Abstract
Although intimate partner violence (IPV) is a particularly prevalent public health concern among Latina populations, the evidence-based treatment options for Latinas who experience IPV are limited. The present study tested the efficacy of the Moms’ Empowerment Program (MEP), an intervention for Spanish-speaking Latina mothers who had recently experienced IPV. Participants (N = 95) were assigned to a Treatment (n = 55) or a waitlist Control (n = 40) condition, and those in the Treatment group completed a 10-week intervention designed to address the problems associated with IPV. Intent-to-treat analyses using multiple regression revealed that Latinas’ participation in the MEP was associated with reductions in IPV exposure. These findings provide preliminary evidence that the MEP may reduce exposure to physical violence among Spanish-speaking Latinas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Intimate partner violence (IPV), defined as the use of physical or sexual violence, stalking, or psychological aggression by a spouse, dating partner, or ongoing sexual partner, affects millions of men and women across the United States each year (Breiding et al. 2015). Nearly one-third of American women—over 38 million women—experience slapping, pushing, shoving, hitting, kicking, beating, choking, burning, or having a weapon used against them by an intimate partner in their lifetime (Breiding et al. 2014). Although men and women experience IPV at similar rates, women are more likely to be exposed to severe forms of violence (e.g., beating, choking, burning, use of a knife or gun) inflicted by a partner than are men, and one in five American women will experience severe IPV at some point in their lives (Ansara and Hindin 2010; Breiding et al. 2014).
Because the violence experienced by women tends to be more severe, women are at greater risk than men of experiencing IPV-related injuries, fatalities, and adverse mental health consequences as a result of IPV (Ansara and Hindin 2010; Straus 2011). Thousands of women are killed each year at the hand of an intimate partner, and nonfatal IPV has lifelong consequences for those who are exposed, including depression, anxiety, traumatic stress, and increased physical health problems (Ellsberg et al. 2008; Lilly and Graham-Bermann 2009). In a study comparing health care costs between women with ongoing, recent, remote, or no histories of IPV, Bonomi and colleagues (2009b) found that health care costs for women with ongoing IPV were 42 percent higher than women with no abuse history. Notably, health care costs for women with remote histories of IPV—that is, having experienced IPV over 5 years prior to the study—were also significantly higher (19 percent) than women with no history of IPV, indicating that the adverse effects of IPV on women’s physical and emotional health are enduring (Bonomi et al. 2009b). Rivara and colleagues (2007) estimated that the excess health care costs attributable to IPV amount to over 19 million dollars for every 100,000 women in the United States. Given these great costs to both women and society, it is clear that IPV represents a national public health concern.
The Consequences of Repeated IPV Exposure
In addition to the severity of IPV experienced by women, the chronicity of IPV is equally alarming. Studies have shown that over 90 percent of women exposed to one incident of IPV have experienced other abuse by the same perpetrator at another point in time (Thompson et al. 2003). Results from the National Violence Against Women Survey revealed that women raped by an intimate partner experienced an average of nearly five rapes by the same perpetrator, and that women who experienced physical IPV had been assaulted by the same partner an average of nearly seven times. Among those victimized multiple times by the same perpetrator, approximately 70% reported that the abuse occurred for longer than 1 year (Tjaden and Thoennes 2000). In another study of women experiencing IPV, the average length of their violent relationship was 10 years (Graham-Bermann and Miller-Graff 2015). Further, a large survey of IPV-exposed women showed that nearly half had experienced more than one type of violence (e.g., physical and sexual assault), 21% had been abused by multiple partners, and as many as 13% had experienced IPV for over 20 years (Thompson et al. 2006).
Multiple studies have shown the consequences of repeated exposure to IPV to be more severe than outcomes associated with isolated experiences of IPV. In a study comparing physical and mental health consequences of IPV among women experiencing chronic, repeated IPV characterized by a pattern of coercive control (intimate terrorism), and those who experienced situational IPV, Johnson and Leone (2005) found that women experiencing intimate terrorism faced more serious adverse consequences, including greater risk for injury, elevated posttraumatic stress symptoms, and higher likelihood of missing work than those who reported less chronic IPV. Repeated and prolonged exposure to IPV has been found to be associated with serious physical health problems (Staggs and Riger 2005), greater incidence of sexually transmitted infections and HIV (Fontenot et al. 2013), and dissociative symptoms (Basu et al. 2013) relative to populations with either recent, distant, or no lifetime history of IPV. Thus, decreasing women’s repeated experience of IPV is of importance not only for the women themselves, but also for the communities that serve them, as IPV increases health care and other service demands.
The implications of repeated or prolonged exposure to IPV for women and society are even greater when the women experiencing IPV are mothers. Studies have shown that couples with children are at greater risk for IPV than couples without children (Peek-Asa et al. 2017) and in the United States, an estimated 7 million children live in a home where violence has occurred in the past year (McDonald et al. 2006). Graham-Bermann and colleagues (2007) found that among children living in homes where IPV is present, 80% are direct eyewitnesses to the events. Such exposure to IPV has a number of detrimental effects on children’s development, including an increased risk for traumatic stress symptoms (Graham-Bermann and Levendosky 1998), internalizing and externalizing problems (Bair-Merritt et al. 2015; Fong et al. 2017), and adverse physical health symptoms such as asthma, allergies, and gastrointestinal issues (Graham-Bermann and Seng 2005). Thus, when mothers experience IPV, the deleterious effects of violence on their own wellbeing are compounded by the difficulties faced by their children. Mothers experiencing IPV may also have greater difficulty leaving a violent relationship, as they may be financially dependent on their partners and hesitant to expose their children to unknown or unfamiliar environments that they perceive as riskier, such as homelessness or domestic violence shelters (Meyer 2012). This suggests a clear need for interventions tailored specifically to the unique effects of IPV on mothers whose children may also be struggling as a result of IPV exposure.
IPV Among Latinas
In a study of ethnoracial variation in women’s experiences of IPV, Clark and colleagues (2016) found that Latina mothers reported significantly higher rates of all types of IPV, and severe and injurious violence in particular, relative to African-American and non-Hispanic White mothers. Although other studies have not detected greater IPV among Latinas relative to other ethnoracial groups (e.g., Breiding et al. 2014), research has consistently shown that women who identify as Latina or Hispanic experience more of the adverse consequences associated with IPV, including physical health problems, symptoms of depression and posttraumatic stress, suicidal ideation, and interference with work (Black et al. 2011; Bonomi et al. 2009a; McFarlane et al. 2005; Montalvo-Liendo et al. 2016). Researchers have suggested that these disparities may be due, in part, to sociocultural and environmental factors that limit Latinas’ access to appropriate prevention and intervention programs (Bloom et al. 2009; DiCorcia et al. 2016; Gonzalez-Guarda et al. 2011).
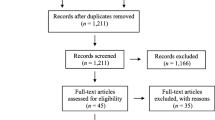
Latinas, particularly Latina immigrants, face unique barriers to healthcare and domestic violence services including social isolation, limited English proficiency, unstable residency status, and institutional discrimination (Kelly 2006; Reina and Lohman 2015). Many IPV-exposed Latinas in the United States are distant from extended family, and culturally appropriate resources are often not available to them, creating a sense of profound social isolation that is compounded for women who are financially dependent on their partners (Bauer et al. 2000). Latina mothers experiencing IPV are especially concerned with the welfare of their children and often choose not to disclose IPV to healthcare providers because they perceive intervention by institutional entities as uncontrollable, unpredictable, and likely to result in separation from their families (Kelly 2009). Women who do choose to disclose IPV often face discrimination or a lack of support from their providers. Research has shown that nearly one in three physicians view women experiencing IPV as partially responsible for the violence (Garimella et al. 2000). Latinas experiencing IPV are particularly vulnerable to such stereotyping, as ethnic minorities and patients of limited English proficiency tend to be viewed by providers as less intelligent and less educated (United States Department of Health and Human Services 2001). These barriers make it more difficult for Latinas to leave violent relationships and may exacerbate mental and physical health symptoms (Amanor-Boadu et al. 2012; Edelson et al. 2007; Torres 1991). Despite these difficulties, there are few evidence-based interventions specifically tailored to the needs of IPV-exposed Latinas (Gonzalez-Guarda et al. 2013). In fact, a systematic review intended to evaluate the effectiveness of interventions for reducing IPV among Latinas identified out of 1,274 studies screened only one randomized controlled trial (RCT) with an exclusively Latino population, described below (Alvarez et al. 2016).
Interventions to Reduce IPV Among Latinas
Among interventions developed to meet the unique needs of the Latina population who experience IPV, only one has been rigorously tested in a RCT. SEPA (Salud, Educación, Promoción y Autocuidado; “Health, Education, Promotion, and Self-Care”), a five-session group intervention covering topics ranging from sexually transmitted infection (STI) prevention, partner communication, and IPV, was developed to reduce HIV risk among Latinas in the United States. In a large RCT (N = 548) with women from the United States and several Central and South American countries (including Colombia, Cuba, Peru, and the Dominican Republic) who self-identified as Hispanic, SEPA was found to decrease risky sexual behaviors and to enhance partner communication skills, and these gains were maintained at a 12-month follow-up (Peragallo et al. 2012). Furthermore, IPV among intervention participants was significantly reduced relative to waitlist controls (i.e., participants who were offered the intervention after the conclusion of the study period) over the course of one year, and this change was mediated by participants’ improved partner communication skills (McCabe et al. 2015).
While SEPA represents an effective intervention to reduce IPV among Latinas, it was primarily developed to diminish HIV risk and was available to women with and without experiences of IPV. Thus, SEPA does not directly consider the myriad concerns unique to the experience of IPV among Latina mothers. For example, the SEPA program does not address the possible effects of IPV exposure on children in the home, and modules on identifying various types of IPV and its effects on women’s mental health and coping are absent. Further, as partner communication is a major focus in SEPA, the program may not be suitable for women who wish to leave a violent partner. IPV interventions might better serve these women by including sessions on safety planning and parenting in the context of IPV.
Other interventions that have been developed to address the unique concerns among Latinas experiencing IPV have been less rigorously tested. Kelly and Pich (2014) implemented a community-based group psychotherapy program designed to increase self-efficacy and to enhance social support among participants (N = 22). Similarly, Nicolaidis and colleagues (2013) developed Proyecto Interconexiones, a twelve-week group intervention (N = 10) with cognitive therapy and case management components aimed at reducing women’s depressive symptoms and enhancing their safety planning. While both interventions were developed specifically for Latinas who had experienced IPV, and participants in both studies demonstrated reductions in mental health symptoms at follow-up, neither included a waitlist control or comparison group. Thus, it remains unclear whether the gains made over the course of the program were an effect of the intervention, or simply due to the passage of time. Further, sample sizes for both projects were small, and IPV was not included as an outcome of either study. Consequently, the effectiveness of these interventions in enhancing women’s safety by reducing IPV remains unknown.
Although few interventions have been developed to specifically address the issue of IPV among Latina mothers, there are interventions that have been found to improve the lives of women experiencing IPV in other ethnic minority groups. For example, the Grady Nia Project (“Nia;” Kaslow et al. 2010) is a 10-session group intervention that was developed to assist suicidal African-American women experiencing IPV. In a RCT (N = 131), Kaslow and colleagues (2010) found that participation in Nia, which incorporated modules related to problem-solving, self-efficacy, and social connectedness, was associated with reductions in suicidal ideation and depressive symptoms relative to women who received treatment as usual. In another large RCT of an intervention for pregnant African-American women (N = 1,044) that emphasized women’s empowerment, safety behaviors, and advocacy, Kiely, El-Mohandes, El-Khorazaty, and Gantz (2010) found that mothers who participated in the intervention reported significantly lower rates of IPV postpartum than women receiving usual care. As both of these interventions were developed specifically for the needs of African-American women, there is evidence pointing to the effectiveness of culturally informed interventions that incorporate elements of empowerment, advocacy, social support, and safety behaviors for ethnic minority women experiencing IPV. Further, Kiely and colleagues (2010) demonstrated these effects among mothers specifically, for whom it is especially important to reduce violence given the known effects of IPV exposure on children.
The Moms’ Empowerment Program
The Moms’ Empowerment Program (MEP; Graham-Bermann 2012) is a 10-week group intervention for mothers who have recently experienced IPV and was developed to address the lack of evidence-based treatment options for this unique population. The MEP is community-based in that it was developed in partnership with community agencies and domestic violence shelters and is intended for dissemination in similar settings. It is a manualized intervention with a structured curriculum for each session, and in all empirical studies of the MEP, group facilitators receive extensive training in program implementation by the author of the MEP manual.
In keeping with prior research suggesting the efficacy of interventions emphasizing empowerment, advocacy, social support, and safety behaviors in reducing violence among other ethnic minorities, the MEP utilizes an interpersonal relationship and strengths perspective to empower women through positive reinforcement and support around psychological, practical, and emotional struggles. Thus, the program follows the Empowerment Process Model, described by Cattaneo and Goodman (2015). This model posits that self-efficacy, knowledge, competence, and action are necessary facilitating factors of empowerment, and evidence points to the effectiveness of these components in engendering positive change for women with histories of IPV (Chronister and McWhirter 2006). The MEP aims to increase women’s self-efficacy and reduce their self-blame through participation in group discussions and providing group support. The focus of the intervention is on supporting the strengths and capabilities of women to increase access to resources and to address their biopsychosocial needs, including creating increased safety for themselves and their children. Mothers’ knowledge and competence are enhanced through didactic elements of sessions that emphasize emotion regulation and conflict resolution skills. Finally, women take action toward personally meaningful, power-oriented goals by creating plans to change elements of their lives that they share with the group, and then receive support and encouragement as they implement their plans. Subsequent progress, results and barriers to success are discussed.
Because women experiencing IPV are not in control of their partners’ behavior, the MEP emphasizes women’s agency to make changes in areas of their lives that they can control, including accessing and utilizing existing social supports, prioritizing self-care, and safety planning. This study was designed to test whether the MEP would enhance the safety of Spanish-speaking women and their children by reducing mothers’ exposure to IPV. Several clinical trials provide evidence that the MEP decreases overall distress and increases the well-being of mothers in a number of ways, such as reliably reducing posttraumatic stress symptoms in African-American and White women experiencing IPV (Galano et al. 2017; Graham-Bermann and Miller 2013), relative to a waitlist no-treatment comparison group. Additional findings reveal the effectiveness of the treatment in decreasing depressive symptoms (Graham-Bermann and Miller-Graff 2015), reducing violence (Miller et al. 2014), and increasing positive parenting practices (Howell et al. 2015) in mothers. While initially developed for English-speaking populations, this program has not been implemented and evaluated with Spanish-speaking Latinas in the United States.
The Present Study
Following the review of research in this area highlighting the need for help for this high-risk group of women, and based on prior studies indicating the effectiveness of the MEP in reducing IPV among English-speaking mothers (Miller et al. 2014), the present study was intended to determine whether Spanish-speaking Latinas would similarly benefit from participation in a Spanish-language version of the program. It was hypothesized that when controlling for IPV exposure at baseline, prior to the intervention period (“Time 1”), women who participated in the MEP would report lower levels of all measured types of IPV after the 10-week intervention or wait period (“Time 2”) than those in the waitlist control group. It was further expected that Time 1 IPV exposure would interact with experimental group assignment such that women reporting higher levels of IPV exposure at Time 1 would benefit most from the intervention, experiencing the greatest reduction in IPV scores over time.
Method
Participants
Participants (N = 95) were a convenience sample of Spanish-speaking mothers who identified as Latina and who had experienced IPV within the past 2 years. Women were recruited in Texas, Michigan, and Ohio, and were of an average age of approximately 35 years (SD = 7.31). Most participants (87.5%) were immigrants, with 85.0% reporting Mexico as their country of origin and 2.5% coming from other countries in Central America. All other participants (12.5%) were from the United States. In order to protect the confidentiality and safety of participants, women were not asked to report their documentation status. Participants’ monthly income was low (M = $609.05, SD =$490.02) and the majority (89.0%) of women had not obtained education beyond high school. Women predominantly self-identified as single, divorced, or separated from their partners (82.1%), though 10.9% of participants were living with a violent partner at the time of the interview (See Table 1).
Procedures
Upon approval from the University’s Institutional Review Board, participants were recruited through flyers and brochures that advertised the study, and via referrals from agencies serving IPV-exposed women and children in each of the three intervention sites. Women recruited through flyers and brochures contacted study coordinators using a toll-free number and completed a brief phone screen to determine eligibility. All other women were recruited through referrals from community providers who offered the intervention at their agencies. In the present study, the MEP was offered in conjunction with the Kids’ Club program (Graham-Bermann 1992), a 10-week intervention for children of mothers experiencing IPV that emphasizes children’s emotion regulation, attitudes and beliefs about violence, and safety planning. Thus, women were eligible for this study if they were Spanish-speaking, had experienced IPV, and their child was between the ages of 4 and 12, the target age range for the Kids’ Club.
In total, 95 women were recruited and eligible to participate in the study. Due to the nature of the recruitment process across multiple intervention sites, the number of women who saw flyers and brochures or who were personally approached and provided with information about the study is unknown. After a sufficient number of eligible participants were recruited to form intervention groups of six to ten women, participants were sequentially assigned to treatment or waitlist control groups. This design was selected in order to reduce attrition and to decrease the time between baseline interview completion and intervention participation. The randomization procedure yielded 55 women in the Treatment condition and 40 in the Control condition. Treatment and Control groups did not significantly differ in terms of monthly income, age, immigration status, country of origin, relationship status, educational attainment, employment status, or total IPV exposure at Time 1, indicating successful implementation of sequential randomization.
Women were interviewed at two time points: prior to the 10-week intervention and immediately following the intervention or wait period. The treatment group participated in the Moms’ Empowerment Program after the Time 1 interview, while those in the waitlist control group were offered the intervention upon completion of the Time 2 interview 10 weeks later. Women provided informed consent prior to the Time 1 interview indicating awareness that the study would involve participation in an intervention program for mothers and children. Participants were informed that they may be required to wait 10 weeks to receive the intervention, and that if they were required to wait, participation in the intervention would be optional. Women were blinded to treatment condition at the time of the Time 1 interview. All participants completed structured interviews in Spanish, administered by clinical psychology graduate students and research assistants who were fluent in Spanish and trained in structured interviewing and research ethics. Interviews included questions about women’s physical and mental health, violence exposure, and demographic information and were approximately 90 minutes in duration. Women were compensated $40 for each interview. Data collection and intervention implementation occurred over the course of 2 years between 2013 and 2015.
The MEP was administered at community agencies serving Spanish-speaking families in Michigan, Texas, and Ohio, although the majority (82%) of participants were recruited in Texas. Groups were facilitated by bilingual community service providers who received extensive training from the author of the MEP manual (Graham-Bermann 2012) prior to the implementation of the intervention. Groups met at intervention sites for 1 hour weekly for ten consecutive weeks, and the content to be covered in each session was clearly described in the MEP manual. Topics ranged from parenting to self-care and safety planning, and all sessions considered culturally appropriate issues (e.g., discrimination, social isolation, and difficulties communicating with authorities). Because the purpose of the research evaluation was to determine the efficacy of a Spanish-language version of the MEP for Spanish-speaking Latina mothers, little was changed from the original format of the MEP program aside from Spanish translation. However, in a focus group study with Spanish-speaking Latinas and their care providers, Davila and colleagues (2007) found that the ideal IPV intervention for participants would use process groups with interactive activities in their preferred language and would be administered in safe locations so as not to raise the suspicions of their partners. Accordingly, MEP facilitators partnered with existing agencies that were trusted by Spanish-speaking Latinas living in the community to shape the program for the needs of each specific group of women. These partnerships were intended to foster a sense of trust between group members and facilitators, which was imperative for this study population, as the majority of mothers were immigrants to the United States. With this established sense of trust, women were empowered to share their experiences of discrimination and systemic oppression within MEP sessions, which the group members and leaders—in partnership with community stakeholders—could work together to address.
Measures
A team of researchers who were fluent in Spanish translated all measures and instructions for the Spanish language interview protocol from the original English version. Another translation team then back-translated the protocols into English. To ensure accuracy, native Spanish-speakers verified all translations prior to interview administration.
Demographic Information
Women responded to questions indicating their age, household monthly income, employment status, country of origin, educational attainment, and relationship status.
IPV
The Revised Conflict Tactics Scale (CTS2; Straus et al. 1996) was used to assess women’s experiences of IPV. This 39-item questionnaire measures exposure to various conflict tactics, and responses indicate how often each incident occurred in the past year, ranging from never to 20 times or more. Of note, responses at Time 2 were representative of violence exposure during the 10-week treatment interval as opposed to past year exposure.
Items on the CTS2 belong to one of five subscales: Physical Assault (12 items), Psychological Aggression (8 items), Sexual Coercion (7 items), Injury (6 items), and Negotiation (6 items; excluded from these analyses). Each subscale includes items representing mild or severe forms of violence (e.g., “My partner insulted or swore at me” represents mild psychological aggression, while, “My partner used a knife or gun on me” indicates severe physical assault). Thus, by summing items indicative of Mild Violence (14 items) and Severe Violence (19 items), respective subscale scores were generated. A total violence exposure score (33 items) was calculated by summing responses across all violence subscales.
In order to capture the breadth of women’s experiences of IPV, a variety scoring method was used for the items on the CTS2. Scores were calculated by coding 0 for never responses and 1 for all other endorsed items indicating exposure to violence, regardless of frequency. Thus, the maximum score for each subscale represented the number of items in the subscale (12 for Physical Assault, 8 for Psychological Aggression, 7 for Sexual Coercion, 6 for Injury, 14 for Mild, and 19 for Severe; see Table 2 for further descriptive statistics). Prior studies have established the strong reliability and validity of the CTS2 across subscales using variety scoring (Stith et al. 2000; Straus and Douglas 2004). The Spanish-language version of the CTS2 has further been found to effectively assess IPV exposure among Latinas of Mexican descent (Connelly et al. 2005). Reliability for the present study was strong (α = 0.93).
Attrition
Approximately 27.4% (n = 26) of participants were unable to be located at the 10-week follow-up. Of the participants lost to attrition, 73.1% (n = 19) were assigned to the control condition at Time 1, and women in the control condition were significantly more likely to drop out of the study relative to intervention participants, X2(1, N = 95) = 14.09, p < .001. Women who were unable to be located at the 10-week follow-up did not significantly differ from retained participants on any of the IPV exposure variables, monthly income, relationship status, educational attainment, employment status, age, or country of origin at Time 1. Further attrition analyses were conducted using logistic regression to assess interactions between experimental group assignment and monthly income, relationship status, partner residence, educational attainment, employment status, age, country of origin, intervention site, and all IPV exposure variables. These analyses provided no indications of differential attrition by treatment condition, as none of these interactions significantly predicted participant dropout.
Analytic Strategy
Multiple regression was used to determine the effect of the MEP in reducing IPV among study participants. Separate models were run to test the intervention effect for each subscale of the CTS2 (Physical Assault, Psychological Aggression, Injury, Sexual Coercion, Mild Violence, Severe Violence, and Total Exposure). Each regression model assessed the portion of the variance in Time 2 CTS2 subscale or total scores accounted for by CTS2 subscale or total scores at Time 1, the dichotomous variable indicating experimental group assignment, and an interaction term between CTS2 scores at Time 1 and experimental group assignment to assess whether the effect of the intervention depended on the extent of participants’ Time 1 IPV exposure. To determine whether there were differences in CTS2 scores at Time 2 between intervention sites, each model further included a dichotomous variable indicating the site from which participants were recruited. The intervention site variable distinguished participants recruited in Texas from those in Michigan and Ohio; the Michigan and Ohio populations were combined because the same team of researchers and clinicians collected data and administered the intervention in both states. All analyses were intent-to-treat.
Missing data were accounted for using multiple imputation, with 25 imputed datasets. Because the present study evaluated treatment effects for seven outcomes, the sequential Bonferroni-type procedure described by Benjamini and Hochberg (1995) was used to control the false discovery rate. This procedure posits that the p-value required to warrant the rejection of the null hypothesis for any given family of hypothesis tests is represented thusly:
Here, p i denotes the ordered p-value (from smallest to largest) yielded from each hypothesis test, where i indicates the ordinal position (1, 2, ..., m) of the p-value in the family of hypothesis tests and q represents the predetermined false discovery rate. For the present study, q was set to 0.05, and only those p-values meeting the above criterion were interpreted as statistically significant.
Results
CTS2 descriptive statistics indicated that scores were lower on all subscales at Time 2 relative to Time 1, and there was a fair amount of variation between scores on each subscale. There were no significant differences in CTS2 subscale scores between Treatment and Control groups at Time 1 (See Table 2).
Assessing Intervention Effects
Initial analyses using multiple regression indicated that the interaction between Time 1 IPV scores and experimental group assignment did not significantly contribute to the prediction of Time 2 IPV scores on any of the IPV exposure outcomes assessed. Accordingly, the interaction term was removed in order to accurately assess the main effect of experimental group assignment.
Total IPV Exposure
Multiple regression was used to assess the portion of variance in CTS2 Total IPV scores at Time 2 accounted for by CTS2 Total IPV scores at Time 1, experimental group assignment, and intervention site. Of these variables, experimental group assignment accounted for a significant portion of the variance in Time 2 Total IPV scores, such that Time 2 Total IPV scores for participants in the Treatment group were significantly lower than those for participants in the Control group, β = − 5.83, p = .005. Time 1 IPV scores did not contribute to the prediction of Time 2 Total IPV scores. There was an intervention site effect, such that participants in Michigan and Ohio reported lower Total IPV at Time 2 relative to participants in Texas, β = − 1.59, p < .001.
Subscale Analyses
Separate multiple regression models were used to assess the relative contributions of Time 1 subscale scores, experimental group assignment, and intervention site to the prediction of Time 2 scores on the Physical Assault, Psychological Aggression, Injury, Sexual Coercion, Mild Violence, and Severe Violence subscales of the CTS2.
After controlling for all other variables in the models, Time 1 subscale scores accounted for a significant portion of the variance in Time 2 Sexual Coercion (β = 0.18, p = .013) subscale scores only. There were site effects for Physical Assault (β = − 0.63, p < .001), Injury (β = − 0.52, p < .001), Sexual Coercion (β = − 0.41, p < .001), Mild Violence (β = − 0.60, p = .001), and Severe Violence (β = − 0.99, p < .001) subscale scores, such that participants in Michigan and Ohio received lower subscale scores at Time 2 than participants in Texas.
To test the hypothesis that intervention participation would be associated with lower CTS2 subscale scores at Time 2, the effect of experimental group assignment was tested in all regression models. These analyses revealed that after controlling for Time 1 CTS2 subscale scores and intervention site, participants in the Treatment condition reported lower levels of Physical Assault (β = − 1.95, p = .006) and Mild Violence (β = − 3.26, p = .015) at Time 2. These findings indicate that women who participated in the intervention were exposed to fewer incidents of mild violence and physical assault over the treatment interval relative to women assigned to the waitlist Control group (See Table 3).
Cohen’s d values for the Treatment group on all measured forms of IPV were larger than the corresponding Cohen’s d values for the Control group. Treatment group Cohen’s d values ranged from 0.03 to 0.35, indicating a small effect size. Control group Cohen’s d values ranged from − 0.16 to 0.04 (See Table 4).
Discussion
The results of the present study support the hypothesis that Latinas’ participation in the MEP would lead to greater reductions in IPV over time. Specifically, controlling for IPV subscale scores at Time 1 and intervention site, MEP participants reported lower Total IPV, Physical Assault, and Mild Violence scores at Time 2. These results point to the efficacy of the MEP in reducing general violence exposure, and physical assault and milder forms of violence in particular, over the 10-week treatment interval. Accordingly, this study provides evidence for the adaptability of the MEP to suit the unique needs of Spanish-speaking Latinas who experience IPV, replicating Miller and colleagues’ (2014) prior study of the efficacy of the MEP in reducing IPV among English-speaking populations.
The MEP represents a targeted, community-based treatment option available to Spanish-speaking women experiencing IPV. Prior interventions to reduce IPV among Latinas were limited in their focus and evidence base. The MEP is specifically aimed to address problems associated with IPV, while SEPA was developed with the purpose of reducing HIV risk. Thus, the MEP is the only IPV-specific, focused intervention to use waitlist control groups in order to rule out alternative explanations for violence reduction among Latinas. Previous studies, including those by Kelly and Pich (2014) and Nicolaidis and colleagues (2013), were developed to address IPV, but no waitlist control groups were utilized. Accordingly, it remains unclear whether any improvements were due to the intervention or to the passage of time alone. The descriptive statistics in the present study appear to suggest that some reductions in IPV exposure can be expected over time, emphasizing the importance of waitlist control groups in empirical studies of interventions to reduce violence against women.
After applying Benjamini and Hochberg’s (1995) sequential Bonferroni-type procedure to control the false discovery rate, the results of the present study indicated that the interaction between experimental group assignment and Time 1 IPV scores did not significantly predict Time 2 IPV scores. This was an unexpected finding, as it was hypothesized that higher baseline IPV scores would be more amenable to change over time. However, the effectiveness of the intervention regardless of the level of IPV to which women were exposed prior to participating in the MEP further underscores its utility for Spanish-speaking women with a range of IPV experiences.
These analyses further revealed intervention site effects indicating that at Time 2, women in Michigan and Ohio reported lower levels of physical assault, injurious violence, sexual coercion, mild violence, and severe violence than participants in Texas. These findings may be due to the considerable variation between Midwestern and Southern regions of the United States in terms of systemic pressures as well as the availability of safe, accessible community resources for Spanish-speaking women exposed to IPV. Further research is necessary to determine the factors that maximize the benefit of the intervention regardless of implementation site, as these effects limit the external validity of the intervention.
Limitations
While the present study provides compelling evidence in support of the efficacy of the MEP in reducing violence among Spanish-speaking Latinas, it is not without limitations. First, although intervention participants reported lower Total IPV scores at Time 2 relative to participants assigned to the Control group, this result appeared to be driven most by reductions in mild violence and physical assault. Given the well-documented associations between chronic, severe IPV exposure and functional impairment (Basu et al. 2013; Johnson and Leone 2005; Staggs and Riger 2005), it is possible that more intensive or longer-term interventions are necessary to significantly reduce experiences of severe and injurious violence. Reductions in high levels of psychological aggression may be particularly difficult to obtain, as these tactics may represent intimate terrorism, described by Johnson and Leone (2005) as a form of IPV that is especially resistant to change. It is also possible that women experiencing severe and injurious IPV at baseline are most isolated from the resources designed to assist them, and that greater reductions in their IPV exposure could be observed in a longer-term follow-up study. Further research is needed to determine the factors that promote violence reduction among women experiencing severe and injurious IPV.
Second, these results may not be generalizable to all Latina populations. Latinas are a large, diverse group in terms of Spanish language use, socioeconomic status, immigration status, and national origin. While ethnicity represents shared social, cultural, and national experiences, such identification may vary by the individual and depend on factors such as immigration status, level of acculturation, or generation of residence in the United States. The participants in this study were recruited from three states with significant Latina populations, most were immigrants of Mexican ancestry, and all used Spanish as their primary language. The experiences of and opportunities available to Latinas in other parts of the country and from other national ancestries were not included. Accordingly, the findings reported here cannot be construed as representing Latina culture.
The generalizability of the present study is further limited in that all of the women recruited for this study were mothers of school-age children. Women without children or those with younger or older children may have different experiences. Thus, results cannot be generalized to women in other settings or those living in other family configurations. This study’s external validity was also threatened by high levels of attrition. Although no factor other than experimental group assignment appeared to influence participant dropout, these results may not necessarily reflect the experiences of women who were unable to be reached for a follow-up interview.
Because the research evaluation did not include the number of MEP groups or the number of participants per MEP group in the design, this study does not rule out differential treatment outcomes by group. The MEP groups—comprised by six to ten women—are intended to be small enough to allow space for each of the women to fully participate and share their perspectives, but also large enough to provide a diversity of experiences and opinions. However, it is possible that there is an optimal group size in which women benefit most from the intervention, and further research on the MEP would do well to examine this question.
The measure used to assess IPV in this study, while representing the gold standard in the field of IPV studies, relies on the women’s self-report. The addition of other kinds of evidence for the presence of IPV would have added to the strength of this study. For example, using police reports, medical records that document injuries, as well as reports from others in the family, could provide information to further document change in IPV. Still, given the known disparities in police and medical reports, there is no assurance that these sources would provide consistent and accurate information for a sample of women experiencing IPV. This is especially true for Latinas who may be unable or unwilling to contact police following violent attacks.
Cattaneo and Goodman (2015) recommend evaluating both the process and the outcomes of empowerment programs. This study measured the outcome of the MEP program but not the process through which success was obtained. Future studies would do well to dissect elements that contribute to empowerment for individual women, such as the number of sessions attended, the extent of support received, the use of external resources, how much women felt the group contributed to attaining their goals, and the ways in which the program contents and procedures as described in the training manual were factors in their success. Such studies could include an additional control group condition in which women participate in weekly support meetings but do not receive the didactic or skills-based elements of the MEP. This type of study would allow researchers to compare the benefits of the social support provided by the MEP against its more substantive components.
While the current study represents an improvement in current knowledge by testing a program specifically designed to address the needs of women who experience IPV, and by employing a comparison group, there was high attrition from those who did not participate in the program. Attrition among Control group participants may have been due to the relatively long 10-week interval between Time 1 and Time 2 interviews. When working with populations with numerous psychosocial stressors, perhaps greater retention could be achieved by incorporating strategies to maintain regular contact with study participants, such as mailing thank-you letters and reminder cards with invitations and incentives to update their contact information when necessary. Further studies with high-risk populations would do well to utilize such techniques to facilitate retention.
The internal validity of the study was further threatened by the experimental design, as participants were sequentially assigned to treatment conditions. Without perfect random assignment, one cannot rule out confounding variables that may have affected the results. Still, by comparing women who participated in the MEP to the waitlist control this study showed changes associated with participation in the program rather than just the passage of time, as was the case in several previously reported evaluation studies. Future research might employ a design that compares different types of treatment, including the MEP, for Latinas experiencing IPV in order to produce information on which kinds of therapy would best assist them.
Finally, the present study lacks a longer-term follow-up. Only two waves of data were available for analyses. This was due in part to the needs and policies of agencies serving these women and to the project investigators’ recognizing the clinical need to provide services as soon as possible to this high-risk group of women. Thus, all women in the comparison group were invited to participate in the MEP program immediately following their second interview. Still, results show that over 10 weeks, the intervention was successful in reducing violence for MEP participants.
Clinical Implications and Future Directions
This study demonstrated that the MEP is able to significantly reduce Latinas’ exposure to IPV, relative to a control group. Given the high rates of IPV among Latinas, as well as the dearth of resources for Latinas who experience IPV, these findings have important implications for treatment and intervention with IPV-exposed women. Specifically, the MEP is an economic and culturally sensitive treatment choice that is also able to reduce IPV for participants. Additionally, the MEP is appropriate for use both in clinic and community settings, making it a highly flexible and portable manualized treatment. Thus, it appears to be a good, reliable tool for intervening in the highly prevalent, problematic issue of IPV among Latinas.
Although this study provides evidence that the MEP is adaptable to multiple treatment settings and populations, further research could be done to assess the features of the MEP that facilitate reductions in IPV exposure. Through this work, perhaps the scalability of the intervention could be improved by distilling the components of the MEP to those that promote the most change. Using only these elements, a briefer version could be implemented in treatment settings with more limited resources, as is the case for many community agencies serving Latina mothers.
Future work should also aim to be more nuanced in its approach to culturally adaptive programs. Though this study represents a strong first step, it is well known that the category of Latina actually encompasses women of varying cultural backgrounds. Thus, culturally sensitive intervention research should be mindful of this and tailor intervention work appropriately. Future research in this area should also examine the long-term effects of treatment. As research has demonstrated that IPV is generally a chronic experience, it is important to understand the long-term impact of brief intervention on the trajectory of IPV exposure, an area where there is currently little research. In doing so, researchers in the field will make meaningful strides toward reducing this significant public health issue.
References
Alvarez, C. P., Davidson, P. M., Fleming, C., & Glass, N. (2016). Elements of effective interventions for addressing intimate partner violence in Latina women: a systemic review. PLoS One, 11, e0160518.
Amanor-Boadu, Y., Messing, J. T., Stith, S. M., Sullivan, C. S., & Campell, J. C. (2012). Immigrant and nonimmigrant women: factors that predict leaving an abusive relationship. Violence Against Women, 18, 611–633.
Ansara, D. L., & Hindin, M. J. (2010). Exploring gender differences in the patterns of intimate partner violence in Canada: a latent class approach. Journal of Epidemiology and Community Health, 64, 849–854.
Bair-Merritt, M. H., Ghazarian, S. R., Burrell, L., Crowne, S. S., McFarlane, E., & Duggan, A. K. (2015). Understanding how intimate partner violence impacts school age children’s internalizing and externalizing problem behaviors: a secondary analysis of Hawaii Healthy Start program evaluation data. Journal of Child & Adolescent Trauma, 8, 245–251.
Basu, A., Levendosky, A. A., & Lonstein, J. S. (2013). Trauma sequelae and cortisol levels in women exposed to intimate partner violence. Psychodynamic Psychiatry, 41, 247–276.
Bauer, H. M., Rodriguez, M. A., Quiroga, S. S., & Flores-Ortiz, Y. G. (2000). Barriers to health care for abused Latina and Asian immigrant women. Journal of Health Care for the Poor and Underserved, 11, 33–44.
Benjamini, Y., & Hochberg, Y. (1995). Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, 57, 289–300.
Black, M. C., Basile, K. C., Breiding, M. J., Smith, S. G., Walters, M. L., Merrick, M. T., Chen, J., & Stevens, M. R. (2011). The National Intimate Partner and Sexual Violence Survey (NISVS): 2010 summary report. Atlanta: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention.
Bloom, T., Wagman, J., Hernandez, R., Yragui, N., Hernandez-Valdovinos, N., Dahlstrom, M., & Glass, N. (2009). Partnering with community-based organizations to reduce intimate partner violence. Hispanic Journal of Behavioral Sciences, 31, 244–257.
Bonomi, A. E., Anderson, M. L., Cannon, E. A., Slesnick, N., & Rodriguez, M. A. (2009a). Intimate partner violence in Latina and non-Latina women. American Journal of Preventative Medicine, 36, 43–48.
Bonomi, A. E., Anderson, M. L., Rivara, F. P., & Thompson, R. S. (2009b). Health care utilization and costs associated with physical and nonphysical-only intimate partner violence. Health Services Research, 44, 1052–1067.
Breiding, M. J., Smith, S. G., Basile, K. C., Walters, M. L., Chen, J., & Merrick, M. T. (2014). Prevalence and characteristics of sexual violence, stalking, and intimate partner violence victimization–national intimate partner and sexual violence survey, United States, 2011. Morbidity and Mortality Weekly Report, 63, 1–18.
Breiding, M. J., Basile, K. C., Smith, S. G., Black, M. C., & Mahendra, R. (2015). Intimate partner violence surveillance: Uniform definitions and recommended data elements,Version 2.0. Atlanta: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention.
Cattaneo, L. B., & Goodman, L. A. (2015). What is empowerment anyway? A model for domestic violence practice, research, and evaluation. Psychology of Violence, 5, 84–94.
Chronister, K. M., & McWhirter, E. H. (2006). An experimental examination of two career interventions for battered women. Journal of Counseling Psychology, 53, 151–164.
Connelly, C. D., Newton, R. R., & Aarons, G. A. (2005). A psychometric examination of English and Spanish versions of the revised conflict tactics scales. Journal of Interpersonal Violence, 20, 1560–1579.
Clark, H. M., Galano, M. M., Grogan-Kaylor, A. C., Montalvo-Liendo, N., Graham-Bermann, S. A. (2016). Ethnoracial variation in women’s exposure to intimate partner violence. Journal of Interpersonal Violence, 31, 531–552.
Davila, Y. R., Bonilla, E., Gonzalez-Ramirez, D., & Villarruel, A. M. (2007). HIV-IPV intervention: perceptions of what Latinas want and need. Hispanic Health Care International, 5, 101–108.
DiCorcia, D. J., Stein, S. F., Grogan-Kaylor, A., Galano, M. M., Clark, H. M., & Graham-Bermann, S. A. (2016). Undiagnosed depression in Spanish speaking Latina women exposed to intimate partner violence. Families in Society, 97(4), 313–320.
Edelson, M. G., Hokoda, A., & Ramos-Lira, L. (2007). Differences in effects of domestic violence between Latina and non-Latina women. Journal of Family Violence, 22, 1–10.
Ellsberg, M., Jansen, H., Heise, L., Watts, C. H., & Garcia-Moreno, C. (2008). Intimate partner violence and women’s physical and mental health in the WHO multi-country study on women’s health and domestic violence: an observational study. The Lancet, 371, 1165–1172.
Fong, V. C., Hawes, D., & Allen, J. L. (2017). A systematic review of risk and protective factors for externalizing problems in children exposed to intimate partner violence. Trauma, Violence, & Abuse. https://doi.org/10.1177/1524838017692383.
Fontenot, H. B., Fantasia, H. C., & Sutherland, M. (2013). The effects of intimate partner violence chronicity on personal- and partner-mediated sexual risk behaviors. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 42, S79-S91.
Galano, M. M., Grogan-Kaylor, A. C., Stein, S. F., Clark, H. M., & Graham-Bermann, S. A. (2017). Posttraumatic stress disorder in Latina women: examining the efficacy of the Moms’ Empowerment Program. Psychological Trauma: Theory Research Practice Policy, 9, 344–351.
Garimella, R., Plichta, S. B., Houseman, C., & Garzon, L. (2000). Physician beliefs about victims of spouse abuse and about the physician role. Journal of Women’s Health and Gender-Based Medicine, 9, 405–411.
Gonzalez-Guarda, R. M., Florom-Smith, A. L., & Thomas, T. (2011). A syndemic model of substance abuse, intimate partner violence, HIV infection, and mental health among Hispanics. Public Health Nursing, 28, 366–378.
Gonzalez-Guarda, R. M., Cummings, A. M., Becerra, M., Fernandez, M. C., & Mesa, I. (2013). Needs and preferences for the prevention of intimate partner violence among Hispanics: a community’s perspective. Journal of Primary Prevention, 34, 221–235.
Graham-Bermann, S. A. (1992). The Kids’ Club: a preventative intervention program for children of battered women. Ann Arbor: University of Michigan, Department of Psychology.
Graham-Bermann, S. A. (2012). The Moms’ Empowerment Program: a training manual. Ann Arbor: Department of Psychology, University of Michigan.
Graham-Bermann, S. A., & Levendosky, A. A. (1998). Traumatic stress symptoms of children of battered women. Journal of Interpersonal Violence, 13, 111–128.
Graham-Bermann, S. A., & Miller, L. E. (2013). Intervention to reduce traumatic stress following intimate partner violence: an efficacy trial of the Moms’ Empowerment Program (MEP). Psychodynamic Psychiatry, 41, 329–349.
Graham-Bermann, S. A., & Miller-Graff, L. E. (2015). Community-based intervention for women exposed to intimate partner violence: a randomized control trial. Journal of Family Psychology, 29(4), 537–547.
Graham-Bermann, S. A., & Seng, J. (2005). Violence exposure and traumatic stress symptoms as additional predictors of health problems in high-risk children. The Journal of Pediatrics, 146, 349–354.
Graham-Bermann, S. A., Lynch, S., Banyard, V., DeVoe, E. R., & Halabu, H. (2007). Community-based intervention for children exposed to intimate partner violence: an efficacy trial. Journal of Consulting and Clinical Psychology, 75, 199–209.
Howell, K. H., Miller, L. E., Lilly, M. M., Burlaka, V., Grogan-Kaylor, A. C., & Graham-Bermann, S. A. (2015). Strengthening positive parenting through intervention: evaluation of the Moms’ Empowerment Program for women experiencing intimate partner violence. Journal of Interpersonal Violence, 30, 232–252.
Johnson, M. P., & Leone, J. M. (2005). The differential effects of intimate terrorism and situational couple violence. Journal of Family Issues, 26, 322–349.
Kaslow, N. J., Leiner, A. S., Reviere, S., Jackson, E., Bethea, K., Bhaju, J., … Thompson, M. P. (2010). Suicidal, abused African American women’s response to a culturally informed intervention. Journal of Consulting and Clinical Psychology, 78, 449–458.
Kelly, U. (2006). “What will happen if I tell you?” Battered Latina women’s experiences of health care. Canadian Journal of Nursing Research, 38, 78–95.
Kelly, U. (2009). “I’m a mother first:” the influence of mothering in the decision-making processes of battered immigrant Latino women. Research in Nursing and Health, 32, 286–297.
Kelly, U., & Pich, K. (2014). Community-based PTSD treatment for ethnically diverse women who experienced intimate partner violence: a feasibility study. Issues in Mental Health Nursing, 35, 906–913.
Kiely, M., El-Mohandes, A. A., El-Khorazaty, M. N., & Gantz, M. G. (2010). An integrated intervention to reduce intimate partner violence in pregnancy: a randomized controlled trial. Obstetrics and Gynecology, 115, 273–283.
Lilly, M. M., & Graham-Bermann, S. A. (2009). Ethnicity and risk for symptoms of posttraumatic stress following intimate partner violence: prevalence and predictors of European American and African American women. Journal of Interpersonal Violence, 24, 3–19.
McCabe, B. E., Gonzalez-Guarda, R. M., Peragallo, N. P., & Mitrani, V. B. (2015). Mechanisms of partner violence reduction in a group HIV-risk intervention for Hispanic women. Journal of Interpersonal Violence, 1–22.
McDonald, R., Jouriles, E. N., Ramisetty-Mikler, S., Caetano, R., & Green, C. E. (2006). Estimating the number of American children living in partner-violent families. Journal of Family Psychology, 20, 137–142.
McFarlane, J., Malecha, A., Watson, K., Gist, J., Batten, E., Hall, I., & Smith, S. (2005). Intimate partner sexual assault against women: frequency, health consequences, and treatment outcomes. Journal of Obstetrics & Gynecology, 105, 99–108.
Meyer, S. (2012). Why women stay: a theoretical examination of rational choice and moral reasoning in the context of intimate partner violence. Australian & New Zealand Journal of Criminology, 45, 179–193.
Miller, L. E., Howell, K. H., & Graham-Bermann, S. A. (2014). The effect of an evidence-based intervention on women’s exposure to intimate partner violence. The American Journal of Orthopsychiatry, 84, 321–328.
Montalvo-Liendo, N., Grogan-Kaylor, A. C., & Graham-Bermann, S. A. (2016). Ethnoracial variation in depression symptoms of women exposed to intimate partner violence. Hispanic Health Care International, 14(2), 81–88.
Nicolaidis, C., Meija, A., Perez, M., Alvarado, A., Celaya-Alston, R., Quintero, Y., & Aguillon, R. (2013). Proyecto interconexiones: a pilot test of a community based depression care program for Latina violence survivors. Progress in Community Health Partnerships: Research, Education, and Action, 7, 395–401.
Peek-Asa, C., Saftlas, A. F., Wallis, A. B., Harland, K., & Dickey, P. (2017). Presence of children in the home and intimate partner violence among women seeking elective pregnancy termination. PLoS One, 12, e0186389.
Peragallo, N., Gonzalez-Guarda, R. M., McCabe, B. E., & Cianelli, R. (2012). The efficacy of an HIV risk reduction intervention for Hispanic women. AIDS Behavior, 16, 1316–1326.
Reina, A. S., & Lohman, B. J. (2015). Barriers preventing Latina immigrants from seeking advocacy services for domestic violence victims: a qualitative analysis. Journal of Family Violence, 30, 479–488.
Rivara, F. P., Anderson, M. L., Fishman, P., Bonomi, A. E., Reid, R. J., Carrell, D., & Thompson, R. S. (2007). Healthcare utilization and costs for women with a history of intimate partner violence. American Journal of Preventative Medicine, 32, 89–96.
Staggs, S. L., & Riger, S. (2005). Effects of intimate partner violence on low-income women’s health and employment. American Journal of Community Psychology, 36, 133–145.
Stith, S. M., Rosen, K. A., Busch, A. L., Lundeberg, K., & Carlton, R. P. (2000). The intergenerational transmission of spouse abuse: a meta-analysis. Journal of Marriage and Family, 62, 640–654.
Straus, M. A. (2011). Gender symmetry and mutuality in perpetration of clinical level partner violence: empirical evidence and implications for prevention and treatment. Aggression and Violent Behavior, 16, 279–288.
Straus, M. A., & Douglas, E. M. (2004). A short form of the revised conflict tactics scales, and typologies for severity and mutuality. Violence and Victims, 19, 507–520.
Straus, M. A., Hamby, S. L., Boney-McCoy, S., & Sugarman, D. B. (1996). The revised conflict tactics scales (CTS2): development and preliminary psychometric data. Journal of Family Issues, 17, 283–316.
Thompson, M. P., Saltzman, L. E., & Johnson, H. (2003). A comparison of risk factors for intimate partner violence-related injury across two national surveys on violence against women. Violence Against Women, 9, 438–457.
Thompson, R. S., Bonomi, A. E., Anderson, M., Reid, R. J., Dimer, J. A., Carrell, D., & Rivara, F. P. (2006). Intimate partner violence: prevalence, types, and chronicity in adult women. American Journal of Preventative Medicine, 30, 447–457.
Tjaden, P., & Thoennes, N. (2000). Extent, nature, and consequences of intimate partner violence: Findings from the national violence against women survey, research report. Washington, DC: National Institute of Justice.
Torres, S. (1991). A comparison of wife abuse between two cultures: perceptions, attitudes, nature, and extent. Issues in Mental Health Nursing, 12, 113–131.
United States Department of Health and Human Services. (2001). Mental health: Culture, race, and ethnicity – A supplement to mental health: A report of the surgeon general. Washington, DC.
Funding
This research was funded by the Curtis Center at the University of Michigan School of Social Work, the Blue Cross Blue Shield of Michigan Foundation, and the Office of the Provost’s third Century Global Initiative at the University of Michigan. The views expressed in this manuscript do not necessarily reflect those of the granting agency.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Clark, H.M., Grogan-Kaylor, A., Galano, M.M. et al. Reducing Intimate Partner Violence Among Latinas Through the Moms’ Empowerment Program: an Efficacy Trial. J Fam Viol 33, 257–268 (2018). https://doi.org/10.1007/s10896-018-9957-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10896-018-9957-4