Abstract
Executive function (EF) skills, parent–child conflict, and high blood glucose (BG) may impact child externalizing behaviors. We examined these child and parent factors in families of 5–9 year olds with recent-onset type 1 diabetes (T1D). Parents (N = 125) reported child EF, child externalizing behaviors, and conflict regarding T1D-specific tasks. We used self-monitoring BG uploads to calculate the percentage of time children had high BG (> 180 mg/dl). We entered data into a moderated path analysis using MPlus8. The path analysis revealed a positive direct effect for parent-reported child EF and child externalizing behavior (p < .01). Further, T1D-specific conflict moderated the positive association between parent-reported child EF and child externalizing behaviors (p < .05). Early screening of child EF, externalizing behavior, and family conflict may be particularly important in the recent-onset period of T1D. The introduction of T1D-related conflict after diagnosis may impact child externalizing behavior and limited child EF skills that pre-date diagnosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Type 1 diabetes (T1D) is a common medical condition that affects approximately 167,000 children in the United States and 1.94 per 1000 children worldwide (Chiang et al., 2014; Dabelea et al., 2014). T1D is characterized by a loss of natural insulin production, a hormone necessary to regulate blood glucose. Therefore, children with T1D must rely on exogenous insulin to maintain normal glycemic levels (e.g., 72–142 mg/dl), and engage in a complex daily treatment management regimen (e.g., adequate carbohydrate intake, regular physical activity, and glucose monitoring) to maintain optimal glycemic levels. When T1D care is not closely managed, however, children are at risk for developing severe hyperglycemia (i.e., blood glucose concentration ≥ 181 mg/dl) and urgent hypoglycemia (i.e., ≤ 54 mg/dl), which may negatively impact the developing brain’s glucose utilization and affect optimal executive functioning (Cameron, 2015; Gonder-Frederick et al., 2009).
Executive functioning (EF) encompasses a set of skills (e.g., behavioral inhibition, selective attention, working memory, mental flexibility, problem solving, and planning) that develop throughout childhood and are critical for cognitive functioning, managing behavior, regulating emotions, and engaging in social interaction (Anderson, 2002; Diamond, 2013). Children who exhibit lower EF skills than their peers are more likely to display increased negative emotional responses and disruptive (i.e., externalizing) behavior (Barkley, 1997; Clark et al., 2002). Unfortunately, some evidence suggests that children with T1D may evidence more deficits in EF skills than peers without T1D (Northam et al., 2001), and these deficits associate with reduced self and parent-reported T1D treatment management (Perez et al., 2017). For example, a child with T1D and suboptimal EF may have a more difficult time cooperating with tasks that require behavioral inhibition (e.g., dosing insulin before eating), organization (e.g., remembering to keep T1D supplies on hand or keep track of a continuous glucose monitor transmitter), and short-term memory skills (e.g., recalling T1D management tasks performed earlier in the day). Further, there is evidence that T1D-specific family conflict (e.g., parent and child disagreements regarding T1D treatment management tasks and daily activities that impact glycemic levels) and under-developed child EF skills associate with suboptimal T1D treatment management and glycemic control (Bagner et al., 2007; Hilliard, Holmes, et al., 2013; Hilliard, Wu, et al., 2013; McNally et al., 2010). In addition to family conflict and suboptimal EF, behavioral issues, including externalizing behaviors (e.g., oppositionality, defiance, hyperactivity) can exacerbate problems with T1D management during school-aged years because these management tasks require child cooperation (Duke et al., 2008). Families of school-age children with T1D in particular seek clinical assistance with child externalizing behaviors because poor child cooperation can interfere with the completion of important T1D management tasks which may ultimately affect the child’s glycemic control (Cohen et al., 2004). To date, no study has sought to examine how parent–child conflict and child EF relate to child externalizing behaviors in youth with T1D, in a single model, thereby limiting our understanding of how they may relate to children at risk for suboptimal glycemic control.
In considering factors that may impact the association between EF and externalizing in children with T1D, glycemic control may play a role. This study utilized the pediatric psychology transactional model to explore how T1D-specific conflict, glycemic control, parent-reported child EF, and externalizing behavior may relate to each other. The transactional model proposes reciprocal interactions between child health and behavior, and parent characteristics and experiences (Fiese & Sameroff, 1989). In a previous study, researchers have explored how blood glucose variability (i.e., fluctuating periods of hyperglycemia and hypoglycemia) and parent stress associate with child externalizing behavior (Hilliard et al., 2011). Blood glucose variability did not emerge as a significant predictor, possibly due to findings that suggest more time in the hyperglycemic range associate with increased externalizing behavior compared to time in the hypoglycemic range (McDonnell et al., 2007; Northam et al., 2005). Here, this study seeks to conduct a novel extension of these associations by examining blood glucose values as moderators of EF and externalizing behaviors, and focusing on children aged 5–9 years with recent-onset T1D. Children aged 5–9 years with new onset T1D are at risk for declining glycemic control in the years following diagnosis (Clements et al., 2014). It may be clinically important to identify factors that can complicate glycemic control soon after diagnosis in an age group where glycemic control begins to deteriorate to identify potential early intervention targets. We also believed that it was novel to focus on children with recent-onset T1D to extend the use of the transactional model in T1D. Therefore, we tested the moderating role of T1D-specific conflict and percent of high blood glucose values on the association between child EF and child externalizing behavior in a recent-onset sample. We hypothesized that T1D-specific conflict and high blood glucose values would add unique variance and exacerbate the association between child EF and child externalizing behavior.
Methods
Participants
We recruited 131 families from two large endocrinology clinic networks in the Midwestern and Rocky Mountain regions of the U.S. to participate in a longitudinal study examining glycemic control in children aged 5 to 9 years old with recent-onset T1D. To be eligible for this study, children had to be less than 12 months from their T1D diagnosis, between 5 and 9 years old, English speaking, and on intensive insulin therapy (e.g., multiple daily injections or insulin pump). This study excluded children with a developmental delay (i.e., autism, cerebral palsy, or intellectual disability), any comorbid chronic condition (e.g., renal disease), a diagnosis of Type 2 or monogenic diabetes, and any medication use that could impact glycemic control (e.g., systemic steroids). One hundred twenty-five families completed the baseline assessment, and their data are included in the present analyses.
Procedures
The Institutional Review Boards of both participating hospitals provided ethical approval for all study procedures prior to study recruitment. A study coordinator approached eligible families during a regularly scheduled diabetes clinic visit or recruited families via telephone. A parent/legal guardian provided written informed consent for their child, and when age appropriate, children completed an assent form. Parents completed study measures on a tablet computer. Researchers used blood glucose data uploaded from children’s glucometers for the 2 weeks prior to the study visit. Parents received $30 for completing the questionnaires and each child received a toy valued at $10 for their participation.
Measures
Demographic Information
Parents reported their child’s date of birth, T1D duration, sex, race/ethnicity, treatment regimen (e.g., multiple daily injections or continuous subcutaneous insulin infusion), continuous glucose monitor use (yes or no), and any T1D-related adverse events (e.g., severe hypoglycemia, seizure) at their baseline visit. Parents also reported family income, parent employment status, and parent education level. Researchers verified medical data through electronic health record (EHR) review. Research staff noted very few discrepancies between parents’ responses to questions related to their child’s medical history (e.g., insulin regimen, continuous glucose monitor use, T1D-related adverse events) and their child’s EHR. In the few cases of a discrepancy (e.g., frequency of severe hypoglycemia), researchers used the parents’ response as families may not report these events to their child’s diabetes provider.
Blood Glucose
Families used their own blood glucose test strips and glucometers to measure their child’s blood glucose concentration throughout the day. Researchers downloaded 2 weeks of self-monitoring blood glucose data from the glucometers for the weeks just prior to each study visit. Researchers used the glucose value ranges recommended by Bergenstal et al. (2013) to estimate the percentage of time each child was low (< 70 mg/dl), in range (70–180 mg/dl), and high (> 180 mg/dl). Researchers assessed the frequency each child and family checked blood glucose each day and did not include glucose values on days where the total number of glucose checks was two standard deviations below the mean number of checks for the total study period.
Parent-Reported Executive Functioning
Researchers used the Behavior Rating Inventory of Executive Function (BRIEF) to measure parent-reported deficits in child executive functioning. The BRIEF is a valid measure of EF for children and adolescents aged 5–18 (Gioia et al., 2000). It includes 86 items in which parents’ rate how often an item has occurred in the previous 6 months using a 3-point Likert scale (i.e., never, sometimes, often). The BRIEF includes two index scores (e.g., Behavioral Regulation Index [BRI] and Metacognition Index [MI]) and one composite score (e.g., Global Executive Composite [GEC]). In all cases, lower scores indicate better executive functioning. Internal consistencies for the GEC, MI, and BRI in the current sample were α = 0.93, α = 0.92, and α = 0.81, respectively.
Child Externalizing Behaviors
We used the Eyberg Child Behavior Inventory (ECBI) to measure parent-report of child externalizing behavior (Eyberg & Ross, 1978). The ECBI includes 36 items that parents respond to using a 7-point Likert scale (i.e., never to always). The scores from the Likert scale form the Intensity Scale. Parents also rate if they perceived each behavior as problematic via a dichotomous “yes/no” response. In this case, the sum of “yes” responses for items forms the Problem Scale. For both the Intensity and Problem Scales, higher scores indicate more externalizing behaviors. The internal consistency for the ECBI in the current sample was α = 0.96.
Diabetes-Specific Conflict
We used the Revised Diabetes Family Conflict Scale (DFCS) to measure parent-reported T1D-specific conflict (Hood et al., 2007). The DFCS has 19 items and parents respond using a 3-point Likert scale (i.e., 1 = never argue, 2 = sometimes argue, and 3 = always argue), with higher scores indicating higher conflict. The DFCS includes two subscales, one that reflects conflict related to routine T1D management tasks (Direct, i.e., rotating injection sites or infusion sets, eating meals, and snacks) and one that reflects conflict related to periodic T1D management tasks (Indirect, i.e., what to eat when away from home). We used the Direct subscale as the measure of T1D-specific conflict in our model as the Indirect subscale was deemed less developmentally appropriate for the age range of the study sample. The internal consistency for the Direct subscale for the current sample was α = 0.89.
Data Analysis
We first assessed for possible covariates by examining bivariate correlations between demographic variables (i.e., HbA1c, duration of T1D, child age, child sex, child ethnicity) and the scores from the parent-reported questionnaires. Then, we entered data into a moderated path analysis model using MPlus8 (Muthén & Muthén, 2017) to test the moderating role of percent of high blood glucose values and T1D-specific conflict on the association between parent-reported EF and child externalizing behaviors. We constructed one latent construct representing Externalizing Behaviors. The Externalizing Behavior latent variable used the two subscales of the ECBI measure, representing the intensity and number of child externalizing behaviors. We then regressed child externalizing behaviors onto parent-reported child EF, percent high blood glucose values, parent perceived T1D-specific conflict, and each two-way interaction (i.e., parent-reported child EF by percent high blood glucose values and parent-reported child EF by parent perceived T1D-specific conflict). To probe for significant interactions, we conducted simple slopes analysis in Mplus using the model constraint command and conditional values of 0 and 1 to denote differences between one standard deviation above and below mean T1D-specific conflict. All models used maximum likelihood estimation with robust standard errors. To examine overall model fit, we evaluated the model chi-square χ2 test of significance, comparative fit index (CFI), standardized root mean square residual (SRMR), and the root-mean-squared error of approximation (RMSEA). We used established benchmarks of model fit, such that CFI values > 0.90 and SRMR and RMSEA values < 0.10 indicated better model fit.
Results
Descriptive Statistics
Children had a mean time since T1D diagnosis of 4.61 months (SD = 3.19) and a mean age of 7.45 years (SD = 1.34). Most parents identified their child as non-Hispanic White (89.3%) and approximately half the sample identified their child as female (52%). Mean child hemoglobin A1c (HbA1c) at baseline was 7.63% (SD = 1.37; 58 mmol/mol). Parents had a mean age of 36.62 years (SD = 6.40 years), 88.8% were mothers, and 80.8% were married. Seventeen percent of children used an insulin pump, 83% used multiple daily injections, and 20% percent of children used a continuous glucose monitor (CGM). Families checked blood glucose levels 6.82 (SD = 2.71) per day on average. Regarding EF, parents reported clinically significant deficits on the GEC for 15.4% of children, and clinically significant deficits on the MI and BRI for 14.6% and 16.9% of children, respectively. Approximately 8.5% of parents reported clinically significant problems on the ECBI; common concerns included the child getting angry when they do not get their way, lingers at mealtimes, and refuses to go to bed on time. Parents reported an average DFCS score of 23.07 (SD = 3.58) and a mean Direct Conflict score of 11.8 (SD = 3.6). Parents commonly reported higher perceived conflict when rotating injection or infusion sites, during meals and snacks, and when remembering to check blood glucose. Children’s blood glucose values were high 31.8% of the time, on average, for the entire sample. Additional descriptive statistics are in Table 1. Prior to conducting our primary analyses, we examined bivariate correlations between HbA1c, duration of T1D, child age, child sex, child ethnicity, and parent-reported scores. We observed a significant correlation between duration of T1D diagnosis and parent-reported T1D-specific conflict (r = 0.21) and no other correlations were significant.
Path Analysis
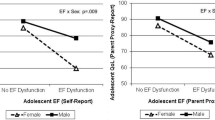
The model fit statistics indicated good fit, \({\chi }_{M}^{2}\)(4) = 11.107, p = .049; RMSEA = 0.057, 90% CI [0.003, 0.103], pRMSEMA<=0.05 = 0.336, CFI = 1.00, and SRMR = 0.08. We entered duration of T1D diagnosis in the path analysis as a covariate and the moderated path analysis revealed a main effect for parent-reported child EF and child externalizing behavior (β = 8.04, p = .01), such that there was an association between greater deficits in parent-reported child EF and higher levels of child externalizing behavior. There was no main effect for percent high blood glucose (p = .66) or parent perceived T1D-specific conflict (p = .33). While these relationships were non-significant, their direction was in the expected positive direction. However, a two-way interaction emerged indicating that T1D-specific conflict moderated the relationship between parent-reported child EF and child externalizing behaviors (β = 1.03, p = .01). Results of simple slopes tests revealed that the slope of the line representing the association between parent-reported child EF and child externalizing behaviors was significant for parent perceived T1D-specific conflict one SD above the mean. This finding suggests that when T1D-specific conflict is elevated, parents who perceive more EF deficits in their child also report more externalizing behaviors (β = 16.40, p = .05). Figure 1 presents our path model describing the associations among parent-reported child EF, percent high blood glucose, parent perceived T1D-specific conflict, and child externalizing behaviors.
Discussion
The present study examined several predictors of child externalizing behavior in a sample of children with recent-onset T1D. Our findings suggested that child externalizing behaviors may associate with T1D-specific conflict in families of children with recent-onset T1D and parent-reported child deficits in EF but does not appear related to our proxy of child glycemic control. In this way, our findings may offer important treatment considerations for clinicians working with families during the recent-onset period of T1D.
Previous research indicates that child cooperation and adequate EF skills are important for T1D management (Holmes et al., 2006). In particular, one study suggests parent-reported child EF deficits associate with suboptimal treatment engagement and lower child-reported quality of life (Perez et al., 2017). Daily T1D management requires several complicated behaviors, including dosing for insulin, monitoring blood glucose levels, counting carbohydrates, moderating dietary intake, and monitoring physical activity to treat non-normal blood glucose levels. Performing T1D management tasks effectively could be difficult for parents of a school-aged child with T1D who has deficits in the primary components of EF, such as behavioral inhibition, organization, and following routines. For example, deficits in EF could make it harder for a child with T1D to comply with adult directives to moderate their food intake or activity levels related to a high or low glucose level, to keep track of T1D management supplies, or to follow through with scheduled T1D management tasks (e.g., seeking adult help with insulin dosing before eating; Bagner et al., 2007). Moreover, under-developed EF skills would make it more challenging for school-age children to become more involved in their T1D management tasks and to begin to assume any autonomy for their T1D management (Wasserman et al., 2015). Thus, when treating school-age children with T1D, clinicians may consider assessing children’s EF levels to inform appropriate T1D management expectations. In addition, these data could inform T1D education. Based on a child’s EF levels, parents could consider modeling T1D management behavior with their child for building skills and whether offering immediate positive feedback for newly acquired skills could help encourage maintenance of new skills. In particular, praise and rewards may be helpful for younger children or helpful for children who struggle with behavioral disinhibition. Children with deficits in behavioral disinhibition and organization might also benefit from one-step prompts as they are beginning to complete T1D management tasks more independently, while environmental cues and reminders might also help if children have trouble following a routine.
Future studies may consider examining how child EF skills relate to shared responsibility of daily T1D management tasks between the parent and child when considering factors that impact child glucose outcomes. For example, if a school-age child assumes some responsibility for completing their own T1D self-management tasks, and their EF skills are under-developed, we may expect to see some effect on their blood glucose levels due to an imbalance of EF skill and increased cognitive demand. Lastly, the present study did not assess for parental EF skills; however, previous studies demonstrate that youth are more likely to have suboptimal glycemic control if their parents have poor problem-solving skills (Wysocki et al., 2008), and there may be a link between lower parent EF skills and challenging child behavior (Deater-Deckard et al., 2012). Researchers may consider how parental EF skills fit in models of child glycemic control and behavior in youth with T1D in future studies.
Our results also suggest that T1D-specific family conflict may exacerbate the relationship between child EF and child disruptive behavior, which may have implications for T1D outcomes. Indeed, several published studies show a positive association between child externalizing behaviors and family conflict and a negative association between child externalizing behaviors and child cooperation around T1D management behaviors (Anderson et al., 2002; Miller & Drotar, 2003; Weinger et al., 2001). There are also two published studies reporting positive associations between child misbehavior and externalizing behaviors and suboptimal T1D outcomes without the influence of family conflict (Cohen et al., 2004; Patton et al., 2006). In the present study, parent-reported conflict was higher than previous reports (Laffel et al., 2003) suggesting that the recent-onset period may be a particularly challenging time for parents and school-age children with T1D. Thus, when aiming to intervene in the recent-onset period of T1D, clinicians may want to consider how high levels of family conflict related to child disruptive behaviors could thwart interventions aimed to improve child health outcomes. In the event, family conflict is a barrier, clinicians should focus on incorporating principles from behavioral family systems therapy to improve positive communication habits, assist families in problem-solving specific points of conflict, and address unhelpful beliefs and attitudes about each person’s behavior (Wysocki et al., 2006).
High glucose levels may impact a child’s cognitive performance, a dimension of EF, which could have important implications for children with T1D (Gonder-Frederick et al., 2009). Interestingly, the results of the present study did not suggest that high blood glucose levels moderate the relationship between parent-reported child EF and child externalizing behaviors. Rather, the findings of the present study align with previous studies that suggest certain measures of glycemia or glycemic control may not associate with parent ratings of child behavior (Hilliard et al., 2011). The present study did not measure family adherence to insulin requirements; however, the variability in a child’s response to their insulin treatment could influence the percentage of time they experience high glucose values. Future research studies should consider assessing other factors of T1D management, such as insulin regimen, which may be more salient when assessing child disruptive behaviors or family functioning in families of children with T1D.
While the present study provides the opportunity for clinicians to consider intervention targets in children recently diagnosed with T1D, there are some limitations to note. First, we used a transactional framework for constructing our theoretical model; however, other frameworks would suggest alternative factors to explore (e.g., coercion theory would suggest we study parenting style in our model). Therefore, we need additional research testing alternative models and theoretical frameworks. Second, we solely collected parent self-report of three similar constructs measured cross sectionally which limit our ability to make temporal or causal assumptions. Future studies aiming to use a moderation analysis should consider an experimental research design where the predictors or moderators may be altered to rigorously examine the proposed interactions. A multi-method, multi-reporter (e.g., other parents/caregivers, teachers) longitudinal design would provide additional opportunities to gain new information regarding the associations of interest. Third, the original validation of the DFCS included children older (i.e., 8–18 years old) than the current study sample. To address this, we choose to omit the Indirect Management subscale of the DFCS in the path model because the items on this subscale are less developmentally appropriate for the younger age range in our sample. The items in the Direct Management subscale more appropriately assess for conflict between the parent and child regarding the time needed to complete daily task, rather than assessing who takes responsibility for the task. Fourth, our sample was largely homogeneous regarding race and ethnicity, and while the demographics were typical of the participating clinics and for T1D in general, this may limit generalizability. Fifth, we were unable to control for the potential impact of the honeymoon period in our model because children with T1D may exit the honeymoon period at varying times during the recent-onset period. Lastly, our EF measure is a parent-report behavioral rating scale of the child’s observable behavior and not a performance-based measure. Toplak et al. (2013) report that behavioral rating scales for EF best capture higher-order processes (e.g., planning, problem solving), while performance-based measures best capture lower-order processes (e.g., working memory, inhibitory control). Therefore, it is possible that we did not obtain a complete assessment of child EF. However, because planning and problem solving are skills essential for optimal T1D management (e.g., dosing insulin based on carbohydrate intake or coordinating eating and physical activity to maintain safe blood glucose levels), and these skills can be accurately captured in behavioral rating scales, we perceive this as a minor limitation.
The findings of the present study may guide assessment and intervention in the recent-onset period of T1D by specifically calling for early screening of child EF, family conflict, and child externalizing behavior. While it is likely that child externalizing behavior and limited child EF skills will pre-date T1D for most families, a diagnosis of T1D is life changing and likely to add considerable stress in families (Whittemore et al., 2012). Therefore, it is possible that the additional stress and worry associated with T1D could further exacerbate conflict in families who already perceive child EF deficits and problematic behavior. Fortunately, problem-solving interventions can reduce T1D-specific conflict and yield promising results for glycemic control and better parent involvement in T1D management (Cook et al., 2002; Mulvaney et al., 2011). Further, our findings also highlight a need for additional research examining screening tools to identify children with behavioral issues and limited EF skills, as well as families with T1D-specific conflict in children recently diagnosed with T1D. The American Diabetes Association currently recommends screening for internalizing symptoms (i.e., depression, anxiety) and eating disorders; however, there are no specific guidelines for the assessment of other behaviors at the time of diagnosis or during routine follow-up care. To fill this gap in the literature and improve patient care, researchers and clinicians may consider the addition of these screening tools during the recent-onset period in order to better assess families’ needs for psychological care and to accelerate the generation of real-world evidence regarding family functioning in the recent-onset period.
Data Availability
To inquire about data used for the present study, contact the corresponding author.
Code Availability
Not applicable.
References
Anderson, B. J., Vangsness, L., Connell, A., Butler, D., Goebel-Fabbri, A., & Laffel, L. M. B. (2002). Family conflict, adherence, and glycaemic control in youth with short duration Type 1 diabetes. Diabetic Medicine, 19(8), 635–642. https://doi.org/10.1046/j.1464-5491.2002.00752.x
Anderson, P. (2002). Assessment and development of executive function (EF) during childhood. Child Neuropsychology, 8, 71–82. https://doi.org/10.1076/chin.8.2.71.8724
Bagner, D. M., Williams, L. B., Geffken, G. R., Silverstein, J. H., & Storch, E. A. (2007). Type 1 diabetes in youth: The relationship between adherence and executive functioning. Children’s Health Care, 36(2), 169–179. https://doi.org/10.1080/02739610701335001
Barkley, R. A. (1997). Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychological Bulletin, 121(1), 65–94. https://doi.org/10.5860/choice.41-3334
Bergenstal, R. M., Ahmann, A. J., Bailey, T., Beck, R. W., Bissen, J., Buckingham, B., & Wesley, D. M. (2013). Recommendations for standardizing glucose reporting and analysis to optimize clinical decision making in diabetes: The ambulatory glucose profile (AGP). Diabetes Technology & Therapeutics, 15(3), 198–211. https://doi.org/10.1089/dia.2013.0051
Cameron, F. J. (2015). The impact of diabetes on brain function in childhood and adolescence. Pediatric Clinics of North America, 62(4), 911–927. https://doi.org/10.1016/j.pcl.2015.04.003
Chiang, J. L., Kirkman, M. S., Laffel, L. M. B., & Peters, A. L. (2014). Type 1 diabetes through the life span: A position statement of the american diabetes association. Diabetes Care, 37(7), 2034–2054. https://doi.org/10.2337/DC14-1140
Clark, C., Prior, M., & Kinsella, G. (2002). The relationship between executive function abilities, adaptive, behaviour, and academic achievement in children with externalising behaviour problems. Journal of Child Psychology and Psychiatry and Allied Disciplines, 43(6), 785–796. https://doi.org/10.1111/1469-7610.00084
Clements, M. A., Lind, M., Raman, S., Patton, S. R., Lipska, K. J., Fridlington, A. G., & Kosiborod, M. (2014). Age at diagnosis predicts deterioration in glycaemic control among children and adolescents with type 1 diabetes. BMJ Open Diabetes Research and Care, 2(1), e000039. https://doi.org/10.1136/bmjdrc-2014-000039
Cohen, D. M., Lumley, M. A., Naar-King, S., Partridge, T., & Cakan, N. (2004). Child behavior problems and family functioning as predictors of adherence and glycemic control in economically disadvantaged children with type 1 diabetes: A prospective study. Journal of Pediatric Psychology, 29(3), 171–184. https://doi.org/10.1093/jpepsy/jsh019
Cook, S., Herold, K., Edidin, D. V., & Briars, R. (2002). Increasing problem solving in adolescents with type 1 diabetes: The choices diabetes program. The Diabetes Educator, 28(1), 115–124. https://doi.org/10.1177/014572170202800113
Dabelea, D., Mayer-Davis, E. J., Saydah, S., Imperatore, G., Linder, B., Divers, J., & Hamman, R. F. (2014). Prevalence of Type 1 and Type 2 Diabetes Among Children and Adolescents From 2001 to 2009. JAMA, 311(17), 1778. https://doi.org/10.1001/jama.2014.3201
Deater-Deckard, K., Wang, Z., Chen, N., & Bell, M. A. (2012). Maternal executive function, harsh parenting, and child conduct problems. Journal of Child Psychology and Psychiatry, 53(10), 1084–1091.
Diamond, A. (2013). Executive Functions. Annual Review of Psychology, 64, 135–168. https://doi.org/10.1146/annurev-psych-113011-143750
Duke, D. C., Geffken, G. R., Lewin, A. B., Williams, L. B., Storch, E. A., & Silverstein, J. H. (2008). Glycemic control in youth with type 1 diabetes: Family predictors and mediators. Journal of Pediatric Psychology, 33(7), 719–727. https://doi.org/10.1093/jpepsy/jsn012
Eyberg, S. M., & Ross, A. W. (1978). Assessment of child behavior problems: The validation of a new inventory. Journal of Clinical Child Psychology, 7(2), 113–116. https://doi.org/10.1080/15374417809532835
Fiese, B. H., & Sameroff, A. J. (1989). Family context in pediatric psychology: A transactional perspective. Journal of Pediatric Psychology, 14(2), 239–260. https://doi.org/10.4324/9780203763063
Gioia, G., Isquith, P., Guy, S., & Kenworthy, L. (2000). Behavior rating inventory of executive function. Child Neuropsychology, 6(3), 235–238. https://doi.org/10.1076/chin.6.3.235.3152
Gonder-Frederick, L. A., Zrebiec, J. F., Bauchowitz, A. U., Ritterband, L., Magee, J. C., Cox, D. J., & Clarke, W. L. (2009). Cognitive function is disrupted by both hypo-and hyperglycemia in school-agedchildren with type 1 diabetes: A field study. Diabetes Care, 32(6), 1001–1006.
Hilliard, M. E., Monaghan, M., Cogen, F. R., & Streisand, R. (2011). Parent stress and child behaviour among young children with type 1 diabetes. Child: Care, Health and Development, 37(2), 224–232. https://doi.org/10.1111/j.1365-2214.2010.01162.x
Hilliard, M. E., Holmes, C. S., Chen, R., Maher, K., Robinson, E., & Streisand, R. (2013). Disentangling the roles of parental monitoring and family conflict in adolescents’ management of type 1 diabetes. Health Psychology, 32(4), 388–396. https://doi.org/10.1037/a0027811
Hilliard, Marisa E., Wu, Y. P., Rausch, J., Dolan, L. M., & Hood, K. K. (2013). Predictors of deteriorations in diabetes management and control in adolescents with type 1 diabetes. https://doi.org/10.1016/j.jadohealth.2012.05.009
Holmes, C. S., Chen, R., Streisand, R., Marschall, D. E., Souter, S., Swift, E. E., & Peterson, C. C. (2006). Predictors of youth diabetes care behaviors and metabolic control: A structural equation modeling approach. Journal of Pediatric Psychology, 31(8), 770–784. https://doi.org/10.1093/jpepsy/jsj083
Hood, K. K., Butler, D. A., Anderson, B. J., & Laffel, L. M. B. (2007). Updated and revised diabetes family conflict scale. Diabetes Care, 30(7), 1764–1769. https://doi.org/10.2337/dc06-2358
Laffel, L. M. B., Connell, A., Vangsness, L., Goebel-Fabbri, A., Mansfield, A., & Anderson, B. J. (2003). General quality of life in youth with type 1 diabetes: Relationship to patient management and diabetes-specific family conflict. Diabetes Care, 26(11), 3067–3073. https://doi.org/10.2337/diacare.26.11.3067
McDonnell, C. M., Northam, E. A., Donath, S. M., Werther, G. A., & Cameron, F. J. (2007). Hyperglycemia and externalizing behavior in children with type 1 diabetes. Diabetes Care, 30(9), 2211–2215.
McNally, K., Rohan, J., Pendley, J. S., Delamater, A., & Drotar, D. (2010). Executive functioning, treatment adherence, and glycemic control in children with type 1 diabetes. Diabetes Care, 33(6), 1159–1162. https://doi.org/10.2337/dc09-2116
Miller, V. A., & Drotar, D. (2003). Discrepancies between mother and adolescent perceptions of diabetes-related decision-making autonomy and their relationship to diabetes-related conflict and adherence to treatment. Journal of Pediatric Psychology, 28(4), 265–274. https://doi.org/10.1093/jpepsy/jsg014
Mulvaney, S. A., Rothman, R. L., Osborn, C. Y., Lybarger, C., Dietrich, M. S., & Wallston, K. A. (2011). Self-management problem solving for adolescents with type 1 diabetes: Intervention processes associated with an Internet program. Patient Education and Counseling, 85(2), 140–142. https://doi.org/10.1016/j.pec.2010.09.018
Muthén, L. K., & Muthén, B. O. (2017). MPlus: Statistical analysis with latent variables user’s guide. In Muthén & Muthén. www.StatModel.com
Northam, E. A., Anderson, P. J., Jacobs, R., Hughes, M., Warne, G. L., & Werther, G. A. (2001). Neuropsychological profiles of children with type 1 diabetes 6 years after disease onset. Diabetes Care, 24(9), 1541–1546. https://doi.org/10.2337/diacare.24.9.1541
Northam, E. A., Matthews, L. K., Anderson, P. J., Cameron, F. J., & Werther, G. A. (2005). Psychiatric morbidity and health outcome in Type 1 diabetes: Perspectives from a prospective longitudinal study. Diabetic Medicine, 22(2), 152–157. https://doi.org/10.1111/j.1464-5491.2004.01370.x
Patton, S. R., Dolan, L. M., & Powers, S. W. (2006). Mealtime interactions relate to dietary adherence and glycemic control in young children with type 1 diabetes. Diabetes Care, 29(5), 1002–1006. https://doi.org/10.2337/dc05-2354
Perez, K. M., Patel, N. J., Lord, J. H., Savin, K. L., Monzon, A. D., Whittemore, R., & Jaser, S. S. (2017). Executive function in adolescents with type 1 diabetes: Relationship to adherence, glycemic control, and psychosocial outcomes. Journal of Pediatric Psychology. https://doi.org/10.1093/jpepsy/jsw093
Toplak, M. E., West, R. F., & Stanovich, K. E. (2013). Practitioner review: Do performance-based measures and ratings of executive function assess the same construct? Journal of Child Psychology and Psychiatry, and Allied Disciplines, 54(2), 131–143. https://doi.org/10.1111/jcpp.12001
Wasserman, R. M., Hilliard, M. E., Schwartz, D. D., & Anderson, B. J. (2015). Practical strategies to enhance executive functioning and strengthen diabetes management across the lifespan. Current Diabetes Reports, 15(8), 1–9.
Weinger, K., O’Donnell, K. A., & Ritholz, M. D. (2001). Adolescent views of diabetes-related parent conflict and support: A focus group analysis. The Journal of Adolescent Health : Official Publication of the Society for Adolescent Medicine, 29(5), 330–336. https://doi.org/10.1016/s1054-139x(01)00270-1
Whittemore, R., Jaser, S., Chao, A., Jang, M., & Grey, M. (2012). Psychological experience of parents of children with type 1 diabetes: A systematic mixed-studies review. The Diabetes Educator, 38(4), 562–579. https://doi.org/10.1177/0145721712445216
Wysocki, T., Harris, M. A., Buckloh, L. M., Mertlich, D., Lochrie, A. S., Taylor, A., & White, N. H. (2006). Effects of behavioral family systems therapy for diabetes on adolescents’ family relationships, treatment adherence, and metabolic control. Journal of Pediatric Psychology, 31(9), 928–938.
Wysocki, T., Iannotti, R., Weissberg-Benchell, J., Laffel, L., Hood, K., Anderson, B., Committee F.M of C. D. S. (2008). Diabetes problem solving by youths with type 1 diabetes and their caregivers: Measurement, validation, and longitudinal associations with glycemic control. Journal of Pediatric Psychology, 33(8), 875–884.
Funding
This research was supported by a Grant R01-DK100779 from the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases.
Author information
Authors and Affiliations
Contributions
All authors contributed to the concept of study design and preparing the manuscript. ADM performed the statistical analyses.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interests exist for authors ADM, CCC, and SRP. MAC is the chief medical officer for Glooko, has consulted with Medtronic Diabetes, Eli Lilly, and receives research support from Abbott Diabetes.
Ethical Approval
The Institutional Review Board (IRB) provided ethical approval for all study procedures.
Human and Animal Rights and Informed Consent Statement
The authors conducted the study with the understanding and written consent of all parents. The study conforms with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The authors obtained Institutional Review Board approval from Children’s Mercy-Kansas City and the University of Colorado Anschutz Medical Campus prior to launching the study. The study does not include any methods or procedures involving animals.
Consent to Participate
All parents provided consent and all children provided assent for study participation.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Monzon, A.D., Cushing, C.C., Clements, M.A. et al. Parent–Child Conflict Moderates the Relationship Between Executive Functioning and Child Disruptive Behaviors in Youth with T1D. J Clin Psychol Med Settings 29, 357–364 (2022). https://doi.org/10.1007/s10880-021-09838-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-021-09838-5