Abstract
Organ donation rates in the United States are lowest among Asians. Physicians are highly respected in Asian communities and may be influential in promoting donor registration, but little is known about their organ donor registration attitudes. We assessed associations between knowledge, attitudes, personal/professional experience, cultural/religious beliefs surrounding organ donation and donor registration status using multivariable logistic regression. We surveyed 121 Asian physicians in Queens, New York; 22% were registered donors. Registered donors were more likely to discuss donation wishes with their family (OR 9.47, 95% CI 2.60–34.51), know that donor human leukocyte antigen does not need to match organ recipients (OR 6.47, 95% CI 1.66–25.28), and have experience advising patients about organ donation (OR 5.35, 95% CI 1.50–19.02). Culturally tailored educational materials providing updated information to promote family discussion about organ donation could potentially increase Asian physicians’ level of comfort and expertise in discussing organ donor registration with patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Organ transplantation is a life-saving treatment for patients with organ failure. However, the number of patients waiting for organ transplantation continues to far outpace the number of available organs [1,2,3]. For the approximately 120,000 individuals in the United States on the national organ transplant waiting list in 2019, there were only 19,250 organ donations (living and deceased) [4]. Despite various efforts to improve organ donation registration rates, the number of registered organ donors has remained stagnant, particularly among minority populations [4, 5].
Between 2000 and 2015, the Asian population in the United States grew 72% from 11.9 million to 20.4 million with Chinese, Indian and Filipino groups predominantly driving the increase [6]. Nationally, Asian Americans represent 8.3% of the total number of individuals waiting for transplantation but make up only 3.3% of donors in 2019 [7]. In New York State, Queens County is the second most populated county in the state with 2.3 million residents, 27% of whom are Asian Americans [8, 9]. While Asians comprised 11.2% (1072/9554) of the New York State transplant waitlist in 2019, only 5.6% (32/568) of organ donors were Asian, reflecting the widest disparity of any racial/ethnic group [10].
Asians Americans are less likely to register as organ donors among all ethnicities [5, 11,12,13]. The reasons for low organ donation rates among Asian Americans remain incompletely understood and are thought to be related to attitudes toward organ donation, previous experience with organ donation, the role of the family in decision-making, healthcare system mistrust, religious and cultural beliefs, and level of acculturation [14,15,16]. In a scoping review of the literature, Deedat et al. reported on the effectiveness of interventions to increase organ donor registration among minority populations in the United Kingdom (South Asians and individuals of African descent) and North America (African Americans and Hispanics). Interventions fell into one of three categories, mass media campaigns or community-based education alone or in combination [17]. Most effective were ethnically targeted educational interventions, alone or in combination with mass media approaches, that included a strong interpersonal component and the opportunity to register immediately. It has been proposed that culturally competent and sensitive approaches are needed to improve organ donation awareness and registration rates in Asian American communities [14] but, to date, no systematic efforts have been developed to address this issue.
Conceptual Framework
In Asian communities, physicians are greatly respected and play an important sociocultural role, especially among Chinese and Korean subpopulations. Physicians are often viewed as a family advisor with whom the patient has a personal relationship [18] and are sought out for advice beyond immediate health concerns. We hypothesized that physicians could potentially leverage their influence to promote organ donation registration within Asian communities. There is, however, a relative paucity of information about knowledge, attitudes and behaviors related to organ donor registration among Asian physicians to inform their position to influence Asian patients and community members and increase rates of donor registration.
This study aims to bridge the gap by assessing the knowledge and attitudes toward organ donation as well as factors affecting organ donation registration among Asian physicians in Queens County. As an effort supported by the National Institutes of Health (NIDDK R01 DK114893) to improve organ donation rates among Chinese and Korean Americans, the results of this survey study will be used to inform the development of culturally competent interventions among Asian physicians to increase organ donation registration rates in Queens, New York and to serve as a model that can be employed in other areas around the country with large Asian populations.
Methods
Participants and Data Collection
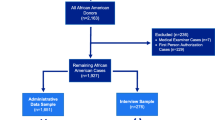
We administered a survey to Asian American physicians practicing in Queens, New York between February and November 2019. To build our relationship with physicians, we reached out to two local physician organizations in Queens (Korean American Physician Independent Practice Association (KAPIPA) and the Association of Chinese American Physicians (ACAP)), attended groups meetings and presented our study to their membership. Each organization then distributed via email an invitation to their members inviting them to participate in a brief survey to better understand the physician’s perspective surrounding organ donation registration. The invitation included an introduction to the study with an anonymous link to a Qualtrics survey that was supported by the organizational leader and signed by the study principal investigator. From among the 487 emails distributed on our behalf (35 from KAPIPA and 452 from ACAP), we received 15 responses. Based on this response, we revised our sampling strategy. Our preliminary analysis of the community demonstrated that approximately two-thirds of the community population in Queens is Chinese American and one-third Korean American. Through a Google search of physicians in the zip code areas, we identified Chinese and Korean physicians with medical practices located in Flushing, Queens and purposively recruited and enrolled physicians to represent the underlying patient population. Our bilingual research coordinators (Chinese/English and Korean/English) reached out to Chinese and Korean physicians at community health events and made visits to community-based clinics and single provider practices within Flushing, Queens to administer surveys in-person. A total of 179 physicians were approached in person and, of these 112 physicians (62%) (72 Chinese, 39 Korean, and 1 Other) agreed to participate in our study and responded the survey. At the time of the face-to-face meeting with the physicians, informed consent was obtained prior to the administration of the survey. Upon completion of the survey, physicians were offered an incentive valued at approximately $25 as compensation for their time and effort. All procedures were approved by the Columbia University Irving Medical Center Institutional Review Board.
Measures
Measures for this survey were gleaned from a systematic literature review [15] coupled with the results of 15 face-to-face key informant interviews conducted (data not published) as part of our formative evaluation. Questions related to the participant and his/her practice, organ donation and donation registration behaviors, knowledge of and attitudes toward organ donation, religious beliefs, and professional experience and training related to organ donation were asked in the survey that was approximately 30 min in duration.
We assessed demographic characteristics including ethnicity (Chinese, Korean, other), sex, age (≤ 50 vs. > 50 years, dichotomized at the mean), marital status (married vs. other), nativity, number of years living in the U.S. (≤ 30 vs. > 30 years, dichotomized at the median), and level of acculturation using a single question that queried participants about the extent of their perceived affiliation with Asian and American cultures [19]. Level of acculturation was then recoded as predominantly American (relatively acculturated), Asian and American identification (bicultural) and predominantly Asian (relatively unacculturated). Participants were also asked questions about the country in which they received their medical education (U.S. vs. non-U.S), practice specialty (primary care vs. other), and any academic affiliations (Yes/No). To assess behaviors related to organ donation registration, we inquired the physicians about their organ donation registration status, whether they had ever discussed their organ donation wishes with family members and whether they had ever donated blood in the past.
We evaluated knowledge of organ donation and donor registration using 16 questions (Cronbach’s α = 0.78) culled from educational material that is widely disseminated by the local organ procurement organization (OPO), LiveOnNY (www.liveonny.org), which is widely responsible for organ donation related activities in the New York metropolitan region. The knowledge questions were framed as True/False/Don’t know questions and later recoded as Correct/Incorrect where “Don’t know” was considered an incorrect response. Questions were grouped as general knowledge about organ donation (n = 4), social issues related to organ donation (n = 5), and the clinical aspects of organ donation (n = 7). We also asked participants to report on their professional experience using 5 items (e.g., “Have any of your patients ever asked you how to become an organ donor?”) and evaluated organ donation related training using a single item (“I have had training and/or attended lectures or courses about discussing the steps to organ donation”). Competence and confidence in discussing organ donation issues with patients was assessed using two questions (“I know enough about organ donation to speak with my patients and their families competently” and “I feel confident in answering questions from relatives of potential organ donors and discussing issues related to organ donation with them”), each scored on a 4-point Likert scale (strongly agree through strongly disagree).
Attitudes and beliefs surrounding organ donation included 14 items (6 positive and 8 negative) (Cronbach’s α = 0.75) that were informed by the existing literature on evaluating organ donation attitudes [20,21,22,23,24]. Religious and spiritual beliefs included 7 items (Cronbach’s α = 0.78) which focused on how different religious beliefs affect individuals’ organ donation intentions [20,21,22,23,24]. Participants were asked the extent to which they agreed or disagreed with attitude and beliefs and religious/spiritual questions based on a 4-point Likert scale.
Analysis
We conducted descriptive analyses that included frequency distributions for categorical variables and, using bivariable analyses (chi-square and Fisher’s exact tests for categorical variables and Wilcoxon rank-sum tests for continuous variables), we examined the relationships between physician demographic and professional characteristics, organ donation-related behaviors, organ donation knowledge, experience, and training, competence and confidence in communicating information about organ donation, attitudes toward organ donation, and religious beliefs and organ donation registration status (registered vs. not registered). Cronbach’s alpha analysis was calculated for knowledge, attitude, and religious scales to assess internal consistency reliability for each scale. Factors associated with organ donor registration were examined using logistic regression. Controlling for sex, independent variables and covariates with P value < 0.05 in the unadjusted analyses were retained and tested in the multivariable model. Results were reported as odds ratios with 95% confidence intervals. P value of < 0.05 determined significance. Data was analyzed using IBM SPSS, version 27 [25].
Results
A total of 127 physicians participated in the survey and, of these 6 were missing > 50% of responses and were excluded from the final analysis. Twenty-seven physicians (22%) were registered organ donors (Table 1). The majority (n = 80, 66%) were Chinese, 60% (n = 72) were male, 92% (n = 112) were born outside of the United States, and among those born abroad, 45% (n = 51) reported living in the U.S. a median of 30 years. More than half (60%, n = 72) identified as Asian or Asian American, more Asian. Sixty-two percent (n = 75) were educated in a country other than the United States, 79% (n = 95) identified as primary care providers, and very few had an academic affiliation (12%, n = 15). No differences in demographic characteristics and organ donation registration were observed.
Less than one-quarter of physicians (22%, n = 27) reported having a family discussion about their wishes regarding their decision to become a registered organ donor, however 56% (n = 15) of registered donor physicians stated that they had communicated this wish to their families compared to 13% (n = 12) of those who were not registered donors (p < 0.001) (Table 2). Knowledge of general information related to organ donation was generally high except for knowledge that New York State has the lowest percentage of registered donors in the country (27%, n = 32). Most were aware of facts related to the social aspects of organ donation but only 36% (n = 43) recognized that all major religions approve of organ donation. With regard to clinical knowledge, participants were less familiar with relatively new information that the donor’s human leukocyte antigen (HLA) does not have to be an identical match to the organ recipient (44%, n = 53) and that Hepatitis C virus (HCV) carriers can be solid organ donors (28%, n = 34). Those who correctly stated that HLA does not have to be an identical match more often were registered donors (74%, n = 20 vs. 35%, n = 33, p = 0.001). Although 74% (n = 89) of participants had cared for a patient who have received a transplant, fewer had experiences communicating with patients about organ donation (34%, n = 41), had patients who were organ donors (34%, n = 41), had patients who were on the waiting list for a transplant (62%, n = 75), or referred a patient for transplant (52%, n = 63). Registered donors twice as often reported that they had been engaged in a conversation about becoming an organ donor with a patient (56%, n = 15 vs. 28%, n = 26, p = 0.007). A little more than one-third (35%, n = 42) stated that they had ever received any type of training about organ donation and less than half felt they knew enough about organ donation to speak competently with patients (42%, n = 51) or were confident in answering questions from patient family members about issues related to organ donation (45%, n = 55).
In general, respondents held positive attitudes toward organ donation (Table 3). All respondents agreed that organ donation is a charitable and noble act that benefits society All registered donors (n = 27) agreed that medical teams would work just as hard to save a life of a registered donor; surprisingly, 95% (n = 89) of non-registered donors also agreed with this statement which is an often cited concern among those who do not register. Negative attitudes were not as frequently mentioned as positive attitudes and the most reported negative attitude was having an uneasy feeling at the thought of their body being cut up or taken apart after death (49%, n = 59). While 20% (n = 24) of participants felt that organ donation was against filial piety, 80% (n = 97) did not think organ donation is antithetical to filial piety, one of the Confucius ideologies frequently cited as a reason for not becoming registered organ donors among Asians [15]. Negative attitudes more often reported by those not registered included thoughts that their family would object if they registered (43%, n = 40 vs. 19%, n = 5, p = 0.02), the importance of the body to remain complete and intact after death (49%, n = 46 vs. 22%, n = 6, p = 0.01), that it is uncomfortable to think or talk about organ donation (46%, n = 43 vs. 22%, n = 6, p = 0.03), and that the thought of the body being cut up after death creates an uneasy feeling (56%, n = 53 vs. 22%, n = 6, p = 0.002).
Approximately two-thirds (67%, n = 83) of the respondents identified themselves as either religious or spiritual, and thought religious and spiritual beliefs are an important part of life (60%, n = 73) (Table 3). All participants agreed that organ donation is a charitable and noble act and very few respondents expressed agreement with negative statements such as organ donation disturbs the process of passing away (20%, n = 24) and made the body incomplete (15%, n = 18). Overall religious and spiritual beliefs were not significantly different between registered and non-registered respondents.
In the multivariable logistic regression analysis testing the association of factors related to being a registered organ donor, we included sex, level of acculturation, having had a discussion with the family about personal wishes surrounding organ donation, and selected knowledge, experience, and attitude questions found to be statistically significant in the univariable tests (Table 4). Results showed that organ donor registration among Asian physicians is associated with having a family discussion about one’s wishes (odds ratio [OR] 9.47, 95% confidence interval [95% CI] 2.60–34.51), knowledge that the donor’s HLA does not need to be identical to the transplant recipient (OR 6.47, 95% CI 1.66–25.28), and having had a patient ask advice about becoming an organ donor (OR 5.35, 95% CI 1.50–19.02).
Discussion
As the potential role that physicians can play in improving organ donation awareness and registration rates among the public is in large part driven by their professional experience and training and personal attitudes and beliefs, these issues deserve further investigation. Physicians, especially in Asian communities, are often seen as thought leaders to whom patients can turn to for advice beyond immediate health concerns [26,27,28]. In this study, we assessed physicians’ knowledge and experience, attitudes, and religious and spiritual beliefs regarding organ donation, and evaluated their relationship with physicians’ organ donation registration status. We found that only 22% of physician respondents were registered organ donors and, among those who were registered, a discussion with the family was strongly associated with organ donor registration as was knowledge of the newest information related to the donor eligibility, and professional experience that includes communicating directly with patients about organ donation and registration.
That Asian physicians who are registered donors more often engaged in family discussion regarding this decision is not surprising and is consistent with previous studies which also reported knowledge and family discussion being positively associated with organ donation registration among Asians [21, 26, 29, 30]. Confucian ideology prioritizing family above all, highlighting the importance of culturally sensitive educational materials [29, 30] and the role of culture-specific values and beliefs involved in the decision whether to register as an organ donor among Asian Americans. Although, the literature is scant on U.S. physicians’ attitudes toward organ donation, a study of medical residency and fellowship program directors across the U.S. in which 76.3% (539/706) of responding physicians were registered donors, reasons for declining organ donation registration included religious reasons, concerns about poor medical care should a donor require care, and negative beliefs about the current organ allocation system [31]. A second study of 106 American surgeons and medical students in New York City with 49% who reported being a registered donor found that refusers cited experience on the transplant service underlying their decision not to register (18%), with the majority of those (83%) citing the procurement procedure specifically as the barrier, another 16% refused based on religious beliefs [32]. Conversely, we did not find that religious beliefs or clinical experience differed between Asian American physicians who registered vs. those who have not registered as organ donors in our cohort.
Overall knowledge was significantly higher among registered respondents, consistent with the findings of previous studies [21, 26, 33, 34]. However, it was surprising that majority of physicians performed poorly on the clinical questions. While physicians who were registered donors more often knew that the human leukocyte antigen (HLA) of the donor does not need to be identical to the transplant recipient, less than one-third of the respondents knew that Hepatitis C virus carriers can also be solid organ donors, albeit this is a relatively recent development in transplantation with the potential to expand the donor pool. This finding suggests that additional educational efforts may be needed to provide physicians with updates beyond their initial training.
Further, there was also an overall lack of confidence to speak with patients about organ donation related topics among the surveyed physicians. This lack of confidence to speak with patients about organ donation may reflect the lack of organ donation-related training and professional experiences reported by many. This suggests an opportunity for patient-driven physician behavior dynamic, where physicians may feel compelled to learn more about the topics that are inquired about by patients. We suggest this is evidence that the current training and educational materials are not sufficient to ensure physicians are up to date with information about organ donation, but that receiving any training, regardless of the quality, might have a beneficial effect on physicians’ confidence level for discussing organ donation with patients.
While our study was limited by a relatively small sample size and was observational in nature, it is the first of its kind to evaluate the factors that contribute to organ donation registration among Asian physicians. Our study was limited to a specific geographic location (Queens, NY) and to Chinese and Korean physicians, but this lack of geographic/demographic diversity was by design. Due to the low organ donation registration rate among Asian Americans in the U.S. and the wide disparity in organ transplant need and organ donors in Asian populations, the high concentration of Asians in Queens provided a unique environment in which to conduct our investigation. Although we inquired about organ donation discussions with the family, we did not specifically ask about the temporality of the discussion. That is, we did not ascertain if the conversation occurred prior to registration for those who registered or afterward and thus cannot comment on the impact of the family to dissuade an individual from registering if the discussion occurred first. Because of physician reluctance to disclose their precise age among 17% of participants, we were unable to assess the relationship of age to organ donor registration status, but others have found that individuals 54 years of age and younger are more likely to be a designated organ donor compared to those 55 years of age and older (OR 1.31, 95% CI 1.03–1.67) [35].
New Contribution to the Literature
This study identified several factors that appear to influence physicians’ organ donor registration status and indicates the opportunity for education for the physicians. Culturally competent educational materials tailored to address specific cultural values and provide updated information to promote family discussion about organ donation could potentially increase Asian physicians’ willingness to register as organ donors themselves and increase their level of comfort and expertise in discussing organ donor registration with patients and lay members of the community, thus contributing to increased registration among Asians.
References
Wolfe RA, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341(23):1725–30.
Rabbat CG, et al. Comparison of mortality risk for dialysis patients and cadaveric first renal transplant recipients in Ontario, Canada. J Am Soc Nephrol. 2000;11(5):917–22.
Oniscu GC, et al. Impact of cadaveric renal transplantation on survival in patients listed for transplantation. J Am Soc Nephrol. 2005;16(6):1859–65.
United States Department of Health and Human Services Health Resources and Services Administration (HRSA). Organ Procurement and Transplantation Network, National data. https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/. (2020). Accessed 3 June 2020.
Weaver M, et al. Organ donation among Asians and Pacific Islanders: preliminary research findings. J Health Care Poor Underserved. 2003;14(2):182–93.
Lopez G, et al. Pew Research Center: Key facts about Asian Americans, a diverse and group population. Pew Research Center. https://www.pewresearch.org/fact-tank/2017/09/08/key-facts-about-asian-americans/. (2017). Accessed 26 July 2020.
United States Department of Health and Human Services Office of Minority Health. Organ donation and Asian Americans. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=57#:~:text=While%208.3%20percent%20of%20the,Asian%20American%20donors%20in%202019. (2020). Accessed 26 July 2020.
United States Census Bureau. QuickFacts: Queens County (Queens borough), New York. https://www.census.gov/quickfacts/queenscountyqueensboroughnewyork. (2019). Accessed 3 June 2020.
Asian American Federation. New York City Council Districts and Asian Communities. http://www.aafederation.org/cic/briefs/2017citycouncilbrief.pdf. (2017). Accessed 3 June 2020.
(HRSA) USDoHaHSHRaSA. Organ procurement and transplantation network: State data. https://optn.transplant.hrsa.gov/data/view-data-reports/state-data/. (2020). Accessed 26 July 2020.
Rubens AJ. Racial and ethnic differences in students’ attitudes and behavior toward organ donation. J Natl Med Assoc. 1996;88(7):417–21.
Organ Procurement and Transplantation Network. National data. https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/. (2020). Accessed 3 June 2020.
United States Census Bureau. The Asian Population: 2010, Census Briefs. https://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf. (2012). Accessed 3 June 2020.
Siminoff LA, et al. Family first: Asian Americans’ attitudes and behaviors toward deceased organ donation. J Racial Ethn Health Disparities. 2020;7(1):72–83.
Li MT, et al. Cultural barriers to organ donation among Chinese and Korean individuals in the United States: a systematic review. Transpl Int. 2019;32(10):1001–18.
Park HS, et al. Ethnic differences in intention to enroll in a state organ donor registry and intention to talk with family about organ donation. Health Commun. 2009;24(7):647–59.
Deedat S, Kenten C, Morgan M. What are effective approaches to increasing rates of organ donor registration among ethnic minority populations: a systematic review. BMJ Open. 2013;3(12):e003453.
Yang Q, et al. Chinese minority perceives the doctor-patient relationship differently: a cultural and economic interpretation. Front Public Health. 2019;7:330–330.
Suinn RM, et al. The Suinn-Lew Asian Self-Identity Acculturation Scale: concurrent and factorial validation. Educ Psychol Meas. 1992;52(4):1041–6.
Rumsey S, et al. Influence of knowledge and religiousness on attitudes toward organ donation. Transpl Proc. 2003;35(8):2845–50.
Chung CK, et al. Attitudes, knowledge, and actions with regard to organ donation among Hong Kong medical students. Hong Kong Med J. 2008;14(4):278–85.
Luo AJ, Xie WZ, Wei W, Wan QQ, Deng XT. Public opinion on organ donation after death and its influence on attitudes toward organ donation. Ann Transpl. 2016;21:516–24.
Parisi N, Katz I. Attitudes toward posthumous organ donation and commitment to donate. Health Psychol. 1986;5(6):565–80.
Lam WA, McCullough LB. Influence of religious and spiritual values on the willingness of Chinese-Americans to donate organs for transplantation. Clin Transpl. 2000;14(5):449–56.
IBM SPSS Statistics for Windows, Version 27.0 [computer program]. Armonk, NY: IBM Corp.; 2020
Hu D, Huang H. Knowledge, attitudes, and willingness toward organ donation among health professionals in China. Transplantation. 2015;99(7):1379–85.
Kim JR, et al. Korean health professionals’ attitudes and knowledge toward organ donation and transplantation. Int J Nurs Stud. 2004;41(3):299–307.
Andresen J. Cultural competence and health care: Japanese, Korean, and Indian patients in the United States. J Cult Divers. 2001;8(4):109–21.
Chung J, et al. Knowledge and opinions of deceased organ donation among middle and high school students in Korea. Transpl Proc. 2015;47(10):2805–9.
Wu AM. Discussion of posthumous organ donation in Chinese families. Psychol Health Med. 2008;13(1):48–54.
Alkhatib AA, Maldonado AQ, Adbel Jalil A, Hutson W. Physicians’ attitude toward organ donation and trasnplantation in the USA. Clin Transpl. 2014;28(2):149–51.
Hobeika MJ, et al. U.S. surgeon and medical student attitudes toward organ donation. J Trauma. 2009;67(2):372–5.
Bresnahan M, et al. A theory of planned behavior study of college students’ intention to register as organ donors in Japan, Korea, and the United States. Health Commun. 2007;21(3):201–11.
Bresnahan M, et al. The culture of the body: attitudes toward organ donation in China and the US. Chin J Commun. 2008;1(2):181–95.
Sehgal NKR, et al. The relationship between verified organ donor designation and patient demographic and medical characteristics. Am J Transpl. 2016;16(4):1294–7.
Acknowledgements
This study was supported by a Grant from the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases (NIH/NIDDK R01 DK114893) to Drs. Sumit Mohan and Grace Hillyer.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, M.T., Hillyer, G.C., Kim, D.W. et al. Factors that Influence Organ Donor Registration Among Asian American Physicians in Queens, New York. J Immigrant Minority Health 24, 394–402 (2022). https://doi.org/10.1007/s10903-021-01182-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-021-01182-y