Abstract
The recent increases in childhood obesity rate among the Hispanics living in the US is a major public health concern. To date, interventions seeking to reduce childhood obesity often target the youth or the parents; however, few engage both groups within the intervention. This systematic review explores current studies that aim to control obesity in Hispanic children through family-centered interventions and assesses the effects and outcomes of these interventions in Hispanic children (2–12 years old). Data bases (PubMed, Cochrane, and EBSCO) were used to search for articles published from 2013 to 2019 that used interventions to prevent or reduce childhood obesity in Hispanic populations. Out of the initial 110 articles, only nine articles met the inclusion criteria and were included in the analysis. The majority of the current interventions included in this systematic analysis were effective in controlling Hispanic childhood obesity. Shorter interventions (i.e. 8–36 weeks) found changes in health behaviors (e.g. sugary drink consumption, screen time) and health outcomes (e.g. health-related quality of life), but many did not see changes in anthropometric variables (e.g. body mass index [BMI], blood pressure). However, interventions measured over longer timeframes (i.e. 48–144 weeks) found some decreases in sustained behaviors (e.g. caloric intake) and anthropometric measures. There is a lack of literature pertaining to culturally relevant, family-centered interventions for Hispanic youth and their families. Future studies should use culturally tailored strategies to develop interventions specifically made for Hispanic youth and education to engage their families within the program.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity rates among Hispanic children living in the US continue to increase, with recent evidence suggesting one in four Hispanic children is obese (i.e., BMI > 30) [1]. As part of the fastest growing ethnic minority groups in the US, Hispanic preschool children have higher rates of obesity (16.7%) than other racial/ethnic populations (11.3% non-Latino black, 3.5% of non-Latino white, and 3.4% of non-Latino Asian) [2]. This epidemic has become a serious public health concern, creating a need for culturally relevant and effective interventions.
Some studies have found social and cultural risk factors for childhood obesity in the Hispanic population to include family members’ perceptions about weight [3, 4]. For instance, Hispanic parents perceive their overweight or obese children to be healthy, and they believe a larger contexture indicates the child is well fed [1, 5, 6]. Allowing digital media use (TV, cell phones, and video games) and providing unhealthy foods as a reward or emotional control has also potentially contributed to childhood obesity, particularly among Hispanic youth [7,8,9,10].
Literature has noted the lack of social and behavioral interventions that seek to reduce obesity among diverse communities (e.g., Hispanic youth) [11]. Many interventions for treating or preventing childhood obesity target either only the obese child or their parents, but not both [12,13,14,15,16,17]. Other programs were created particularly for non-Hispanic youth; thus, they might not be successful in Hispanic children [11, 18,19,20,21]. Family-centered interventions (FCI) recognize families play an important role in influencing children’s behaviors [22]. Adopting healthy behaviors, such as healthy eating, increased physical activity, adequate sleep, and decreasing screen time is crucial to combat childhood obesity and is greatly influenced by family involvement [23]. However, it is currently unknown if FCI created for Hispanic children with obesity improve these children’s health outcomes. The purpose of this systematic review is to identify studies focused on FCI for obesity in Hispanic children and to determine if this approach can effectively improve these children’s health outcomes.
Methods
Study Selection
Eligible studies were published in English between 2013 and 2019, conducted in the US and included overweight and obese Latino children between 2 and 12 years of age. Interventions were described as Latino family-based or FCI that sought to address childhood obesity. Some studies that focused on eating behavior and weight gain included children with normal weight. These studies were included within the search due to their focus on behaviors known to attribute to increased weight gain [24, 25].
Search Strategy
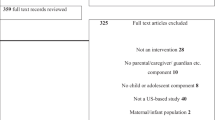
The systematic search employed the following databases: PubMed, Cochrane, and EBSCO. Peer-reviewed papers were identified using the terms: family-based intervention; parent-based intervention; caregiver intervention; prevention; treatment; obesity child; obesity infant; obesity childhood; Hispanic OR Latino; Latina; Latin; Mexican. Overall, 110 studies were identified in the initial search. After removing duplicate articles (26) and reviewing abstracts for eligibility criteria, 84 additional articles were removed. Finally, two coders reviewed the full text of 39 studies (one study was identified from the reference list of another article), and nine studies met the criteria and were included in the final analysis. A flow diagram of the search and selection process is presented in Fig. 1.
Studies Description
Of the nine articles reviewed, six were randomized controlled trials (RCT) [5, 26,27,28,29,30], two were non-experimental pretest–posttest design [31, 32], and one was a quasi-experimental intervention [33]. All studies were conducted in the US and utilized FCI. All interventions were designed to promote positive behavioral changes in obese children of Hispanic families. A detailed description of all nine studies is presented in Table 1.
Four of the studies did not use a control intervention. The studies testing the Vida Saludable (Healthy Life) program [31] and the Niños Activos y Sanos (Healthy and Active Children, HAC) program [32] utilized a non-experimental design and did not have a control group. The other two studies, Familias Activas y Saludables (Active and Healthy Families, AHF) [28] and a two component program (Power up and culturally sensitive coaching based on the American Association of Pediatrics (AAP) guidelines for treatment and prevention of childhood obesity) [26], used a waitlisted sample as a control group.
Out of the five remaining, the Nutrition and Exercise Start Today (NEST) study compared a standard care intervention adhering to the AAP guidelines with (experimental) or without (control) the inclusion of additional behavioral components [29]. Foster, Aquino, Gil, Gelfond and Hale [5] utilized participants from Head Start, a government funded program for low income families focusing on school readiness and health. The authors compared the delivery of an intervention based on the EatPlayGrow curriculum by parent mentors (peer parents of healthy weight children) or by community health workers (control intervention) who provided healthy meals and circulating newsletters containing information about healthy behaviors [5].
In three long-term (over one year) obesity prevention studies, the GROW Healthier intervention, a three-year, three phase program that focused on behavior change, was compared to the GROW Smarter program, a standard school readiness program [27], the three-year Niños Sanos, Familia Sana (Healthy Children, Healthy Family, HCHF) program utilized two rural communities to compare a community-based multifaceted intervention based on the AAP guidelines in the experimental community to a non-nutrition community-based program in the control community [33],and the Familias Saludables Activas (Healthy Families’ Active, HFA) intervention was compared to an oral health control intervention [30]. Part of the oral health intervention encouraged participants to avoid sugar as a cause of cavities, not for nutritional reasons. The one year active intervention included a four-month intensive educational intervention (eight classes) and an eight-month reinforcement phase (monthly mail/telephone contact) [30].
Study Population Description
Subjects characteristics of all nine studies are summarized in Table 2. The population targeted in these studies were parent–child dyads from Hispanic families. The age of children participants ranged between 2–12 years [5, 26,27,28,29, 33] With the exception of the GROW Healthier [27], HFA [30], and the HCHF [33] studies, that aimed at obesity prevention, at least 70% of the sample populations included either overweight or obese children [5, 26, 28, 29].
Intervention Description
All nine studies sought to reduce or prevent Latino childhood obesity and focused on nutritional changes (e.g., increase fruit/vegetable intake, reduce sweetened beverages, increase healthy snacks availability, provide cooking class, demonstrate shopping skills) [5, 26,27,28,29,30,31,32,33], increased physical activity [5, 26,27,28,29,30,31,32,33], increased sleep time [5, 27], and/or decreased screen time [5, 27,28,29,30, 32] to both the child and their family members. The in-person counseling sessions described in all nine studies ranged from 4–22 sessions, and only six studies included coaching telephone calls in addition to in-person counseling [5, 26,27,28,29,30].
Four of the intervention programs provided objects such as pedometers, water pitchers, physical activity items (basketballs), cereal bowls, kitchen tools, or food preparation equipment as incentives to keep participants motivated with the intervention [26, 28, 30, 32]. Falbe et al. [28] and Hull et al. [30], were some of the few interventions that offered tangible resources in the form of a culturally relevant recipe book, while Parra-Medina, Mojica, Liang, Ouyang, Ramos and Gomez [29] provided newsletters and healthy recipes in addition to healthy lifestyle guidelines to promote healthy eating and physical activity (e.g., play outside at least one hour per day).
Results—The Efficacy of Family Centered Interventions
Anthropometric Changes
Several benefits were reported for FCI in the treatment and prevention of childhood obesity in Hispanic families, including reduced BMI and improved health outcomes and dietary behavior (see Table 1). Falbe and colleagues [28] reported the AHF program resulted in significantly lower BMI following the 10-week intervention. Similarly, decreased BMI was also reported following the EatPlayGrow [5] and HCHF [33] interventions. Foster, Aquino, Gil, Gelfond and Hale [5] reported children with higher BMI values showed a larger drop in BMI following the intervention.
Other FCI did not reduce BMI but reported successful weight maintenance in the experimental groups. Vida Saludable, an intervention focused on reducing the consumption of sugar-sweetened beverages, resulted in successful weight maintenance in children, demonstrated by stable BMI throughout the 36-week intervention [31]. Parra-Medina et al. [29] also reported successful weight maintenance in the GROW Healthier participants compared to children in the GROW Smarter program. Although no significant changes were reported in BMI, significant differences were found in body weight and waist circumference, which increased in less children in the experimental program compared to the control group (44% and 68.5% of children in the experimental group vs 68.6% and 89.7% of children in the control group for increased waist circumference and weight gain, respectively) [29]. Although the growth rate of BMI among participants in Hull et al.’s study did not differ between the control and intervention groups, there was a slower increase in BMI among those who were overweight/obese in the intervention group [30]. Only three programs did not successfully decrease BMI compared to baseline levels or to the control group [26, 27, 30]. Falbe, Cadiz, Tantoco, Thompson and Madsen [28] reported improved blood triglycerides, while Arauz Boudreau, Kurowski, Gonzalez, Dimond and Oreskovic [26] found that blood cholesterol levels decreased in the intervention group and increased in the waitlist group following the 24-week intervention. They found no differences in blood markers or blood pressure between children in the AHF program and their waitlisted counterparts [28].
Behavioral Changes
FCIs successfully achieved meaningful changes with improvements in healthy behaviors (physical activity, fruit and vegetable intake, sleep time) and decrease in unhealthy behaviors (screen time, consumption of sugar-sweetened beverages). The Vida Saludable program reduced consumption of soda and sugary drinks and increased water intake; consumption of milk and 100% juice was not significantly reduced [31]. Similarly, the HAC community-based, FCI, led by trained paraprofessional women from within the community, successfully increased intake of fruit/vegetable, low fat dairy products, and fruit availability in obese children of Hispanic families. This program also decreased in the consumption of energy-dense snacks and fast food [32]. Similarly, following a three-year multicomponent behavioral intervention, in contrast to school-readiness sessions group, Barkin et al. [27] reported a significantly lower mean caloric intake in the intervention group. Foster, Aquino, Gil, Gelfond and Hale [5] reported mixed results following the parent-mentor led program. Although subjects in the experimental group successfully reduced weekday screen time, their sleeping behavior did not improve. The HFA intervention significantly increased weekend moderate physical activity and decreased weekend screen time among overweight and obese children [30]. Dietary intake frequencies were not collected due to technical issues [30].
Health Related Quality of Life
Arauz Boudreau, Kurowski, Gonzalez, Dimond and Oreskovic [26] demonstrated obese children from Latino families experienced a poor health-related quality of life, measured by the PedsOL questionnaire. Following the 24-week FCI, PedsQL scores improved; however, this improvement was not statistically significant. The authors attributed the lack of statistical significance to a small sample size and speculated a more intensive intervention including scheduled coaching and/or changes to the environmental context might have been more successful [26]. Foster, Aquino, Gil, Gelfond and Hale [5] showed no significant changes in PedsQL scores in either the intervention or control group throughout the interventions. However, after six months the emotional functioning score, which was associated with greater changes in BMI and a healthier diet, improved significantly in both groups [5].
Risk of Bias
The risk for the following biases was identified within the studies analyzed in this review. Two studies were nonrandomized [31, 32] and five studies utilized small sample sizes [5, 26, 28, 31, 32]. Reporting bias was present in studies that involved parental self-reporting [5, 26, 27, 30, 32]. Six studies targeted a homogeneous sample of low income Hispanic families, limiting the generalization to other populations [26,27,28,29, 31, 33]. Three studies reported missing data which could have affected some of their outcome measures, such as clinical blood tests [26, 28, 29].
Discussion
The purpose of this systematic review was to collect and analyze studies that utilized FCIs to prevent/reduce obesity in Hispanic children in order to present useful strategies that can be effectively implemented within this population. The prevalence of obesity in Hispanic children under 18 years has dramatically increased in recent years and is posing a significant public health burden [34]. Family participation, particularly among parents, is an essential component in intervention programs targeting childhood obesity, especially in early life because children are more likely to adhere to new healthy behaviors [35]. Interestingly, very few articles focused on FCIs to combat childhood obesity in Hispanic families and almost none compared FCIs to interventions targeting only the child or the parent. One study compared child-only to parent-only intervention and found parent involvement to be crucial for successful weight loss, but this study did not include Hispanic subjects and was not conducted in the US [36].
Childhood obesity among Hispanic populations may be influenced by additional factors such as parents lack of adequate knowledge about healthy child nutrition, living in a food desert area, low-income, increased screen time, and/or sleep deprivation [37, 38]. Thus, FCIs (through family education) may be more effective in promoting positive health behaviors and mitigating some barriers and limitations many Hispanic families may encounter. FCIs that employ parental behavioral modeling and provide experiential learning opportunities for children may be able to elicit greater anthropometric changes (e.g. BMI and waist circumference) than interventions that do not engage families within the process [39]. The success of FCI in the Hispanic population is also affected by their unique cultural background. One strategy that may be effective among Hispanic children and parents is the utilization of culturally familiar objects and concepts. For example, a culturally relevant recipe book that shows foods and beverages that are frequently consumed by Hispanic families (e.g. tacos, tortillas, conchas, and empanadas) [40].
Additionally, more than 50% of parents from six studies had not completed high school [26,27,28, 30, 31, 33], which may have been a barrier to improve their kids’ healthy weight. Five trials had more than 50% of families living below the poverty line [5, 27, 29, 32, 33], a factor linked to childhood obesity. One study noted the relation between poverty and obesity among 111,799 children students (68 public schools) in Massachusetts, where the highest rates of obesity were among Hispanic and African American. This study concluded low income had a greater and significant association with weight status than with ethnicity/race [41].
The two longest interventions (144 weeks) both prevented obesity in Hispanic children [27, 33]. The study with the shortest duration (eight weeks) focused on physical activity and diet changes. While significant changes were found in the consumption of fruit/vegetables, low fat dairy products, energy dense snacks and fast food and in physical activity, children’s BMI did not change [32]. These findings might suggest longer interventions may not be necessary to improve short-term outcomes but are essential to achieve long-term weight maintenance. However, Ottebach et al. [32] did not track the assimilation of these behavioral changes after the termination of the program and new behaviors transform into habits after a minimum of six months; [42] thus, more research is needed to support this statement. Some studies showed behavioral changes, such as decreasing sedentary behaviors and increasing physical activity levels, were associated with a better health-related quality of life [43].
This systematic review was subject to limitations. First, the analyzed articles were published over a short time-period (2013–2019). A larger time range may have yielded more studies that would have met the inclusion criteria. Second, the total number of participants from all studies was 2373 Hispanic parent–child pairs, mostly from Tennessee (n = 1201) [27, 30], California (n = 868) [28, 31, 33], and Texas (n = 178) [5, 29]. The Hispanic population in the US is estimated at 59.9 million people, living in all 50 states [44]. More research is needed to evaluate the efficacy of FCIs for the treatment and prevention of childhood obesity in Hispanic families in other states where there is a growing Hispanic population such as New Mexico, Arizona, and Nevada.
To date, current interventions have helped to reduce childhood obesity among Hispanic youth; however, limitations remain. Barriers faced by parents over the 24-week intervention in Arauz-Boudreau et al.’s [26] study included: lack of knowledge about healthy eating behaviors, physical activity limitation (higher cost, unsafe places, and limited time) and lack of access to transportation. New methods could reduce the presence of barriers. Such programs could be implemented at different locations where this ethnic group congregates (e.g., churches, parks, schools), and the use of parent-mentor facilitators from within the community could make families feel more supported, understood, and motivated due to their shared culture and experiences. Home-based interventions could be effective for those that do not have transportation (rural areas), as well as mobile counseling, mobile apps and text messages do not require internet most of the time. Such counseling could seek to reduce stress, a factor linked to higher consumptions of fast food among 2–17 year olds [45]. AHF was the only intervention program in this review that offered sessions focused on relief of stress specifically caused by immigration [28]. Future studies may focus on the relation between Hispanic family’s stress caused by immigration and childhood obesity risk. Finally, participation of school institutions is an essential support network to consider for future interventions, due to the amount of time a child spends in school. In Arauz-Boudreau et al.’s [26] intervention, parents mentioned not having control of school meals, and 82.4% kids informed having a negative perception of school lunches.
Conclusion
The studies examined in this review included FCIs demonstrated promising results in improving health and behavioral measures related to obesity. Utilizing and including local people (Latino parent mentors), community institutions (schools), tangible resources (recipes, guidelines), and multidisciplinary teams (psychologists, physical activity coaches, nurses, behavioral counselors, dieticians, and/or Spanish interpreters) were essential components that empowered Hispanic families to adopt healthy lifestyles. Future research should employ qualitative methodology to identify needs of this population not currently measured with close-ended measures or questionnaires. Such method could help to better understand and respect the cultural practices that influence dietary choices, physical activity, and other behaviors related to childhood obesity. By exploring theses perceptions, comments, and recommendations from parents, future interventions could culturally tailor content to be more accepted and utilized among Hispanic families.
References
Hales, C. M., Carroll, M. D., Fryar, C. D., et al. (2017). Prevalence of obesity among adults and youth: United States, 2015–2016. NCHS Data Briefs, 288, 1–8.
Ogden, C. L., Carroll, M. D., Fryar, C. D., et al. (2015). Prevalence of Obesity Among Adults and Youth: United States, 2011–2014. NCHS Data Briefs, 219, 1–8.
Chaparro, M. P., Langellier, B. A., Kim, L. P., et al. (2011). Predictors of accurate maternal perception of their preschool child's weight status among hispanic WIC participants. Obesity, 19(10), 2026–2030.
Taveras, E. M., Gortmaker, S. L., Mitchell, K. F., et al. (2008). Parental perceptions of overweight counseling in primary care: the roles of race/ethnicity and parent overweight. Obesity, 16(8), 1794–1801.
Foster, B. A., Aquino, C. A., Gil, M., et al. (2016). a pilot study of parent mentors for early childhood obesity. Journal of Obesity, 2016, 2609504.
Guerrero, A. D., Slusser, W. M., Barreto, P. M., et al. (2011). Latina mothers' perceptions of healthcare professional weight assessments of preschool-aged children. Maternal and Child Health Journal, 15(8), 1308–1315.
Hackie, M., & Bowles, C. L. (2007). Maternal perception of their overweight children. Public Health Nursing, 24(6), 538–546.
Lindsay, A. C., Sussner, K. M., Greaney, M. L., et al. (2011). Latina mothers' beliefs and practices related to weight status, feeding, and the development of child overweight. Public Health Nursing, 28(2), 107–118.
Powell, E. M., Frankel, L. A., & Hernandez, D. C. (2017). The mediating role of child self-regulation of eating in the relationship between parental use of food as a reward and child emotional overeating. Appetite, 113, 78–83.
Blissett, J., Haycraft, E., & Farrow, C. (2010). Inducing preschool children's emotional eating: relations with parental feeding practices. American Journal of Clinical Nutrition, 92(2), 359–365.
Ash, T., Agaronov, A., Young, T., et al. (2017). Family-based childhood obesity prevention interventions: a systematic review and quantitative content analysis. International Journal of Behavioral Nutrition and Physical Activity, 14(1), 113.
Berge, J. M. (2009). A review of familial correlates of child and adolescent obesity: what has the 21st century taught us so far? International Journal of Adolescent Medicine and Health, 21(4), 457–483.
Golan, M., & Weizman, A. (2001). Familial approach to the treatment of childhood obesity: conceptual mode. Journal of Nutrition Education, 33(2), 102–107.
Golan, M., Kaufman, V., & Shahar, D. R. (2006). Childhood obesity treatment: targeting parents exclusively v. parents and children. British Journal of Nutrition, 95(5), 1008–1015.
Kitzman-Ulrich, H., Wilson, D. K., George, S. M. S., et al. (2010). The integration of a family systems approach for understanding youth obesity, physical activity, and dietary programs. Clinical Child and Family Psychology Review, 13(3), 231–253.
Ling, J., Robbins, L. B., & Hines-Martin, V. (2016). Perceived parental barriers to and strategies for supporting physical activity and healthy eating among head start children. Journal of Community Health, 41(3), 593–602.
Nelson, S. A., Corbin, M. A., & Nickols-Richardson, S. M. (2013). A call for culinary skills education in childhood obesity-prevention interventions: current status and peer influences. Journal of the Academy of Nutrition and Dietetics, 113(8), 1031–1036.
Isasi, C. R., Rastogi, D., & Molina, K. (2016). Health issues in Hispanic/Latino youth. Journal of Latina/o Psychology, 4(2), 67–82.
Berge, J. M., & Everts, J. C. (2011). Family-based interventions targeting childhood obesity: a meta-analysis. Childhood Obesity, 7(2), 110–121.
Seo, D.-C., & Sa, J. (2010). A meta-analysis of obesity interventions among US minority children. Journal of Adolescent Health, 46(4), 309–323.
Tovar, A., Renzaho, A. M., Guerrero, A. D., et al. (2014). A systematic review of obesity prevention intervention studies among immigrant populations in the US. Current Obesity Reports, 3(2), 206–222.
Gentile N, Kaufman T, Maxson J, et al. (2018). The effectiveness of a family-centered childhood obesity intervention at the YMCA: A pilot study. Journal of Community Medicine and Health Education, 8, 591. https://doi.org/10.4172/2161-0711.1000591.
Savage, J. S., Fisher, J. O., & Birch, L. L. (2007). Parental influence on eating behavior: conception to adolescence. Journal of Law, Medicine and Ethics, 35(1), 22–34.
Birch, L., Savage, J. S., & Ventura, A. (2007). Influences on the development of children's eating behaviours: from infancy to adolescence. Canadian Journal of Dietetic Practice and Research, 68(1), s1–s56.
Nestle, M. (2000). Soft drink "pouring rights": marketing empty calories to children. Public Health Reports, 115(4), 308–319.
Arauz Boudreau, A. D., Kurowski, D. S., Gonzalez, W. I., et al. (2013). Latino families, primary care, and childhood obesity: a randomized controlled trial. American Journal of Preventive Medicine, 44(3 Suppl 3), S247–257.
Barkin, S. L., Heerman, W. J., Sommer, E. C., et al. (2018). Effect of a behavioral intervention for underserved preschool-age children on change in body mass index: a randomized clinical trial. JAMA, 320(5), 450–460.
Falbe, J., Cadiz, A. A., Tantoco, N. K., et al. (2015). Active and healthy families: a randomized controlled trial of a culturally tailored obesity intervention for latino children. Academic Pediatrics, 15(4), 386–395.
Parra-Medina, D., Mojica, C., Liang, Y., et al. (2015). Promoting weight maintenance among overweight and obese Hispanic children in a rural practice. Childhood Obesity, 11(4), 355–363.
Hull, P. C., Buchowski, M., Canedo, J. R., et al. (2018). Childhood obesity prevention cluster randomized trial for Hispanic families: outcomes of the healthy families study. Pediatric Obesity, 13(11), 686–696.
Bender, M. S., Nader, P. R., Kennedy, C., et al. (2013). A culturally appropriate intervention to improve health behaviors in Hispanic mother-child dyads. Childhood Obesity, 9(2), 157–163.
Otterbach, L., Mena, N. Z., Greene, G., et al. (2018). Community-based childhood obesity prevention intervention for parents improves health behaviors and food parenting practices among Hispanic, low-income parents. BMC Obesity, 5, 11.
Sadeghi, B., Kaiser, L. L., Hanbury, M. M., et al. (2019). A three-year multifaceted intervention to prevent obesity in children of Mexican-heritage. BMC Public Health, 19(1), 582.
Hruby, A., & Hu, F. B. (2015). The Epidemiology of Obesity: A Big Picture. PharmacoEconomics., 33(7), 673–689.
Gray, L. A., Hernandez Alava, M., Kelly, M. P., et al. (2018). Family lifestyle dynamics and childhood obesity: evidence from the millennium cohort study. BMC Public Health, 18(1), 500.
Golan, M., Fainaru, M., & Weizman, A. (1998). Role of behaviour modification in the treatment of childhood obesity with the parents as the exclusive agents of change. International Journal of Obesity and Related Metabolic Disorders, 22(12), 1217–1224.
Commission, K. (2013). Health coverage for the Hispanic population today and under the affordable care act. Menlo Park: The Kaiser Family Foundation.
Juckett, G. (2013). Caring for Latino patients. American Family Physician, 87(1), 48–54.
Zoorob, R., Buchowski, M. S., Beech, B. M., et al. (2013). Healthy families study: design of a childhood obesity prevention trial for Hispanic families. Contemporary Clinical Trials, 35(2), 108–121.
Li, R., Raber, M., Mejia, L., et al. (2015). Development and feasibility of a culturally sensitive cooking and physical activity program designed for obese Hispanic families. ICAN, 7(2), 86–93.
Rogers, R., Eagle, T. F., Sheetz, A., et al. (2015). The relationship between childhood obesity, low socioeconomic status, and race/ethnicity: lessons from Massachusetts. Childhood Obesity, 11(6), 691–695.
Stonerock, G. L., & Blumenthal, J. A. (2017). Role of counseling to promote adherence in healthy lifestyle medicine: strategies to improve exercise adherence and enhance physical activity. Progress in Cardiovascular Diseases, 59(5), 455–462.
Yackobovitch-Gavan, M., Nagelberg, N., Phillip, M., et al. (2009). The influence of diet and/or exercise and parental compliance on health-related quality of life in obese children. Nutrition Research, 29(6), 397–404.
U.S. Census Bureau PD. Estimates of the components of resident population change: April 1, 2010 to July 1, 2018 Available: https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=PEP_2018_PEPTCOMP&prodType=table.
Parks, E. P., Kumanyika, S., Moore, R. H., et al. (2012). Influence of stress in parents on child obesity and related behaviors. Pediatrics, 130(5), e1096–e1104.
Funding
This study was not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tamayo, M.C., Dobbs, P.D. & Pincu, Y. Family-Centered Interventions for Treatment and Prevention of Childhood Obesity in Hispanic Families: A Systematic Review. J Community Health 46, 635–643 (2021). https://doi.org/10.1007/s10900-020-00897-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-020-00897-7