Abstract
Health information exchange (HIE) makes previously inaccessible data available to clinicians, resulting in more complete information. This study tested the hypotheses that HIE information access reduced emergency room visits and inpatient hospitalizations for ambulatory care sensitive conditions among medically indigent adults. HIE access was quantified by how frequently system users’ accessed patients’ data. Encounter counts were modeled using zero inflated binomial regression. HIE was not accessed for 43% of individuals. Patient factors associated with accessed data included: prior utilization, chronic conditions, and age. Higher levels of information access were significantly associated with increased counts of all encounter types. Results indicate system users were more likely to access HIE for patients for whom the information might be considered most beneficial. Ultimately, these results imply that HIE information access did not transform care in the ways many would expect. Expectations in utilization reductions, however logical, may have to be reevaluated or postponed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Exchanging patients’ health information across organizational boundaries through automated systems holds the promise of quality improvements and cost savings for healthcare service organizations [1]. The United States’ “highly fragmented”[2] method of storing health data places an individual’s clinically relevant information in multiple independent repositories. Vital information may be totally unavailable or ineffectively shared when first seeking care at a facility [3, 4] or with a physician [5] because of disparate storage. This problem is illustrated by Finnell and colleagues report that one-quarter of emergency department patients had medical information stored in another hospital system [6]. Similarly, a recent survey of primary care visits reported clinically relevant information was missing in 14% of the time and physicians believed the data were stored outside their information systems in the majority of those instances [7]. The Institute of Medicine (IOM) identified this reality as a threat both to the safety [8] and to the overall quality of healthcare as providers must deliver care “without the benefit of complete information about the patient’s condition, medical history, services provided in other settings, or medications prescribed by other clinicians”[2, p. 4].
In select clinical settings, decisions frequently occur with incomplete medical knowledge;[9] clinicians perceive missing data threatens patient well-being and increases staff time [7]. The availability of a more comprehensive clinical history could improve efficiency by reducing redundancy, particularly in the area of diagnostic testing [10]. Likewise, the availability of a more comprehensive medication history can improve safety [11]. Furthermore, lack of access to information stored by other organizations can be a barrier to effective coordination of care in disease management programs [12, 13], and to the continuity of care [14].
Health information exchange (HIE) makes previously inaccessible data available, resulting in the availability of more complete clinical information, which could improve the quality of care [4, 15]. The available electronic clinical information at the point of care addresses the quality dimension of timeliness [2]. The IOM recommended financial support of, and a commitment to information technology in order to improve quality and efficiency [16]. Additionally, reports suggest HIE may make care more patient centered [17]. Estimates promise substantial savings at the local level [18] and savings measured in the billions from a national HIE system [19].
In addition, reduced utilization in the form of patient encounters is an expected [20] and intended primary effect of HIE [21]. Inpatient hospitalizations generate costs, and preventable hospitalizations are a potential indicator of an inappropriate quality of care [22]. Emergency room utilization is costly [23], associated with both inappropriate care seeking behaviors [24] and indicative of lower health status [25]. Relevant to the practice of healthcare, HIE may be most effective in emergency room settings [4, 15], and a way to reduce inpatient hospitalizations [18]. For policy makers, the recent and substantial investment in health information exchanges [26] makes questions concerning HIE ability to prevent unnecessary encounters particularly relevant [27].
To date, unfortunately, we lack substantial and consistent empirical demonstrations of the effectiveness of HIE [27–29]. A randomized controlled pilot reported sharing of electronic clinical data between emergency departments reduced patient encounter charges [30]. The reported cost reduction, however, occurred under very select circumstances and not uniformly across all study sites. Furthermore, a recent randomized trial of the electronic delivery of a single Canadian emergency department’s information to family physicians found no beneficial results [31]. While furthering our understanding and the acceptability of HIE, theory building case-studies [32], financial estimations [18], implementation concerns [15], and policy discussions [19] dominate the HIE literature. The limited empirical evidence of the effectiveness of HIE in improving outcomes constitutes a serious barrier to its adoption [32, 33].
This investigation addresses this lack of evidence by examining the following hypotheses:
-
1.
Access of HIE information will be associated with a lower inpatient hospitalizations for ambulatory care sensitive conditions.
-
2.
Access of health information exchange information will be associated with lower emergency room utilization.
Materials and methods
Data source
Data for this cohort study come from the Integrated Care Collaboration (ICC) of Central Texas’ master patient index/clinical data repository called I-Care. (The ICC was formerly known as the Indigent Care Collaboration of Central Texas.) Austin area safety net providers, with additional funding from the Robert Wood Johnson Foundation and the Health Resources & Services Administration, founded the ICC in 1997 as a means to improve access, quality, and cost of health care services for the medically indigent. The ICC exists as a separate nonprofit entity with eighteen member organizations including: hospital systems, public and private clinics, and governmental agencies operating federally qualified health centers. The ICC serves a multi-county area and is supported by voluntary membership contributions (Harrington et al., 2007, unpublished).
I-Care is the ICC’s centralized database containing electronic demographic and clinical information from 2002 onwards. As of 2007, I-Care contains more than 3.1 million service encounters representing more than 600,000 unique individuals. ICC’s goal is that I-Care will exist as a shared longitudinal electronic health record for the medically indigent. Therefore, I-Care does not systematically include encounters covered by private insurance or Medicare (unless dual Medicaid eligible). Member organizations contribute patient electronic data to I-Care through secure electronic interfaces. In turn, each location may access data from I-Care at a secured website using a desktop computer with internet access. I-Care is not a full electronic medical record. However, absence of a full electronic medical record is not a barrier to achieving progress to quality improvements [2].
The study dataset is a subset of the entire I-Care population seeking care between January 1, 2005 and June 30, 2007. Since I-Care does not capture privately insured encounters, the individuals in the database do not constitute a fixed cohort. That is, during period of uninsurance, an individual’s encounters are recorded in the database, but during periods of private coverage no records are generated. Study inclusion criteria were defined to select a consistently medically indigent adult population in order to primarily guard against this attrition. Figure 1 summarizes the inclusion criteria. First, the study only included Travis County residents 18 to 64 years old and excluded encounters at the public mental health provider and Planned Parenthood. The latter two providers suppress too many data elements for use in this analysis.
As evident from Fig. 1, Travis County adult residents constituted a minority of the individuals in the system. Data were further restricted to only include individuals who had an I-Care recorded encounter at a private or public health clinic during each of the three calendar years. This requirement reduced the likelihood an individual experienced a privately insured healthcare encounter or left the Austin area, either of which would generate outcomes not included in the dataset. Finally, the ICC collects all encounters of the medically indigent, but only allows the information to be seen across providers if the individual provides written consent. The final data set excluded individuals who had provided consent prior to 2005 and individuals who had not authorized the ICC to share their data across providers. The final study population included 6,114 persons.
Dependent variables
Inpatient hospitalizations due to ambulatory care sensitive hospitalizations (ACSHs) and emergency department visits were the two dependent variables of interest. Both outcomes only included events occurring after the first date of HIE authorization in 2005. All events with ICD-9 codes associated with accidents or pregnancy, labor and delivery were also excluded. ACSHs included those inpatient hospitalizations due to conditions such as asthma, diabetes, ear infections, or pelvic inflammatory disease. ACSHs are preventable hospitalizations [34], and indicators of an absence of timely and appropriate ambulatory care [35]. In addition, ACSHs reduction represents a stated goal of the ICC [36]. Inpatient hospitalizations were classified as ACSHs using the ICD-9 list provided by Shi and colleagues [37].
Independent variables
Electronic security logs documenting I-Care use by healthcare staff were transformed into an information access index in order to measure the degree to which a patient’s HIE information was accessed. The I-Care interface is comprised of several web pages or screens. As part of HIPPA compliance, I-Care security logs document the user’s location, the patient viewed, the date accessed, and information screen viewed. The initial I-Care screen includes basic patient identifying information. From that point, system users may access the available information on previous medical encounters, diagnoses, orders, detailed demographics, medication orders, and payer sources on different screens. The number of different dates on which a patient’s I-Care data were viewed by a system user provided an index of information access. In order to improve model fit due to small counts, the information access index was categorized into four levels. An index value of zero, meaning patients’ data were not accessed, constituted the reference category; the low, medium and high categories were defined by tertile values. The categorized information access index was further reduced to a simple binary variable denoting HIE information viewed or no HIE information viewed. Views by database administrators were not included in calculating the information access index values, nor were any activities like report generation.
Potential confounding variables included clinical, demographic, and service measures. Comorbidity is potential confounding factor as it is associated with utilization outcomes and is a component of underlying health status [38]. The respective ICD-9 codes recorded at any encounter identified asthma, diabetes, hypertension, ischemic heart disease, hypercholesterolemia, and stroke patients. The total number of the aforementioned chronic conditions summed to develop a chronic condition count index. Previous research has shown that basic counts have good predictive, concurrent, and construct validity as a measure of comorbidity [39]. Patient demographics included age, gender, race/ethnicity and marital status at time of first clinic visit in 2005. Service utilization history included the frequency of clinic visits, emergency room usage and hospitalizations in the year prior to the study. Previous frequent emergency department utilization has been demonstrated to be a predictor of continued frequent utilization [40]. Previous utilization history variables were dichotomized into simple occurrence and no occurrence variables.
Statistical analysis
The entire study population was described using frequencies and percents. In addition, descriptive statistics were stratified into persons with no information accessed in the HIE and persons with any information accessed. As a first stage, the simple binary variable denoting HIE information accessed or no HIE information accessed was modeled as the dependent variable in a series of logistic regressions in an attempt to understand the differing levels of HIE information access. A multivariate model was created using a backwards elimination approach based on likelihood ratio testing [41]. Associations were described using odds ratios and 95% confidence intervals.
The second stage of the analysis consisted of the formal hypothesis testing. Individuals were modeled with the categorized information access index as the primary exposure of interest using zero inflated negative binomial regression. Zero inflated negative binomial regression, appropriate for count models, was preferred over both Poisson and negative binomial regression based on overdispersion, the large number of zeros, Vuong test and other standard tests [42, 43]. Unadjusted models were created for each independent variable. A backwards elimination approach based on likelihood ratio testing and Bayesian Information Criterion values was used to create multivariate models. Significance testing for the coefficients was set at alpha = 0.05. Exponentiated parameter coefficients expressed the factor change in the expected outcome for a change in the independent variable.
Results
Table 1 describes the total study population and those with and without information accessed in the HIE. The total study population was predominately female (only 20.9% male) and Hispanic (66.9%). The mean age was 39 years old. The majority of the study population had a least one chronic condition (55.9%), with hypertension (36.7%) and hypercholesterolemia (33.5%) being the most common.
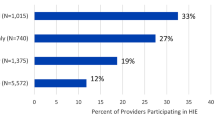
Just more than half (56.6%) of individuals had information accessed in the system. The proportion of patients accessed was much higher than that reported in a previous study [44]. Those whose information was accessed tended to be older (mean = 42.5 vs 35.3), have more chronic conditions (66.4% vs 42.2%) and had more health care encounters in 2004.
Numerous factors were associated with any HIE information access, as indicated in Table 2. Unadjusted for confounding factors, patients who were male (odds ratio (OR) = 1.38), single/divorced/widow (OR = 1.60), homeless (OR = 1.53), or had any of the chronic conditions, all had significantly higher odds of having their HIE information accessed by system users. In addition, a prior year clinic visit, emergency room visit or inpatient hospitalization raised the odds of HIE information access by 130%, 173% and 374% respectively. After adjusting for confounding factors, increasing age (OR = 1.03), number of chronic conditions (OR = 1.13), at least one prior year clinic visit (OR = 1.63), a prior year emergency room visit (OR = 1.96), and being hospitalized in 2004 (OR = 2.02) all increased the odds of HIE information access.
The associations between the level of HIE information access and utilization outcomes of interest are displayed in Table 3. Unadjusted for any confounding factors, increasing HIE information access was statistically associated with the number of emergency room visits. Compared to the individuals without, patients with HIE information accessed one time had an 83% higher expected count of emergency room visits. Likewise, those in the medium access category had a 158% higher expected count and those in the highest access category had a 290% higher expected count. Furthermore, HIE information access level was still associated with increased expected emergency room visits after adjusting for confounding factors. In the best fitting model, all levels of HIE information access were associated with increased expected emergency room visits compared to no information access. Individuals in the highest information access category had a 213% higher expected emergency room visit count. The Cragg–Uhler [42] pseudo-r 2 for the best fitting model was 0.28.
Similar to the models of emergency room usage, more HIE information access was also associated with increased ACSHs. The unadjusted expected count of ACSHs were 261% and 104% higher for the high and medium HIE information access levels, respectively, compared those with no HIE information accessed. Estimates did not vary greatly once adjusted for confounding factors. Both the medium and high levels of HIE information access were statistically associated with increases in the expected counts of inpatient hospitalizations in the best fitting model. The best model had a Cragg–Uhler pseudo-r 2 of 0.27. Figure 2 summarizes how the more HIE information was accessed, the higher the expected counts of emergency room visits and ACSHs.
Discussion
This analysis found accessed HIE information, contrary to the hypothesized relationships, was associated with increased health service utilization. This relationship was consistent both before and after multivariate adjustments for confounding, and for both utilization events examined. In the best fitting models for each of the outcomes, the highest level of information access was statistically higher than the effect from a medium level of access. Results also demonstrated providers’ HIE system access was not random, but specific patient factors increased the odds of information access.
Why was it the case the more a person’s HIE data were examined, the more likely that person was to have more emergency room visits and inpatient hospitalizations? One explanation would be the HIE information was either inadequate or ineffectively utilized. An HIE is a necessary, but in and of itself, an insufficient condition to change healthcare utilization. The existence, retrieval and application of previously inaccessible information are also necessary conditions. However, clinical information seeking is fraught with information retrieval failure [45]. Potentially the HIE system did not provide the necessary data either through absence in the system or it was simply missed by the user. Either of these reasons could fail to transform care and reduce utilization. This conclusion highlights that the application of the HIE information in the care process was unknown in this study. Although the security logs on which the information access index was created document the pages viewed, they tell nothing of system user specific motivation, what information or knowledge was actually sought, or acquired [46].
As an alternative explanation, one could argue the association between increased HIE access and utilization was expected. Factors potentially indicative of complex cases, or in other words simply sicker people, increased the odds of providers accessing the HIE information. Consistent with information seeking theory [47] and information sought by clinicians [48–50], providers may have accessed the data for whom the information would be most useful. The patient characteristics associated with HIE access are characteristics one would expect to generate large amounts of disparately stored health information. Patients whose information was accessed had visits with different providers (hospital or emergency room verses clinic) and had characteristics that can require multiple diagnostics tests and medications [51]. Whereas individuals presenting with minor complaints, or those without chronic conditions, may not have warranted the time and effort to access the system [52]. The later type of patient was less likely to have increased utilization encounters; in contrast, chronic conditions, increased age, prior utilization and other risk factors were predictors of increased utilization. However, multivariate analysis adjusted for differences in health measures and the relationship still persisted. Again, this suggests the HIE as utilized was not associated with a transformation in healthcare.
Additionally problematic, the data indicate the overall quality of care may not have improved either. Implicit in much of the discussion of proposed benefits of HIE endeavors is the assumption more information leads to more informed or better clinical decisions and therefore better quality [4, 9, 15]. While this study did not examine the clinician–patient encounter directly, ACSHs serve as a measure of appropriate and timely care [35, 37]. Overall, hospitalizations from conditions that adequate ambulatory care should prevent [53] increased with levels of HIE.
The potential bias from attrition is the primary threat to this study’s internal validity. The population was selected, at cost to generalizability, to guard against attrition. Although a reasonably consistent medically indigent, local resident population was selected, individuals still could have had healthcare encounters not captured in the system. These encounters could have been either during a period of insurance coverage or occurred in a geography outside the ICC’s catchment area. However, for this to bias results away from a null association, attrition would have had to vary by level of HIE information access. In addition, while all prior utilization variables occurred before and all outcomes were accessed after a patient was included in the HIE system, the level of HIE access was assessed concurrently with the outcome. Therefore sufficient temporal sequence ambiguity prevents any statements of causality.
The generalizability of these results is limited in terms of patients, the HIE system itself and the setting. The study population was comprised solely of medically indigent persons. Therefore, results may not be applicable to the elderly, children, or the insured due to differences in utilization patterns. Also results are not generalizable to the medically indigent excluded from the study population including those who only sought care in emergency departments or did not consistent to participation in the HIE. In actuality, the treatment in this study not only included HIE access, but also the architecture of the system, and the form and content of the information delivered to the provider. While many other HIE systems exist across the country [26], none probably match the I-Care system exactly on all of these points. Further investigations would be necessary to determine the salient points of this system. Finally, this study was set in a single metropolitan area that may not be generalizable both in terms of the population and the local healthcare system.
Also, this study has limitations in construct validity. As stated above, the number of chronic conditions and prior utilization were suggested to be indicators of a case complexity construct. Other factors such, as behaviors, attitudes, or perceived efficacy for example, could be indicators of the same construct or independent constructs, but were unmeasured in this study. It is unknown from the available data the importance these unmeasured indicators in HIE usage.
While these results did not demonstrate the effectiveness of HIE in reducing select healthcare utilizations, they do contribute significantly to our understanding HIE study, operation and potential improvement. First, these results echo the recent identification of knowing who accesses HIE systems and for what purposes as significant needs in our understanding of HIE [21, 54]. The literature already establishes both user characteristics as critical to the usage of electronic health information [55, 56] and the organizational context as a determinant of information technology usage in general [57, 58]. This study adds an empirical demonstration that patient characteristics also influences providers’ HIE access. Additionally, reduced utilization in the form of encounters exists in the literature as an expected outcome from HIE implementation. This expectation is not illogical, particularly since health information technology, in general, improves efficiency [29]. However, this study suggests any expectations of overall reductions in utilization may have to be re-evaluated, or at least postponed until individuals have a larger number of encounters with the system in order to see any benefits.
Significant and substantial resources are required to establish any HIE effort [26], those contemplating adoption HIE have to rely on the experiences of others [59]. Research on the relationships of HIE systems to healthcare utilization that is observable to other healthcare systems, organizations and clinicians is necessary to promote HIE adoption. However, adoption of the HIE cannot be the final stage. HIE organizations like Regional Health Information Organizations, in addition to their concerns over funding, exchange standards and sustainability, need to incorporate plans to evaluate actual usage of the system in the care process [60].
References
U.S. General Accounting Office, Medical ADP systems: automated medical records hold promise to improve patient care. Washington, D.C., 1991.
Institute of Medicine, Crossing the quality chasm: A new health system for the 21st century. National Academy, Washington, D.C., 2001.
Institute of Medicine, The computer-based patient record: an essential technology for health care. revised edition. In: Dick, R. S., Steen, E. B., and Detmer, D. E. (Eds.), National Academy, Washington, D.C., 1997.
National Research Council, Networking health: prescriptions for the internet. National Academy, Washington, D.C., 2000.
Gandhi, T. K., Sittig, D. F., Franklin, M., et al., Communication breakdown in the outpatient referral process. J. Gen. Intern. Med. 15(9):626–631, 2000. doi:10.1046/j.1525-1497.2000.91119.x.
Finnell, J. T., Overhage, J. M., Dexter, P. R., et al., Community clinical data exchange for emergency medicine patients. AMIA Annual Symposium Proceedings 235–238, 2003
Smith, P. C., Araya-Guerra, R., Bublitz, C., et al., Missing clinical information during primary care visits. JAMA. 293(5):565–571, 2005. doi:10.1001/jama.293.5.565.
Institute of Medicine, To err is human, building a safer health system. In: Kohn, L. T., Corrigan, J. M., and Donaldson, M. S. (Eds.), National Academy, Washington, D. C., 2000.
Kalra, J., Medical errors: an introduction to concepts. Clin. Biochem. 37:1043–1051, 2004.
Institute of Medicine. Fostering rapid advances in health care: learning from system demonstrations. In: Corrigan, J., Greiner, A, and Erikson, S. (Eds), Washington, D.C.: National Academy Press, 2003
Bieszk, N., Patel, R., Heaberlin, A., et al., Detection of medication nonadherence through review of pharmacy claims data. Am. J. Health Syst. Pharm. 60(15):360–366, 2003.
Casalino, L., Gillies, R. R., Shortell, S. M., et al., External incentives, information technology, and organized processes to improve health care quality for patients with chronic diseases. JAMA. 289(4):434–441, 2003. doi:10.1001/jama.289.4.434.
Gamm, L., Bolin, J. N., and Kash, B. A., Organizational technologies of chronic disease management programs in large rural multispecialty group practice systems. J. Ambul. Care Manage. 28(3):210–221, 2005.
Kilo, C. M., Transforming care: Medical practice design and information technology. Health Aff. 24(5):1296–1301, 2005. doi:10.1377/hlthaff.24.5.1296.
Shapiro, J. S., Kannry, J., Lipton, M., et al., Approaches to patient health information exchange and their impact on emergency medicine. Ann. Emerg. Med. 48(4):426–432, 2006. doi:10.1016/j.annemergmed.2006.03.032.
Schoen, C., How, S. K. H., Weinbaum, I., et al., Public views on shaping the future of the U.S. health system. The Commonwealth Fund, New York, NY, 2006.
Biondich, P. G., and Grannis, S. J., The Indiana network for patient care: an integrated clinical information system informed by over thirty years of experience. J. Public Health Manag. Pract. (S81–6), 2004.
Frisse, M. E., and Holmes, R. L., Estimated financial savings associated with health information exchange and ambulatory care referral. Journal of Biomedical Informatics. 40(6 S1):S27–S32, 2007.
Walker, J., Pan, E., Johnston, D., et al., The value of health care information exchange and interoperability. Health Aff, 2005. hlthaff.w5.10.
United States Government Accountability Office, Health and Human Services’ Estimate of Health Care Cost Savings Resulting from the Use of Information Technology 2005.
Hripcsak, G., Kaushal, R., Johnson, K. B., et al., The United Hospital Fund meeting on evaluating health information exchange. J. Biomed. Inform. 40(Supplement 1(6)):S3–S10, 2007. doi:10.1016/j.jbi.2007.08.002.
Billings, J., Zeitel, L., Lukomnik, J., et al., Impact of socioeconomic status on hospital use in New York City. Health Aff. (Millwood). 12(1):162–173, 1993. doi:10.1377/hlthaff.12.1.162.
Baker, L. C., and Baker, L. S., Excess cost of emergency department visits for nonurgent care. Health Aff. 13(5):162–171, 1994. doi:10.1377/hlthaff.13.5.162.
Ruger, J. P., Richter, C. J., Spitznagel, E., et al., Analysis of costs, length of stay, and utilization of emergency department services by frequent users: implications for health policy. Acad. Emerg. Med. 11(12):1311–1317, 2004.
Zuckerman, S., and Shen, Y. C., Characteristics of occasional and frequent emergency department users: do insurance coverage and access to care matter? Med. Care. 42(2):176–182, 2004. doi:10.1097/01.mlr.0000108747.51198.41.
Overhage, J. M., Evans, L., and Marchibroda, J., Communities’ readiness for health information exchange: the National Landscape in 2004. J. Am. Med. Inform. Assoc. 12(2):107–112, 2005. doi:10.1197/jamia.M1680.
Marchibroda, J. M., Health information exchange policy and evaluation. Journal of Biomedical Informatics. 40(6 S1):S11–S16, 2007.
Hripcsak, G., Developing common methods for evaluating health information exchange. Journal of Biomedical Informatics. 40(6 S1):S1–S2, 2007.
Chaudhry, B., Wang, J., Wu, S., et al., Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann. Intern. Med. 144(10):742–752, 2006.
Overhage, J., Deter, P., Perkins, S., et al., A randomized, controlled trial of clinical information shared from another institution. Ann. Emerg. Med. 39(1):14–23, 2002. doi:10.1067/mem.2002.120794.
Lang, E., Afilalo, M., Vandal, A. C., et al., Impact of an electronic link between the emergency department and family physicians: a randomized controlled trial. CMAJ. 174(3):313–318, 2006. doi:10.1503/cmaj.050698.
Solomon, M. R., Regional health information organizations: a vehicle for transforming health care delivery? J. Med. Syst. 31(1):35–47, 2007. doi:10.1007/s10916-006-9041-0.
Burton, L. C., Anderson, G. F., and Kues, I. W., Using electronic health records to help coordinate care. Milbank Q. 82(3):457–481, 2004. doi:10.1111/j.0887-378X.2004.00318.x.
Ansari, Z., Laditka, J. N., and Laditka, S. B., Access to health care and hospitalization for ambulatory care sensitive conditions. Med. Care Res. Rev. 63(6):719–741, 2006. doi:10.1177/1077558706293637.
Pappas, G., Hadden, W. C., Kozak, L. J., et al., Potentially avoidable hospitalizations: inequalities in rates between US socioeconomic groups. Am. J. Public Health. 87(5):811–816, 1997.
Indigent Care Collaboration of Central Texas. Summaries of ICC Major Initiatives 2002–2003. 2003 [cited 2007 Sept 6th]; Available from: http://www.icc-centex.org/library/updates/Summaries%20of%20ICC%20Major%20Initiatives%202002–03.pdf.
Shi, L., Samuels, M. E., Pease, M., et al., Patient characteristics associated with hospitalizations for ambulatory care sensitive conditions in South Carolina. South. Med. J. 92(10):989–998, 1999.
Klabunde, C. N., Warren, J. L., and Legler, J. M., Assessing comorbidity using claims data: An overview. Med. Care. 40(8):IV26–IV35, 2002. doi:10.1097/00005650-200208001-00004.
de Groot, V., Beckerman, H., Lankhorst, G. J., et al., How to measure comorbidity: a critical review of available methods. J. Clin. Epidemiol. 56(3):221–229, 2003. doi:10.1016/S0895-4356(02)00585-1.
Okuyemi, K. S., and Frey, B., Describing and predicting frequent users of an emergency department. J. Assoc. Acad. Minor. Phys. 12(1–2):119–123, 2001.
Kleinbaum, D. G., and Klein, M., Logistic Regression, 2nd edition. Springer, New York, 2002.
Long, J. S., and Freese, J., Regression models for categorical dependent variables using Stata, 2nd edition. Stata, College Station, TX, 2006.
Hilbe, J. M., Negative binomial regression. Cambridge University Press, Cambridge, NY, 2007.
Wilcox, A., Kuperman, G., Dorr, D. A., et al., Architectural strategies and issues with health information exchange. AMIA Annual Symposium Proceedings 814–818, 2006.
Elson, R. B., Faughnan, J. G., and Connelly, D. P., An industrial process view of information delivery to support clinical decision making: implications for systems design and process measures. J. Am. Med. Inform. Assoc. 4(4):266–278, 1997.
Haigh, S., Megarity, J., Measuring web site usage: Log file analysis. Network Notes 1998 [cited Oct 9, 2007]; Available from: www.collectioncanada.ca/9/1/pl-256-e.html.
Afifi, W. A., and Weiner, J. L., Toward a theory of motivated information management. Commun. Theory. 14(2):167–190, 2004. doi:10.1111/j.1468-2885.2004.tb00310.x.
González-González, A. I., Dawes, M., Sánchez-Mateos, J., et al., Information needs and information-seeking behavior of primary care physicians. Ann. Fam. Med. 5(4):345–352, 2007. doi:10.1370/afm.681.
Pluye, P., Grad, R. M., Dawes, M., et al., Seven reasons why health professionals search clinical information-retrieval technology (CIRT): Toward an organizational model. J. Eval. Clin. Pract. 13(1):39–49, 2007. doi:10.1111/j.1365-2753.2006.00646.x.
Nygren, E., and Henriksson, P., Reading the medical record. I. Analysis of physicians’ ways of reading the medical record. Comput. Methods Programs Biomed. 39(1–2):1–12, 1992. doi:10.1016/0169-2607(92)90053-A.
Colley, C., and Lucas, L., Polypharmacy. J. Gen. Intern. Med. 8(5):278–283, 1993. doi:10.1007/BF02600099.
Ely, J. W., Osheroff, J. A., Chambliss, M. L., et al., Answering physicians’ clinical questions: obstacles and potential solutions. J. Am. Med. Inform. Assoc. 12(2):217–224, 2005. doi:10.1197/jamia.M1608.
Institute of Medicine. Access to health care in America. In: Millman, M (Ed), Washington, D.C.: National Academy, 1993.
Ash, J. S., and Guappone, K. P., Qualitative evaluation of health information exchange efforts. J. Biomed. Inform. 40(Suppl 1(6)):S33–S39, 2007. doi:10.1016/j.jbi.2007.08.001.
Gamm, L. D., Barsukiewicz, C. K., Dansky, K. H., et al., Pre- and post-control model research on end-users’ satisfaction with an electronic medical record: preliminary results. Proc AMIA Symp. 225–229, 1998.
Dansky, K. H., Gamm, L. D., Vasey, J. J., et al., Electronic medical records: Are physicians ready?/Practitioner application. J. Healthc. Manag. 44(6):440, 1999.
Tornatzky, L. G., and Fleischer, M., The processes of technological innovation. Lexington Books, Lexington, MA, 1990.
Zhu, K., Kraemer, K. L., and Xu, S., The process of innovation assimilation by firms in different countries: A technology diffusion perspective on e-business. Manage. Sci. 52(10):1557–1576, 2006. doi:10.1287/mnsc.1050.0487.
Rogers, E. M., Diffusion of innovations, 5th edition. Free Press, New York, 2003.
Labkoff, S. E., and Yasnoff, W. A., A framework for systematic evaluation of health information infrastructure progress in communities. J. Biomed. Inform. 40(2):100–105, 2007. doi:10.1016/j.jbi.2006.01.002.
Acknowledgements
The author thanks the staff of the Integrated Care Collaboration of Central Texas, particularly Sandy Coe Simmons; and from TAMHSC SRPH Dr. Charles Phillips, SangNam Ahn, Patricia Moore, Darcy Moudouni and Laura Wills for helpful comments and suggestions.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vest, J.R. Health Information Exchange and Healthcare Utilization. J Med Syst 33, 223–231 (2009). https://doi.org/10.1007/s10916-008-9183-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10916-008-9183-3