Abstract
Efficient management of the operating room (OR) contributes to much of today’s healthcare expenditure and plays a critical role in generating revenue for most healthcare systems. Scheduling of OR cases with the same team and surgeon have been reported to improve turnover time between cases which in turn, improves efficiency and resource utilization. We aim to assess different operating room procedures within multiple subspecialties and explore the factors that positively and negatively influence turnover time (TOT) in the operating room. We conducted a retrospective review of cases that were completed on weekdays between 0600 and 2359 from July 2017 through March 2018. Cases between 0000 and 0559 were excluded from this study. Of the total 2,714 cases included in our study, transplant surgery had the highest mean TOT (71 ± 48 min) with orthopedic surgery cases without robots having the lowest mean TOT. OR cases in rooms with the same specialty had significantly less mean TOT compared to rooms switching between different subspecialties (70 vs. 117 min; p < 0.0001). Similarly, cases with the same surgeon and anesthesia team had a significant lower TOT (p < 0.0001). Consecutive specialty, surgeon, anesthesiologist, and prior procedure ending before 15:00 were all independent predictors of lower TOT (p < 0.0001). Our study shows scheduling cases with the same OR team for elective cases can decrease TOT and potentially increase operating room efficiency during the day. Further studies may be needed to assess the long-term effects of such variables affecting OR TOT on healthcare expenditure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The effective management of operating room (OR) start times and turnover times (TOT) have been linked to better management of hospital resources and meeting the increasing demands of quality, low-cost healthcare [1]. Most of today’s healthcare expenditure and hospital’s revenue are generated in the OR [2], making the intraoperative period—the moment the patient rolls into the OR—a target for efficiency efforts among the staff and surgical teams. With the current ruling CMS-1694-F from the Centers for Medicare and Medicaid Services on the transparency of healthcare costs to the general public [3], hospital systems have shifted focus on implementing ways to improve healthcare delivery efficiency, with most emphasis in the OR. Thus, a well-managed and efficient OR contributes significantly to the financial stability of many healthcare systems.
Efficiency in the OR can be measured during both the operative and non-operative period and includes staff utilization, scheduling and timing accuracy of cases, the preoperative testing period, case start times and the time patients get wheeled in and out of the OR which also considers the time spent in the intraoperative period. The operative and non-operative related factors to improving TOT have been studied to improve healthcare operations and meet the expectations of patients. A prospective study demonstrated that a robust OR efficiency training of the staff involved in the TOT can positively influence faster turnover rates and procedural start times [4]. With regards to the influence the OR staff have on TOT, some studies have examined the positive effects that a nursing team in the OR during the turnover phase is associated with increase in surgical time and total procedure time [5], while other studies found no association between consistent OR staff and TOT [6]. Studies have also explored how the overlapping of anesthetic inductions, and pre-operative regional anesthesia block before the patient enters the OR influences the TOT [7, 8]. These studies highlight the importance of the human resource related factors and the multidisciplinary approach in ensuring that longer operative times are minimized. Yet, less attention has been paid to the influence of TOT in specific OR team members—the surgeon, anesthesia team and nursing team together—have on the OR turnover rate, and the overall implication of the operating work environment in the effective utilization of hospital resources.
In this study, we aim to assess different operating room procedures by different subspecialties and explore the factors that positively and negatively influence turnover time in the operating room. This study specifically explores if the same surgeon, specialty dedicated ORs, and same anesthesiology team improve efficiency in terms of TO. In addition, we analyze the OR TOT data to identify the etiology of delays and propose recommendations to enhance the workflow process to meet patients’ needs while concurrently improving the intraoperative efficiency.
Methods
Study population
A retrospective review of scheduled procedures from July 1, 2017 through March 31, 2018 completed in the ORs of a tertiary, academic teaching hospital. Analyzed cases were restricted to adult elective, scheduled surgical procedures that were completed on weekdays and occurred between 0700 and 2359. Pediatric cases, urgent and emergent cases, add-on cases, and cases starting between 0000 and 0659 were excluded.
Data collection
Case data was tracked prospectively within the institution’s electronic health record system. Baseline characteristics included case type, patient status (inpatient vs outpatient), patient check-in time, specialty, type of procedure, primary surgeon, and primary anesthesiologist. Procedural variables analyzed include American Society of Anesthesiologists (ASA) Physical Status, procedure start time, procedure end time, wheel-in time, and wheel-out time. TOT was defined as the time from when the preceding procedure ended to when the subsequent case was wheeled into the OR (wheel-in time minus procedure end time).
Statistical analysis
Baseline characteristics and outcome variables were classified as categorical or continuous variables. The univariate analysis was performed using Wilcox and Kruskal–Wallis tests. A multivariate analysis was performed using a Poisson multivariate regression with TOT as the dependent variable to analyze the impact of confounders including procedure end time with a cut-off of 15:00 given that that is the time for nursing staff shift change, ASA physical status, consecutive surgeon, consecutive anesthesia team, consecutive surgeon, and anesthesia team, whether the surgeon was operating in multiple rooms simultaneously. Statistical analyses were performed using R version 3.6.3 [9]. For the statistical analyses, the following R packages were used: car, dvmisc, generalhoslem, MASS, RColorBrewer, tidyverse, and writexl R packages [10]. Odds ratios (OdR) were calculated with a 95% confidence interval (CI) and significance was determined by p-value less than 0.05.
Results
A total of 2,714 cases were included in the analysis. Cases were divided based on 13 different subspecialties. Mean TOT was highest for transplant surgery cases (109 ± 86 min) and lowest for orthopedic surgery cases (71 ± 48 min) (Table 1 and Fig. 1). When comparing each specialty TOT to other specialties, orthopedic and general surgery cases without robotics had lower mean TOT than all other subspecialties combined, while general surgery with robotics, transplant surgery, plastic surgery, urology, and thoracic surgery had longer mean TOT times than all other subspecialty cases (Supplemental Table).
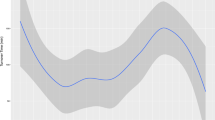
Cases were next analyzed based on the ASA physical status of the following patient. Mean TOT was highest for ASA level 4 cases and this was significantly different from ASA level 2 cases (Table 2 and Fig. 2). ORs with cases with the same specialty had lower mean TOT than rooms with cases switching between specialties (70 vs. 117 min; p < 0.0001). Cases with the same surgeon and/or anesthesiologist team had a lower TOT than cases with different surgeons and/or anesthesiologist (p < 0.0001; Table 3 and Fig. 3).
Upon multivariate analysis of relevant variables affecting turnover, consecutive specialty (OdR 0.86; p < 0.0001), consecutive surgeon (OdR 0.58; p < 0.0001), anesthesiologist (0.72; p < 0.0001), and prior procedure ending before 15:00 (OdR 0.89; p < 0.0001) were independent predictors of lower TOT, while a surgeon running simultaneous procedures in two rooms was predictive of a greater TOT (OdR 1.04; p < 0.0001) (Table 4).
Discussion
This retrospective study of 2,714 OR cases demonstrates that the transition of primary specialty, surgeon, or anesthesiologist in each OR is associated with an increase in TOT between cases throughout the day. This underscores the importance of a cohesive team or unit within a functional OR. Through a multivariate analysis, our results showed that rooms with a consecutive surgeon, consecutive anesthesiologist, as well as case end-times prior to 1500 were all independently associated with decreased TOT.
Our study found an association between change in primary surgeon on TOT. Specifically, results showed that TOT between cases with the same surgeon was shorter than TOT between cases with different surgeons (median TOT: 66 vs. 110 min, p < 0.0001). These findings were similar to a study of 53,036 cases by Austin et al. who found the mean TOT for rooms following cases with the same surgeon to be lower than rooms with different surgeons in following cases by 7.4 min (43.6 vs. 50.0, p < 0.0001). Another study also found prolonged tracheal extubation if there are less than five previous interactions between the anesthesia team and primary surgeon [11]. One possible reason for the observed prolonged time increase is that different surgeons typically use different instrumentation and set up thus requiring more time between cases [12]. Institutions will often use block booking, the practice of scheduling one surgeon to one operating room for up to a full day, as a strategy to meet elective surgical demand and maximize anesthesia productivity. Keeping the same surgeon in the room, when possible, would also decrease the amount of communication required between teams assigned to each case. Theoretically, this could decrease the amount of time needed to change equipment or alter set up to fit the preferences of a different surgeon.
Our study also found an association with significance among TOT in ORs that followed cases with surgeons of the same specialty. Results found median TOT to be 70 min in rooms with surgeons following in the same specialty compared to 117 min in ORs following with surgeons of a different specialty (p < 0.0001). Austin et al. found there to be a small increase (7.3 min) in TOT when changing specialties between cases [12]. Another study that looked at TOT from the perspective of tardiness as defined by minutes beyond the scheduled time a patient is rolled into the OR showed no significant delay in the second case when switching specialties [13]. One possible explanation for these findings is that designating ORs for a given specialty allows for easier communication within departments and understanding of OR preferences to optimize the time between cases.
Additionally, our study found that there is a significant decrease in TOT based on consecutive anesthesiologist/anesthesia teams (mean 68 vs. 98, p < 0.0001) as compared to cases with different teams. The association between TOT and OR teams has been studied and reported in the literature. A study by Stepaniak et al. which evaluated fixed OR teams and turnover times, found that these teams had lower preparation times and TOT among the same consecutive cases. When asked to describe the experience within fixed teams, the study found that surgeons believed that because of extended debriefing at the start of the day and team morale, OR handling was optimized [14]. All in all, this has its scheduling implications and as stated above may be beneficial for specialty designated ORs with significant decrease in TOT.
To assess if patient comorbidities as a variable affects TOT, our study also examined the relationship between different ASA physical status classification system and TOT. The ASA physical status classification has long been established to assess pre-anesthesia medical comorbidities in surgical patients. Since its genesis, this classification system has functioned in conglomeration with other factors (such as type of procedure, frailty, etc.) as a predictor of perioperative complications with rising classes [15]. We found the highest mean TOT (97 min) in ASA level 4 cases and a significantly different TOT in these cases from ASA level 2 cases although this difference was noted when compared to ASA level 1 patients most likely given the lower portion of patients designated ASA level 1 status. Increased average TOT is likely related to the comorbidities associated with difficult or longer intubation/extubation times or immediate post-operative complications. Lindeborg et al. found comorbidities such as chronic obstructive pulmonary disease which may increase risk of extubation failure [16]. Complications such as these can increase time between patients and delay start times of subsequent procedures. In theory, if ASA physical status can be used to manage OR scheduling to prevent stacking of these patient profiles, longer TOT can be anticipated and better optimized to maintain efficiency.
Similarly, effective utilization of the OR staff and support teams schedules could significantly affect the time in between cases. In our study, we found a significant difference in TOT when looking at procedures that began before 1500 and after 1500 (mean 78 vs 96, p < 0.0001). It is worth noting that at 1500 is when most of the shift changes happen for the OR nursing and support staff; thereby, highlighting the importance of understanding how staff changes affect overall OR productivity. Interestingly, Marsusky et al. found no increase in turnover time if the anesthesia team received incremental financial incentive after 1530 to stay after for late OR cases in their study [17]. The significance of these findings underscores the complexity of this study and requires more investigation to determine if the differences are due to inadequate level of staffing once the shift-change occurs or a result of the differences in incentivization structure between the shift-based versus case-based employees.
Our findings warrant further investigation into the long-term implications of these shift-based changes on organizational operational costs. A study that looked at four academic tertiary hospitals estimated that a reduction in average TOT of 3 to 9 min would result in a 0.8 to 1.8% decrease in staffing costs, while reductions in 10 to 19 min would result in 2.5 to 4.0% reduction in staffing costs [18]. While these predictions are specific to the impact reducing TOT could have on staffing costs, it is possible that the impact can be extrapolated to decreasing operational costs. The considerations that exist with ensuring that there is adequate staffing to cover an OR requires coordination between the different groups that comprise the OR teams.
Another technique frequently used to increase efficiency in the OR is scheduling overlapping cases. Decisions surrounding overlapping surgery involves balancing multiple legal, ethical, and operational considerations, as well as regulatory and political pressures within the hospital. In this scenario, the primary attending surgeon must assign immediate availability in the first operating room to another attending surgeon. The patient needs to be informed in either of these circumstances. From a surgeon’s perspective, the rationale behind running two overlapping ORs is to complete more cases efficiently and safely in a day. Theoretically, this allows for the surgeon to operate during the turnover time of the other room. Currently, the decision is often based primarily on patient demand for a specific surgeon and available OR capacity. Our analysis shows that running overlapping ORs actually increases TOT. For the benefits of increased throughput to be realized, other factors such as patient safety, operational/cost factors, and regulatory compliance, need to be considered. It is important to note that economic benefits may be offset by medical-legal risks or lessened overall efficiency if overlapping surgeries are not managed appropriately [19]. Therefore, comparison of overlapping and non-overlapping surgical procedures needs to be further characterized to ensure the safety of running simultaneous ORs [20].
Effective utilization and management of the OR to improve healthcare costs have not only been studied within the healthcare industry but in the corporate world as well. Over the years, several industries including Toyota and Motorola have created the lean management systems and the six-sigma operational model respectively, to streamline their workflow and utilize their resources effectively [21]. These processes were adapted by these corporations to eliminate processes that do not add to product value. Due to its effectiveness in boosting the productivity in the corporate world, lean management systems and six-sigma model have been adopted by not just the automotive industry, but also the Department of Defense [22]. Similarly, it is prudent for the healthcare industry to assess the similarities in these interventions and how they can be applied with the framework of today’s evolving healthcare. Both industries: corporations and healthcare all exist to serve the needs of its consumers or patients, provide safety, and thrive based on the satisfaction of its patrons: consumers and patients alike. Thus, within the operating room workflow, process mapping and deep examinations of each step of the patient journey from preoperative visit to postoperative discharge can have multiplicative benefits that extend from cost savings to maintaining the focus on improving quality and patient/customer safety. Overall, this study underscores the need for a longitudinal assessment of the effects of the perioperative workflow either improves or worsens healthcare expenditure and patient satisfaction.
Limitations
Although a large study in terms of sample size, the retrospective design of our study remains a limitation. The data and documentation available to us based on operative and anesthesia records which limits our ability to verify accuracy. There are certain variables that we were not able to account for in this study including postoperative anesthesia care unit hold times which may lengthen turnover time as patients are held in the OR until a recovery bed is available. Another variable is extubation time (time from procedure end to patient out of room), which may be increased in certain procedures depending on level of anesthesia. This study is also a single institution study. Specific institutional culture and behaviors are likely to be institution-specific and may not be reflective of other academic medical centers. Moreover, there may not be equal representation of all subspecialties within the study as only 13 gynecology oncology cases were included while neurosurgical and orthopedic cases make up more than half the cases reviewed. We also only included elective cases. Urgent or emergent cases that occur usually delay elective cases if there is not another available OR.
Conclusion
TOT can be affected by changes in OR team members, including surgeon and anesthesiologist. Assigning specific ORs to the same team members for elective cases can decrease TOT and potentially increase operating room efficiency during the day. Further prospective, larger studies may be needed to delineate the effect of individual variables on OR efficiency and healthcare cost.
References
Mason SE, Nicolay CR, Darzi A. The use of Lean and Six Sigma methodologies in surgery: a systematic review. Surgeon. 2015;13:91–100.
Barbagallo S, Corradi L, de Ville de Goyet J, Iannucci M, Porro I, Rosso N, et al. Optimization and planning of operating theatre activities: an original definition of pathways and process modeling. BMC Med Inform Decis Mak. 2015;15:38.
Centers for Medicare and Medicaid Services. CMS-1694-F. 2018 [cited 10 Jul 2021]. Available from: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/FY2019-IPPS-Final-Rule-Home-Page-Items/FY2019-IPPS-Final-Rule-Regulations
Overdyk FJ, Harvey SC, Fishman RL, Shippey F. Successful strategies for improving operating room efficiency at academic institutions. Anesth Analg. 1998;86:896–906.
Azzi AJ, Shah K, Seely A, Villeneuve JP, Sundaresan SR, Shamji FM, et al. Surgical team turnover and operative time: An evaluation of operating room efficiency during pulmonary resection. J Thorac Cardiovasc Surg. 2016;151:1391–5.
Bathish MA, McLaughlin M, Kleiner C, Talsma A. The effect of rn circulator-scrub person dyad consistency on total or time and turnover time. AORN J. 2021;113:276–84.
Eappen S, Flanagan H, Lithman R, Bhattacharyya N. The addition of a regional block team to the orthopedic operating rooms does not improve anesthesia-controlled times and turnover time in the setting of long turnover times. J Clin Anesth. 2007;19:85–91.
Torkki PM, Marjamaa RA, Torkki MI, Kallio PE, Kirvelä OA. Use of anesthesia induction rooms can increase the number of urgent orthopedic cases completed within 7 hours. Anesthesiology. 2005;103:401–5.
R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. 2020.
Jay, M. generalhoslem: Goodness of fit tests for logistic regression models. R Package version 134. 2019 [cited 30 May 2020]; Available from: https://CRAN.R-project.org
Epstein RH, Dexter F, Cajigas I, Mahavadi AK, Shah AH, Abitbol N, et al. Prolonged tracheal extubation time after glioma surgery was associated with lack of familiarity between the anesthesia provider and the operating neurosurgeon. A retrospective, observational study. J Clin Anesth. 2020;60:118–24.
Austin TM, Lam HV, Shin NS, Daily BJ, Dunn PF, Sandberg WS. Elective change of surgeon during the OR day has an operationally negligible impact on turnover time. J Clin Anesth. 2014;26:343–9.
Dexter F, Epstein RH, Schwenk ES. Tardiness of starts of surgical cases is not substantively greater when the preceding surgeon in an operating room is of a different versus the same specialty. J Clin Anesth. 2019;53:20–6.
Stepaniak PS, Vrijland WW, de Quelerij M, de Vries G, Heij C. Working with a fixed operating room team on consecutive similar cases and the effect on case duration and turnover time. Arch Surg. 2010;145:1165–70.
Hackett NJ, De Oliveira GS, Jain UK, Kim JYS. ASA class is a reliable independent predictor of medical complications and mortality following surgery. Int J Surg. 2015;18:184–90.
Lindeborg MM, Puram SV, Sethi RKV, Abt N, Emerick KS, Lin D, et al. Predictive factors for prolonged operative time in head and neck patients undergoing free flap reconstruction. Am J Otolaryngol. 2020;41:102392.
Masursky D, Dexter F, Garver MP, Nussmeier NA. Incentive payments to academic anesthesiologists for late afternoon work did not influence turnover times. Anesth Analg. 2009;108:1622–6.
Dexter F, Abouleish AE, Epstein RH, Whitten CW, Lubarsky DA. Use of operating room information system data to predict the impact of reducing turnover times on staffing costs. Anesth Analg. 2003;97:1119–26, table of contents.
Morris AJ, Mello MM, Sanford JA, Green RB, Wald SH, Kadry B, et al. Commentary: How should hospitals respond to surgeons’ requests to schedule overlapping surgeries? Neurosurgery. 2018;82:E91–8.
Hyder JA, Hanson KT, Storlie CB, Glasgow A, Madde NR, Brown MJ, et al. Safety of overlapping surgery at a high-volume referral center. Ann Surg. 2017;265:639–44.
Tagge EP, Thirumoorthi AS, Lenart J, Garberoglio C, Mitchell KW. Improving operating room efficiency in academic children’s hospital using Lean Six Sigma methodology. J Pediatr Surg. 2017;52:1040–4.
Niñerola A, Sánchez-Rebull M-V, Hernández-Lara A-B. Quality improvement in healthcare: Six Sigma systematic review. Health Policy. 2020;124:438–45.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Previous presentation or submissions
None. We confirm that this manuscript has not been previously published in whole or in part, nor has it been submitted elsewhere for review.
Short title
Operating Room Turnover.
Conflicts of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Topical Collection on Implementation Science & Operations Management
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sarpong, K., Kamande, S., Murray, J. et al. Consecutive Surgeon and Anesthesia Team Improve Turnover Time in the Operating Room. J Med Syst 46, 16 (2022). https://doi.org/10.1007/s10916-022-01802-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-022-01802-6