Abstract
Ethnic disparities in labor pain management exist. Our purpose is to identify patients’ attitudes and beliefs about epidural analgesia in order to develop a culturally competent educational intervention. A prospective observational study was conducted in patients admitted for vaginal delivery between July 1st–31st, 2009. Inclusion criteria were: singleton, term, cephalic, normal fetal heart tracing and no contraindications for epidural. Patients were surveyed regarding their wishes for analgesia, and their reasons for declining epidural. The obstetrics physician performed pain management counseling as is usually done. Patients were asked again about their choice for analgesia. Likert scale questionnaires were used. Wilcoxon signed ranked test was used for categorical variables. Logistic regression was performed to look for predictors of epidural request. Fifty patients were interviewed. Average age was (27.9 ± 6.7), gestational age (39.3 ± 1.3), and a median parity of 2 (range 0–6). 72% declined epidural upon admission, and 61% after counseling (P = 0.14). Most common reasons for declined epidural were ‘women should cope with labor pain’ (57%), ‘fear of back pain’ (54%) and ‘family/friends advise against epidural’ (36%). Acculturation was assessed by years living in the US (10 ± 6.3), preferred language (Spanish 80%) and ethnic self-identification (Hispanic 98%). 38% were high school graduates. In multivariate logistic regression, graduation from high school was the only variable associated to request for epidural in labor (OR 4.94, 95% CI 1.6–15.1). Educational level is associated to requesting an epidural in labor. Knowledge of patients’ fears and expectations is essential to develop adequate counseling interventions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
The process of labor is accompanied by intense pain in many women. There is no other situation in which it is considered acceptable for a person to experience untreated severe pain, amenable to safe intervention, while under a physician’s care [1].
Pain relief is an important aspect of the management in laboring women. The American College of Obstetricians and Gynecologists recommends the administration of analgesia in labor upon patient request [1]. Regional analgesia provides a superior level of pain relief during labor when compared with systemic drugs and should be available to all women.
The Institute of Medicine report, “Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare” shows evidence that there are important differences in health and the healthcare experience based on race, sex, age, socioeconomic status, and community characteristics [2]. There are two distinctive sources of disparities: (1) healthcare systems and the legal and regulatory climate in which they operate and (2) discrimination such as biases, stereotyping, and uncertainties in clinical communication and decision making [2]. In an elegant review of racial and ethnic disparities in pain, Green et al. [3] identified the need of further research to assess the impact of economic factors, language, acculturation, and family and health support in the treatment of pain.
The cornerstone for quality pain care is appropriate assessment of pain; however there is evidence that minorities are less likely to have their pain assessed. When their pain is assessed, minorities often receive less pain medication than their white counterparts, suggesting variability in physician decision making [4].
There are several theories of why racial and ethnic minorities are less likely to receive epidural in labor. Pain perception, patient preferences and provider bias are some possibilities [5]. Mistrust of the healthcare system by minorities has also being implicated in the underuse of epidural analgesia [6].
There are cultural differences that also may explain the choice of analgesia in labor. In addition, the family influence in decision making is well recognized in the Latino population [7].
Partner influence, as whether to select an epidural has been documented. In a survey of 320 women the day after delivering, Harkins et al. [8] reported a strong association between partner preference and epidural acceptance (OR 25.1 95% CI 5.2–122).
Different strategies can be applied to educate patients and their relatives regarding pain control during labor. Such educational interventions are most beneficial if done prior to the onset of labor (i.e. during prenatal care visits), since it has been shown that an antenatal analgesia plan is strongly associated with the likelihood of requesting and receiving analgesia [9]. Unfortunately, given the high percentage of patients who present in labor in certain hospitals, with little prenatal care, this is not always feasible. Therefore, a survey of patient’s expectations and perceptions regarding epidural analgesia would help discern reservations about pain relief in this population, and also would allow the development of adequate educational interventions.
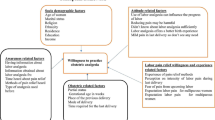
Our primary objective was to explore different factors that might influence the patient’s perception of epidural analgesia. Our secondary objective was to develop a comprehensive culturally competent educational tool for pain relief during labor.
Materials and Methods
We performed a prospective observational study of patients admitted to the Labor and Delivery unit at our institution between July 1–31st 2009. Inclusion criteria were pregnant women admitted for delivery at term, with a singleton in cephalic presentation, a normal fetal heart rate tracing, and no contraindications to receive epidural anesthesia. We created a short survey using nine questions assessing attitudes towards epidural analgesia, with the responses in a five-point Likert-format. We also included demographic information in the survey. We created the survey using a focused discussion among the authors based on the available literature [8, 9]. Health practitioners in our unit examined the final survey for content validity.
After determination of labor or reason for induction subjects were given the survey in the triage area. Once in a labor and delivery room, the obstetrics resident physician performed counseling for pain management, and offered the patient the different options for pain relief. The patients were then asked again regarding their analgesia choice. All patients were approached in their native language with the help of an interpreter if the resident physician was not proficient in Spanish.
Statistical analysis was performed using Stata 10 (College Station, TX). Wilcoxon signed-rank test was used to compare pre and post counseling responses regarding desire for epidural analgesia. Contingency tables with chi-squared testing compared independent sample proportions. Multiple logistic regression analysis examined potential predictors of epidural request. All statistical tests were two-tailed, and P values less than 0.05 were considered significant. The protocol was reviewed and approved by the Committee for the Protection of Human Subjects at the University of Texas Health Science Center at Houston (HSC-MS-09-0272).
Results
Fifty patients admitted to the Labor and Delivery unit at LBJ hospital were interviewed. The average age was 27.9 ± 6.7 years, gestational age 39.3 ± 1.3 weeks, and median parity 2 (0–6). Number of years living in the US was 10.2 ± 6.3. Table 1 shows demographic and baseline characteristics. Ninety- two% of subjects had prenatal care starting during the first or second trimester. Only 27% of patients recall any explanation of analgesia options for labor during their visits. From these subjects who recall analgesia discussions in the clinic 21.4% (3/14) requested an epidural upon arrival, as opposed to 30.5% (11/36) of patients that did not recall counseling in the clinic (P = 0.51). 2 patients reported attendance to antenatal education classes. The degree of acculturation was measured by the years living in the US (10 ± 6.3), percentage of patient’s life spent in the US (37 ± 24%) preferred language (Spanish 80%) and ethnic self-identification (Hispanic 98%). 72% of patients were originally from Mexico and the rest were from different Central American countries. Table 2 lists the responses to the different questions asked regarding pain control in labor and epidurals upon admission.
Twenty-eight % (n = 14) of subjects responded agree/strongly agree to planning on having an epidural pre-counseling which increased to 38% (n = 19) after they received analgesia counseling, however this difference did not reach statistical significance (P = 0.28). Acceptability of epidurals decreased in 7 patients after counseling. Eighty-nine % of the subjects expressed satisfaction with the counseling provided. Forty-six % (n = 23) actually received an epidural before a vaginal delivery, 20% (n = 10) received parenteral analgesia and 34% (n = 17) did not receive any pain relief. This number compares to the epidural rate of 39% for vaginal deliveries (1498/3482) in the previous year at our institution. From the 22 patients that requested an epidural, 65% did so at 5–6 cm cervical dilation. Among these 22 patients, 8, changed from initially not wanting to wanting an epidural, 12 did not change their request, and 2 opted to decline an epidural. There were not clinically important differences in the cervical dilation of the 3 groups. The most common cited health reasons to avoid an epidural was fear of paralysis (76%), followed by fear of chronic back pain (54%).
As seen in Table 3, number of years living in the US, degree of education and admission in labor showed a statistically significant association with the decision to ask for an epidural on admission, in the univariate analysis.
We performed a logistic regression analysis with the number of years living in the US, admission in labor, and level of education as the predictor variables and the initial intention to get an epidural as the criterion variable. Level of education was the only variable that remained statistically significant (Adjusted OR 4.94, 95% CI 1.6–15.1).
Discussion
Our results support the notion that level of education is related to the request of adequate pain relief in labor. We theorize that patients with a higher level of education have a better understanding of the true risks and benefits of the epidural analgesia and the actual risk magnitude. We think that a well informed patient will have less fear of this type of analgesia. In agreement with our results, Sheiner et al. [10] reported in 447 consecutive laboring patients, a strong association between high education level and epidural analgesia acceptance (OR 90.09, 95% CI 27.02–257.06). In our sample we did not find an association between any of the questions that intended to measure acculturation and the desire to get an epidural.
In our sample, we had an epidural rate use of 46% for vaginal deliveries, similar to a 39% epidural rate during the previous year in our institution. This rate is slightly lower than the 51% percent rate reported in a national survey of hospitals with more than 1,500 deliveries per year [11]. Our hospital serves exclusively patients in the public sector, and this could influence the lower epidural uptake rate as previously reported in similar patient populations [5, 12].
Our study is limited by a small sample size. However, our primary goal was to explore the barriers to adequate pain relief in our patients in order to develop a culturally sensitive educational tool. Even though a large percentage of patients agreed that pain was a fact of labor, 73% answered that epidurals should be available upon request. This finding supports the notion that there is no evidence that minority patients have different pain management expectations [13]. As health care providers we are obligated to ensure that these expectations are met.
We recognize that we do not have data in all eligible consecutive patients, mainly due to limitations in the study personnel availability during the weekends or at night. This could explain the observed higher than expected induction rate in our sample, and also could have influenced the results, since patients admitted in labor were indeed more likely to request an epidural.
Our numbers don’t allow definitive conclusions regarding the effect of counseling on a patient’s acceptance of epidural. Patients who changed their mind towards getting an epidural had more advanced cervical dilation. Goldberg et al. [9] described that the strongest factor for epidural analgesia was an antenatal plan to have an epidural; in our study, however, patients who had discussed epidurals with their provider during their prenatal care were no more likely to accept epidurals.
The rate of prenatal care was surprisingly high, which is encouraging because it will give us a better opportunity for counseling in the clinic setting. In our sample 4% of the patients reported attendance to antenatal education classes, and only 27% of patients recalled any analgesia discussion in the clinic. This finding gives us at least 2 additional settings in which we could greatly improve our patient counseling process.
We found that the most common reasons cited for the patients to avoid an epidural were the fear of paralysis and chronic back pain. Thirty-six % reported that their family and friends advised them against an epidural. With this information, we have developed an educational tool to address the issues identified as barriers for adequate pain relief during labor. The educational tool consists of a patient education pamphlet addressing the fears and misconceptions regarding epidural, with real numbers from the literature, explained in simple terms. In addition an interactive session with the results of the study will be given to residents in OB and anesthesia, as well as CRNA’s. In the next phase of the study we will assess the impact of the educational tool.
In conclusion, educational level is associated to requesting an epidural in labor. Even though the patients may not ask for an epidural, it should be available at all times during the labor course. Being aware of patients’ fears and expectations is essential to develop adequate counseling interventions.
References
Pain relief during labor. ACOG Committee Opinion No 295. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2004;104:213.
Institute of Medicine of the National Academies: Unequal Treatment: Confronting racial and Ethnic Disparities in Healthcare. In: Smedley BC, Stith AY, Nelson AR, editors. Washington DC: National Academies Press, 2002.
Green C, et al. The unequal burden of pain: confronting racial and ethnic disparities in pain. Pain Med. 2003;4(3):277–94.
Green C. Racial and ethnic disparities in the quality of pain care. Anesthesiology. 2007;106:6–8.
Glance LG, et al. Racial differences in the use of epidural analgesia for labor. Anesthesiology. 2007;106:19–25.
Lillie-Blanton M, Brodie M, Rowland D, Altman D, McIntosh M. Race, ethnicity, and the health care system: public perceptions and experiences. Med Care Res Rev. 2000;57(Suppl 1):218–35.
Marin G, Marin B. Research with Hispanic populations. Newbury Park: Sage; 1991.
Harkins J, Carvalho B, Evers A, Mehta S, Riley E. Survey of the factors associated with a woman’s choice to have an epidural for labor analgesia. Anesthesiology research and practice 2010; 2010 Article ID 356789 Epub Jun 29 2010.
Goldberg A, Cohen A, Lieberman E. Nulliparas’ preferences for epidural analgesia: their effects on actual use in labor. Birth. 1999;26(3):139–43.
Sheiner E, Sheiner EK, Shoham-Vardi I, Gurman G, Press F, Mazor M, Katz M. Predictors of recommendation and acceptance of intrapartum epidural analgesia. Anesth Analg. 2000;90:109–13.
Hawkins JL, Gibbs CP, Orleans M, et al. Obstetric anesthesia work force survey, 1981 versus 1992. Anesthesiology. 1997;87:135–43.
Roberts CL, Tracy S, Peat B. Rates for obstetric intervention among private and public patients in Australia: population based descriptive study. BMJ. 2000;321:137–41.
Lee WW, Burelbach AD, Fosnocht D. Hispanic and non-Hispanic white patient pain management expectations. Am Emerg Med. 2001;19:549–50.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Orejuela, F.J., Garcia, T., Green, C. et al. Exploring Factors Influencing Patient Request for Epidural Analgesia on Admission to Labor and Delivery in a Predominantly Latino Population. J Immigrant Minority Health 14, 287–291 (2012). https://doi.org/10.1007/s10903-011-9440-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10903-011-9440-2