Abstract
Preventive medicine plays a central role in the reducing the number of deaths due to preventable causes of premature deaths. General Preventive Medicine Residency programs have not been studied in relation to training in this area. A three-wave mail survey was conducted with email and telephone follow-ups. The outcome measures were the portion of program directors involved in training residents on firearm injury prevention issues and their perceived benefits and barriers of training residents on firearm injury prevention issues. Only 25% of the programs provided formal training on firearm injury prevention. Program directors who provided formal training perceived significantly higher number of benefits to offering such training than did directors who did not provide such training but no significant difference was found between the two for number of perceived barriers. If preventive medicine residency graduates are to play a role in reducing premature morbidity and mortality from firearms it will require more residencies to offer formal training in this area. The Association for Prevention Teaching and Research needs to develop guidelines on specific curriculum topics regarding firearm injury prevention.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Preventive medicine plays a central role in reducing the number of deaths due to preventable causes. Every encounter with a primary care physician is an opportunity for anticipatory guidance and shared decision-making with patients regarding injury prevention behaviors. One of the leading causes of injury death is firearm mortality, the 7th leading cause of death overall in adults and the 4th leading cause of death in youths [1, 2]. This is not surprising given the ubiquity of firearms in the United States. A recent nationally representative household telephone survey found that 38% of households (42 million) and 26% of individuals (57 million) reported owning a gun and 16% reported owning at least one handgun. Firearms in the home, especially handguns, have repeatedly been linked to increased risks of violent death of household members [3–8]. Compared to individuals without access to firearms; household access to firearms has been associated with a 17-fold increase in the risk of suicide by firearms [8].
The burden firearm trauma imposed on our society in 2005, the most recent year of comprehensive data, can be measured from a variety of perspectives, including firearm morbidity (nearly 70,000 received treatment for injuries) [9], firearm mortality (30,694 deaths) [10], societal costs (fear of firearm victimization and reduction in the quality of life), and financial costs (direct medical costs of $2 billion and indirect costs of $98 billion each year) [11]. To help reduce the costs of firearm injury, prevention activities by preventive medicine graduates can take many forms, including anticipatory guidance of patients (e.g., consequences of possession of firearms and proper storage of firearms), programs designed for community prevention (e.g., gun lock programs or firearm training), public policy advocacy regarding firearms, and the development of firearm trauma research agendas, all of which can help reduce firearm morbidity and mortality.
However, these activities are only likely to be engaged in by preventive medicine graduates if they have had residency training programs to improve their self-efficacy with regard to firearm preventive interventions. This endemic of firearm trauma in the United States has led to numerous medical specialty societies recommending that their members provide anticipatory guidance to patients regarding keeping firearms in the home and the need for appropriate firearm storage [12–17]. Thus, the purpose of this study was to determine the extent to which preventive medicine residency programs have incorporated information and activities regarding firearm violence and the perceived barriers to offering such training.
Methods
Sample
The entire population of 38 Preventive Medicine Residency (PMR) Program Directors in the United States was used for this study. The American College of Preventive Medicine Residency Programs Directory (ACPM) and Fellowship and Residency Interactive Database (FREIDA) of the American Medical Association (AMA) were used to identify the residency programs [18, 19].
Instrument
A comprehensive review of the empirical literature on firearms and physicians’ training on firearm injury prevention was used to create a questionnaire with adequate face validity. Subsequently, the questionnaire was sent to a panel (n = 4) of experts in the area of survey research and firearms to establish content validity. Minor wording changes to the questionnaire were incorporated based on reviewer comments.
The final questionnaire consisted of 22 items: Stages of Change (precontemplation, contemplation, preparation, action, maintenance) [20], key components of the Health Belief Model (perceived barriers for providing firearm injury prevention training to residents, perceived benefits of providing firearm injury prevention training to residents) [21], perceptions of firearm injury prevention activities and background/demographic questions. Most questions on the survey were closed format questions with multiple possible responses. Likert-type scales were used to assess program directors’ perceptions and beliefs.
Procedure
In Spring 2008, a three-wave postal mailing procedure using published techniques to increase response rates was used [22, 23]. For those who did not respond to the mail surveys, emails were sent and this was followed with telephone calls to the directors. The survey was approved by the University Human Subject’s Research Institutional Review Board.
Data Analysis
Data were analyzed using Statistical Package for Social Sciences (SPSS, Version 15.0, SPSS Inc., Chicago, IL). Level of significance was set a priori at p < 0.05. Frequency distributions were performed on categorical variables. Descriptive statistics were used to describe item responses. Cross-tabulations were calculated using Pearson’s chi-square tests, or independent samples t test were calculated to assess mean differences, as appropriate. Responses to open-ended questions were aggregated as descriptive information.
Results
Demographic/Background Characteristics
Of the 38 questionnaires mailed, 28 completed surveys (73.6%) were returned by program directors. The majority of respondents were females (60.7%), aged 40-49 years (50.0%), white (85.7%) and employed full time by the residency program (64.3%). Few (17.9%) program directors owned a gun and when they did it was used for personal protection, hunting or for personal collection. The majority of graduates from these residencies obtained jobs with government agencies (53.6%) or academic institutions (28.6%).
Current Attitudes and Practices in Training Residents on Firearm Injury Prevention
Program directors were asked to identify the firearm injury prevention training practices characteristic of their program (Stages of Change). A majority (53.6%) reported that they have not seriously thought about providing firearm injury prevention training to their residents (precontemplation). While 17.9% of program directors indicated they have been training residents in firearm injury prevention for more than a year (maintenance) and 14.3% of program directors were willing to discuss firearm injury prevention with residents only if the residents requested such information/training. An equal proportion of program directors (3.6% each) reported that they have been seriously discussing the possibility of including firearm injury prevention training in the future (contemplation) or they have been training residents in firearm injury prevention issues for less than 1 year (action). Few program directors (7.1%) affirmed that they use to train residents but now they do not train residents in firearm injury prevention (relapse).
Program directors were subsequently asked to report their current practices in routine screening of patients/clients for firearm ownership and more than two-thirds of the program directors (67.9%) reported that residents do not routinely screen their clients/patients for firearm ownership. Only 10.7% of the program directors reported that they routinely screen patients/clients for firearm ownership, the rest (21.5%) were either unsure of screening practices or had no routine interaction with patients.
Firearm Injury Prevention Topics Covered in the Residency Curriculum
Formal training topics on firearm injury prevention were listed and the program directors were asked to identify the training topics covered in their residency program (Table 1). Three-fourths (75.0%) of the program directors reported that they do not provide formal training on firearm injury prevention. The remaining program directors (25.0%) reported the three most important topics covered were, in order: politics of firearm sales in the United States (17.9%), types and relevance of the data sources on firearm issues (17.9%) and economic consequences of morbidity and mortality related to firearms (17.9%).
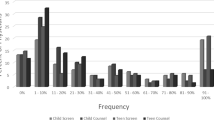
The programs were divided into two categories, programs that did not provide formal training for firearm injury prevention (75.0%) and programs that provided some form of training (25.0%). The two groups of programs were compared by number of residents in the programs (based on a median split of 5 or fewer residents versus 6 or more residents) and the duration of employment as the program director (based on a median split of 5 years or less versus 6 years or more). A chi-square test for number of residents in the programs was not associated with firearm injury prevention training status. However, the duration of employment of the program director was significantly (χ2 = 10.163, p < 0.001) associated with training status. Program directors who were employed for 5 years or less were less likely (5.6%) to report that they provided formal training compared to program directors employed for more than 5 years (60.0%).
Perceived Benefits and Barriers to Providing Firearm Injury Prevention Training
Program directors were asked to identify the potential benefits and barriers of providing firearm injury prevention training to their residents (Table 2). The four most important perceived benefits of providing firearm injury prevention training were, in order: increases attention by health departments towards firearm trauma prevention (67%), improved policies regarding firearms in the community (57.1%), reduction in health care costs due to firearm trauma (57.1%) and reduces morbidities associated with firearms in the community (53.6%). The ten perceived benefits of providing firearm injury prevention training were summed to create a training benefit score (potential range from 0 to 10). An independent samples t test found that the mean benefit score for program directors who provided firearm injury prevention training to residents (M = 6.00, SD = 2.70) was significantly (t = 2.910, p < 0.007) higher than the mean benefit score of program directors who did not provide any training (M = 3.19, SD = 2.04).
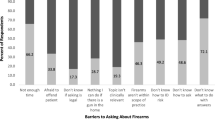
The four most important barriers to providing firearm injury prevention training to residents were, in order: no guidelines are provided by The Accreditation Council for Graduate Medical Education (ACGME) approved curriculum competencies (46.4%), lack of standardized teaching material for training the residents (39.3%), lack of existing guidelines for training residents on firearm issues (39.3%) and lack of faculty expertise on firearm issues in our residency training program (35.7%) (Table 2). The 15 perceived barrier items for providing firearm injury prevention training were summed to create a training barrier score (potential range from 0 to 15). Independent samples t test found that the mean barriers score for program directors who provided some form of training to residents was not significantly different than the mean for program directors who did not provide any training.
The program directors were also requested to quantify the mean didactic time spent on firearm injury prevention training over the 2-year residency and the mean amount of time spent was 0.6 h with a minimum of 0 h (78.1% programs) and a maximum of 4 h (3.6% programs).
Perceptions of Firearm Injury Prevention Activities
Equal numbers of program directors (39.3% each) agreed that the clients/patients of their residents would be accepting of the physician providing anticipatory guidance on firearm safety and the clients/patients would view the physician as an appropriate source of information regarding firearm safety (Table 3). Almost 9 out of 10 (89.3%) of the program directors perceived firearm control as a serious public health issue rather than an ideology or partisanship issue. About 2 in 5 (42.8%) program directors agreed that the residents in their program did not expect the residency training faculty to discuss firearm injury prevention issues. The Association for Prevention Teaching and Research (APTR) should provide guidelines on specific curriculum topics regarding firearm injury prevention was supported by a majority (78.6%) of the program directors.
Program directors were asked to comment on the amount of research funding by government agencies and foundations for firearm injury prevention and 78.6% agreed that the funding was not adequate. While 7.1% of the program directors thought that the funding was about right. Half (50%) of the program directors thought that their residents would be able to address the issues of firearm injury prevention if requested by clients/patients. The rest thought that their residents would not be able to address the issues of firearm injury prevention or were not sure about the capabilities of their residents regarding this topic.
Discussion
The vast majority (75%) of preventive medicine residency programs do not provide formal training on firearm injury prevention. Additionally, only 1 in 10 (10.7%) programs routinely screened their patients for firearm ownership. This was in spite of the fact that the vast majority (89.3%) perceived firearm control as a serious public health issue and not just an ideological or partisanship issue. These items are significant because most of the residents end up working for government agencies (53.6%) or academic institutions (28.6%), both positions have the unique opportunities to affect policies and to be role models for helping to reduce firearm injury violence.
Studies of other medical specialties (family medicine and pediatric residency training programs) identified similar perceived barriers to training that were identified in the current study (no trained personnel, lack of educational resources/guidelines and lack of time) [24, 25]. The percentages of programs providing formal training on firearm injury prevention differed across medical specialties. One-third (33.0%) of the pediatric residency training programs and 16.0% of the family practice residency programs provided formal training compared to 25.0% of the preventive medicine residency programs in this study [24, 25]. Preventive medicine specialists have an extra onus with not addressing a leading cause of premature mortality, firearm trauma, since they are uniquely placed in the medical professions to provide population services for injury prevention, diagnosis and treatment. Program directors identified increased attention by health departments to firearm injuries as one of the major potential benefits of providing training to residents but still, few preventive medicine residents are required to participate in firearm injury prevention training. This lack of participation is surprising given the fact that these residency programs are more prevention based than their primary care counterparts, family practice and pediatrics. The paucity of programs providing training is consistent with lack of standardized guidelines, lack of faculty expertise and lack of student interest as reported by the program directors. An integrated approach throughout the continuum of medical education is needed to change the attitude and practices of the residents and their mentors. In June 2008, the American Medical Associations’ Liaison Committee on Medical Education released another update of curricular mandates in medical education which stated “The curriculum must prepare students for their role in addressing the medical consequences of common societal problems, for example, providing instruction in the diagnosis, prevention, appropriate reporting, and treatment of violence and abuse.” [26] Furthermore, injury prevention is a crucial component of the core competencies and performance indicators for preventive medicine residents. Competencies are stated in behavioral terms; they are intended to define what preventive medicine residents can do as opposed to what they know or understand. Keeping this in mind it remains to be seen how program directors, institutions and residents work together to address the issues of firearm violence in the population.
The results of this study are potentially influenced by several limitations. First, because the response rate was acceptable (73.6%) but less than 100%, if the non-respondents differed significantly from respondents in their perceptions and practices, this would limit the external validity of the findings. Second, the closed format of the structured questionnaire was based on a comprehensive review of the firearm literature. To the extent that there may have been important perceptions regarding residency training on firearms not listed on the questionnaire this would have been a threat to the internal validity of the findings. In many of the questions this was minimized by having the option “other” and a space where respondents could write in alternative responses. Third, the responses were self reported and are subject to reporting bias. Finally, residency directors may have thought about the topic of firearm injury training in an uncharacteristic way because the questionnaire was on one topic (monothematic). To the extent this occurred it would have been a threat to the internal validity of the findings. A possibility of recall biases and socially desirable responding on the part of directors cannot be excluded.
References
Mokdad, A. H., Marks, J. S., Stroup, D. F., & Gerberding, J. L. (2004). Actual causes of death in the United States, 2000. Journal of the American Medical Association, 291, 1238–1245. (Errata, Journal of the American Medical Association 2005, 293–294).
Price, J. H., Murnan, J., Thompson, A. J., Dake, J. A., & Telljohann, S. K. (2005). Elementary school teachers’ involvement in firearm safety education. Journal of School Health, 75, 105–111.
Kellermann, A. L., & Reay, D. T. (1986). Protection or peril? An analysis of firearm-related deaths in the home. New England Journal of Medicine, 314, 1557–1560.
Bailey, J. E., Kellerman, A. L., Somes, G. W., et al. (1997). Risk factors for violent death of women in the home. Archives of Internal Medicine, 157, 777–782.
Miller, M., Azrael, D., & Hemenway, D. (2002). Rates of household firearm ownership and homicide across US regions and states, 1988–1997. American Journal of Public Health, 92, 1988–1993.
Kellermann, A. L., Rivara, F. P., Rushforth, N. B., et al. (1993). Gun ownership as a risk factor for homicide in the home. New England Journal of Medicine, 329, 1084–1091.
Kellermann, A. L., Somes, G., Rivara, F. P., et al. (1998). Injuries and deaths due to firearms in the home. Journal of Trauma, 45, 263–267.
Wiebe, D. J. (2003). Homicide and suicide risks associated with firearms in the home: A national case–control study. Annals of Emergency Medicine, 41, 771–782.
Wintemute, G. J. (2008). Guns, fear, the constitution, and the public’s health. New England Journal of Medicine, 358, 1421–1424.
Centers for Disease Control and Prevention. WISQARS (Web-based Injury Statistics Query & Reporting System). Accessed April 5, 2008, from http://www.cdc.gov/ncipc/wsqars.
Cook, P. J., & Ludwig, J. (2000). Gun Violence—the real costs (pp. vii–x). New York: Oxford University Press.
American Academy of Pediatrics, Committee on Injury, Poison Prevention. (2000). Firearm-related injuries affecting the pediatric population. Pediatrics, 105, 888–895.
American College of Physicians. (1998). Firearm injury prevention. Annals of Internal Medicine, 128, 236–241.
American Academy of Family Physicians. Firearms/handgun firearms, handguns and assault weapons. http://www.aafp.org/x6823.xml.
American Association of Orthopedic Surgeons. Firearms violence. http://www.aaos.org/wordhtml/papers/position/1134.html.
American Medical Association. H-145,000 firearms: Safety and regulation. http://www.ama-assn.org/apps/pf_online.
Committee on Trauma of the American College of Surgery. (2000). Statement on firearm injuries. Bulletin of the American College of Surgeons, 85, 24.
American College of Preventive Medicine. Residency directory at a glance. Accessed February 9, 2008, from http://www.acpm.org/education/residency/ataglance.htm.
American Medical Association. Fellowship and Residency Interactive Database (FREIDA). Accessed February 9, 2008, from http://www.ama-assn.org/ama/pub/category/2997.html.
Prochaska, J. O., DiClemente, C. C., & Norcross, J. (1992). In search of how people change: Applications to addictive behaviors. American Psychologist, 47, 1102–1114.
Janz, N., & Becker, M. (1984). The health belief model: A decade later. Health Education Quarterly, 11, 1–47.
Edwards, P., Roberts, I., Clarke, M., et al. (2002). Increasing response rates to postal questionnaires: Systematic review. British Medical Journal, 324, 1183–1187.
King, K. A., Pealer, L. N., & Bernard, A. L. (2001). Increasing response rates to mail questionnaires: A review of inducement strategies. American Journal of Health Education, 32, 4–15.
Price, J. H., Conley, P. M., & Oden, L. (1997). Training in firearm safety counseling in pediatric residency programs. Archives of Pediatric and Adolescent Medicine, 151, 306–310.
Price, J. H., Bedell, A. W., Everett, S. A., & Oden, L. (1997). Training in firearm safety counseling in family practice residency programs. Journal of Community Health, 22, 91–99.
The Liaison Committee on Medical Education (LCME). Current LCME accreditation standards. Accessed July 3, 2008, from http://www.lcme.org/standard.htm.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khubchandani, J., Price, J.H. & Dake, J.A. Firearm Injury Prevention Training in Preventive Medicine Residency Programs. J Community Health 34, 295–300 (2009). https://doi.org/10.1007/s10900-009-9156-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-009-9156-6