Abstract
Colorectal cancer (CRC) remains a leading cause of morbidity and mortality in the U.S. Disparities in access to care contribute to advanced CRC stage at diagnosis, and these disparities are most pronounced among underserved populations and ethnic minorities. We aim to evaluate race/ethnicity-specific disparities in CRC stage at diagnosis among an ethnically diverse, urban safety-net hospital. We retrospectively evaluated all adult CRC patients diagnosed from January 1, 2009 to October 1, 2015. CRC cases were confirmed by histopathology specimens from biopsies and/or surgical resection. CRC staging utilized American Joint Committee on Cancer (AJCC) staging systems and were stratified by race/ethnicity. Multivariate logistic regression models were utilized to evaluate disparities in AJCC stage at presentation (stage 3–4 vs. stage 0–2). Among 311 patients with CRC [51.5% male, 25.3% black, 18.7% Hispanic, 32.0% Asian, and mean age at diagnosis 58.1 years (SD 10.3)] 61.4% had advanced ACC stage 3–4 CRC at diagnosis. Among black patients with CRC, 73.3% had AJCC stage 3–4 cancer at time of diagnosis. On multivariate regression, blacks were nearly four times more likely to have advanced AJCC stage 3–4 CRC at diagnosis compared to whites (OR 3.70; 95% CI 0.97–14.11; p = 0.055). Among a diverse underserved population, over 60% of CRC were AJCC stage 3–4 at diagnosis, and nearly 75% of blacks with CRC had AJCC stage 3–4 at diagnosis. Advanced stage CRC at diagnosis limits options for potentially curative therapies, and increases the risk for cancer recurrence and mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is one of the most common and deadly cancers in the world. In the United States, CRC accounts for 8% of all new cancer cases and nearly 9% of all cancer-related deaths [1, 2]. While the overall 5-year survival among patients with CRC is 64.5%, patients with earlier staged disease at presentation have significantly better survival compared to those diagnosed with more advanced disease [1–4]. Early detection through effective CRC screening and surveillance programs improves opportunities for potentially curative treatment options [5–7].
The implementation of effective CRC screening initiatives has led to significant improvements in CRC outcomes in recent decades [5–7]. In 1975, the overall 5-year relative survival rate for CRC was 49% compared to 66.5% in 2007 [2]. A similar improvement can be observed for CRC incidence. The incidence rate was 59.5 (per 100,000 persons) in 1975 versus 38.5 (per 100,000 persons) in 2012, reflecting the impact of reducing CRC incidence via removing adenomatous polyps that have long-term malignant potential [2]. Despite these improvements, CRC remains the third leading cause of cancer-related mortality in the United States among both men and women [1, 2]. While the development of effective screening tools has been vital to improve CRC outcomes, addressing potential barriers in access to CRC screening as well as treatment among those with CRC, especially among underserved populations, will continue to improve overall CRC-related outcomes.
CRC exhibits strong demographic trends for incidence and mortality. Its margin of disparity among race/ethnicity is well documented [8–14]. In the United States, African-Americans suffered from the highest burden of CRC in both incidence and mortality from 2006 to 2010 [1, 2]. In a large study of CRC patients from 1991 to 2005 by Silber et al. white CRC patients had significantly higher survival compared to black patients with CRC even while controlling for age, sex, diagnosis year, and geography [9]. Understanding the causal factors behind these race disparities is complex and requires a large number of diverse studies to identify potential explanations. Furthermore, the race/ethnicity-specific disparities that do exist are hypothesized to be more significant among urban underserved populations given the compounding factors (e.g. system-level barriers, access to care, socioeconomic status) that are typical of safety-net population. Better understanding disparities is the first step to identify potential targets for education and quality improvement initiatives. Thus, the aim of our study is to evaluate race/ethnicity-specific disparities in CRC stage at diagnosis among an ethnically diverse urban safety-net hospital population.
Methods
Study Cohort
We conducted a retrospective cohort study to evaluate all adult (age ≥ 18) CRC patients diagnosed from January 1, 2009 to October 1, 2015 at a large ethnically diverse safety-net hospital system. All cases of CRC were confirmed by histopathology specimens from biopsies and/or surgical resection.
Study Outcomes
The primary outcome of our study was to evaluate CRC stage of disease at presentation using the American Joint Committee on Cancer (AJCC) staging system, stratified by age at diagnosis and race/ethnicity. Major race/ethnicity categories included White, Black, Hispanic, Asian, and Other.
Statistical Analysis
Patient demographics were presented as mean and standard deviation or median and range for continuous variables and proportion and frequencies for categorical variables. Categorical variables were compared using chi-squared methods and Student’s t test or analysis of variance was used to compare continuous variables. Stage of disease at presentation and CRC treatment received were stratified by sex and race/ethnicity. Predictors of advanced CRC stage (AJCC stage 3–4) at time of diagnosed was evaluated with multivariate logistic regression models. Variables included in the model were determined a priori based on clinical significance and those that demonstrated significance in the univariate model with p < 0.10. The multivariate model was adjusted for age, sex, AJCC stage of disease, race/ethnicity, and first-degree family history of CRC. All statistical analyses were performed using the Stata statistical package (version 10, Stata Corp, College Station, TX) with a two-tailed p value <0.05 to determine statistical significance. This study was approved by the Institutional Review Board at Alameda Health System.
Results
There were a total of 311 cases of colorectal cancer confirmed by histopathology specimens from biopsy and/or surgical resection in our study. Table 1 presents the characteristics of the study cohort. 51.5% were male with an average age at diagnosis of 58.1 years (SD = 10.3). 84% were of non-white ethnicities including 32% Asian, 18.7% Hispanic, and 25.3% Black. When divided by anatomic location 249 cases (80.1%) originated from the colon and 62 cases (19.9%) originated from the rectum. Among colon cancers cases, 150 involved the left colon, 10 involved the transverse tumors, and 74 involved the ascending colon. Family history of any cancer was reported in 76 cases (46.1%) and family history of CRC was reported in 26 cases (15.8%) (Table 1).
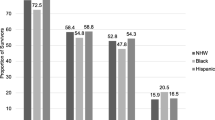
When stratified by stage of disease at diagnosis, nearly 65% of patients were diagnosed with AJCC stage 3–4 at diagnosis, with 22.3% AJCC stage 4 at diagnosis (Fig. 1). Early stage disease (stage 0–1) accounted for 12.7% of patients. We further evaluated CRC stage of disease at presentation stratified by age and race/ethnicity (Fig. 2). Among CRC patients age <50 years 56.8% had AJCC stage 3–4 at diagnosis compared to 65.3% among CRC patients age 50 years and over, p = 0.338 (Fig. 2). When stratified by race/ethnicity, black patients with CRC had the largest proportion of advanced AJCC stage 3–4 CRC at time of diagnosis and Hispanic patients had the lowest proportion of AJCC stage 3–4 CRC at diagnosis. Compared to white patients with CRC, there was a trend toward higher proportion of AJCC stage 3–4 CRC among blacks (73.3 vs. 58.8%, p = 0.15) (Fig. 2).
On multivariate logistic regression, compared to white patients with CRC, black patients with CRC were nearly four times more likely to have AJCC stage 3–4 disease at time of diagnosis (OR 3.70; 95% CI 0.97–14.11; p = 0.055) (Table 2). No significant differences in odds of AJCC stage 3–4 disease was observed among Hispanics and Asians when compared to whites. Compared to females, there was a trend towards greater odds of advanced CRC stage of disease at diagnosis (OR 2.03; 95% CI 0.90–4.61; p = 0.09).
Discussion
Among a large ethnically diverse urban hospital system, over 60% of patients with CRC were diagnosed at AJCC stage 3–4, and nearly 71% of blacks with CRC had AJCC stage 3–4 at diagnosis. Furthermore, black patients with CRC were nearly four times more likely to have advanced CRC stage at diagnosis when compared to white patients with CRC.
The proportion of advanced disease at time of CRC diagnosis in our cohort exceeds the observed proportion of advanced stage of CRC disease across several multi-center and single institution studies [1, 8, 15–18]. This discrepancy in the proportion of advanced disease may be due to the unique demographic makeup of our study cohort, specifically underserved safety-net populations. Using data from the SEER registry from 1988 to 2000, Chien et al. observed that black patients with CRC were 40% more likely to have AJCC stage 4 CRC at diagnosis compared to non-Hispanic whites with CRC [14]. Several other ethnic minority groups including Chinese, Mexicans, and American Indians were also observed to have higher risk of advanced CRC at diagnosis; 43% of whites, 49% of Asians, 47% of Hispanics, and 50% of blacks had AJCC stage 3–4 at time of diagnosis [14, 19]. Our study cohort is predominantly ethnic minorities, with 84% being of non-white race/ethnicity, and this demographic distribution may account for the overall higher risk of advanced CRC stage at diagnosis. In our cohort, 47% of whites, 63% of Asians, 52% of Hispanics, and 71% of blacks with CRC had AJCC stage 3–4 at time of diagnosis.
In a more recent study using updated registry data from SEER, Tawk et al. evaluated CRC outcomes by race/ethnicity and insurance status [19]. The study observed a significantly higher risk of advanced CRC among blacks compared to non-Hispanic whites (OR 1.181; 95% CI 1.103–1.264; p < 0.001). In addition, the authors demonstrated that patients with Medicaid (OR 1.187; 95% CI 1.085–1.299; p < 0.001) or no insurance (OR 1.654; 95% CI 1.414–1.934; p < 0.001) were significantly more likely to have advanced CRC at diagnosis compared to patients with commercial insurance, highlighting the impact of insurance status on access to care [19]. Our safety-net population is predominantly insured by Medicaid-type insurance, which may be another factor contributing to the high rates of advanced AJCC stage CRC at diagnosis observed.
The etiology of the disparities in stage of CRC disease by race/ethnicity is unclear. However, it is reasonable to hypothesize that disparate socioeconomic status contributing to disparities in timely access to preventative CRC screening and surveillance programs are at play. In addition, delays in timely implementation of CRC screening are also affected by provider-specific factors (e.g. delays in referral for CRC screening, lack of an integrated program for automatic and systematic reminders for CRC screening) and patient-specific factors (e.g. lost to follow up with clinical care, avoidance of CRC screening due to fear, anxiety, or lack of understanding) [8, 20]. While the socioeconomic and patient-specific factors are challenging, previous studies have suggested that race/ethnicity-specific disparities in CRC survival outcomes can be mitigated when socioeconomic factors are more normalized across all groups [20–22]. Among our safety-net population, socioeconomic disparities are clearly at play and likely impact to some degree timely access to preventive CRC screening and surveillance. Better understanding patient-specific and provider-specific factors in addition to socioeconomic factors that may contribute to delays in timely implementation of CRC screening and surveillance may provide opportunities to develop targeted programs and education towards both providers and patients to improve CRC outcomes among our underserved populations [23].
While our study’s focus on safety-net populations with CRC highlights the disparities in CRC outcomes among underserved ethnic minorities, the utilization of a single-centered population limits the generalizability of our findings to populations with different demographics. While we assume that the population in our study utilizes our hospital system for medical care, especially for cancer-related care, there exists the possibility that some of our patients received care at other institutions, including previous CRC diagnosis and treatment, prior to presenting to our hospital, potentially contributing to lost to follow up. Our focus on CRC stage at diagnosis is a surrogate for measures of access to preventative CRC screening. However, timely access to CRC screening is a complex process, and involves timely testing and referral by providers and patient navigation through the system to undergo diagnostic colonoscopy. While we were able to accurately assess the stage of CRC at diagnosis, we were not able to fully evaluate factors contributing to potential delays in access to colonoscopy (e.g. delayed referral, inability to contact patient, patient no-show to appointments). Nevertheless, our findings raise concern over the large proportion of patients, especially ethnic minorities diagnosed with advanced CRC stage.
In summary, among a large ethnically diverse cohort of underserved safety-net hospital patients, over 60% of patients were diagnosed with advanced stage CRC despite the existence of CRC screening and surveillance programs. Even more striking, over 70% of black patients with CRC with diagnosed with advanced stage disease. Advanced stage CRC at diagnosis limits the options for potentially curative therapies, and increases the risk for recurrence and lower long term survival. The goal of an effective CRC screening and surveillance program is reducing the incidence of CRC and early diagnosis such that curative treatments can be offered to increase long term CRC mortality. More programs are needed to target education and awareness to improve CRC screening and surveillance among underserved safety-net hospital populations and the providers that care for them.
Abbreviations
- AJCC:
-
American Joint Committee on Cancer
- CRC:
-
Colorectal cancer
- OR:
-
Odds ratio
- SD:
-
Standard deviation
References
Siegel, R. L., Miller, K. D., & Jemal, A. (2016). Cancer statistics, 2016. CA: A Cancer Journal for Clinicians, 66(1), 7–30. doi:10.3322/caac.21332.
Surveillance E, and End Results (SEER) Program (http://www.seer.cancer.gov) SEER*Stat Database: Incidence - SEER 9 Regs Research Data, Nov 2012 Sub (1973–2010) < Katrina/Rita Population Adjustment> - Linked To County Attributes - Total U.S., 1969–2011 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch, released April 2013, based on the November 2012 submission.
Gupta, A. K., Melton, L. J. 3rd, Petersen, G. M., et al. (2005). Changing trends in the incidence, stage, survival, and screen-detection of colorectal cancer: A population-based study. Clinical Gastroenterology and Hepatology: The Official Clinical Practice Journal of the American Gastroenterological Association, 3(2), 150–158.
Wong, R. J. (2010). Marked variations in proximal colon cancer survival by race/ethnicity within the United States. Journal of Clinical Gastroenterology, 44(9), 625–630. doi:10.1097/MCG.0b013e3181c64a7a.
Regula, J., Rupinski, M., Kraszewska, E., et al. (2006). Colonoscopy in colorectal-cancer screening for detection of advanced neoplasia. The New England Journal of Medicine, 355(18), 1863–1872. doi:10.1056/NEJMoa054967.
Mandel, J. S., Bond, J. H., Church, T. R., et al. (1993). Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota Colon Cancer Control Study. The New England Journal of Medicine, 328(19), 1365–1371. doi:10.1056/NEJM199305133281901.
Mandel, J. S., Church, T. R., Bond, J. H., et al. (2000). The effect of fecal occult-blood screening on the incidence of colorectal cancer. The New England Journal of Medicine, 343(22), 1603–1607. doi:10.1056/NEJM200011303432203.
Lai, Y., Wang, C., Civan, J. M., et al. (2016). Effects of cancer stage and treatment differences on racial disparities in survival from colon cancer: A United States population-based study. Gastroenterology, 150(5), 1135–1146. doi:10.1053/j.gastro.2016.01.030.
Silber, J. H., Rosenbaum, P. R., Ross, R. N., et al. (2014). Racial disparities in colon cancer survival: A matched cohort study. Annals of Internal Medicine, 161(12), 845–854. doi:10.7326/M14-0900.
May, F. P., Almario, C. V., Ponce, N., & Spiegel, B. M. (2015). Racial minorities are more likely than whites to report lack of provider recommendation for colon cancer screening. The American Journal of Gastroenterology, 110(10), 1388–1394. doi:10.1038/ajg.2015.138.
Almario, C. V., May, F. P., Ponce, N. A., & Spiegel, B. M. (2015). Racial and ethnic disparities in colonoscopic examination of individuals with a family history of colorectal cancer. Clinical Gastroenterology and Hepatology: The Official Clinical Practice Journal of the American Gastroenterological Association, 13(8), 1487–1495. doi:10.1016/j.cgh.2015.02.038.
Myers, R. E., Sifri, R., Daskalakis, C., et al. (2014). Increasing colon cancer screening in primary care among African Americans. Journal of the National Cancer Institute, 106(12), dju344. doi:10.1093/jnci/dju344.
Polite, B. N., Dignam, J. J., & Olopade, O. I. (2005). Colorectal cancer and race: Understanding the differences in outcomes between African Americans and whites. The Medical Clinics of North America, 89(4), 771–793. doi:10.1016/j.mcna.2005.03.001.
Chien, C., Morimoto, L. M., Tom, J., & Li, C. I. (2005). Differences in colorectal carcinoma stage and survival by race and ethnicity. Cancer, 104(3), 629–639. doi:10.1002/cncr.21204.
Schoen, R. E., Razzak, A., Yu, K. J., et al. (2015). Incidence and mortality of colorectal cancer in individuals with a family history of colorectal cancer. Gastroenterology, 149(6), 1438–1445. doi:10.1053/j.gastro.2015.07.055.
Schoen, R. E., Pinsky, P. F., Weissfeld, J. L., et al. (2012). Colorectal-cancer incidence and mortality with screening flexible sigmoidoscopy. The New England Journal of Medicine, 366(25), 2345–2357. doi:10.1056/NEJMoa1114635.
Nishihara, R., Wu, K., Lochhead, P., et al. (2013). Long-term colorectal-cancer incidence and mortality after lower endoscopy. The New England Journal of Medicine, 369(12), 1095–1105. doi:10.1056/NEJMoa1301969.
Jung, H. M., Lee, J. S., Lairson, D. R., & Kim, Y. (2015). The effect of national cancer screening on disparity reduction in cancer stage at diagnosis by income level. PLoS ONE, 10(8), e0136036. doi:10.1371/journal.pone.0136036.
Tawk R, Abner A, Ashford A, & Brown CP.( 2016). Differences in colorectal cancer outcomes by race and insurance. International Journal of Environmental Research and Public Health, 13(1), 48. doi:10.3390/ijerph13010048.
Le, H., Ziogas, A., Lipkin, S. M., & Zell, J. A. (2008). Effects of socioeconomic status and treatment disparities in colorectal cancer survival. Cancer epidemiology, biomarkers & prevention: A publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive. Oncology, 17(8), 1950–1962. doi:10.1158/1055-9965.EPI-07-2774.
Clegg, L. X., Reichman, M. E., Miller, B. A., et al. (2009). Impact of socioeconomic status on cancer incidence and stage at diagnosis: Selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes & Control, 20(4), 417–435. doi:10.1007/s10552-008-9256-0.
Pruitt, S. L., Shim, M. J., Mullen, P. D., Vernon, S. W., & Amick, B. C. 3rd, (2009). Association of area socioeconomic status and breast, cervical, and colorectal cancer screening: A systematic review. Cancer epidemiology, biomarkers & prevention: A publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive. Oncology, 18(10), 2579–2599. doi:10.1158/1055-9965.EPI-09-0135.
Jones, R. M., Devers, K. J., Kuzel, A. J., & Woolf, S. H. (2010). Patient-reported barriers to colorectal cancer screening: A mixed-methods analysis. American Journal of Preventive Medicine, 38(5), 508–516. doi:10.1016/j.amepre.2010.01.021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Chan, C., Lopez, A., Castaneda, G. et al. Black Patients with Colorectal Cancer Have More Advanced Cancer Stage at Time of Diagnosis: A Community-Based Safety-Net Hospital Experience. J Community Health 42, 724–729 (2017). https://doi.org/10.1007/s10900-016-0309-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-016-0309-0