Abstract
Researchers have established a link between motor and social development. Power mobility devices (PMDs) can impact the social skills of children who are unable to move independently. The purpose of this systematic review was to explore the evidence on PMD interventions on social skills outcomes of young children with disabilities (CWD) and to provide guidance for future research on PMD interventions. A systematic search was conducted using three electronic databases: PubMed/Medline, Web of Science, and Cumulative Index to Nursing and Allied Health Literature to identify relevant studies. Twelve articles met the inclusion criteria and were included for analyses. Seven studies reported a significant impact of the PMD interventions on social skills. Although theories are supporting the relation between early mobility and social skills, in this review research shows variable results about the impact of PMDs on the social skills of young CWD. The research on this topic appears to be at an early stage, suggestions for further exploration are offered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Independent mobility such as crawling and walking is a significant contributor to the development of social skills in typically developing young children (Kim et al. 2016), and researchers have established a link between motor and social development (Favazza and Siperstein 2016). Social development is dependent on children’s experience using independent mobility to explore environments, access play, and build friendships with peers on the playground, at school, and at home (Favazza et al. 2013; Thelen 2000). Proficiency in social skills increases opportunities for young children to engage in activities (Rimm-Kaufman et al. 2000). Social skills are defined as specific behaviors that result in positive social interactions and include verbal and non-verbal behaviors used for effective interpersonal communication (e.g., Gresham 1988; Gresham and Elliott 1987; Rao et al. 2008). Social functioning is another term used in this review. Social functioning is a broader concept of social skills, including social, cognitive, and verbal and nonverbal behaviors to engage in positive interpersonal interactions (Adolphs 2009; Voorman et al. 2010). Examples of social skills or social functioning are smiling, making eye contact, asking and responding to questions, engaging in positive peer and adult social interactions, and being socially independent (Rao et al. 2008).
Many young children with disabilities (CWD), including physical disabilities, have deficits and/or delays in social skills and pre-academic skills (Gehrman et al. 2014; Kim et al. 2016). Limited independent mobility may arise from orthopedic conditions (e.g., arthrogryposis), degenerative conditions that impact one’s motor abilities (e.g., muscular dystrophy), or neurological conditions (e.g., cerebral palsy; Heller 2009). Because of their limited independent mobility, children must rely on others to transfer them from one place to another, bring them toys to play with, and initiate play. As a result, delays and deficits in social development (e.g., fewer opportunities for the child to interact with others) as well as learned helplessness (e.g., low self-efficacy) may occur or be apparent in young CWD. These delays may influence early school experiences and task performance as children get older (Guerette et al. 2013). Therefore, methods for providing young CWD with increased access to their environments merit exploration.
Power mobility devices (PMDs) are one example of high-tech assistive technology and include power wheelchairs and robotic devices (e.g., modified ride-on-car, mobile robot, and Boss toy car). Researchers have demonstrated that AT devices and services can support the development of and maximize accessibility for CWD and can improve the educational outcomes of CWD (Section 601 (c)(5)(H) of IDEA 2004). PMDs can provide independent mobility for young CWD to accommodate their limitations in independent movement (e.g., crawling, walking) and trigger social and cognitive development (Becker et al. 2014). Researchers also reported that independent mobility is the major driving force for increasing peer-to-peer interactions of young CWD (Feldner et al. 2015; Ragonesi et al. 2010). As such, young CWD using PMDs can move independently without exerting much physical effort, initiate play with their peers, and interact with their environments (Kim et al. 2016). These outcomes could facilitate and enhance learning, socialization, and self-esteem, which are vital for children’s success in school. To date, literature reviews have mainly focused on the clinical implementation and experience when using PMDs; the most recent review was related to power mobility training methods for children and young adults with disabilities (Kenyon et al. 2018). No reviews specifically focused on outcomes related to the social skills of young CWD. The purpose of this review is to explore the effects of PMD interventions in promoting social skills for CWD. The review addressed the following research question: What effects do PMD interventions have on the social skills of CWD?
Method
Study Selection Criteria
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) framework (Moher et al. 2009). Studies that met all of the following inclusion criteria were included in the review: (a) study design included randomized control trials, quasi-experimental designs, pre-posttest studies, or single-case designs; (b) at least one child participant had a disability and was 6 years old or younger. This age range was chosen because research demonstrated CWD as young as 7 months of age can use power mobility devices (Lynch et al. 2009) and functional self-controlled mobility during early childhood (6 years or younger) is critical for the development of social skills and decrease the risk of developing learned helplessness and social isolation (Feldner et al. 2015; Nilsson and Nyberg 2003); (c) social skills were one of the measured outcomes of the PMD intervention; (d) the study was published in a peer-reviewed journal before January 2019; and (e) the study was published in English. Articles were excluded when (a) they were published in non-English languages and non-peer-reviewed sources such as conference proceedings, comments, letters, reviews, and dissertations; and (b) the interventions targeted only typically developing children.
Search Strategy
We performed a keyword search in PubMed/Medline, Web of Science, and Cumulative Index to Nursing and Allied Health Literature (CINAHL). The search algorithm included all possible combinations of keywords from the following four groups: (a) physical disability, developmental disability, cerebral palsy, or spinal bifida; (b) preschoolers, child, young children, kid, or toddler; (c) power mobility, power wheelchair, assistive technology, or mobility aids; and (d) social skills, communication, language, or quality of life. We screened titles and abstracts of the articles identified through the keyword search based on the study selection criteria. We retrieved the potentially relevant articles for the full-text evaluation.
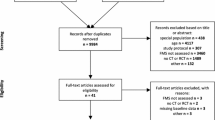
We conducted a cited reference search (i.e., forward reference search) and a reference list search (i.e., backward reference search) using the relevant articles that met the selection criteria. Next, we further evaluated and selected the articles identified through the forward/backward reference search using the same selection criteria. We identified one article through this process. We conducted a repeated reference search on all newly identified articles until no additional relevant articles were found. We found a total of 577 articles: 202 from Web of Science, 328 from PubMed, 46 from CINAHL, and 1 from forward/backward reference search. The entire search was completed by March 18, 2019 (see Fig. 1). The first author determined the inclusion or exclusion of all articles retrieved in full text. The third author checked for reliability and independently assess the selected studies based on the inclusion and exclusion criteria. Intercoder agreement across the 12 included articles was 100%.
Study selection flowchart using PRISMA framework (Moher et al. 2009)
Data Extraction and Synthesis
We used a standardized data extraction form to collect the following methodological and outcome variables from each included study: (a) author(s), publication year, and country where a study was conducted, (b) purpose of the study, (c) sample size including control and treatment groups, (d) participants’ characteristics (i.e., gender, age, and types of disabilities), (e) settings, (f) types of PMDs, (g) social skills outcomes and measures, (h) length of intervention, and (i) key findings.
Study Quality Assessment
We were using the CEC Standards for Evidence-Based Practices in Special Education (Council for Exceptional Children 2014) to assess the methodological quality of each study included in this review. The quality indicators established by CEC include both group design and single-case design and are divided into eight categories: (a) context and setting; (b) participants; (c) intervention agent; (d) description of practice; (e) implementation fidelity; (f) internal fidelity, (g) outcome measures; and (h) data analysis. According to Cook et al. (2014), a methodologically sound study must meet all of the quality indicators (i.e., group design: 24 quality indicators; single-case design: 22 quality indicators). The first and third authors independently scored each study based on these quality indicators. Intercoder agreement across the included articles averaged 89% (range: 68–100%). Disagreements were resolved through discussion to consensus. Scores for each indicator were: met (score = 1) or not met (score = 0). The possible total study score ranged from 0 to 24 for group design studies and from 0 to 22 for single-case studies. The purpose of the study quality score was to measure the strength of each study design rather than to determine the inclusion of studies. The same reliability process was performed for the methodologies and outcome variables (i.e., social skills) between first and third authors for 50% (n = 6) of the studies (the coding guide is available upon request). The intercoder agreement was 100%.
Results
Study Selection
We identified a total of 577 articles through the keyword and reference searches. We excluded 21 articles due to duplication and 533 articles at the title and abstract screening stage. We reviewed the remaining 23 articles for the full texts and excluded 11 of them because they did not meet the inclusion criteria (i.e., six were not focused on the social outcome, and five were not intervention studies). We included the remaining 12 studies (Agrawal et al. 2016; Bottos et al. 2001; Butler 1986; Deitz et al. 2002; Guerette et al. 2013; Huang and Chen 2017; Huang and Chen 2017; Huang et al. 2018a; Huang et al. 2018b; Jones et al. 2012; Logan et al. 2016; Ross et al. 2018) in this review (see Fig. 1).
Basic Characteristics of Included Studies
Table 1 reports the basic characteristics of each of the 12 articles included in the review. It includes descriptive information related to (a) purposes, (b) participants, (c) study designs and settings, and (d) types of PMDs. Table 2 summarizes the key characteristics across all selected studies, such as designs, settings, and children’s disabilities. Table 3 describes the (a) outcomes and measures, (b) length of interventions, and (c) key findings. Table 4 summarizes the key findings regarding the effects of the PMD interventions on social skills, and Table 5 summarizes the characteristics of PMDs.
Publication Year and Countries
Among the 12 eligible studies, nine (75%) were published between 2008 and 2018. The remaining studies were published between 1986 and 2002 (n = 3, 25%). Studies were conducted in three countries: South Korea, the United States, and Taiwan (see Table 1).
Study Designs and Settings
Of the 12 included studies, one study (8.4%) was a randomized controlled trial (Jones et al. 2012), seven studies (58.3%) were pre-and posttests with and without control groups (Agrawal et al. 2016; Bottos et al. 2001; Guerette et al. 2013; Huang and Chen 2017; Huang et al. 2017; Huang et al. 2018a; Huang et al. 2018b), and four studies (33.3%) were single-case designs (Butler 1986; Deitz et al. 2002; Logan et al. 2016; Ross et al. 2018). Regarding the settings in which the studies were conducted, five of the 12 interventions (41.7%) were delivered in hospitals. Three studies (25%) were conducted at participants’ homes, while two studies (8.4%) were implemented in schools. One study (8.4%) was conducted in a laboratory setting (Agrawal et al. 2016), and one study (8.4%) was conducted in mixed settings (Bottos et al. 2001).
Participants
A total of 199 children participated in the 12 studies. About 77.9% of the participants (n = 155) were between 6 months and 3 years old, and 1% of the participants (n = 2) were between 4 and 6 years old. Both mean age and range of age rather than individual ages were reported for approximately 21.1% of the participants (n = 42). The majority of the studies (80.9%) reported the gender of the participants (n = 161); males made up 47.8% of the 161 participants (n = 77), and females made up 52.2% of the 161 participants (n = 84). Participants were identified as having cerebral palsy (n = 97; 48.7%), developmental delays (n = 53; 26.6%), and Down syndrome (n = 5; 2.5%). Forty-four participants (22.2%) were identified as CWD, but the researchers did not specify the types of disabilities they had (see Table 2).
Outcome Measures
Social skills were measured by the Pediatric Evaluation of Disability Inventory (Haley et al. 1992) in four studies. The Pediatric Evaluation of Disability Inventory quantifies social functioning in children from 6 months to 7 years of age and is a parent report. Another five studies used an observation method (i.e., video recording) to measure participants’ facial expressions, initiations with others, or direct interaction with peers or adults. The remaining three studies used the revised Dimensions of Mastery Questionnaire (MacTurk et al. 1995), the Impact of Childhood Illness Scales (Hoare and Russell 1995), the Adaptive Social Behavior Inventory (Hogan et al. 1992), and the Preschool and Kindergarten Behavior Scales (Merrell 1994). See Table 3 for a list of outcomes and measures.
Social Skills Outcomes
Table 4 highlights the findings regarding the effects of PMD interventions on children’s social skills. Regarding PMDs used among the 12 eligible studies, four used power wheelchairs (Bottos et al. 2001; Butler 1986; Guerette et al. 2013; Jones et al. 2012) and eight used robotic devices including six studies using modified ride-on-cars (Huang and Chen 2017; Huang et al. 2017; Huang et al. 2018a; Huang et al. 2018b; Logan et al. 2016; Ross et al. 2018), one using a mobile robot (Agrawal et al. 2016), and the remaining one using a Boss toy car (Deitz et al. 2002). Six outcome variables were found in the selected studies that measured social skills, including (a) social functioning, (b) social persistence, (c) social participation, (d) facial expression, (e) direct peer or adult interaction, and (f) initiation of contact with others. Each variable is discussed next.
Social Functioning
Four of the 12 research studies reported significant improvements in social skills using social functioning as a variable (Agrawal et al. 2016; Guerette et al. 2013; Huang and Chen 2017; Huang et al. 2018a). Among these four studies, Huang and Chen (2017) reported that the treatment group showed significant improvements in social functioning from pre- to post-interventions, but no significant difference was found while comparing with the control group. Agrawal et al. (2016) conducted two pilot studies comparing 6-week-long and 12-week-long interventions. Their findings showed that children who participated in the 12-week intervention showed significant improvements in social functioning, but there was no significant effect on children who were in the 6-week training. Guerette et al. (2013) used the Adaptive Social Behavior Inventory (Hogan et al. 1992) and the Preschool and Kindergarten Behavior Scales (Merrell 1994) to measure social functioning. This research team used power wheelchairs and pre- and posttests without a control group in 23 CWD. Findings showed significant increases in parental perceptions of positive social skills. However, Jones et al. (2012) conducted a randomized controlled trial on a home-based intervention for 14 CWD and found no significant change in social skills.
Social Persistence
Social persistence with adults and children were measured by the revised Dimensions of Mastery Questionnaire (MacTurk et al. 1995). Huang et al. (2018b) conducted a pre- and posttests with a control group on 15 CWD and used a modified ride-on-car in a hospital setting. Results showed no significant changes in social persistence with adults and children for both the intervention and control groups.
Social Participation
Changes in social participation were measured using the Impact of Childhood Illness Scales (Hoare and Russell 1995). Bottos et al. (2001) conducted a pre- and posttests without a control group and used power wheelchairs with 29 children with cerebral palsy. No significant change was noted in the scores of the Impact of Childhood Illness Scales.
Facial Expression
Deitz et al. (2002), Huang et al. (2017), and Logan et al. (2016) used facial expressions as a proxy for social skills, which included the number of times positive facial expressions (i.e., smiling and laughing) were observed during interactions. Huang et al. (2017) used modified ride-on-cars in a group design with 10 CWD and reported more positive facial expressions. Logan et al. (2016) used modified ride-on-cars with a single-case design for three CWD and observed increased positive facial expressions. In contrast, Deitz et al. (2002) used a Boss toy car and reported no clear impact on positive affect.
Direct Peer or Adult Interaction
Direct peer or adult interaction is defined as an engagement in verbal or physical interaction with a peer or adult. Verbal, nonverbal, and physical interactions directed to and/or from target children were coded as peer interaction. Both Butler (1986) and Ross et al. (2018) used single-case designs. Butler (1986) used power wheelchairs with six CWD, and the findings demonstrated that increased frequencies of adult interaction. However, Ross et al. (2018) used a modified ride-on-car with five CWD and reported no intervention effect on peer or adult interaction.
Initiation of Contact with Others
Child-initiated contacts with peers or adults were counted when (a) the child-initiated contact without observable prompting or initiating behavior from another person or (b) the child independently vocalized (e.g., shouting, laughing, and grunting) or physically pointed at or touched another person, indicating that he or she wanted something. Deitz et al. (2002) conducted a single-case design and used a Boss toy car with two children with complex developmental delays. They observed an increased number of initiations with adults, whereas Huang et al. (2017) reported that no significant change was found in 15 CWD compared with a control group.
PMD Interventions
Among the 12 eligible studies, eight used robotic devices including six studies using modified ride-on-cars (50%), one using a mobile robot (8.3%), and the remaining one using a Boss toy car (8.3%). The remaining four studies (33.4%) used power wheelchairs (see Table 5 for the features of the modified ride-on-car, mobile robot, Boss toy car, and power wheelchairs).
Robotic Devices
Eight studies used robotic devices with participants with cerebral palsy, developmental delays, Down syndrome, or other disabilities. The mean age of the participants was 1.56 years, and the average length of intervention was 2.3 months. Among the eight studies, six of them used a modified ride-on-car, one used a mobile robot, and the remaining study used a Boss toy car to explore the impact on social skills for CWD.
Modified ride-on-car. Huang et al. (2017) conducted a 9-week modified ride-on-car intervention without a control group. Participants included 10 children with either cerebral palsy, Down syndrome, developmental delays, or other disabilities. Results showed that positive facial expressions (i.e., smiling and laughing) during interventions were significantly improved. Logan et al. (2016) examined the use of a modified ride-on-car for three young children with complex medical needs, which required a tracheotomy tube and a mechanical ventilator for breathing. The single-case design study was conducted in a hospital setting. Findings showed that the modified ride-on-car was feasible for children with complex medical needs and led to increased positive facial expressions (i.e., smiling and laughing). Ross et al. (2018) conducted a modified ride-on-car intervention using a single-case design with five young children with either cerebral palsy or Down syndrome for 11 weeks during an inclusive playgroup in school. The findings showed that children did not experience significant changes in direct peer interactions.
Huang et al. (2018a) and Huang et al. (2018b) used modified ride-on-cars combined with an adult-directed social interaction training program to support the social needs of CWD in a hospital setting. The program included three steps. First, one-on-one instruction was provided to participants regarding how to perform desired social behaviors such as greetings, gestures, and vocalizations. Second, therapists guided the participants to perform desired social behaviors while meeting people in the hallway, and therapists provided positive feedback for encouragement. Third, participants were asked to complete social interaction tasks such as sharing toys. Both studies appeared to use the same group of participants and similar interventions, but different measures were used to quantify social skills. Huang et al. (2018a) found significant improvements in social skills compared to the control group; they used the Chinese version of the Pediatric Evaluation of Disability Inventory (Chen et al. 2009) to measure social functioning. Huang et al. (2018a) showed no intervention effects on social persistence with children or adults; they used the revised Dimensions of Mastery Questionnaire (MacTurk et al. 1995). Also, Huang and Chen (2017) examined the effects of a 9-week modified ride-on-car training versus conventional therapy (i.e., physical, occupational, and speech therapy) on social functioning for 20 CWD (n = 10 in the intervention group; n = 10 in the control group). The findings showed that the treatment group demonstrated improvements in social functioning, but no significant difference was found between the two groups.
Mobile robot. Agrawal et al. (2016) used a mobile robot to study short-term (i.e., 6 weeks) and long-term (i.e., 12 weeks) effects on children with cerebral palsy in a laboratory setting. Five children with cerebral palsy participated in each intervention (n = 5 for 6 weeks and n = 5 for 12 weeks). Findings demonstrated significant improvement in social skills during the 12-week intervention but not during the 6-week intervention.
Boss toy car. Deitz et al. (2002) used a single-case design to examine the effects of a Boss toy car on the participation behaviors of two young children with complex developmental delays in school. The findings showed positive changes in initiation with others but did not have a clear impact on positive facial expressions.
Power Wheelchair
Four studies used power wheelchairs to explore their impact on the social skills of participants with cerebral palsy and other disabilities. The mean age of the participants was 3.44 years, and the average length of intervention was 6.8 months. Three of the four studies (Butler 1986; Guerette et al. 2013; Jones et al. 2012;) were conducted in homes and the fourth (Bottos et al. 2001) was in mixed settings (i.e., school and home). Jones et al. (2012) conducted a randomized controlled trial using power wheelchairs with 14 CWD in a treatment group and 14 CWD in a control group. The mean age for both sets of participants was 1.8 years, and the intervention lasted for approximately 1 year. Both Bottos et al. (2001) and Guerette et al. (2013) conducted pre- and posttests (without control groups) with children with either cerebral palsy or other orthopedic disabilities. Butler (1986) used power wheelchairs and a single-case design to evaluate the effects of a 10-day intervention on six CWD. This was the shortest intervention across all power wheelchair interventions.
Study Quality
Table 6 reports the results of the study quality assessment. The included studies on average scored 20.25 out of 24.00 possible points for group design and 15.50 out of 22.00 possible points for single-case design. Four of eight group design studies were not qualified for CEC standards because these studies have no comparison groups. All 8 studies provide sufficient information regarding the setting, participants, description of practice (intervention), and data analysis. In contrast, none of the reviewed studies reported implementation fidelity. Only two research teams reported internal reliability, inter-observer reliability, or test-retest reliability. None of the reviewed single-case design studies controlled for the common threats to internal validity and provided at least three demonstrations of experimental effects at three different times.
Discussion
The purpose of this review was to explore the existing evidence on the effects of PMD interventions on the social skills for young CWD. Twelve peer-reviewed studies met the inclusion criteria and were included in this review. Six studies reported significant impacts of the PMD interventions on social skills, but an insufficient agreement can be drawn about the impact of PMDs on the social skills of young CWD. The research in this area appears to be at an early stage which agrees with the findings from Livingstone and Field (2014) on power mobility outcomes for individuals with mobility delays or disabilities. Thus, supplementing PMD interventions with evidence-based social skills intervention is recommended until future research provides evidence on the effects of PMD interventions on social skills.
Age is an important factor for PMD interventions. Typically developing children develop reaching and rolling (3–4 months), crawling (7–9 months), and walking (12–13 months) to enable them to explore their surroundings, with resultant changes in cognitive and social behavior. Using PMD interventions at similar ages (developing milestones) is recommended for CWD to accommodate their limited mobilities and facilitate the development of other domains such as social and cognition (Rosen et al. 2009). Regarding the age of young CWD who participated in PMD interventions, it tends to differ by the type of PMD used, which may also relate to the duration of PMD interventions. In this review, the average age of the 44 participants who used the robotic devices in eight studies (Agrawal et al. 2016; Deitz et al. 2002; Huang and Chen 2017; Huang et al. 2017; Huang et al. 2018a; Huang et al. 2018b; Logan et al. 2016; Ross et al. 2018) was 1.47 years, and their ages ranged from 0.5 to 5.8 years. On the other hand, the average age of participants in the four studies using power wheelchairs was 3.44 years (range: 1.2–8.0 years old) (see Table 4 for the characteristics of the groups). Thus, the age of participants tends to be younger in robotic device interventions than in power wheelchair interventions. In addition, the average intervention duration for robotic devices and power wheelchairs were 9.2 weeks (range: 9–14 weeks) and 27.2 weeks (range: 10 days-48 weeks), respectively. The length of intervention tends to be shorter for robotic device interventions compared to power wheelchair interventions. One of the possible reasons for this difference is that children might learn how to drive robotic devices more quickly than they can learn how to drive a power wheelchair (Lynch et al. 2009). Allegretti et al. (2018) claim that children require significant time to develop proficiency in driving power wheelchairs, and Jones et al. (2012) reported that seven of the 11 participants in their study had not mastered all the power wheelchair’s driving skills after participating in an intervention program for a year. However, there is no general agreement on what type of PMD intervention protocol or training method positively impacts the social skills of CWD.
There were some noticeable variations across the 12 studies, which made it difficult to compare the outcomes and effects of the studies. First, the measures of social outcomes were highly varied. Five studies used observation methods to quantify social skills, and three different measures were used (i.e., facial expression, direct peer and adult interaction, social initiations). Seven studies used standardized assessment tools to quantify the impact of PMDs on social skills. Among those seven studies, three used different outcome measures (i.e., the revised Dimensions of Mastery Questionnaire, the Adaptive Social Behavior Inventory, the Pediatric Evaluation of Disability Inventory, and the Impact of Childhood Illness Scales). In fact, only four of the 12 studies used the same outcome measure (i.e., the Pediatric Evaluation of Disability Inventory) to quantify social skills, which made it difficult to compare the outcomes and effects of the studies. Second, none of the studies reported or assessed implementation fidelity to ensure that the interventions were conducted as planned, based on the evaluation of the CEC’s quality indicators. Implementation fidelity plays an important role in the effect of interventions and children’s outcomes (Cook and Odom 2013; Fixsen et al. 2009). Low fidelity of implementation might negatively affect the degree of change in outcomes (Davidson et al. 2009; Strain and Bovey 2011), and future researchers should consider measuring and then reporting implementation fidelity in their dissemination activities.
Limitations and Implications
Several limitations exist in this literature review. First, this review focused mainly on social skills outcomes, which is only one of several key measures of PMD intervention. This focus might not provide a broad overview of the impact of PMD interventions on young CWD. Future researchers might explore the impact of PMD on other school readiness domains such as cognition or communication. Second, this review excluded qualitative studies related to the children’s, families’, and therapists’ perspectives on PMD interventions. Excluded studies may provide qualitative information related to the impact of PMD interventions on social skills outcomes. Future reviews might include different types of research designs to better understand the impact of PMD interventions. Third, the review focused on studies with young children (6 years old and younger) and, therefore, the results are for this specific age group and it is possible that including studies with children in different age groups would reveal different findings. Finally, reliability was assessed only for the final identified 12 studies and not during the screening process, future reviews should include reliability measures for each step in the search and screening process.
Additional limitations are related to the studies included. First, none of the 12 studies met all quality standards and this limits the ability to interpret and evaluate the findings. Because rigorous studies are needed to demonstrate the value of PMD interventions, future studies should use quality indicators and standards to allow a careful evaluation of the impact of PMD interventions on young CWD. Second, half of the reviewed studies were conducted in laboratory and hospital settings. Learning to use a PMD is a long and complex process that requires determination, practice, and family support (Kenyon et al. 2018). Natural environments (e.g., home and school) provide children with more frequent opportunities to practice, which may help children learn to use PMDs and simultaneously promote participation and peer interaction. Future studies might consider using the natural environments as a context to examine the impact of PMD interventions.
There was no adverse report on social skills, and five studies reported significant impacts on social skills in this review, suggesting that PMD interventions might have a potentially positive impact on social skills of young CWD. However, the current literature is limited by the number of studies that specifically measured social skills outcomes, the wide ranges of measures used in the identified studies, and the rigor of the identified studies. The research on this topic appears to be at an early stage and additional studies are needed.
References
Adolphs, R. (2009). The social bra neural basis of social knowledge. Annual Review of Psychology, 60(1), 693–716. 10.1146/ annurev.,psych. 60.110707.163514.
Agrawal, S. K., Kang, J., Chen, X., Kim, M. J., Lee, Y., Kong, S. W., et al. (2016). Robot-enhanced mobility training of children with cerebral palsy: Short-term and long-term pilot studies. IEEE Systems Journal, 10(3), 1098–1106.
Allegretti, A., Barnes, K., Berndt, A. (2018). Impact of use of a ride-on toy car by children with mobility impairment. American Journal of Occupational Therapy, 72(4), 1, 1-10.
Becker, D. R., McClelland, M. M., Loprinzi, P., & Trost, S. G. (2014). Physical activity, self-regulation, and early academic achievement in preschool children. Early Education & Development, 25(1), 56–70.
Bottos, M., Bolcati, C., Sciuto, L., Ruggeri, C., & Feliciangeli, A. (2001). Powered wheelchairs and independence in young children with tetraplegia. Developmental Medicine & Child Neurology, 43, 769–777.
Butler, C. (1986). Effects of powered mobility on self-initiated behaviors of very young children with locomotor disability. Developmental Medicine & Child Neurology, 28, 325–332.
Chen, K. L., Hsieh, C. L., Sheu, C. F., Hu, F. C., & Tseng, M. H. (2009). Reliability and validity of a Chinese version of the pediatric evaluation of disability inventory in children with cerebral palsy. Journal of Rehabilitation Medicine, 41(4), 273–278.
Cook, B. G., Buysse, V., Klinger, J., Landrum, T. J., McWilliam, R. A., Tankersley, M., & Test, D. W. (2014). CEC’s standards for classifying the evidence base of practices in special education. Remedial and Special Education, 36, 220–234.
Cook, B. G., & Odom, S. L. (2013). Evidence-based practices and implementation science in special education. Exceptional Children, 79, 135–144.
Council for Exceptional Children. (2014). Council for Exceptional Children standards for evidence-based practices in special education. Retrieved from: http://www.cec.sped.org/~/media/Files/Standards/Evidence%20based%20Practices%20and%20Practice/CECs%20Evidence%20Based%20Practice%20Standards.pdf.
Davidson, M. R., Fields, M. K., & Yang, J. (2009). A randomized trial study of a preschool literacy curriculum: The importance of implementation. Journal of Research on Educational Effectiveness, 2, 177–208.
Deitz, J., Swinth, Y., & White, O. (2002). Powered mobility and preschoolers with complex developmental delays. The American Journal of Occupational Therapy, 56(1), 86–96.
Favazza, P. C., & Siperstein, G. N. (2016). Motor skill acquisition for young children with disabilities. In B. Reichow, B. A. Boyd, E. E. Barton, & S. L. Odom (Eds.), Handbook of early childhood special education (pp. 225–245). Switzerland: Springer.
Favazza, P. C., Siperstein, G. N., Zeisel, S. A., Odom, S. L., Sideris, J. H., & Moskowitz, A. L. (2013). Young athletes program: Impact on motor development. Adapted Physical Activity Quarterly, 30(3), 235–253.
Feldner, H. A., Logan, S. W., & Galloway, J. C. (2015). Why the time is right for a radical paradigm shift in early powered mobility: The role of powered mobility technology devices policy and stakeholders. Disability and Rehabilitation: Assistive Technology, 2(11), 89–102.
Fixsen, D. L., Blase, K. A., Naoom, S. F., & Wallace, F. (2009). Core implementation components. Research on Social Work Practice, 19(5), 531–540.
Gehrman, F. E., Coleman, A., Weir, K. A., Ware, R. S., & Boyd, R. N. (2014). School readiness of children with cerebral palsy. Developmental Medicine & Child Neurology, 56, 786–793.
Gresham, F. M. (1988). Social skills. In J. C. Witt, S. N. Elliott, & F. M. Gresham (Eds.), Handbook of behavior therapy in education (pp. 523–546). Boston: Springer.
Gresham, F. M., & Elliott, S. N. (1987). The relationship between adaptive behavior and social skills: Issues in definition and assessment. The Journal of Special Education, 21(1), 167–181.
Guerette, P., Furumasu, J., & Tefft, D. (2013). The positive effects of early powered mobility on children’s psychosocial and play skills. Assistive Technology, 25, 39–48.
Haley, S. M., Coster, W. J., Ludlow, L. H., Haltiwanger, J. T., & Andrellos, P. J. (1992). Pediatric evaluation of disability inventory (PEDI). Boston: Department of Rehabilitation Medicine, New England Medical Center.
Heller, K. W. (2009). Learning and behavioral characteristics of students with physical, health, or multiple disabilities. In K. W. Heller, P. E. Forney, P. A. Alberto, S. J. Best, & M. N. Swartzman (Eds.), Understanding physical, health, and multiple disabilities (2nd ed., pp. 18–34). Upper Saddle River: Pearson Education, Inc..
Hoare, P., & Russell, M. (1995). The quality of life of children with chronic epilepsy and their families: Preliminary findings with a new assessment measure. Developmental Medicine & Child Neurology, 37, 689–696.
Hogan, A. E., Scott, K. G., & Bauer, C. R. (1992). The adaptive social behavior inventory (ASBI): A new assessment of social competence in high-risk three-year-olds. Journal of Psychoeducational Assessment, 10(3), 230–239.
Huang, H. H., & Chen, C. L. (2017). The use of modified ride-on cars to maximize mobility and improve socialization: A group design. Research in Developmental Disabilities, 61, 172–180.
Huang, H. H., Chen, Y. M., & Huang, H. W. (2017). Ride-on car training for behavioral changes in mobility and socialization among young children with disabilities. Pediatric Physical Therapy, 29(3), 207–213.
Huang, H. H., Chen, Y. M., Huang, H. W., Shih, M. K., Hsieh, Y. H., & Chen, C. L. (2018a). Modified ride-on cars and young children with disabilities: Effects of combining mobility and social training. Frontiers in Pediatrics, 5, 299–308.
Huang, H. H., & Galloway, J. C. (2012). Modified ride-on toy cars for early power mobility: A technical report. Pediatric Physical Therapy, 24(2), 149–154.
Huang, H. H., Huang, H. W., Chen, Y. M., Hsieh, Y. H., Shih, M. K., & Chen, C. L. (2018b). Modified ride-on cars and mastery motivation in young children with disabilities: Effects of environmental modifications. Research in Developmental Disabilities, 83, 37–46.
Jones, M. A., McEwen, I. R., & Neas, B. R. (2012). Effects of power wheelchairs on the development and function of young children with severe motor impairments. Pediatric Physical Therapy, 24(2), 131–140.
Kenyon, L. K., Hostnik, L., McElroy, R., Peterson, C., & Farris, J. P. (2018). Power mobility training methods for children: A systematic review. Pediatric Physical Therapy, 30(1), 2–8.
Kim, H., Carlson, A. G., Curby, T. W., & Winsler, A. (2016). Relations among motor, social, and cognitive skills in pre-kindergarten children with developmental disabilities. Research in Developmental Disabilities, 53-54, 43–60.
Livingstone, R., & Field, D. (2014). Systematic review of power mobility outcomes for infants, children and adolescents with mobility limitations. Clinical Rehabilitation, 28(10), 954–964.
Logan, S. W., Feldner, H. A., Galloway, J. C., & Huang, H. H. (2016). Modified ride-on car use by children with complex medical needs. Pediatric Physical Therapy, 28(1), 100–107.
Lynch, A., Ryu, J., Agrawal, S., & Galloway, J. C. (2009). Power mobility training for a 7-month-old infant with spina bifida. Pediatric Physical Therapy, 21(4), 362–368.
MacTurk, R. H., Morgan, G. A., Jennings, K. D. (1995). The assessment of mastery motivation in infants and young children. In R. H. MacTurk, & G. A. Morgan (Vol. Eds.), Mastery motivation: Origins, conceptualizations, and applications: Vol. 12, (pp. 19–56). Norwood, NJ: Ablex Publishing Corporation.
Merrell, K. W. (1994). Preschool and kindergarten behavior scales. Austin: PRO-ED, Inc..
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine, 151(4), 264–269.
Nilsson, L. M., & Nyberg, P. J. (2003). Driving to learn: A new concept for training children with profound cognitive disabilities in a powered wheelchair. American Journal of Occupational Therapy, 57, 229–233.
Ragonesi, C. B., Chen, X., Agrawal, S., & Galloway, J. C. (2010). Power mobility and socialization in preschool: A case study of a child with cerebral palsy. Pediatric Physical Therapy, 22, 322–329.
Rao, P. A., Beidel, D. C., & Murray, M. J. (2008). Social skills interventions for children with Asperger’s syndrome or high-functioning autism: A review and recommendations. Journal of Autism and Developmental Disorders, 38(2), 353–361.
Rimm-Kaufman, S. E., Pianta, R. C., & Cox, M. J. (2000). Teachers’ judgments of problems in the transition to kindergarten. Early Childhood Research Quarterly, 15(2), 147–166.
Rosen, L., Arva, J., Furumasu, J., Harris, M., Lange, M. L., McCarthy, E., et al. (2009). RESNA position on the application of power wheelchairs for pediatric users. Assistive Technology, 21(4), 218–226.
Ross, S. M., Catena, M., Twardzik, E., Hospodar, C., Cook, E., Ayyagari, A., Inskeep, K., Sloane, B., MacDonald, M., & Logan, S. W. (2018). Feasibility of a modified ride-on car intervention on play behaviors during an inclusive playgroup. Physical & Occupational Therapy in Pediatrics, 38(5), 493–509.
Section 601(c)(5)(H) of Individuals with Disabilities Education Act of 2004. 2004 U.S. Department of Education. Retrieved from http://idea.ed.gov/explore/view/p/,root,statute,I,A,601,c,5,H.
Strain, P. S., & Bovey, E. H. (2011). Randomized, controlled trial of the LEAP model of early intervention for young children with autism spectrum disorders. Topics in Early Childhood Special Education, 31, 133–154.
Thelen, E. (2000). Grounded in the world: Developmental origins of the embodied mind. Infancy, 1, 3–28.
Voorman, J. M., Dallmeijer, A. J., Van Eck, M., Schuengel, C., & Becher, J. G. (2010). Social functioning and communication in children with cerebral palsy: Association with disease characteristics and personal and environmental factors. Developmental Medicine & Child Neurology, 52(5), 441–447. https://doi.org/10.1111/j.1469-8749.2009.03399.x.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
All authors declare that they have no conflict of interest.
Ethical Approval
No procedures performed in studies involved human participants. The manuscript includes a review of published articles.
Informed Consent
No informed consents were used because the review includes only analysis of published articles.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cheung, W.C., Meadan, H. & Yang, H.W. Effects of Powered Mobility Device Interventions on Social Skills for Children with Disabilities: A Systematic Review. J Dev Phys Disabil 32, 855–876 (2020). https://doi.org/10.1007/s10882-020-09729-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10882-020-09729-x