Abstract
Despite the growing body of evidence demonstrating the high prevalence of intimate partner violence (IPV) among male couples and the unique antecedents to IPV that male couples may experience, research efforts have focused almost exclusively on North American populations. Missing from the literature is an understanding of the experience of IPV among male couples in African nations where social norms and legal restrictions around same-sex behavior may be more conservative. This paper presents data from an innovative study of male couples (Together Tomorrow) from two Southern African countries characterized by high prevalence of HIV: Namibia and South Africa. A one-time cross-sectional survey was conducted with 140 partnered MSM (70 couples) in Namibia and 300 partnered MSM (150 couples) in KZN, South Africa, for a total sample size of 440 partnered MSM (220 couples). Surveys measured the recent (12 month) experience of physical, sexual and emotional IPV and the experience of sexuality-related stressors. Reporting of IPV was relatively low: 7.3% reported being the victim of IPV from their male partner in the 12 months prior to the survey, and 10.2% reported participating in bi-directional IPV in their relationship in the previous 12 months. Men who reported different experiences of internalized homophobia and external acts of discrimination were more likely to report IPV and bi-directional IPV. The results offer several potential intervention points to disrupt pathways between stigma and IPV for partnered MSM in South Africa and Namibia, and point to the need for services for this critically overlooked population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization (2012) defines intimate partner violence (IPV) as any behavior between a dyad that involves acts of physical and sexual violence, emotional and psychological abuse, and controlling behavior. Despite recognition that IPV can occur between partners of any gender (Ali et al. 2016; Capaldi et al. 2007), programmatic and research attention has largely focused on female victim and male perpetrator forms of IPV. The past ten years has witnessed the emergence of a substantial body of literature illustrating that that men who have sex with men (MSM) experience IPV at rates that are substantially higher than those experienced by men who do not have sex with men, and rates that are comparable or higher to those among heterosexual women (Finneran and Stephenson 2013). Based almost exclusively on estimates from the US, the estimated prevalences for the recent (past 12 month) receipt of IPV among MSM vary greatly by type of IPV, although estimates for the experience of any form of IPV ranges from 32% (Houston and McKirnan 2007) to 54% (Pantalone et al. 2012). The recent experience of physical IPV ranges from 12% (Stephenson et al. 2010) to 45% (Craft and Serovich 2005), while for sexual IPV the range is from 1.8% (Bartholomew et al. 2008) to 33% (Craft and Serovich 2005). Similarly, estimates of the prevalence of emotional/psychological IPV range from 28% (Pruitt et al. 2015) to 64% (Bartholomew et al. 2008). Perpetration rates of violence have been comparatively less studied among MSM, and estimates for recent perpetration (past 12 months) range from to 8.3% (Carvalho et al. 2011) to 36% (Welles et al. 2011) – both substantially higher than those reported by men who have sex with women, yet similar to the prevalence reported by women in opposite sex relationships. Of particular importance to MSM is emergent evidence demonstrating a link between IPV and risk for HIV infection (Feldman et al. 2008; Greenwood et al. 2002; Koblin et al. 2006; Relf 2001; Stephenson et al. 2011a). Several studies have shown significant associations between IPV victimization and having unprotected intercourse (Osinde et al. 2011) and substance use among MSM (Kalokhe et al. 2012), with participation in unprotected sex or substance use both likely stress-response behaviors to exposure to IPV.
There is also recent evidence that while same-sex male couples experience IPV at rates similar to opposite-sex couples, male couples may experience unique antecedents to IPV that are linked to their sexual minority status (Finneran and Stephenson 2013). In a survey of 1075 MSM in Atlanta, Stephenson and Finneran (2017a, b) reported that while many of the triggers for IPV identified by studies of opposite-sex couples emerged as significant antecedents for IPV among male couples, (including general life stressors such as alcohol, drugs, jealousy, and financial stress), there were a number of triggers to IPV that were specific to male couples. These included one or both partners not having disclosed their sexual identity, disagreements around sexual positioning, and threats to masculinity created by both men striving to be the “alpha male” in the relationship (Stephenson and Finneran 2017a, b). Using qualitative data from the same sample, Goldenberg et al. (2016), identified additional sources of tension shaping the risk of IPV in their relationship, including gender role conflict, dyadic inequalities (e.g., differences in income and education), differences in “outness” about sexual identity, substance use, and external homophobic discrimination.
One specific antecedent to IPV among male couples that has received significant recent research attention is the role of sexual minority stress. Meyer (1995, 2003) defined minority stress as the “excess stress to which individuals from stigmatized social categories are exposed as a result of their social, often a minority, position”. Several studies have identified correlations between internalized homophobia (negative feelings about one’s own sexual identity) and perpetration of physical IPV (Balsam and Szymanski 2005; Burgard et al. 2012: Edwards and Sylaska 2012), sexual IPV (Balsam and Szymanski 2005), and emotional/psychological IPV (Balsam and Szymanski 2005). Homophobic discrimination and sexual orientation concealment are also correlates of perpetration of physical IPV (Lewis et al. 2017). Experiences of minority stress can evoke feelings of anxiety, shame, and victimization, resulting in self-devaluation (Stephenson and Finneran 2017), predisposing MSM to experiences or perpetration of IPV. Internalized homophobia correlates with poor relationship quality among gay men (Frost and Meyer 2009) and higher levels of internalized homophobia decrease a couple’s belief in their ability to adequately communicate and make joint decisions (Stachowski and Stephenson 2015), all of which may create triggers for IPV.
Despite the growing body of evidence demonstrating the high prevalence of IPV among male couples and the unique antecedents to IPV that male couples may experience, research efforts have focused almost exclusively on North American populations. Missing from the literature is an understanding of the experience of IPV among male couples in African nations – where social norms and legal restrictions around same-sex behavior may be more conservative. Only a small number of studies have examined IPV among MSM in African countries. In a study of men who have sex with men and women (MSMW) in South Africa, Eaton et al. (2013) demonstrated that MSMW experienced sexual and physical violence at elevated rates; compared to men who had sex with men, MSMW reported higher rates of recent episodes of partner violence and perpetrated forced sex. Similarly, using a sample of 521 MSM recruited online in South Africa, Stephenson et al. (2011a, b) demonstrated that prevalence of IPV, both experienced and perpetrated, was relatively high, with 8% of men reporting having experienced recent physical IPV and 4.5% of men reporting recent experiences of sexual IPV. Approximately 4.5% of MSM reported recently perpetrating physical IPV, while the reporting of perpetration of recent sexual IPV was much lower at 0.45%. In a cross-national study using online samples from six countries (US, UK, Canada, Brazil, South Africa and Australia) Finneran et al. (2012) found that the reporting of experiencing physical IPV ranged from 5.75% in the U.S. to 11.75% in South Africa, while experiencing sexual violence was less commonly reported and ranged from 2.54% in Australia to 4.52% in the U.S. Perpetration of physical violence ranged from 2.47% in the U.S. to 5.76% in South Africa.
The few studies to have focused on IPV among MSM in African contexts have used either online samples – restricting enrollment to only those with an online presence – or have failed to examine unique antecedents of IPV that may be linked to sexual minority status. There is now clear evidence that MSM in African countries have an approximately 19 times greater odds of acquiring HIV compared to the general adult male population (United Nations Population Fund 2015). The high levels of sexuality-based stigma experienced by MSM in these contexts limit physical and administrative access to prevention services and shape their risk of HIV acquisition (Andrinopoulos et al. 2015; Arnold et al. 2013; Choi et al. 2008). There is a clear need to understand the prevalence and correlates of IPV among MSM in African settings characterized by high levels of sexuality-based stigma and resultant risk of HIV. This paper presents data from an innovative study of male couples from two Southern African countries: Namibia and South Africa. The paper aims to model, for the first time, the factors associated with reporting the experience of IPV victimization and bidirectional IPV among a large sample of male couples. Understanding the experience of IPV for MSM in these contexts is a vital first step in designing interventions that can address IPV reduction and interrupt pathways between stigma, IPV and poor physical and mental health outcomes for partnered men in these countries.
Study Settings
South Africa and Namibia are both in the midst of catastrophic HIV/AIDS epidemics. Between 11 and 20% of South African adults are HIV infected, with 420, 000 children orphaned by AIDS, and approximately 1500 new infections daily (Statistics South Africa 2018). Between 17 and 23% (approximately 200,000) of Namibian adults are living with HIV (CDC in Namibia 2020). South Africa is significantly ahead of many other African nations in terms of advancing LGBT human rights through decriminalization of homosexuality (1996) and legalization of same-sex marriage (2007). The 2017–2022 South African National LGBTI HIV Prevention plan includes MSM as a priority group for HIV prevention and care (South African National AIDS Council, 2017, https://sanac.org.za/wp-content/uploads/2017/06/LGBTI-HIV-Plan-Final.pdf). A significant number of HIV prevention and care programs have been implemented specifically for MSM, adopting a rights-based framework to encourage equal access to HIV prevention and services (Van der Pol et al. 2018). As in many other sub-Saharan African countries, MSM exist in a climate of homophobia and criminalization in Namibia. When Namibia became independent in 1990, leaders were quick to establish a constitution that was seen as progressive and inclusive; however there was no specific mention of equal rights for LGBT individuals, and the constitution included difficult to enforce anti-sodomy laws. However, in 1996, President Nujuma called for the expulsion of LGBT individuals from Namibia, leading to an outbreak of anti-gay violence and persecution (Ottonson 2007). Same-sex sexual behavior remains illegal in Namibia and MSM are routinely left out of national HIV programming efforts.
Methods
Data from this study are from a cross-sectional survey conducted with male couples in South Africa and Namibia. The data were collected by the Human Sciences Research Council (HSRC) KwaZulu-Natal (KZN), South Africa in collaboration with the Pietermaritzburg Gay and Lesbian Network (South Africa) and Positive Vibes (Namibia), under a project entitled Together Tomorrow. Ethical review was conducted and approved by the HSRC in South Africa and the Ministry of Health and Social Services (MoHSS) in Namibia. A one-time cross-sectional survey was conducted with 140 partnered MSM (70 couples) in Namibia and 300 partnered MSM (150 couples) in KZN, South Africa, for a total sample size of 440 partnered MSM (220 couples). Data were collected November 2016–March 2017. The survey was prepared in English and translated into isiZulu and Afrikaans and back translated into English for verification. In South Africa, male couples were sampled from Pietermaritzburg and Durban. In Namibia, due to smaller population numbers and issues experienced in accessing MSM communities, male couples were sampled from Windhoek, Keetmanshoop and Walvis Bay/Swakopmund.
Recruitment for the survey targeted self-identified MSM over 18 years, residing in the study area and who reported that they have been in a relationship with another man for at least three months and have had anal/oral sex with each other in the last 3 months preceding the survey. A partner was defined as “a man with whom you are having a sexual relationship and feel emotionally committed to above others, you may call this man a boyfriend, partner, lover etc.” It is possible that men may have concurrent sexual relationships/ partnerships with other men. Men were asked to choose one man they defined as their main partner, using the definition above, although the survey also asked participants about other concurrent sexual and romantic partners. To participate, both partners needed to identify each other as their primary partner and provide consent individually.
Participants were recruited through a venue-based sampling (VBS) approach that led to a constrained snowball sample (Heckathorn 1997). Traditional probability sampling could not be applied due to the lack of an adequate sampling frame and anti-homophobic stigma in the study communities. VBS is a derivative of time-space sampling in which sampling occurs within prescribed blocks of time at particular venues. As a method to access hard-to-reach populations, VBS is a process in which a sampling frame of venue-time units is created through formative research with key informants and community members. After creating a list of potential venues, study staff members visited each venue to confirm that the venue is active at those times and the population in question accesses the venue. A diverse range of venues was selected to represent social, cultural (i.e. churches), and health care settings. Venues were selected from our formative work and in consultation with community partners. Participants were given study cards to pass to men with main partners in their social network. Each participant was given only two cards, to prevent all participants from being recruited from one social network. Participants were asked to explain participation in the study to their contacts/friends. Referred participants who completed the study were also given two cards, and thus the sample evolved through a snowball chain-referral process. Participants were reimbursed ZAR 30/N$30 (approximately USD$2.50) in mobile airtime for each participant (up to two participants) successfully recruited to the study. Each participant who completed the survey was reimbursed ZAR 75/ N$75 (approximately USD$5.25) for time and travel expenses.
Participants recruited in venues, or referred by other participants, were asked to attend local study sites to complete the survey. Upon arrival at the study site, the dyad was escorted to two private rooms where they completed written informed consent individually. The interviews were also conducted separately and were interviewer-administered electronically. A couple identifier allowed dyadic data to be linked. Participants self-reported HIV sero-status: those who self-reported sero-negative or unknown sero-status were given HIV testing onsite using a finger-prick rapid test, with prevention counseling, referral to risk-reduction services and linkage to care and confirmatory testing for those testing preliminarily sero-positive.
Demographic Measures
The survey collected self-reported age, race, educational attainment, employment status, socio-economic status, country of origin, HIV-status and religion. Sexual and gender identity were both self-identified, and allowed spaces for participants to write in their identity.
Risk Behaviors and Vulnerability
The CES-D-10 (Radloff 1977) was included to assess depressive symptomology, and hazardous alcohol consumption was measured using the AUDIT-C measure (Saunders et al. 1993). Recent (past 12 months) non-medical drug use, including non-medical injection drug use, was also assessed using the ASSIST scale (Humeniuk et al. 2008). The survey also assessed experiences of arrest and incarceration in the past 12 months.
Intimate Partner Violence
The survey measured both recent (previous 12 months) experience (victimization) and perpetration of IPV using the Gay and Bisexual Men (IPV-GBM) scale (Experience: Cronbach’s alpha >0.78: Perpetration Cronbach’s alpha >0.76) adapted from the Conflict Tactics scale to more accurately measure IPV among gay and bisexual men (Stephenson and Finneran 2013a, b). The IPV-GBM scale was developed to measure the experience of IPV in male couples. Full details of the scale development and validation can be found at Stephenson and Finneran (2013a, b). The IPV-GBM has been used in samples of MSM and gay/ bisexual men to measure the recent prevalence of IPV and to explore associations between IPV and HIV risk behaviors (Stephenson and Finneran 2017a, b). The scale encompasses 23 measures over four domains of IPV: physical and sexual (e.g. “[partner] punched, hit, or slapped you?”, “[partner] raped you?”), emotional (“e.g. “[partner] told you to ‘act straight’ around certain people?”, “[partner] called you fat or ugly?”), controlling (e.g. “[partner] prevented you from seeing your family?”, “[partner] prevented you from seeing your friends?”), and monitoring (e.g. “[partner] demanded access to you email?”, “[partner] read your text messages without your knowledge?”). Respondents provided a nickname for their partner, which was then piped into the question to replace [partner]. Questions were asked about the experience of IPV in the past 12 months and the perpetration of IPV in the past 12 months, as separate sets of questions (“Has your partner done any of the following to you in the past 12 months?”, “Have you done any of the following to your partner in the past 12 months?”
Relationship Characteristics
In terms of relationship characteristics, respondents reported duration of current partnership, co-residency, whether they had ever experienced a break in their current relationship, and the label they assigned to their relationship (i.e. boyfriend, partner, and lover). The survey assessed several measures of relationship quality. Degree of happiness with the relationship was assessed with one item “Please indicate the degree of happiness, all things considered, of your relationship,” with a seven-point response scale ranging from 1 (extremely unhappy) to 7 (Extremely happy).” The Conflict Style Inventory (CSI) (Levinger and Pietromonaco 1989), measured perceived conflict resolution styles in relationships, with higher scores indicating constructive strategies (i.e., more collaborating, more compromising, and less contending). Desire for the future of the relationship was measured with one item: “Which of the following statements best describes how you feel about the future of your relationship?”, options included: “I want desperately for my relationship to succeed, and would go to almost any length to see that it does” and “I want very much for my relationship to succeed, and will do all I can to see that it does.” (Spanier 1976). Commitment to the relationship was assessed with the Investment Model Scale (Rusbult et al. 1998), that included seven questions measuring an individual’s intent to persist in a relationship (i.e. “I am committed to maintaining my relationship with my partner”) with a nine-point response scale ranging from 1 (Do not agree at all) to 9 (Completely agree). The presence of sexual agreements – agreements as to whether the couple could have sex with other partners – the typology of the sexual agreement (i.e. monogamous, sex allowed with other partners), as well as the breaking of agreements and subsequent disclosure in the past 12 months, were also assessed.
Stigma
To examine associations between experiences of sexuality-based stigma and experiences of IPV, the survey included measures of internalized, anticipated and enacted sexuality-based stigma, using validated measures of anticipated stigma (Liu et al. 2009), enacted stigma (Liu et al. 2009) and internalized homophobia (Smolenski et al. 2010). Internalized homophobia was measured using an 8-item scale that measured three factors: (1) personal comfort with a gay identity, (2) social comfort with gay men, and (3) public identification as gay. Enacted stigma was measured with eight questions about how often respondents had experienced different forms of enacted stigma within three general categories: criminal victimization, harassment and threats, and discrimination with a 4-point Likert scale responses. Anticipated stigma was measured by eleven questions designed to rate the degree of respondents’ agreement concerning negative attitudes in the community towards gay individuals.
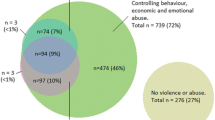
The current analysis examines factors associated with the experience and perpetration of IPV among the sample of partnered MSM. Only 15 participants reported only perpetrating any form of IPV with no bidirectional violence from their partner, too few for multivariable analysis. Two binary outcomes are considered. First is a binary outcome coded one if the respondent reports only experiencing any form IPV in the past 12 months from their current male partner (sexual, physical, emotional, controlling or monitoring), and did not perpetrate IPV against their partner. Second is a binary outcome coded one if the respondent reports both experiencing from and perpetrating IPV against their current male partner in the past 12 months (bidirectional IPV) (sexual, physical, emotional, controlling or monitoring). Data for both countries are analyzed as a pooled data set: the sample size for Namibia was too small to allow country-specific analyses.
For this analysis, N equaled the total number of individuals (n = 440) and not the total number of couples. Alternative statistical approaches, such as Actor Partner Independence Modeling (APIM), would consider the couple as the unit of analysis, and examine the associations between partners A and B’s characteristics on the outcomes. However, the intent of the current analysis is to understand how an individual’s experiences of sexuality-based stressors shape the reporting of IPV. The model therefore takes the form of a multilevel logistic model, with a random intercept for the dyad, to allow for the clustering of observations within dyads.
Separate multilevel logistic regression models were fit to identify independent associations of demographic, relationship quality and dyadic difference characteristics with each of the binary measures of IPV (experience of IPV and bidirectional IPV). Dyadic difference variables were calculated as the difference between responses from partner A and B, and are included as either binary variables (when partners report different versions of events i.e. different sexual agreements) or as continuous variables (when partners report different values on scales). Results are presented as adjusted odds ratios (aORs) with 95% confidence intervals (CIs). Statistical analyses were conducted using STATA v15.
Results
Participants ranged in age from 18 to 55 years, with 34.5% aged 18–24 years and 14.1% aged over 35 years (Table 1). Participants predominantly identified as Black African (68.4%) and gay (71.4%). Just over one-quarter (25.9%) self-reported HIV-positive sero-status. Approximately one-third had education at University/ college level or higher (30.1%) and 51.2% reported current full-time employment. A significant proportion of participants (48.8%) reported relationship lengths of less than 12 months, with 18.2% reporting being together for over three years. Only 34% of participants reported cohabiting with their partner. Approximately one-in-five (19.8%) reported they had a sexual agreement with their partner, and 21.2% reported that they had at some point broken up with their current partner. In terms of HIV risk behaviors, 7% of participants reported participating in transactional sex in the six months prior to the survey, while 77.5% reported binge drinking and 52.7% reported using non-prescription drugs in the previous three months. Approximately half of men in the survey (49.1%) reported having tested for HIV in the past 12 months, and 17.9% reported using a condom at last sex with their primary sex partner (the partner who was enrolled in Together Tomorrow with them). Reporting of IPV was relatively low: 7.3% reported being the victim of IPV from their male partner in the 12 months prior to the survey, and 10.2% reported participating in bi-directional IPV in their relationship in the previous 12 months (Table 2).
Demographic and Risk Factors
Participants in South Africa were less likely to report both the experience of IPV (OR 0.45, 95%CI 0.13, 0.79) and the experience of bi-directional IPV (OR 0.82, 95%CI 0.17, 0.98) in their relationships than men in Namibia. Men who self-reported HIV-positive status were less likely to report having experienced IPV from their male partner (OR 0.45, 95%CI 0.26 0.89), but were more likely to report the presence of bi-directional IPV in their relationships (OR 1.90, 95%CI 1.24, 2.57). Men who reported engaging in recent substance use or binge drinking were more likely to report both experiencing IPV (OR 6.98, 95%CI 4.15, 8.21) and experiencing bi-directional IPV (OR 1.42, 95%CI 1.05, 1.70) in their relationships.
Relationship Characteristics
Several relationship characteristics were significantly associated with reporting IPV. Men reporting higher levels of happiness with their relationship were less likely to report bi-directional IPV (OR 0.75, 95%Ci 0.57, 0.98) and men reporting higher level of commitment to their relationship were less likely to report experiencing IPV (OR 0.95, 95%CI 0.90, 0.99). Relationship durations over three years were associated with significantly greater reporting of both experience of IPV (OR 10.45, 95%CI 8.42, 12.47) and bi-directional IPV in the current relationship (OR 1.62, 95%CI 1.15, 2.85). Men who assigned more formal relationship labels to their relationships (i.e. partner or husband) were more likely to report experiencing IPV than men assigning more informal relationship labels (i.e. fuck-buddy) (OR 1.83 95%CI 1,10, 2.54). Men who lived together were more likely to report bi-directional IPV (OR 2.77, 95%CI 1.25, 6.13), while those who reported that they had ever broken up with their current partner were more likely to report experiencing IPV (OR 1.10, 95%CI 1.02, 1.23).
Stigma
While individual experiences of stigma were not independently associated with reporting IPV, dyadic differences in stigma and relationship characteristics were significant correlates of IPV. Men who reported different sexual agreements to their partners were more likely to report both experiencing IPV (OR 1.55, 95%CI 1.23, 1.86) and bi-directional IPV (OR 2.63, 95%CI 1.15, 4.52) in their relationship. Men who reported a differing level of commitment than their partner were more likely to report experiencing IPV (OR 1.58 95%CI 1.23, 1.86), but were not more likely to experience bi-directional IPV. Men who reported different experiences of both internalized homophobia (experienced IPV: OR 1.45, 95%CI 1.23, 1.78: bi-directional IPV: OR 1.78, 95% CI 1.45, 2.38) and enacted sexuality-based stigma (experienced IPV: OR 1.98, 95%CI 1.45, 2.56: bi-directional IPV: OR 1.57, 95% CI 1.12, 1.98) were more likely to report both experiencing and bi-directional IPV: there was no association between differences in anticipated sexuality-based stigma and reporting of IPV.
Discussion
This innovative study of partnered MSM in South Africa and Namibia represents the first attempt to estimate and understand the correlates of IPV among a vastly overlooked population – coupled men living in contexts characterized by a high prevalence of HIV. Reporting of both the experience of IPV (7.3%) and bi-directional IPV (10.2%) were relatively low compared to prevalence estimates from North American samples, yet were comparable to estimates from the only two other studies of IPV among MSM in South Africa (Finneran et al. 2012; Stephenson et al. 2011a, 2011b).
There are several possible explanations for the generally low levels of reporting of IPV in this sample of male couples. The reporting of low levels of experiencing IPV, relative to high levels of bi-directional IPV, may be shaped by social and cultural norms around masculinity and violence. Previous studies focused on IPV among opposite sex couples have shown associations between the perpetration of IPV by men against women and men’s beliefs and adherence to traditional norms that view masculinity as dominant, violent, or controlling (Moore and Stuart 2005). There is also evidence that men may use violence as a resource for overcoming challenges to masculinity (i.e. unemployment) (Messerschmidt 2000). Hunt et al. (2016) hypothesize that the persisting stereotype that gay men are not masculine may lead gay men to be vulnerable to threats to their masculinity, and react to this challenge by distancing themselves from feminine-stereotyped gay men or by attempting to present themselves as more masculine. Admitting to experiencing IPV may be seen as a challenge to masculinity, and perpetrating IPV may be a reinforcement of masculinity (Hunt et al. 2016). Therefore, men may be more likely to report that they were involved in bi-directional IPV than that they were the victim of violence. Alternatively, there may be issues with the measurement of IPV in this context. It is possible that men do not perceive all the acts they experience as IPV. The questions used to assess IPV ask men to respond to a list of acts (including physical, emotional, controlling, and monitoring) and note whether their partner has done this to them, or they have done this to their partner (as separate questions) in the previous 12 months. The questions do not directly ask the respondents if they have experienced or perpetrated IPV: they report the experience or perpetration of acts, which are then used to classify the presence or absence of IPV in the relationship. While some acts listed fall into more widely accepted definitions of violence, i.e. forced sex, other acts may not be commonly perceived as IPV. If we accept that IPV is a socially undesirable behavior that is likely to be under-reported, men may under-report the prevalence of acts that are seen as IPV: however, this argument is equally applicable to all studies of IPV that rely on self-reported measures. Additionally, there may be locally and culturally specific forms of IPV that are were not included in the scale used to measure IPV, and further work is warranted to understand whether scales need to be further adapted for African MSM.
Many of the correlates of IPV identified are not surprising. Men who were happier and more committed to their relationships were less likely to report IPV: individual levels of commitment and dyadic differences in commitment were associated with IPV, but only individual reports of happiness were associated with bidirectional IPV. Those who had broken up previously reported more IPV. Each of these associations could work in either direction: the lack or presence of IPV could cause greater happiness, commitment or breakups, or the presence of greater happiness, commitment or breakups could act as protective factors or antecedents to IPV. Men who cohabited with their partner, referred to their partnership in more formal terms and had been together longer were more likely to report IPV. This likely reflects both the influence of both time and opportunity: couples who are together longer and spend more time together have greater potential to experience triggers for IPV. Similarly, men who reported different sexual agreements or levels of commitment to their relationships different than their partner were more likely to report IPV. This likely reflects a lack of communication and concordance of feelings within the relationship, which may create tension leading to IPV.
Results point to the role of sexual minority specific stressors in shaping the risk of IPV. At the macro-level, men in South Africa reported less IPV than men in Namibia, likely reflecting the vastly different social and legal environments for MSM in the two countries. Men in Namibia exist in an environment in which same-sex behavior is illegal: this stress likely manifests as anger, frustration and violence among men as they struggle to exist as couples in an environment which deems their relationship as illegal and immoral. In both countries, binge drinking and substance use were highly correlated with IPV. Much has been written about the high levels of alcohol and substance use among MSM (Zhang et al. 2016), including evidence that use may be a coping strategy to deal with exposure to sexual minority stress (McCarty-Caplan et al. 2014). In some contexts, such as environments where homosexuality is highly stigmatized, drug use may be a strategy to mitigate stress associated with internalized homonegativity or experiences of discrimination and to normalize same-sex thoughts, feelings, and behaviors or connect with others in the gay community (Bauermeister 2007; Ha et al. 2015; Peacock et al. 2015). Substance and alcohol use are well known triggers for IPV, creating inhibitions and loss of emotional regulation, and have previously been highlighted as correlates of IPV among MSM. Folch et al. (2010) in a study of MSM in Spain, notes that substance use was lower among partnered MSM, suggesting that being a relationship may provide a buffer to the stressors that drive substance use. However, in the current study, men reported very high levels of binge drinking (77.1%) and substance use (52.4%), suggesting that the high levels of external sexuality-based stressors override the protective effects of relationships, and may be a leading driver of IPV within these relationships.
These results also have implications for HIV risk. Both countries represent context in which MSM experience high prevalence of HIV (in this sample 17.2% were HIV-positive). Factors that are known to increase HIV risk – substance use and binge drinking, a lack of communication around the terms of sex that may be allowed outside of the relationship, and the experience of minority stressors – were significantly associated with increased risks for IPV. For example, men who experience IPV (as victims or perpetrators) may be using substances or alcohol to deal with IPV associated stress, and equally the use of substances or alcohol could fuel conflict within relationships. IPV should be considered a key antecedent of HIV risk in these setting, and there is a need to build into HIV prevention and care programs not only screenings for IPV risks, but opportunities to talk to men about how IPV may shape their risk of HIV.
Interestingly, no individual-level experience of sexuality-based minority stressors were associated with the reporting of IPV: only dyadic differences in the reporting of stressors were significantly associated with reporting IPV. The link between minority stress and IPV in male couples is highly plausible. The negative outcomes associated with minority stress (e.g., drug use) are known to be linked to increased risk of IPV, and therefore, it seems reasonable that the experience of minority stress may also lead to increases in IPV through creating tension, poor communication, lowered self-esteem, and the adoption of maladaptive behaviors in relationships. However, among this sample of male couples, IPV was associated with differences in the experiences of internalized homonegativity and enacted stigma. These differences may reflect differing levels of resiliency and support between the partners, acting to create tension, jealousy or resentment. It is plausible that if one partner is experiencing more episodes of discrimination, this could manifest as anger and violence in the relationship or could reduce the individual’s feelings of self-esteem and self-worth, each making IPV more likely.
While this study represents the first attempt to understand the correlates of IPV among male couples in two African countries, there are several limitations worth noting. Men were recruited through venue-based recruitment, with a focus on gay friendly spaces. This may have produced a sample with a greater degree of community connectedness, which may be a protective factor for IPV. While the survey did not measure community connectedness, further work is warranted with more generalized samples of MSM, and to understand how community connectedness may moderate the risk of IPV. The survey also did not identify which venue participants were recruited from, limiting assessments of differences in participant characteristics by recruitment venue. While this recruitment approach has been found to produce samples similar to alternative recruitment methods (Hernandez-Romieu et al. 2014), it meant the current sample necessarily excluded men who did not access gay-themed or gay-friendly venues during the sampling period. Additionally, the cross-sectional design of this study means that neither causality nor directionality can be inferred. The survey did not include several potential correlates of IPV, including the experience of childhood abuse, exposure to parental IPV as a child, and other stressors such as financial or employment stress. Observed prevalence of IPV was low: the data used in this study were self-reported (for IPV), and social desirability bias may have shaped the participants’ willingness to report IPV. Additionally, all types of IPV were combined into a single variable, prohibiting understanding of whether findings are consistent across all types of IPV or are potentially being driven by one or two types of IPV.
Conclusion
This study provides the first evidence of links between sexuality-based minority stressors and IPV for partnered MSM in two African countries – Namibia and South Africa. While levels of IPV were low and may be under-reported, at least one-in-ten men reported experiencing IPV in their current relationship. The role of stigma, stress and maladaptive coping behaviors (i.e. binge drinking) in shaping IPV points to the need for intervention across socio-ecological levels. Structural interventions that tackle LGBT human rights and legal protection have the potential to reduce stress and improve relationship quality. Screening for IPV should be encouraged during routine HIV/STI testing and counseling, along with IPV prevention strategies, with services targeted specifically for male couples. There is clearly a need for interventions that focus on teaching couples the skills to understand and cope with the unique stressors they experience as male couples. Dyadic interventions focusing on communication skills and stress management have the potential to significantly impact the experience of IPV. However, these should be considered within a wider range of interventions that also tackle conservative social norms towards same-sex behavior as a foundational cause of sexual minority stress and IPV.
References
Ali, P. A., Dhingra, K., & McGarry, J. (2016). A literature review of intimate partner violence and its classifications. Aggression and Violent Behavior, 31, 16–25.
Andrinopoulos, K., Hembling, J., Guardado, M. E., de Maria, H. F., Nieto, A. I., & Melendez, G. (2015). Evidence of the negative effect of sexual minority stigma on HIV testing among MSM and transgender women in San Salvador, El Salvador. AIDS and Behavior, 19(1), 60–71. https://doi.org/10.1007/s10461-014-0813-0.
Arnold, M. P., Struthers, H., McIntyre, J., & Lane, T. (2013). Contextual correlates of per partner unprotected anal intercourse rates among MSM in Soweto, South Africa. AIDS and Behavior, 17(1), 4–11. https://doi.org/10.1007/s10461-012-0324-9.
Balsam, K. F., & Szymanski, D. M. (2005). Relationship quality and domestic violence in Women's same sex relationships: The role of minority stress. Psychology of Women Quarterly, 29, 258–269.
Bartholomew, K., Regan, K. V., White, M. A., & Oram, D. (2008). Patterns of abuse in male same-sex relationships. Violence and Victims, 23(5), 617–636. https://doi.org/10.1891/0886-6708.23.5.617.
Bauermeister, J. A. (2007). It’s all about “connecting”: Reasons for drug use among latino living in the San Francisco bay area. Journal of Ethnicity in Substance Abuse, 6(1), 109–129.
Burgard, S. A., Seefeldt, K. S., & Zelner, S. (2012). Housing instability and health: Findings from the Michigan recession and recovery study. Social Science & Medicine, 75(12), 2215–2224.
Capaldi, D. M., Kim, H. K., & Shortt, J. W. (2007). Observed initiation and reciprocity of physical aggression in young, at-risk couples. Journal of Family Violence, 22, 101–111.
Carvalho, A. F., Lewis, R. J., Derlega, V. J., Winstead, B. A., & Viggiano, C. (2011). Internalized sexual minority stressors and same-sex intimate partner violence. Journal of Family Violence, 26(7), 501–509. https://doi.org/10.1007/s10896-011-9384-2.
CDC in Namibia. US Department of Health and Human Services. (2020). https://www.cdc.gov/globalhealth/countries/namibia/pdf/Namibia_FactSheet.pdf. Accessed 5 May 2020
Choi, K. H., Hudes, E. S., & Steward, W. T. (2008). Social discrimination, concurrent sexual partnerships, and hiv risk among men who have sex with men in Shanghai, China. AIDS and Behavior, 12, 71–77. https://doi.org/10.1007/s10461-008-9394-0.
Craft, S. M., & Serovich, J. M. (2005). Family-of-origin factors and partner violence in the intimate relationships of gay men who are HIV positive. Journal of Interpersonal Violence, 20(7), 777–791. https://doi.org/10.1177/0886260505277101.
der Pol, V., Reygan, F., Gumede, N., Essack, Z., & van Rooyen, H. (2018). A situational analysis and critical review of sexual health and HIV services for men who have sex with men (MSM) in eastern and southern Africa: Final report. Sweetwaters: HSRC.
Eaton, L. A., Pitpotam, E. V., Kalichman, S. C., Sikkena, K. J., Skinner, D., Wat, M. H., & Pieterse, D. (2013). Men who report recent male and female sex Partners in Cape Town, South Africa: An understudied and underserved population. Archives of Sexual Behavior, 42(7), 1299–1308 http://apps.who.int/iris/bitstream/10665/77432/1/WHO_RHR_12.36_eng.pdf. Accessed 5 May 2020
Edwards, K. M., & Sylaska, K. M. (2012). The perpetration of intimate partner violence among LGBTQ college youth: The role of minority stress. Journal of Youth and Adolescence, 42(11), 1721–1731.
Feldman, M. B., Ream, G. L., Díaz, R. M., & El-Bassel, N. (2008). Intimate partner violence and HIV sexual risk behavior among Latino gay and bisexual men: The role of situational factors. Journal of LGBT Health Research, 3(4), 75–87. https://doi.org/10.1080/15574090802226618.
Finneran, C., & Stephenson, R. (2013). Intimate partner violence among men who have sex with men: A systematic review. Trauma Violence Abuse, 14(2), 168–185. https://doi.org/10.1177/1524838012470034.
Finneran, C., Chard, A., & Stephenson, R. (2012). Intimate partner violence and social pressure among gay men in six countries. The Western Journal of Emergency Medicine, 13(3), 260–271.
Folch, C., Esteve, A., Zaragoza, K., Munoz, R., & Casabona, J. (2010). Correlates of intensive alcohol and drug use in men who have sex with men in Catalonia, Spain. The European Journal of Public Health, 20, 139–145.
Frost, D. M., & Meyer, I. (2009). Internalized homophobia and relationship quality among lesbians, gay men, and bisexuals. Journal of Counseling Psychology, 56(1), 91–109.
Goldenberg, T., Stephenson, R., Freeland, R., Finneran, C., & Hadley, C. (2016). 'Struggling to be the alpha': Sources of tension and intimate partner violence in same-sex relationships between men. Culture, Health & Sexuality, 18(8), 875–889.
Greenwood, G. L., Relf, M. V., Huang, B., Pollack, L. M., Canchola, J. A., & Catania, J. A. (2002). Battering victimization among a probability-based sample of men who have sex with men. American Journal of Public Health, 92(12), 1964–1969.
Ha, H., Risser, J. M., Ross, M. W., Huynh, N. T., & Nguyen, H. T. (2015). Homosexuality-related stigma and sexual risk behaviours among men who have sex with men in Hanoi, Vietnam. Archives of Sexual Behavior, 44, 349–356.
Heckathorn, D. (1997). Respondent driven sampling: A new approach to the study of hidden populations. Social Problems, 44(2), 174–199.
Hernandez-Romieu, A. C., Sullivan, P. S., Sanchez, T. H., Kelley, C. F., Peterson, J. L., del Rio, C., Salazar, L. F., Frew, P. M., & Rosenberg, E. S. (2014). The comparability of men who have sex with men recruited from venue-time-space sampling and Facebook: A cohort study. JMIR Research Protocols, 3(3), e37.
Houston, E., & McKirnan, D. J. (2007). Intimate partner abuse among gay and bisexual men: Risk correlates and health outcomes. Journal of Urban Health, 84(5), 681–690.
Humeniuk, R., Ali, R., Babor, T. F., Farrell, M., Formigoni, M. L., Jittiwutikarn, J., de Lacerda, R. B., Ling, W., Marsden, J., Monteiro, M., Nhiwatiwa, S., Pal, H., Poznyak, V., & Simon, S. (Jun 2008). Validation of the alcohol, smoking and substance involvement screening test (ASSIST). Addiction., 103(6), 1039–1047.
Hunt, C. J., Fasoli, F., Carnaghi, A., & Cadinu, M. (2016). Masculine self-presentation and distancing from femininity in gay men: An experimental examination of the role of masculinity threat. Psychology of Men & Masculinity, 17(1), 108–112. https://doi.org/10.1037/a0039545.
Kalokhe, A. S., Paranjape, A., Bell, C. E., Cardenas, G. A., Kuper, T., Metsch, L. R., & del Rio, C. (2012). Intimate partner violence among HIV-infected crack cocaine users. AIDS Patient Care and STDs, 26(4), 234–240.
Koblin, B. A., Torian, L., Xu, G., Guilin, V., Makki, H., Mackellar, D., & Valleroy, L. (2006). Violence and HIV-related risk among young men who have sex with men. AIDS Care, 18(8), 961–967. https://doi.org/10.1080/09540120500467182.
Levinger, G., & Pietromonaco, P. (1989). `a measure of perceived conflict resolution styles in Relationships', unpublished manuscript. Boston: University of Massachusetts.
Lewis, R. J., Mason, T. B., Winstead, B. A., & Kelley, M. L. (2017). Empirical investigation of a model of sexual minority specific and general risk factors for intimate partner violence among lesbian women. Psychology of Violence, 7(1), 110–119.
Liu, H., Feng, T., Rhodes, A. G., & Liu, H. (2009). Assessment of the Chinese version of HIV and homosexuality related stigma scales. Sexually Transmitted Infections, 85, 65–69.
McCarty-Caplan, D., Jantz, I., & Swartz, J. (2014). MSM and drug use: A latent class analysis of drug use and related sexual risk behaviours. AIDS and Behavior, 18(7), 1339–1351.
Messerschmidt, J. W. (2000). Becoming “real men”: Adolescent masculinity challenges and sexual violence. Men and Masculinities, 2(3), 286–307.
Meyer, I. (1995). Minority stress and mental health in gay men. Journal of Health and Social Behavior, 36(1), 38–56.
Meyer, I. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697.
Moore, T. M., & Stuart, G. L. (2005). A review of the literature on masculinity and partner violence. Psychology of Men & Masculinity, 6(1), 46–61.
Osinde, M., Kaye, D. K., & Kakaire, O. (2011). Intimate partner violence among women with HIV infection in rural Uganda: Critical implications for policy and practice. BMC Women's Health, 11(50), 1–7.
Ottonson, D. (2007). State homophobia: A world survey of laws prohibiting same sex activity between consenting adults. Stockholm: Soderton University.
Pantalone, D. W., Schneider, K. L., Valentine, S. E., & Simoni, J. M. (2012). Investigating partner abuse among HIV-positive men who have sex with men. AIDS and Behavior, 16(4), 1031–1043. https://doi.org/10.1007/s10461-011-0011-2.
Peacock, E., Andrinopoulos, K., & Hembling, J. (2015). Binge drinking among men who have sex with men and transgender women in San Salvador: Correlates and sexual health implications. Journal of Urban Health, 92, 701–716.
Pruitt, K. L., White, D., Mitchell, J. W., & Stephenson, R. (2015). Sexual agreements and intimate-partner violence among male couples. International Journal of Sexual Health, 27(4), 429–441. https://doi.org/10.1080/19317611.2015.1037037.
Radloff, L. S. (1977). CES-D scale: A self report depression scale for research in the general populations. Applied Psychological Measurement, 1, 385–401.
Relf, M. V. (2001). Battering and HIV in men who have sex with men: A critique and synthesis of the literature. Journal of the Association of Nurses in AIDS Care, 12(3), 41–48. https://doi.org/10.1016/s1055-3290(06)60143-x.
Rusbult, C. E., Martz, J. M., & Agnew, C. R. (1998). The investment model scale: Measuring commitment level, satisfaction level, quality of alternatives, and investment size. Personal Relationships, 5, 357–391.
Saunders, J., Aasland, O., Babor, T. F., de la Fuente, J., & Grant, M. (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption--II. Addiction., 88(6), 791–804.
Smolenski, D. J., Diamond, P. M., Ross, M. W., & Rosser, B. R. S. (2010). Revision, criterion validity, and multigroup assessment of the reactions to homosexuality scale. Journal of Personality Assessment, 92(6), 568–576.
Spanier, G. B. (1976). Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family, 38, 15–28.
Stachowski, C., & Stephenson, R. (2015). Homophobia and communal coping for HIV risk management among gay men in relationships. Archives of Sexual Behavior, 44(2), 467–474.
Statistics South Africa. Mid-Year Estimates (2018). Statistical release P0302. Statistics South Africa. https://www.statssa.gov.za/publications/P0302/P03022018.pdf/. Accessed 5 May 2020
Stephenson, R., & Finneran, C. (2013a). The IPV-GBM scale: A new scale to measure intimate partner violence among gay and bisexual men. PLoS One, 8(6), e62592. https://doi.org/10.1371/journal.pone.0062592.
Stephenson, R., & Finneran, C. (2013b). The IPV-GBM scale: A new scale to measure intimate partner violence among gay and bisexual men. PLoS One, 8(6), e62592.
Stephenson, R., & Finneran, C. (2017). Minority stress and intimate partner violence among gay and bisexual men in Atlanta. American Journal of Men's Health, 11(4), 952–961.
Stephenson, R., & Finneran, C. (2017a). Receipt and perpetration of intimate partner violence and Condomless anal intercourse among gay and bisexual men in Atlanta. AIDS and Behavior, 21(8), 2253–2260. https://doi.org/10.1007/s10461-017-1709-6/.
Stephenson, R., & Finneran, C. (2017b). Minority stress and intimate partner violence among gay and bisexual men in Atlanta. American Journal of Men's Health, 11(4), 952–961.
Stephenson, R., Khosropour, C., & Sullivan, P. (2010). Reporting of intimate partner violence among men who have sex with men in an online survey. The Western Journal of Emergency Medicine, 11(3), 5.
Stephenson, R., de Voux, A., & Sullivan, P. S. (2011a). Intimate partner violence and sexual risk-taking among men who have sex with men in South Africa. The Western Journal of Emergency Medicine, 12(3), 343–347.
Stephenson, R., Rentsch, C., Salazar, L. F., & Sullivan, P. S. (2011b). Dyadic characteristics and intimate partner violence among men who have sex with men. The Western Journal of Emergency Medicine, 12(3), 324–332.
United Nations Population Fund (2015). Implementing comprehensive HIV-STI programmes MSM: Practical guidance for collaborative interventions; 2014. http://www.unfpa.org/sites/default/files/pub-pdf/MSMIT_for_Web.pdf. Accessed 5 May 2020
Welles, S. L., Corbin, T. J., Rich, J. A., Reed, E., & Raj, A. (2011). Intimate partner violence among men having sex with men, women, or both: Early-life sexual and physical abuse as antecedents. Journal of Community Health, 36(3), 477–485. https://doi.org/10.1007/s10900-010-9331-9.
World Health Organization (2012). Understanding and addressing violence against women. Geneva: World Health Organization. Available at. https://www.who.int/reproductivehealth/topics/violence/vaw_series/en/. Accessed 30 Apr 2020.
Zhang, H., Teng, T., Lu, H., Zhao, Y., Liu, H., Yin, L., … Vermund, S. H. (2016). Poppers use and risky sexual behaviours among men who have sex with men in Beijing, China. Drug and Alcohol Dependence, 160, 42–48.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stephenson, R., Darbes, L.A., Chavanduka, T. et al. Intimate Partner Violence among Male Couples in South Africa and Namibia. J Fam Viol 37, 395–405 (2022). https://doi.org/10.1007/s10896-020-00214-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10896-020-00214-9