Abstract
Housing access and the built environment are both recognized as significant social determinants of health. Numerous studies and articles detail housing-based interventions that result in improved health outcomes. However, less is known about potential financial impacts and which programs and initiatives not only improve health but also generate return on investment (ROI). Through a systematic literature review, the authors identified evidence regarding the economic benefits of housing interventions aimed at improving health, using ROI as a measure of program success. Specifically, housing interventions that are aimed at childhood asthma, HIV, chronic illness among the homeless, and urban blight have demonstrated a positive ROI ranging from 30 to 480%, with most cost savings attributed to meaningful reductions in hospitalizations and emergency department visits.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
1.1 The connection between housing and health
Housing has been established as a significant social determinant of health as access to housing and the safety of the built environment can affect both health and quality of life (Office of Disease Prevention and Health Promotion 2018). Likewise, sufficient evidence now shows that specific housing interventions can improve certain health outcomes (Jacobs et al. 2010). Looking back further, connections between housing quality and health have been well established, as multiple studies have examined how features of the built environment impact health. For example, homes in the United States, especially those built before 1978, can be a considerable source of lead exposure. This exposure can irreversibly affect brain and nervous system development and result in intellectual and learning disabilities (Committee on Environmental Health 2005). Additionally, multiple hazards often coexist in homes and cause co-occurring health problems. In-home exposure to factors such as tobacco smoke, cooking pollutants, asbestos, and volatile organic compounds are correlated with respiratory illnesses and some cancers (Bonnefoy et al. 2004). Serious injuries or death can be caused in part by the lack of or inadequacy in housing features such as smoke detectors, rail guards, balconies and heating systems (Braubach and World Health Organization 2011). Furthermore, mental health is also impacted by housing quality; for instance, crowded housing can result in poorer cognitive and psychomotor development, anxiety, stress, aggression and social withdrawal in children (Evans 2006).
In addition to home quality, being unstably housed (having inconsistent access to permanent housing) can lead to even more adverse outcomes, and homeless individuals and families have been identified as a priority area for both health policy and practice (Fitzpatrick-Lewis et al. 2011). One study of select U.S. cities found that homeless individuals had life expectancies of between 42 and 52 years, compared to 78 in the general population (O’Connell 2005). Homeless individuals also use the Emergency Department (ED) as much as four times more often than low-income but stably-housed individuals (Bharel et al. 2013).
Research has shown that supportive housing initiatives have led to a range of positive outcomes for homeless individuals with chronic illnesses, including decreased ED visits, stress and mortality, as well as increased medication adherence and mental health and wellbeing (Dodd et al. 2018). One possible reason for these outcomes is that housing with a supportive component often includes case management and other services that may serve to address health issues for the tenants (Rog 2004). Not only have housing quality interventions demonstrated similar positive effects on general health, but also reduced activity limitation, fewer missed work and school days, and increased symptom-free days for those with chronic illnesses (Woods et al. 2012; Sommer et al. 2011; Campbell et al. 2015).
1.2 Healthcare trends and expenditures in the U.S
The U.S. spends substantially more on healthcare, both on a per capita basis as well as a percentage of Gross Domestic Product (GDP), than other developed countries with similar life expectancy (Dieleman et al. 2017). In 2016, expenditures for Medicaid, the national healthcare program administered by states that covers medical costs for those with limited income resources, reached $565.5 billion, which accounted for 17% of total National Health Expenditures (CMS.gov). While the expenditure is in-line with the approximately 1 in 5 people in the U.S. who are covered by Medicaid or the Children’s Health Insurance Program (CHIP), improving health and addressing social determinants present unique opportunities and challenges alike.
Health insurance in the U.S., including Medicaid, has moved from predominantly fee-for-service models to managed care with an eye toward value-based payment and risk sharing arrangements between payers (health insurance companies) and healthcare service providers. Risk sharing may create an environment more conducive to large-scale investments in prevention and the impetus for dismantling silos between various service systems (e.g. housing and health), providing a unique opportunity to utilize healthcare spending to address social determinants that drive health outcomes. Managed Care Organizations, which oversee significant health plan coverage in the U.S., may increasingly move from smaller pilot initiatives to scaling up proven models to invest in non-medical health services in-line with the goals of the Triple Aim of Healthcare: improve outcomes, decrease per capita cost, and enhance patient experience (Berwick et al. 2008).
Payers, providers, and policymakers have focused significant time and investment into targeting and predicting who will incur the most healthcare costs followed by strategic interventions that offer savings in the form of reduced service utilization. As policymakers and health care industry leaders aim to build value-based systems that address biomedical and sociomedical issues, housing emerges as an area of investment that could yield benefits to patients, communities, and hospital systems. Medicaid Managed Care Organizations have recently begun to make such investments, directing initiatives toward lower income Americans who are historically more likely to face disproportionate barriers to attaining and maintaining quality housing (Collinson et al. 2015).
1.3 Return on investment—an opportunity to measure impact
Numerous studies and articles detail housing-based interventions that result in improved health outcomes (Thomson et al. 2001, 2009). Gibson et al (2010) also found through a systematic review evidence for improving ‘area characteristics’ and ‘energy efficiency interventions.’ Less is known and has been written, however, regarding findings of potential financial impacts and which programs and initiatives not only improve health but also generate economic benefits. Fenwick et al. (2013) conducted a systematic review of economic analysis of the health impacts of housing improvement programs but found that housing improvement studies often failed to collect relevant economic data or collected data inconsistently. Additionally, Fenwick et al. (2013) found that many studies only considered economic costs and benefits derived by program participants rather than broader costs to the healthcare system.
The present review seeks to investigate evidence for direct economic benefits of housing interventions to healthcare systems. Return on investment (ROI) was chosen as a measure of program success due to its straightforwardness and the ease with which ROIs may be compared across programs. Although the authors did not limit the literature search to articles exclusively pertaining to the U.S., ROI is a particularly salient measure in the U.S. healthcare context where costs are high (Dieleman et al. 2017) and Managed Care Organizations are often for-profit entities (Landon and Epstein 2001).
ROI refers to a measure of program efficiency expressed by the ratio of a program’s net profit to its cost:
While ROI analyses are common in business and commercial contexts, they are also used to evaluate healthcare interventions. Unlike other economic analyses such as cost-benefit analyses (CBAs), cost-effectiveness analyses (CEAs), or cost-utility analyses (CUAs), ROI analyses typically only consider direct costs and savings or gains produced by a program (FGDC 2009). By contrast, CBAs can take into account all net societal gains and costs (FGDC 2009) while CEAs and CUAs are expressed as cost per specific health outcome (e.g. cost per quality adjusted life year gained in the case of CUAs) (Birch and Gafni 1992). Of note, ROI analyses for healthcare interventions in the U.S. may be more complex than in typical business or commercial settings due to systemic relationships between public and private stakeholders. For example, private healthcare providers and payers may be concerned with direct reductions in healthcare costs (e.g. reductions in ED use), but public payers and policy makers may consider “direct costs” more holistically, and factor in costs or savings from other public service utilization.
The present review seeks to determine (1) whether or not there is evidence supporting cost savings associated with housing interventions targeting health and (2) with what aspects of the broader healthcare system are those savings associated. The researchers determined that a systematic literature review on ROI for health-focused housing interventions would be a comprehensive method to address such questions.
2 Methods
The objective of this systematic review is to identify evidence regarding the economic benefits of housing interventions aimed at improving health outcomes.
The authors identified articles pertaining to housing, health, and ROI through a literature search that included the following:
-
Computer searches on May 9, 2018, of ProQuest, Academic Search Complete, and PubMed for studies published from 2000 to the present, using the following keywords: “housing” and “health” and “return on investment” with search terms linked by “and” to capture studies that included at least one search term from each phrase.
-
Discussion with identified key experts in the field who offered knowledge and unique perspectives about housing and healthcare. They suggested key terms for the literature search and coding and referred the authors to publications for consideration.
-
Studies that were included in the bibliographies of articles found the online search or expert consultation.
Articles were included if they met all of the following criteria:
-
1.
Described examples of programs with identified health-specific outcomes achieved through a housing related intervention.
-
2.
Were peer-reviewed articles in scholarly journals.
-
3.
Were published between 2000 and 2018.
-
4.
Included an ROI analysis.
-
5.
Were written in English.
Commentary articles meeting the aforementioned criteria that neither contained a specific study nor ROI analysis were excluded but noted and reviewed as relevant topic background. While the search was not constrained to the United States, the nature of the keywords and topic likely drove the focus of the resulting paper, and the resulted obtained were focused almost exclusively in the U.S. One non-U.S. based article which fit inclusion criteria featured a program and analysis conducted in Ontario, Canada (Choi et al. 2016) that was heavily connected to and influenced by U.S. research regarding housing and HIV prevention.
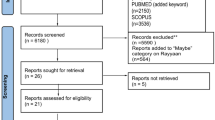
As shown in Fig. 1, 850 abstracts were retrieved, and thirty-two full text articles reviewed for inclusion. Scanning bibliographies revealed one additional relevant article included in the review (Basu et al. 2012). Articles that were included as part of the full-text review but excluded (23 of 32 articles) were initially considered because of potential relevance indicated in their abstracts but ultimately failed to meet the first or fourth review criteria that they must include a description or study of a housing intervention to improve health and an ROI analysis. Additional recent peer-reviewed and gray literature for background and context derived from colleague and expert consultation was also used to help contextualize the paper with broader themes of housing, healthcare, and ROI analysis. These articles are cited and included in the paper’s references (Table 1).
2.1 Coding and analysis
Full-text articles of potentially eligible programs were reviewed based upon the previously described inclusion and exclusion criteria. The authors developed a coding and comparison scheme through multiple meetings and further electronic communication over a 3-week period. The coding approach was developed to record and assess several factors, such as if a study included an ROI analysis and if any demonstrated ROI was positive, what population an intervention targeted, the type of intervention analyzed, whether the program addressed health through housing stability or quality, whether an intervention was conducted to impact at a community or individual level, and the health outcomes that were studied.
Next, articles were divided between the authors, who reviewed and coded their respective articles over a 2-week period. During this time, any questions regarding applying inclusion and exclusion criteria were discussed and resolved. After this initial review, articles were cross-reviewed with significant alignment between reviewers around inclusion and interpretation of findings. Any discrepancies were discussed among all authors until consensus was reached, and rejection of any full text review articles was documented. The resulting output of the literature search drove the analysis and review that follows.
3 Findings
In total, the search identified nine studies looking at eight programs focused on impacting specific health outcomes, conditions, and populations through housing interventions. Eight articles were based on programs and accompanying studies in the United States, predominantly in large urban or metropolitan areas. One article examined a program in Ontario, Canada. While the Canadian healthcare system differs from the U.S. system, the study and intervention included significant overlap with related efforts in the U.S. and provides useful context for researchers, practitioners, and policymakers alike. Five studies looked at ROI in asthma interventions, two on HIV/AIDS, one on homelessness and general chronic disease, and one on urban blight.
The studies varied considerably in terms of design and methodological rigor. This may be in part because of the unique context in which each study was carried out, considering limitations such as monetary resources, population access, and participant attrition. Publication bias presented another limitation. As with other research areas, there is a possibility that studies with positive results and positive ROI’s were more likely to be published. While there is no way to revise this issue, the authors acknowledge that results should be viewed with this potential limitation in mind. Additionally, unless otherwise noted, all results reported across various studies are statistically significant.
The majority of programs reviewed intervened at an individual level (person or household). Two examples approached housing as a social determinant of health from a broader community or population-level lens and included elements such as community education and neighborhood repair or beautification. To be included in this review, any home visit program needed to have a focus on the home itself and mitigating factors related to health outcomes. These may also have included a social service or health assessment component, noted in the respective article descriptions.
Six programs addressed housing quality or environmental factors that could be mitigated within a person’s existing home to improve their health outcomes (e.g. pests, dust, and mold mitigation as commonly identified triggers of asthma symptoms). Two programs focused instead on housing stability, or access, as a driver of improving health outcomes. One program addressed both quality and access through multiple elements.
3.1 Return on investment
Of the nine articles included, eight quantified the program’s economic benefit while one (Takaro et al. 2011) included a theoretical discussion of ROI based on other programming. Five used standard, straightforward methods for calculating ROI: they divided the savings produced by an intervention by its cost. These ROI calculations ranged from 1.32 (32% ROI), to 4.8 (480% ROI). Bielaszka-DuVernay (2011) included an ROI of 4 (400%) based on program administrator self-report. Four articles reported an ROI between 1 and 2.
Two articles drew ROI conclusions using different methods. Basu et al. (2012) reported cost savings produced by a housing program for individuals with chronic illness but not an ROI ratio. Cost savings reported in the study ranged from $6307 for the sample as a whole to $9809 for those who were homeless. Branas et al. (2016) examined the cost savings of housing improvements through urban blight remediation as a method for reducing firearm violence to both taxpayers (through reductions in criminal justice costs) and to society more generally. The authors estimated that the net return to taxpayers was between $5 and $26 for every dollar spent, while the return to society was between $79 and $333 for every dollar spent.
3.2 Specific areas of intervention
3.2.1 Asthma
As the most common chronic health condition in the United States, asthma affects more than 6 million children and is also a common cause of pediatric hospitalizations, with hospitalizations occurring more often in children whose asthma is poorly controlled (Zahran et al. 2018). Asthma management programs that reduce exposure to in-home asthma triggers through home modifications have shown promise in improving asthma symptoms and reducing hospitalizations (Krieger et al. 2005; Morgan et al. 2004). Additionally, structural deficits in homes such as those leading to poor ventilation and dampness can increase the presence of asthma triggers (Fisk et al. 2007; Sharma et al. 2007). For these reasons, an increasing number of housing interventions that seek to reduce asthma triggers have emerged.
Five articles included in this review addressed housing interventions for childhood asthma (Bielaszka-DuVernay 2011; Campbell et al. 2015; Sommer et al. 2011; Takaro et al. 2011; Woods et al. 2012). Home modifications to reduce asthma triggers in these studies included the provision of hypo-allergenic mattress covers, low emissions vacuums, and pest mitigation supplies. Four of the five asthma-focused articles (Bielaszka-DuVernay 2011; Campbell et al. 2015; Sommer et al. 2011; Woods et al. 2012) included home visit programs in which community health workers (CHWs) assisted families with their children’s asthma management. Asthma management interventions included asthma education, support, and service coordination, in addition to mitigation of commonly identified home asthma triggers. All four articles showed a positive ROI. Of those four articles, two (Woods et al. 2012; Sommer et al. 2011), evaluated the same Boston-based community asthma initiative with a calculated ROI of 1.46. Campbell et al. (2015) calculated an ROI of 1.9, while Bielaszka-DuVernay (2011) summarized findings from an asthma program in Cambridge, MA that estimated an ROI of $4 for every $1 spent between 2002 and 2009.
The fifth article (Takaro et al. 2011) evaluated the effects of asthma-friendly home construction compared to the CHW-based program described by Campbell et al. (2015) and conducted a limited ROI analysis. Both interventions took place in Seattle, WA. Takaro et al. (2011) found that asthma-friendly homes were as, if not more, effective at improving asthma symptoms and reducing hospitalizations as the home-visit program. The authors estimated that the cost of adding asthma mitigation features to new home construction ranged from $5000 to $7000 on top of the cost of the home.
The four articles that demonstrated positive ROI attributed the bulk of observed cost savings to meaningful reductions in ED visits and hospitalizations among children with asthma. Woods et al. (2012) found that the percent of participants reporting ED visit declined from 68.5 to 22.9% over 6 months while hospitalizations declined from 51.1 to 10.4%. Takaro et al. (2011) found that asthma-friendly homes reduced the proportion of participants with an asthma-related clinic visit in the last 3 months from 62 to 21% and Bielaszka-DuVernay (2011) reported that over 7 years, the Childhood Asthma Program in Cambridge, MA reduced asthma-related ED visits by 50% and hospitalizations by 45% across the local healthcare system.
3.2.2 HIV
HIV was the second most robust area of research identified. HIV is an expensive diagnosis in the U.S., with an estimated cost per case averaging between $253,000 and $402,000 (Buchanan et al. 2009; Farmham et al. 2013). Unstably housed or homeless individuals are more likely to face barriers with healthcare access, continuity of care and medication adherence, and are up to nine times more likely to have HIV than the stably housed (Wolitski et al. 2007). Additionally, individuals with HIV/AIDS have an 80% higher mortality rate when unstably housed or homeless (Kidder et al. 2008). As HIV is a condition that requires constant monitoring and care, and as housing has been established as an intervening variable, it follows that providing or improving existing housing for unstably housed individuals should have positive effects on health and reduce ED visits, hospitalizations, and hospital days. Past initiatives providing stable housing for individuals with HIV have found that participants report improved physical and mental health and reduced risky behaviors (Holtgrave et al. 2013).
Two articles included in the review examined housing initiatives targeting individuals with HIV (Choi et al. 2016; Dodd et al. 2018), and one additional study mentioned HIV positive individuals in a sub-analysis (Basu et al. 2012). All studies reported a clear positive return on investment. Choi et al. (2016) found and ROI of 4.8 while Dodd et al. (2018) found and ROI of 1.32. One study also focused on a stand-alone housing intervention (Dodd et al. 2018) while the other (Choi et al. 2016) examined major non-biomedical interventions for HIV across the province of Ontario, Canada, and included providing stable housing as one of these. This study did not provide a separate ROI calculation for housing interventions, but created an overall estimate by multiplying the number of HIV infections averted by the lifetime treatment costs, and included only direct savings as opposed to the broader health and social benefits of averted infections.
In addition to the direct cost savings generated for the individual with HIV, another outcome was the estimated aversion of HIV transmissions to uninfected persons. This is in alignment with the ‘Housing First’ model, which believes that the provision of stable housing can be an important first step in helping homeless or unstably housed individuals with addiction or chronic illness achieve better outcomes (Tsemberis et al. 2004). Research has found that housing provision leads to fewer risky behaviors, including exchange and survival sex among those with HIV (Aidala 2005).
3.2.3 Homelessness and chronic disease
In addition to a connection made between homelessness and HIV through housing-related programs and ROI analyses, one included study (Basu et al. 2012) detailed a housing and case management intervention for homeless adults with various chronic medical illnesses. Homelessness is more likely to be experienced by those with health problems and, in turn, exacerbates existing health conditions (Fitzpatrick-Lewis et al. 2011). Participants were recruited from the ED, meaning they had at least one substantial, recent health event and assigned to the intervention arm of the RCT received immediate interim housing, stable longer-term housing and ongoing case management. The intervention group generated an average cost savings of $6307 per person per year, and those with HIV generated an even higher cost savings of between $6622 and $9809. However, the authors concluded that because of the underpowered sample size the results were not statistically significant.
3.2.4 Urban blight remediation
The literature also examined housing through the lens of urban blight, as blighted areas often contain vacant buildings and others that are occupied but not adequately maintained. One research team (Branas et al. 2016) discussed the effect of building and lot upkeep programs and violent assault outcomes. One included study examined the impact of urban blight remediation on assault outcomes (Branas et al. 2016). The researchers assessed two programs involving 5112 abandoned buildings and vacant lots in Philadelphia, PA. Following passage of a local ordinance, one program required owners of abandoned buildings to install working doors and windows, and clean the facades. The other program required owners of vacant lots to remove trash, grade the land, and tend to the vegetation, among others. The treatment groups included 676 abandoned buildings and 4436 vacant lots.
Researchers used two quasi-experimental difference-in-differences analyses to assess firearm and non-firearm assault outcomes. The researchers found that both remediation programs significantly reduced firearm violence. The researchers calculated both taxpayer ROI and societal ROI for both programs, and found that the abandoned building program taxpayer and societal ROI was $5 and $79 respectively, and $26 and $333 respectively, for the vacant lot program. This study represents the broadest definition of direct cost savings included in this review. The authors considered the overall savings to taxpayers caused by reductions in firearm violence through reductions in costs to the healthcare and criminal justice systems as well as the broader savings to society caused by reductions in crime and mortality. Arguably, despite the fact that the authors describe the study as an ROI analysis, Branas et al.’s work may be better characterized as a cost-benefit analysis (FGDC 2009).
4 Limitations and gaps
This literature synthesis and interpretation includes limitations around search terms and parameters, publication bias, and generalizability. For example, three databases were searched using mirror search terms. As a result, it is possible that potentially relevant articles were not identified in the search. Additionally, the search was tailored only to capture studies utilizing ROI. There are several considerations to take into account when interpreting these results. The first is that many community health and housing programs are not evaluated or, if they are, are not beholden to rigorous methods or standardized definitions (Lobo et al. 2014). Because of publication bias, where positive results are more likely to be published (Joober et al. 2012), it is possible that programs which had less successful outcomes exist but are not captured in the literature. Additionally, reflective of the nature of the literature, it is vital to consider that the findings regarding ROI are somewhat uneven. For instance, the amount of detail provided by authors regarding their methodology varied across studies. Finally, although some of the studies described in this review used randomized controlled trials, most were either quasi-experimental or reliant on convenience samples. This limits the generalizability of the outcomes and whether or not the findings would hold true under different contexts.
5 Implications and discussion
Of the nine articles reviewed, all showed a positive ROI or speculated that a positive ROI was likely. While it is difficult to draw firm conclusions based on the number of articles that ultimately met criteria for full text review, the overall trend suggests that housing interventions targeting health outcomes can have robust, positive ROI. The lowest reported ROI was over 30% while the highest was 480%.
The most common intervention types identified were those addressing housing quality for children with asthma and housing stability for homeless and unstably housed persons with HIV or other chronic illnesses. Intervention details varied, but generally, the interventions reviewed included a housing component aimed at providing housing or improving existing housing in combination with case management. The highest ROI observed (Choi et al. 2016) was the product of a suite of HIV interventions occurring in Ontario, Canada, of which housing was only one component. This suggests that while housing interventions may be effective at improving health outcomes, they often do not occur in isolation. It is also important to note that the housing interventions reviewed produced cost savings through a variety of methods and for a variety of stakeholders including healthcare payers, individual participants, and in the case of (Branas et al. 2016) taxpayers, and society.
Somewhat surprisingly, this review did not find any ROI evaluations of housing programs aimed at fall prevention, mental illness, or other chronic health conditions such as diabetes. It is possible that the scope of our systematic review was too narrow to capture the full array of health outcomes targeted by housing programs, but it is also possible that our findings reflect a gap in the current peer reviewed literature. Indeed, as noted previously, healthcare interventions are often not evaluated rigorously or even at all (Lobo et al. 2014). It may be that housing interventions for asthma and HIV are simply more straightforward to evaluate than housing interventions aimed at other conditions. As healthcare payers and providers increasingly recognize housing as an important social determinant of health, future studies may address a broader array of health conditions. Finally, although this review focused on ROI analyses, future research and future reviews could consider a broader array of economic evaluation methods. As Fenwick et al. (2013) note, it would be helpful if future housing intervention studies plan for and include economic impact evaluations in their initial study design.
6 Additional considerations
One important consideration when evaluating the effectiveness of housing interventions is the impact of place. As most of the articles included in this review note, the effects of the interventions described may not be generalizable to all locations or populations. Sommer et al. (2011) highlight the fact that the Community Asthma Initiative organized by Children’s Hospital Boston emerged in response to the very high asthma rates among children in the city and required substantial cooperation and collaboration from clinical partners, government agencies, and community stakeholders. Similarly, the Breathe-Easy Home program described by Takaro et al. (2011) required the support of the Seattle Housing Authority and the U.S. Department of Housing and Urban Development. It is likely that the successes demonstrated by the programs profiled in this review are closely tied to not only the design of the programs themselves, but the needs of population they targeted, and place-based networks of funding, support, and collaboration. Finally, the impact of housing programs often depends on the needs and situations of individual participants with those with the most need benefiting the most (Thomson et al. 2009). As such, housing programs may demonstrate more or less impact in different populations.
7 Conclusion
Housing interventions aimed at childhood asthma, HIV, chronic illness among the homeless, and urban blight have demonstrated positive ROI with return estimates ranging between 1.32 to 4.8 and a plurality of estimates falling between 1 and 2. However, to date only nine peer reviewed articles assessing the ROI of housing intervention aimed at improving health outcomes were identified. The evaluations featured in those articles varied in terms of study design and methodological rigor, but the majority of cost savings observed were attributed to meaningful reductions in hospitalizations and ED visits. As these types of housing-based interventions continue to be implemented, future evaluations and analysis will shed additional light on their economic sustainability and impact.
References
Aidala, A. (2005). Homelessness, housing instability and housing problems among persons living with HIV/AIDS. First National Housing and HIV/AIDS Research Summit, Emory University, Atlanta, GA.
Basu, A., Kee, R., Buchanan, D., & Sadowski, L. S. (2012). Comparative cost analysis of housing and case management program for chronically ill homeless adults compared to usual care. Health Services Research, 47(1pt2), 523–543.
Berwick, D. M., Nolan, T. W., & Whittington, J. (2008). The triple aim: Care, health, and cost. Health Affairs, 27(3), 759–769.
Bharel, M., Lin, W. C., Zhang, J., O’Connell, E., Taube, R., & Clark, R. E. (2013). Health care utilization patterns of homeless individuals in Boston: Preparing for Medicaid expansion under the Affordable Care Act. American Journal of Public Health, 103(S2), S311–S317.
Bielaszka-DuVernay, C. (2011). Taking public health approaches to care in Massachusetts. Health Affairs, 30(3), 435–438.
Birch, S., & Gafni, A. (1992). Cost effectiveness/utility analyses: Do current decision rules lead us to where we want to be? Journal of Health Economics, 11(3), 279–296.
Branas, C. C., Kondo, M. C., Murphy, S. M., South, E. C., Polsky, D., & MacDonald, J. M. (2016). Urban blight remediation as a cost-beneficial solution to firearm violence. American Journal of Public Health, 106(12), 2158–2164.
Braubach, M., & World Health Organization. (2011). Environmental burden of disease associated with inadequate housing: A method guide to the quantification of health effects of selected housing risks in the WHO European Region.
Buchanan, D., Kee, R., Sadowski, L. S., & Garcia, D. (2009). The health impact of supportive housing for HIV-positive homeless patients: A randomized controlled trial. American Journal of Public Health, 99(S3), S675–S680.
Campbell, J. D., Brooks, M., Hosokawa, P., Robinson, J., Song, L., & Krieger, J. (2015). Community health worker home visits for Medicaid-enrolled children with asthma: Effects on asthma outcomes and costs. American Journal of Public Health, 105(11), 2366–2372.
Choi, S. K., Holtgrave, D. R., Bacon, J., Kennedy, R., Lush, J., McGee, F., et al. (2016). Economic evaluation of community-based HIV prevention programs in Ontario: Evidence of effectiveness in reducing HIV infections and health care costs. AIDS and Behavior, 20(6), 1143–1156.
Collinson, R., Gould Ellen, I., & Ludwig, J. (2015). Low income housing policy. Economics of means-tested transfer programs in the United States (Vol. 2). Chicago: University of Chicago Press.
Committee on Environmental Health. (2005). Lead exposure in children: Prevention, detection, and management. Pediatrics, 116(4), 1036–1046.
Dieleman, J., Campbell, M., Chapin, A., Eldrenkamp, E., Fan, V. Y., Haakenstad, A., et al. (2017). Evolution and patterns of global health financing 1995–2014: Development assistance for health, and government, prepaid private, and out-of-pocket health spending in 184 countries. The Lancet, 389(10083), 1981–2004.
Dodd, S. J., Ruffins, J., & Arzola, D. (2018). Improving health while saving money: Lessons learned from a supportive housing program for young adults with HIV. Sexuality Research and Social Policy, 15(2), 163–171.
Evans, G. W. (2006). Child development and the physical environment. Annual Review of Psychology, 57, 423–451.
Farnham, P. G., Gopalappa, C., Sansom, S. L., Hutchinson, A. B., Brooks, J. T., Weidle, P. J., et al. (2013). Updates of lifetime costs of care and quality-of-life estimates for HIV-infected persons in the United States: Late versus early diagnosis and entry into care. JAIDS Journal of Acquired Immune Deficiency Syndromes, 64(2), 183–189.
Federal Geographic Data Committee. (2009). Economic justification: Measuring return on investment (ROI) and cost-benefit analysis (CBA). New Strategic and Business Plan Guidelines. Retrieved from: https://www.fgdc.gov/initiatives/50states/newspbp/EconomicJustification_ROI-CBA-Tutorial_v2_052809_FinalVersa.pdf.
Fenwick, E., Macdonald, C., & Thomson, H. (2013). Economic analysis of the health impacts of housing improvement studies: A systematic review. Journal of Epidemiology and Community Health, 67(10), 835–845.
Fisk, W. J., Lei-Gomez, Q., & Mendell, M. J. (2007). Meta-analyses of the associations of respiratory health effects with dampness and mold in homes. Indoor Air, 17(4), 284–296.
Fitzpatrick-Lewis, D., Ganann, R., Krishnaratne, S., Ciliska, D., Kouyoumdjian, F., & Hwang, S. W. (2011). Effectiveness of interventions to improve the health and housing status of homeless people: A rapid systematic review. BMC Public Health, 11(1), 638.
Gibson, M., Petticrew, M., Bambra, C., Sowden, A., Wright, K., & Whitehead, M. (2010). Housing and health inequalities: A synthesis of systematic reviews of interventions aimed at different pathways linking housing and health. Health & Place, 17(1), 175–184.
Holtgrave, D. R., Wolitski, R. J., Pals, S. L., Aidala, A., Kidder, D. P., Vos, D., et al. (2013). Cost-utility analysis of the housing and health intervention for homeless and unstably housed persons living with HIV. AIDS and Behavior, 17(5), 1626–1631.
Jacobs, D., Brown, M., Baeder, A., Sucosky, M., Margolis, S., Hershovitz, J., et al. (2010). A systematic review of housing interventions and health: Introduction, methods, and summary findings. Journal of Public Health Management & Practice, 16(5), 5–10.
Joober, R., Schmitz, N., Annable, L., & Boksa, P. (2012). Publication bias: What are the challenges and can they be overcome? Journal of Psychiatry and Neuroscience, 37(3), 149.
Kidder, D. P., Wolitski, R. J., Pals, S. L., & Campsmith, M. L. (2008). Housing status and HIV risk behaviors among homeless and housed persons with HIV. Journal of Acquired Immune Deficiency Syndromes, 49(4), 451–455.
Krieger, J. W., Takaro, T. K., Song, L., & Weaver, M. (2005). The Seattle-king county healthy homes project: A randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. American Journal of Public Health, 95(4), 652–659.
Landon, B. E., & Epstein, A. M. (2001). For-profit and not-for-profit health plans participating in medicaid. Health Affairs, 20(3), 162–171.
Lobo, R., Petrich, M., & Burns, S. K. (2014). Supporting health promotion practitioners to undertake evaluation for program development. BMC Public Health, 14(1), 1390–1406.
Bonnefoy X, Annesi-Maesano I, Moreno Aznar L, et al. (2004). Review of evidence on housing and health. In Fourth ministerial conference on environment and health, Budapest: World Health Organization.
Morgan, W. J., Crain, E. F., Gruchalla, R. S., O’Connor, G. T., Kattan, M., Evans, R., III, et al. (2004). Results of a home-based environmental intervention among urban children with asthma. New England Journal of Medicine, 351(11), 1068–1080.
O’Connell, J. J. (2005). Premature mortality in homeless populations: A review of the literature (pp. 2005–2016). Nashville, TN: National Health Care for the Homeless Council.
Office of Disease Prevention and Health Promotion. (2018). Social Determinants of Health. Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health.
Rog, D. J. (2004). The evidence on supported housing. Psychiatric Rehabilitation Journal, 27(4), 334–344. https://doi.org/10.2975/27.2004.334.344.
Sharma, H. P., Hansel, N. N., Matsui, E., Diette, G. B., Eggleston, P., & Breysse, P. (2007). Indoor environmental influences on children’s asthma. Pediatric Clinics, 54(1), 103–120.
Sommer, S. J., Queenin, L. M., Nethersole, S., Greenberg, J., Bhaumik, U., Stillman, L., et al. (2011). Children’s hospital boston community asthma initiative: Partnerships and outcomes advance policy change. Progress in Community Health Partnerships: Research, Education, and Action, 5(3), 327–335.
Takaro, T. K., Krieger, J., Song, L., Sharify, D., & Beaudet, N. (2011). The breathe-easy home: The impact of asthma-friendly home construction on clinical outcomes and trigger exposure. American Journal of Public Health, 101(1), 55–62.
Thomson, H., Petticrew, M., & Morrison, D. (2001). Health effects of housing interventions: A systematic review of intervention studies. British Medical Journal, 28(323), 187–190.
Thomson, H., Thomas, S., Sellstrom, E., & Petticrew, M. (2009). The health impacts of housing improvement: A systematic review of intervention studies from 1887 to 2007. American Journal of Public Health, 99(S3), S681–S692.
Tsemberis, S., Gulcur, L., & Nakae, M. (2004). Housing first, consumer choice, and harm reduction for homeless individuals with a dual diagnosis. American Journal of Public Health, 94(4), 651–656.
Wolitski, R. J., Kidder, D. P., & Fenton, K. A. (2007). HIV, homelessness, and public health: Critical issues and a call for increased action. AIDS and Behavior, 11(2), 167.
Woods, E. R., Bhaumik, U., Sommer, S. J., Ziniel, S. I., Kessler, A. J., Chan, E., et al. (2012). Community asthma initiative: Evaluation of a quality improvement program for comprehensive asthma care. Pediatrics, 129(3), 465–472.
Zahran, H. S., Bailey, C. M., Damon, S. A., Garbe, P. L., & Breysse, P. N. (2018). Vital signs: Asthma in children—United States, 2001–2016. Morbidity and Mortality Weekly Report, 67(5), 149.
Acknowledgements
The authors would especially like to thank Karyn Quinn, Michal Grinstein-Weiss, and Jane Oliphant for their valued contributions to the conceptualization of the project’s focus and methods, and Sam Hsu for support and contributions during the revision process.
Funding
The authors undertook the research and writing of this article with support from the Centene Center for Health Transformation, a partnership between Centene Corporation, Washington University in Saint Louis, and Duke University.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Davison, G., Ferris, D., Pearson, A. et al. Investments with returns: a systematic literature review of health-focused housing interventions. J Hous and the Built Environ 35, 829–845 (2020). https://doi.org/10.1007/s10901-019-09715-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10901-019-09715-6