secondary outcomes the cumulative incidence proportion (CIP) of participants having returned to work during the 2-year follow-up was measured as well as sustained RTW, defined as the percentage of participants working during the last 4 weeks up to the 2-year date after randomisation. Moreover, the median time to RTW was measured. The participants were divided into five groups according to their weekly employment status and the median number of weeks was assessed; (1) working, (2) sick leave benefits, (3) interdisciplinary rehabilitation programme (vocational, educational and social activities with the purpose of improving the person’s ability to work [20]), 4) cash benefits (financial support provided to people unable to support themselves by employment), and 5) disability pension.
Information about vocational outcomes was obtained from the Danish Register for Evaluation of Marginalisation, DREAM, which is administrated by the Danish Agency for Labour Market and Recruitment and contains weekly information on public transfer payments [21].
Health and Disability Outcome
Participants completed a questionnaire about health and disability at baseline and after 2 years. Pain intensity was measured by the Low Back Pain Rating scale, consisting of six questions on actual, worst and average level of back and leg pain within the last two weeks. A sum score (0–60) was calculated, higher scores indicating more pain [22]. Disability was assessed by the Roland Morris disability scale (0–23), which include 23 questions with “yes” (1) or “no” (0) responses, a higher number indicating more disability. In case of a missing answer, it was considered a “no” [23]. Symptoms of bodily distress, illness worry, anxiety and depression were assessed by the Common Mental Disorder Questionnaire (CMDQ) [24]. It contains Likert scales from 0 (not at all) to 4 (extremely) to rate symptoms within the last 4 weeks. Fear avoidance was measured by three items from the Orebro Musculoskeletal Pain Questionnaire [25]. A sum score (0–30) was calculated, and higher scores expressed a higher level of fear avoidance. Health-related quality of life (HRQoL) was measured by Euroqol (5Q-5D-3L) and an index value was calculated by the Danish country-specific values [26].
Analysis
Cox proportional hazards regression analysis was used to compare RTW rates by means of hazard ratios (HR) in the two intervention groups within the group with strong job relations as well as the group with weak job relations. We included death, emigration, early retirement and retirement as competing risks in the analyses. Kaplan Meier curves were made to show the rate and fraction of participants having returned to work. We analysed sustained RTW by using the Chi-squared test and the median number of weeks in the five different groups of employment status using the Wilcoxon rank-sum test.
Changes in scores for health and disability from baseline until 2-year follow-up were analysed by the t-test between the intervention groups in each stratum.
Comparisons of baseline characteristics of non-responders of the 2-year follow-up questionnaire between the intervention groups were made by the Chi-squared test, the t-test, Fisher’s exact test or the Wilcoxon rank-sum test. Furthermore, analysis of baseline characteristics of responders and non-responders of the 2-year follow-up questionnaire was made also using the Chi-squared test, the t-test, Fisher’s exact test or the Wilcoxon rank-sum test.
The statistical significance level was P < 5%, and all statistical analyses were performed in Stata/MP 16.1.
Results
Vocational Outcomes
A total of 476 employees on sick leave due to LBP were included in the study. The 204 participants with weak job relations and no compensation claim were randomised to MDI (n = 102) or BI (n = 102). Likewise, the 272 participants with strong job relations and/or an ongoing compensation claim were randomised to MDI (n = 135) or BI (n = 137). Within the stratum of strong job relations, participants receiving BI had a significantly higher RTW rate than participants receiving MDI (HR = 0.74 (95% CI 0.57; 0.96)) as well as a significantly higher CIP and lower median time to RTW; however, no difference in sustained RTW was observed. In the stratum of weak job relations, no significant difference was seen in RTW rates, CIP, median time to RTW or sustained RTW (Table 1; Fig. 1).
Participants with strong job relations who received BI spent significantly more weeks working compared to participants who received MDI (Table 2). Within the stratum of weak job relations, no significant differences were found regarding weeks spent in the five different groups of employment status between participants in MDI and BI, respectively.
Health and Disability Outcomes
In total, 188 (69%) participants with strong job relations and 131 (64%) participants with weak job relations completed the 2-year follow-up questionnaire (67% overall response rate). Non-responders in the two intervention groups were similar regarding all baseline variables in both strata, except that non-responders randomised to MDI had a significantly higher HRQoL than non-responders randomised to BI among participants with strong job relations (data not shown). In both strata, non-responders were younger than responders among participants randomised to BI, and non-responders with strong job relations randomised to BI had a lower HRQoL compared to responders.
For all health and disability outcomes, no significant difference in changes from baseline until 2-year follow-up was found between any of the intervention groups. In general, pain intensity and disability were reduced, and psychological health was improved, including fear avoidance, illness worry, bodily distress, anxiety and depression symptoms and HRQoL was higher (Table 3).
Discussion
The findings support the 1-year follow-up analysis, showing that employees with strong job relations had a higher RTW rate when receiving BI compared to MDI [18]. Furthermore, hazard ratios between the two interventions for participants with strong job relations obtained at 1-year follow-up and 2-year follow-up were very similar, 0.73 and 0.74 respectively. Similar to 1-year follow-up, no significant difference in RTW rates was found for employees with weak job relations allocated to BI compared to MDI (1.07 and 0.99 after 1- and 2-year follow-up, respectively) [18]. Moreover, the results concerning weeks in different employment status groups are in accordance with the results regarding RTW rates, showing more weeks with work for employees receiving BI compared to those receiving MDI among employees with strong job relations, and no significant differences among employees with weak job relations. There was no difference in sustained RTW between the intervention groups for participants with weak or strong job relations.
As opposed to 1-year follow-up, no significant differences were seen regarding health and disability outcomes in this study. An explanation for this may be dilution over time of the few differences previously found regarding HRQol, bodily distress and symptoms of depression.
Our finding of a significantly higher RTW rate if allocated to BI compared to MDI for participants with strong job relations was supported by a study by Skouen et al. [27]. In that study, men with chronic LBP who received a light-version of MDI had increased RTW compared to those who received a comprehensive version of MDI. Therefore, a more intensive or longer lasting intervention may postpone RTW for some employees. Employees with strong job relations have influence on work planning and do not feel at risk of losing their job, therefore a case manager and a tailored rehabilitation plan for RTW as well as contact with the workplace as a part of the intervention might cause unnecessary delay of RTW for this group of employees.
Other studies comparing BI and MDI found no differences in RTW at 2-year follow-up [13, 15]. Those findings are in accordance with the results for employees with weak job relations in the current study and confirm that a clinical low back examination and reassuring explanations are sufficient for most employees. Less than half of the participants allocated to MDI received a workplace intervention [18], as most of the participants declined that the case manager contacted their workplace. Thus, a potential effect of this part of the intervention cannot be estimated. Sustained RTW was lower among participants with weak job relations compared to participants with strong job relations confirming their feeling of being at risk of losing their job. Therefore, involvement of the workplace might be especially important for this group of employees. According to a Cochrane review [28], workplace interventions have been reported as a crucial element in increasing RTW for individuals on sick leave due to LBP, provided there is close cooperation with the workplace and changes on the workplace are possible. The beneficial effect of workplace interventions in general has been confirmed in a recent meta-analysis, but not for workers on sick leave [29]. Mandatory workplace involvement, or legislation protecting this vulnerable group of employees, could possibly improve the outcome for employees with LBP, especially for those with weak job relations.
The median time working for employees with strong job relations was more than a year (60 and 75 weeks for MDI and BI, respectively), during the 2-year follow-up, while the employees with weak job relations worked around a year (the corresponding weeks were 54 and 57.5). Overall, employees only received cash benefits and disability pension for a few weeks, while a tendency was seen that a slightly higher number of weeks was spent on participation in an interdisciplinary rehabilitation programme. The number of weeks spent in these groups of employment status were very small since being granted these benefits takes time, therefore the trend must be followed.
In the total population, 60% were working at 2-year follow-up (sustained RTW), while 82% at some point during follow-up had returned to work (CIP). When performing a RTW survival analysis, the participants returning to work are excluded (censored), and therefore the percentage of participants returning to work may continue to increase although fewer participants work, because some of the participants succeeding in RTW at first will return to sick leave later. Thus, it is also relevant to estimate the number of participants at work up to the 2-year date, i.e., sustained RTW.
Two years after the start of the intervention only around half of the participants with weak job relations were working, while 60–70% among participants with strong job relations were working. Thus, status after 2 years might provide a more realistic picture of the attachment to the labour market than the CIP.
Methodological Considerations
A major strength of this study was that the vocational outcomes were based on the DREAM register, ensuring complete follow-up and reduced selection bias. As in several other studies, RTW was defined as four consecutive weeks of not receiving social transfer income [14, 30, 31]. The initial clinical examinations were double-blinded, which may have reduced treatment bias. Furthermore, a large sample size and the computer-based randomisation were strengths of the present study. Randomisation of the participants regarding baseline variables was successful [18], which reduced the risk of confounding and selection bias.
Furthermore, the health and disability variables were based on validated questionnaires with modest response rates of 69% for participants with strong job relations and 64% for participants with weak job relations at 2-year follow-up. Non-responders randomised to MDI had a significantly higher HRQoL at baseline than non-responders randomised to BI among participants with strong job relations implicating a risk of selection bias. However, given that non-responders in the two intervention groups were similar regarding all other baseline variables in both strata, we consider the potential selection bias regarding the health and disability outcomes to be minor.
Conclusions
During the 2-year follow-up, employees who reported strong job relations achieved higher RTW rates and worked more weeks when receiving BI compared to MDI. For employees with weak job relations, no differences in RTW rates and weeks working were found between the two intervention groups. These results are in accordance with the results reported at 1-year follow-up.
Based on this study; BI is recommended as the standard intervention in employees on sick leave due to LBP.
Data Availability
Data from the study is only available on request due to privacy/ethical restrictions.
Code Availability
Not applicable.
References
Hoy D, March L, Brooks P, et al. (2014) The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73:968–74. https://doi.org/10.1136/annrheumdis-2013-204428.
Cieza A, Causey K, Kamenov K, et al. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:P2006-2017.
Hoy D, Brooks P, Blyth F, et al. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24:769–81. https://doi.org/10.1016/j.berh.2010.10.002.
Gordon W. The back pain revolution. 2nd edn. Edinburgh: Churchill Livingstone; 2007.
Valentin GH, Pilegaard MS, Vaegter HB, et al. Prognostic factors for disability and sick leave in patients with subacute non-malignant pain: a systematic review of cohort studies. BMJ Open. 2016;6: e007616. https://doi.org/10.1136/bmjopen-2015-007616.
Steenstra IA, Munhall C, Irvin E, et al. Systematic review of prognostic factors for return to work in workers with sub acute and chronic low back pain. J Occup Rehabil. 2017;27:369–81. https://doi.org/10.1007/s10926-016-9666-x.
Werner LE, Côté MP, Fullen AB, et al. Physicians’ determinants for sick-listing LBP patients: a systematic review. Clin J Pain. 2012;28:364–71. https://doi.org/10.1097/AJP.0b013e31822cf64f.
Marin TJ, Van Eerd D, Irvin E, et al. Multidisciplinary biopsychosocial rehabilitation for subacute low back pain. Cochrane Database Systematic Rev. 2017. https://doi.org/10.1002/14651858.CD002193.pub2.
Salathé CR, Melloh M, Crawford R, et al. Treatment efficacy, clinical utility, and cost-effectiveness of multidisciplinary biopsychosocial rehabilitation treatments for persistent low back pain: a systematic Review. Los Angeles: SAGE Publications; 2018. p. 872–86.
Hagen EM, Grasdal RA, Eriksen RH. Does early intervention with a light mobilization program reduce long-term sick leave for low back pain: a 3-year follow-up study. Spine. 2003;28:2309–16. https://doi.org/10.1097/01.BRS.0000085817.33211.3F.
Indahl A, Haldorsen EH, Holm S, et al. Five-year follow-up study of a controlled clinical trial using light mobilization and an informative approach to low back pain. Spine. 1998;23:2625–30. https://doi.org/10.1097/00007632-199812010-00018.
Karjalainen K, Malmivaara A, Mutanen P, et al. Mini-intervention for subacute low back pain: two-year follow-up and modifiers of effectiveness. Spine (03622436). 2004;29:1069–76.
Brendbekken R, Eriksen H, Grasdal A, et al. Return to work in patients with chronic musculoskeletal pain: multidisciplinary intervention versus brief intervention: a randomized clinical trial. J Occup Rehabil. 2017;27:82–91. https://doi.org/10.1007/s10926-016-9634-5.
Jensen C, Jensen OK, Christiansen DH, et al. One-year follow-up in employees sick-listed because of low back pain: randomized clinical trial comparing multidisciplinary and brief intervention. Spine. 2011;36:1180–9. https://doi.org/10.1097/BRS.0b013e3181eba711.
Jensen C, Jensen OK, Nielsen CV. Sustainability of return to work in sick-listed employees with low-back pain. Two-year follow-up in a randomized clinical trial comparing multidisciplinary and brief intervention. BMC Musculoskelet Disord. 2012;13:156. https://doi.org/10.1186/1471-2474-13-156.
Pedersen P, Nielsen CV, Jensen OK, et al. Employment status five years after a randomised controlled trial comparing multidisciplinary and brief intervention in employees on sick leave due to low back pain. Scand J Public Health. 2018;46:383–8. https://doi.org/10.1177/1403494817722290.
Stapelfeldt CM, Christiansen DH, Jensen OK, et al. Subgroup analyses on return to work in sick-listed employees with low back pain in a randomised trial comparing brief and multidisciplinary intervention. BMC Musculoskelet Disord. 2011;12:112. https://doi.org/10.1186/1471-2474-12-112.
Langagergaard V, Jensen OK, Nielsen CV, et al. The comparative effects of brief or multidisciplinary intervention on return to work at 1 year in employees on sick leave due to low back pain: A randomized controlled trial. Clin Rehabil. 2021. https://doi.org/10.1177/02692155211005387.
Pedersen P, Nielsen CV, Andersen MH, et al. Comparing multidisciplinary and brief intervention in employees with different job relations on sick leave due to low back pain: protocol of a randomised controlled trial. BMC Public Health. 2017. https://doi.org/10.1186/s12889-017-4975-3.
Reform of the Disability Pension and Flexi-job Scheme (2012) https://www.star.dk/en/recent-labour-market-policy-reforms/reform-of-the-disability-pension-and-flexi-job-scheme-2012/. Accessed 28–10 2020.
Hjollund NH, Larsen FB, Andersen JH. Register-based follow-up of social benefits and other transfer payments: accuracy and degree of completeness in a Danish interdepartmental administrative database compared with a population-based survey. Scand J Public Health. 2007;35:497–502. https://doi.org/10.1080/14034940701271882.
Manniche C, Asmussen K, Lauritsen B, et al. Low Back Pain Rating scale: validation of a tool for assessment of low back pain. Pain. 1994;57:317–26. https://doi.org/10.1016/0304-3959(94)90007-8.
Albert HB, Jensen A-M, Dahl D, et al. Criteria validation of the Roland Morris questionnaire. A Danish translation of the international scale for the assessment of functional level in patients with low back pain and sciatica. Ugeskrift Laeger. 2003;165:1875–80.
Christensen KS, Toft T, Frostholm L, et al. Screening for common mental disorders: who will benefit? Results from a randomised clinical trial. Fam Pract. 2005;22:428–34. https://doi.org/10.1093/fampra/cmi032.
Linton JS, Boersma JK. Early identification of patients at risk of developing a persistent back problem: the predictive validity of the Örebro musculoskeletal pain questionnaire. Clin J Pain. 2003;19:80–6. https://doi.org/10.1097/00002508-200303000-00002.
EQ-5D-3L User Guide Version 6.0 December 2018, https://euroqol.org/publications/user-guides/. Accessed April 2020.
Skouen JS, Grasdal AL, Haldorsen EM, et al. Relative cost-effectiveness of extensive and light multidisciplinary treatment programs versus treatment as usual for patients with chronic low back pain on long-term sick leave: randomized controlled study. Spine (Phila Pa 1976) 2002; 27: 901–909; discussion 909–910. DOI: https://doi.org/10.1097/00007632-200205010-00002.
van Vilsteren M, van Oostrom SH, de Vet HCW, et al. Workplace interventions to prevent work disability in workers on sick leave. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.CD006955.pub3.
Russo F, Papalia GF, Vadalà G, et al. The effects of workplace interventions on low back pain in workers: a systematic review and meta-analysis. Int J Environ Res Public Health. 2021;18:12614.
Lambeek LC, van Mechelen W, Knol DL, et al. Randomised controlled trial of integrated care to reduce disability from chronic low back pain in working and private life. BMJ. 2010;340:1035. https://doi.org/10.1136/bmj.c1035.
Anema JR, Steenstra IA, Bongers PM, et al. Multidisciplinary rehabilitation for subacute low back pain: graded activity or workplace intervention or both? A randomized controlled trial. Spine (Phila Pa 1976). 2007;32:291–8. https://doi.org/10.1097/01.brs.0000253604.90039.ad.
Acknowledgements
Thank you to all the participants and stakeholders.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
OKJ and CVN contributed to the study conception and design. KKWP made the analyses and wrote the first draft of the manuscript. All authors significantly contributed to the interpretation of data and revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Ethical Approval
This study was performed in accordance with the Declaration of Helsinki. The study was approved by the Danish Data Protection Agency (no. 1-16-02-86-16) and by the Central Denmark Region Committees on Health Research Ethics (no. M-20100193).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
All participants sign informed consent in relation to their participation in the study and to the use of their health data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pedersen, K.K.W., Langagergaard, V., Jensen, O.K. et al. Two-Year Follow-Up on Return to Work in a Randomised Controlled Trial Comparing Brief and Multidisciplinary Intervention in Employees on Sick Leave Due to Low Back Pain. J Occup Rehabil 32, 697–704 (2022). https://doi.org/10.1007/s10926-022-10030-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-022-10030-1