Abstract
Sexual minorities experience higher rates of several physical health problems compared to their heterosexual counterparts. The present study uses Meyer's Minority Stress Model (Psychological Bulletin, 129(5): 674-697, 2003) to examine physical health indicators among 250 adults who identified as sexual minorities. Study hypotheses include that sexual minority stress is predictive of two physical health indicators (i.e., engagement in a health-promoting lifestyle and number of physical health problems) and that planning (i.e., problem-focused) and social support coping will partially mediate the relationship between sexual minority stress and each physical health indicator. Results showed that as level of sexual minority stress increased, engagement in a health-promoting lifestyle decreased and the number of physical health problems increased. Planning and social support coping did not mediate these relationships; however, as levels of coping increased, engagement in a health-promoting lifestyle increased. These findings have implications for researchers and healthcare professionals in their efforts to promote the physical health of sexual minorities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The health of individuals who do not identify as heterosexual, such as individuals who identify as lesbian, gay, or bisexual (hereafter referred to as sexual minorities), is increasingly becoming a major focus of health and health disparities research. This increased focus is evidenced by the participation of national agencies in the understanding and amelioration of health disparities among sexual minorities. For example, among its Healthy People 2020 objectives, the U.S. Department of Health and Human Services included evidence-based health promotion objectives to address the health disparities affecting sexual minorities, e.g., discrimination in healthcare, lack of culturally competent healthcare providers, and unhealthy living environments (Office of Disease Prevention and Health Promotion, 2011). Attention to these disparities is paramount given that the available research shows that sexual minorities experience higher rates of several physical health problems when compared to heterosexual men and women, including: cardiovascular disease (Farmer, Jabson, Bucholz, & Bowen, 2013), obesity-related diseases (Blosnich, Farmer, Lee, Silenzio, & Bowen, 2014; Boehmer, Bowen, & Bauer, 2007; Struble, Lindley, & Montgomery, Hardin, & Burcin, 2011), HIV (CDC, 2015), and certain types of cancer (Conron, Mimiaga, & Landers, 2010). For example, women who identified as a sexual minority were found to have vascular systems that were 7.5% “older” than those of their heterosexual counterparts, making sexual minority women at a significantly higher risk for developing cardiovascular disease (Farmer et al., 2013). Additionally, it has been found that the odds of meeting the criteria for overweight or obesity are 2.25 higher for sexual minority women compared to heterosexual women (Blosnich et al., 2014). It has also been found that sexual minority men account for 81% of the total estimated diagnoses of HIV in the United States in 2013 (CDC, 2015).
The Minority Stress Model (MS Model), which has been used to explain the occurrence of mental health disparities that negatively impact sexual minority populations (Meyer, 2003), may be useful in understanding physical health disparities that negatively impact these populations. In fact, several studies have already demonstrated an association between minority stress and physical health (Institute of Medicine, 2011; Lick, Durso, & Johnson, 2013). The Institute of Medicine (2011) included a minority stress framework as one of four primary frameworks by which to view LGB health disparities. Lick et al. (2013) used the MS Model to describe the mechanisms by which minority stress impacts physical health outcomes. These mechanisms include physiological functioning, psychological processes, and health behaviors.
The MS Model highlights four specific stress processes that are uniquely associated with being a sexual minority (hereafter referred to as sexual minority stress) including: stress related to (a) experiencing prejudiced events, (b) expecting and anticipating the experience of rejection or discrimination, (c) disclosing or concealing one’s identity, and (d) internalizing negative societal attitudes. In the MS Model, coping and social support mediate the relationship between sexual minority stress and mental health outcomes (Meyer, 2007). The outcomes in the MS Model include both positive mental health outcomes (e.g., engaging in stress prevention activities) and negative mental health outcomes (e.g., a diagnosis of a mental illness; Meyer, 2003).
The present study used Meyer’s (2003) MS Model to further the understanding of the relationship between sexual minority stress and physical health indicators (i.e., engaging in a health-promoting lifestyle and self-reported number of physical health problems. The selected outcome variables (i.e., health indicators) in the present study are consistent with those used in the MS Model to explain the relationship between stress and mental health outcomes in that they also include a positive outcome and a negative outcome. Specifically, engaging in a health-promoting lifestyle represents a positive physical health outcome and number of physical health problems represents a negative physical health outcome. Furthermore, these outcomes are important in that they have implications for reducing health disparities among sexual minorities as well as other minority groups.
This study also sought to determine if planning coping (i.e., a form of problem-focused coping) and social support coping are mediators of any existing relationship between sexual minority stress and the aforementioned physical health outcomes. Social support coping was selected as a mediator in the present study because it closely mirrors the social support mediator in the MS Model. Planning coping (which is a form of problem-focused coping) was selected as the second form of coping examined because it is one of the most used forms of coping and has one of the highest Cronbach’s reliability coefficient alphas (α = 0.80) of all the subscales on the Coping Questionnaire (COPE) used in the present study (Carver, Scheier, & Weintraub, 1989). These two forms of coping also represent the two major types of coping strategies according to Lazarus and Folkman’s (1984) classic theory of stress and coping. In this classic theory, planning coping is represented as problem-focused coping and social support coping is represented as emotion-focused coping. It is also the case that forms of problem-focused coping (i.e., planning coping) and emotion-focused coping (i.e., social support coping) were selected as the investigated forms of coping in the present study because use of problem-focused coping and social support have been found to be successful strategies for coping with the negative effects of perceived discrimination on health outcomes (Pascoe & Richman, 2009). See Fig. 1 for an illustration of the investigated relationships.
a Path model for engagement in health-promoting lifestyle outcome. *p < .05, **p < .01. Values represent standardized effect estimates for direct and indirect effects. The c path represents the direct effect of Sexual Minority Stress on Engagement in Health-Promoting Lifestyle plus possible mediating effects of the COPE variables. The c’ path represents the direct effect of Sexual Minority Stress when the possible mediating effects of the COPE variables are removed from the model. The a paths represent the direct effects of Sexual Minority Stress on each mediator. The b paths represent the direct effects of each mediator on Engagement in Health-Promoting Lifestyle. b Path model for physical health problems outcome. *p < .05, **p < .01. Values represent standardized effect estimates for direct and indirect effects. The c path represents the direct effect of Sexual Minority Stress on Physical Health Problems plus possible mediating effects of the COPE variables. The c’ path represents the direct effect of Sexual Minority Stress when the possible mediating effects of the COPE variables are removed from the model. The a paths represent the direct effects of Sexual Minority Stress on each mediator. The b paths represent the direct effects of each mediator on Physical Health Problems
Using a cross-sectional design, the following research hypotheses were investigated:
-
1.
Higher levels of sexual minority stress will predict lower levels of engagement in a health-promoting lifestyle.
-
2.
Higher levels of sexual minority stress will predict a higher number of physical health problems.
-
3.
Both planning coping and social support coping will partially mediate the relationship between sexual minority stress and level of engagement in a health-promoting lifestyle.
-
4.
Both planning coping and social support coping will partially mediate the relationship between sexual minority stress and number of physical health problems.
Method
Participants
A total of 393 individuals consented to participate in the study, which was conducted online; however, only a total of 258 participants completed the online data collection survey, resulting in a 65.6% participation rate. The data of a total of eight participants were removed from the obtained online data collected because these participants did not meet the age criteria for study participation or they had significant missing data (i.e., more than 15% missing data). The final study sample used for data analyses consisted of 250 participants.
Procedure
The Institutional Review Board (IRB) at the university where the researchers are based approved the present study. Participant recruitment and data collection for this study occurred online. Participants in this study were primarily recruited through Yahoo groups, e-mail lists, and media outlets oriented towards sexual minorities. A colleague of the primary researchers who had prior success recruiting sexual minority participants online provided an initial list of Yahoo groups. This list was then supplemented by the addition of Yahoo groups that were found by searching the terms gay, lesbian, bisexual, LGB, LGBT, queer, and pride, and that targeted adult sexual minorities. Some Yahoo groups required administrative approval of online postings that target their group members, while others allowed free posting of information. In an attempt to recruit participants from diverse racial/ethnic backgrounds, online groups for people of color were specifically contacted. Additionally, colleagues with known connections to the LGBT community distributed the recruitment script via Facebook, email listservs, and personal email. The recruitment script described the purposes of the study, which were “to examine how stress related to one’s sexual identity affects physical health problems and engagement in a health-promoting lifestyle” and to “examine what coping styles may adequately address stress in sexual minority adults.” The recruitment script also described the participation criteria, which were as follows: (1) identify as lesbian, gay, bisexual, or as some other sexual minority, (2) is able to read English, and (3) is 18 years of age or older.
A link to the informed consent and measures (i.e., questionnaires) to be completed by participants was included in the e-mail/recruitment script. This link first took participants to a webpage that contained all of the necessary informed consent information. Participants gave consent by clicking on an “agree to terms” option on the webpage. Participants who did not agree were not given access to the measures to be completed; instead, they were sent to a closing webpage that displayed a message of thanks for their time.
After completing the informed consent procedure, participants were directed to a webpage to complete the measures for this study. These measures were counter-balanced (i.e., randomly ordered for each participant), with the exception of the DHIQ, which was used to gather demographic information and was always placed at the end of the group of measures so as not to bias participants’ responses. Completion of the all measures took approximately 15–30 min. Only the researchers for this study had access to the participants’ data. No identifying information, including e-mail addresses, was included with participants’ data. Additionally, the data were password protected. Participants were informed of the procedure for keeping their data confidential.
As an incentive, the 250 participants that completed the online measures for this study were informed that $250 was being donated to the Human Rights Campaign, a civil rights organization that works to achieve equality for LGBT individuals. Participants also were also invited to sign up to receive the results of the study and information regarding the implications of these results for health promotion. After participants were sent a summary of the results and information on the implications of these results, their e-mail addresses, which were kept separate from the rest of the data, were deleted. Participants were informed of these procedures. Online recruitment and data collection lasted 3 months.
Measures
Demographic and Health Information Questionnaire (DHIQ)
The DHIQ is an 11-item survey created by the primary researcher to obtain demographic information for this study, including age, race/ethnicity, sex, sexual orientation, level of education, household income, relationship status, number of people in their household, perceived general health, and diagnosed health conditions. Shively and DeCecco’s (1977) method of assessing sexual orientation was utilized. This method involves asking participants to rate their level of heterosexuality on a 5-point scale and their level of homosexuality on a 5-point scale. Specifically, participants were asked to read the following instructions: “Consider your physical and affectional preference. To what degree are you heterosexual/homosexual (physically attracted to the affectionate with the opposite/same sex)?” Response scales ranged from: 1 = not at all heterosexual/homosexual to 5 = very heterosexual/homosexual. Although this method is somewhat outdated, it uniquely allows for the assessment of sexual orientation using a multi-dimensional scale to capture attraction.
Participants were asked, “In general, how would you describe your health?” The provided 5-point response scale ranged from: 1 = excellent to 5 = poor. Additionally, participants were instructed to complete a checklist on which to check their current physical health problems among those listed and on which to write-in any other current physical health problems not listed on the checklist. Instructions for this question were as follows: “Do you currently have any of the following health conditions?” The physical health problems on the checklist included some of the most prevalent chronic health conditions in the United States (e.g., cardiovascular/heart disease, overweight/obesity, type II diabetes; National Center for Chronic Disease Prevention and Health Promotion, 2015); the checklist also included several disparity physical health conditions that disproportionately affect sexual minorities (e.g., asthma, HIV/AIDS; Institute of Medicine, 2011). In addition to those health conditions listed above, the checklist included high cholesterol, high blood pressure (hypertension), sexually transmitted infection, respiratory problems (e.g., asthma, COPD), gastrointestinal problems (e.g., IBD, ulcer), skin conditions (e.g., eczema, psoriasis), and cancer, including a request to specify the type of cancer. An “Other” response option was included on the part of the checklist where participants were instructed to “please list any additional health conditions.” A response option stating, “I do not have any of these health conditions” was also included. Based on the conditions checked and listed, the number of physical health problems was determined.
Measure of Gay-Related Stressors (MOGS)
The MOGS is a 70-item checklist that is used to assess a series of stressors that are typically experienced by sexual minorities (Lewis, Derlega, Berndt, Morris, & Rose, 2002). Specifically, the MOGS can be used to assess the level of each of the previously described sexual minority stress processes within the MS Model (i.e., experiencing prejudiced events, expecting and anticipating the experience of rejection or discrimination, disclosing or concealing one’s identity, and internalizing negative societal attitudes). When completing this checklist, participants are instructed as follows: “If you experienced the event in the past year AND it was stressful, please select YES. If you have not experienced the event in the past year, please select NO.”
The checklist has ten subscales that include: (1) Family Reaction (nine items; e.g., “Rejection by family members due to my sexual orientation”); (2) Family Reactions to my Partner (three items; e.g., “Introducing a new partner to my family”); (3) Visibility with Family and Friends (seven items; e.g., “Keeping my orientation secret from family and friends”); (4) Visibility with Work and Public (six items; e.g., “Rumors about me at work due to my sexual orientation”); (5) Violence and Harassment (seven items; e.g., “Threat of violence due to my sexual orientation”); (6) Misunderstanding (three items; e.g., “Lack of acceptance of gays in society”); (7) Discrimination at Work (seven items; e.g., “Potential job loss due to sexual orientation”); (8) General Discrimination (three items; e.g., “Housing discrimination due to my sexual orientation”); (9) HIV/AIDS (seven items; e.g., “Fear that I might get HIV or AIDS”); and (10) Sexual Orientation Conflict (four items; e.g., “Difficulty accepting my sexual orientation”). Fourteen inventory items are excluded from the subscales because they had low factor loadings, cross-loaded on multiple subscales, or had inadequate variability of responses. However, only an overall score was used in the present study given sample size limitations and a lack of theoretical justification to focus on any particular subscale over others.
Level of sexual minority stress was calculated by summing the number of items endorsed, with scores ranging from 0 to 70. Higher scores indicate a greater degree of sexual minority stress. Cronbach’s reliability coefficient alpha for the overall score in present sample was .94.
Coping Questionnaire (COPE)
The COPE is a 60-item questionnaire that is used to measure an individual’s level of use of various coping styles (Carver et al., 1989). The instruction on the COPE is to “think about what you usually do when you are under a lot of stress” and then “respond to each of the following items by selecting how frequently you use that response.” These frequency ratings are made using a 4-point Likert-type scale that ranged from: 1 = usually don’t do this at all to 4 = usually do this a lot.
The COPE consists of fifteen subscales, two of which were used in the present study (consisting of eight total items). The two subscales used in the present study were planning coping, a form of problem-focused coping, and social support coping. Example planning coping subscale items are “I try to come up with a strategy about what to do” and “I make a plan of action.” Example social support coping subscale items are “I ask people who have had similar experiences what they did” and “I try to get advice from someone about what to do.” Scores are calculated by summing the ratings of the items in each individual subscale. Higher scores indicate more frequent utilization of each coping style. Cronbach’s reliability coefficient alpha for the present sample was .85 for the planning coping subscale and .86 for the social support coping subscale.
Health-Promoting Lifestyle Profile II (HPLP II)
The HPLP II is a 52-item self-report inventory that measures level of engagement in an overall health-promoting lifestyle (Walker, Sechrist, & Pender, 1987). The inventory instructions inform participants that the “questionnaire contains statements about your present way of life or personal habits” and asks them to “indicate the frequency with which you engage in each behavior.” Response scales ranged from: 1 = never to 4 = routinely.
The HPLP II has six subscales that measure frequency of engagement in health-promoting behaviors within each of six domains (i.e., spiritual growth, interpersonal relations, nutrition, physical activity, health responsibility, and stress management). The spiritual growth subscale has nine items, and example items include “Believe that my life has a purpose” and “Am aware of what is important to me in life.” The interpersonal relations subscale has nine items, and example items include “Discuss my problems and concerns with people close to me” and “Praise other people easily for their achievements.” The nutrition subscale has nine items, and example items include “Limit use of sugars and food containing sugar (sweets)” and “Eat 2–4 servings of fruit each day.” The physical activity subscale has eight items, and example items include “Follow a planned exercise program” and “Exercise vigorously for 20 or more minutes at least three times a week (such as brisk walking, bicycling, aerobic dancing, using a stair climber).” The health responsibility subscale has nine items, and example items include “Report any unusual signs or symptoms to a physician or other health professional” and “Read or watch TV programs about improving health.” The stress management subscale has eight items, and example items include “Take some time for relaxation each day” and “Concentrate on pleasant thoughts at bedtime.” However, only the overall composite score was used in the present study due to sample size limitations and a lack of theoretical justification to focus on any particular subscale over others.
Overall composite scores are obtained by calculating the mean of the individual’s responses to all of the items. Higher scores indicate higher levels of engagement in a health-promoting lifestyle. Cronbach’s reliability coefficient alpha for the overall composite scores in the present sample was .94.
Statistical Analysis
Hypotheses 1–4 were tested using a bootstrapped path analysis using SPSS 19.0 and AMOS 20.0. The use of this empirical method ensures that the asymptotic assumption of normally distributed effects need not be met (Arbuckle, 2008). This method can be useful when testing mediation effects because it takes into account skewed distributions of indirect effects (Preacher & Hayes, 2008; Shrout & Bolger, 2002). The model was fully recursive.
The bootstrapping method produces thousands of resampled data sets (random sampling with replacement) from the original measured data set, each with the same sample size as the original sample. The direct and indirect effects are re-estimated in each random resample. The standard deviation of these effects serves as the empirical standard error used to test the significance of the average direct and indirect effects.
The hypothesized partial mediation is consistent with existing research demonstrating a significant direct effect of sexual minority stress on physical health outcomes (Frost, Lehavot, & Meyer, 2015), which is not expected to be fully accounted for by the coping mediators. Therefore, it is expected that the direct effect of sexual minority stress on physical health outcomes will be reduced, but still significant, with the addition of the coping mediators.
Results
Sample Demographic Characteristics
A total of 250 adults who self-identify as a sexual minority participated in this study. Participants varied in their sexual orientation (see Table 1). Participants ranged in age from 18 to 89 years old (M = 41, SD = 14.56). There were 146 (58.4%) females, 86 (34.4%) males, 12 (4.8%) transgender individuals, and 6 (2.4%) participants who identified as “other” (i.e., genderfluid, queer, two-spirited).
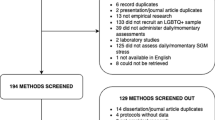
The racial/ethnic composition of the study participants is as follows: 188 (75.2%) non-Hispanic Caucasian/White/European Americans; 26 (10.4%) multi-racial/multi-ethnic individuals; 17 (6.8%) Asians/Asian Americans; 11 (4.4%) Hispanics/Latinos(as); 3 (1.2%) Black/African Americans; 1 (0.4%) American Indian/Alaska Native; and 4 (1.6%) “others” (e.g., Middle Eastern, Texan). The majority of participants were highly educated. One hundred twenty-five (50%) had completed professional/graduate school and 66 (26.4%) had completed a 4-year college/university. The median household income was $30,000. In terms of participants’ ratings of their overall health, 24 (9.6%) rated their health as excellent, 92 (36.8%) rated their health as very good, 89 (35.6%) rated their health as good, 36 (14.4%) rated their health as fair, and 9 (3.6%) rated their health as poor. See Fig. 2 for a breakdown of the number of participants who endorsed each of the physical health status options provided.
Preliminary Analyses
Descriptive statistics of all of the study variables were calculated (see Table 2). The internal reliability of each self-report scale for the study’s sample was calculated using Cronbach’s reliability coefficient alpha (see Table 2 for the obtained and comparative alphas).
Results of the Bootstrapped Path Analysis to Test Hypotheses 1–4
Two statistical packages, AMOS 20.0 and SPSS 19.0, were used to conduct the bootstrapped mediation. All calculations involved were based on standardized values. Table 3 shows the resulting standardized direct regression paths and indirect mediation paths. The overall model accounted for 26% of the variance in level of engagement in a health-promoting lifestyle and 5% of the variance in number of physical health problems.
Direct Effects
The direct effects of sexual minority stress on each physical health indicator were significant; thus, Hypotheses 1 and 2 were supported. Results indicated that sexual minority stress had a significant negative direct effect on engagement in a health-promoting lifestyle (p < .05) and a significant positive direct effect on number of physical health problems (p < .05). The standardized direct effect of sexual minority stress on engagement in a health-promoting lifestyle was −0.258 (SE = 0.052; 95% CI −0.349 to −0.150; p = .021). The standardized direct effect of sexual minority stress on number of physical health problems was 0.187 (SE = 0.077; 95% CI 0.039 to 0.353; p = .01). Results also indicated that planning coping (0.320; SE = 0.051; 95% CI 0.226 to 0.449; p = .007) and social support coping (0.298; SE = 0.057; 95% CI 0.177 to 0.411; p = .012) had a significant positive direct effect on engagement in a health-promoting lifestyle. All other direct effects were not significant. See Table 3 for the selected statistics on all direct effects.
Indirect Effects
The test of the indirect effects, i.e., the effect of sexual minority stress on the physical health indicators when accounting for coping, revealed no significant reduction of the direct effect between sexual minority stress and the physical health indicators and no significant change when adding the coping variables. Specifically, planning coping and social support coping did not significantly mediate the relationship between sexual minority stress and engagement in a health-promoting lifestyle. The standardized indirect effect of sexual minority stress on engagement in a health-promoting lifestyle was −0.225 (SE = 0.049; 95% CI −0.311 to 0.121; p = .028). Similarly, planning and social support coping did not significantly mediate the relationship between sexual minority stress and number of physical health problems. The standardized indirect effect of sexual minority stress on number of physical health problems remained significant despite the presence of the coping variables (0.197; SE = 0.077; 95% CI 0.050 to 0.353; p = .009).
Discussion
Summary of Results
The direct effects within the path model used to test the stated hypotheses in this study suggest that as levels of sexual minority stress increased, engagement in a health-promoting lifestyle decreased. Additionally, the direct effects suggest that as levels of sexual minority stress increased, the number of physical health problems also increased. There were no significant changes when the possible mediation effects of coping were removed from the path model. However, it is notable that as levels of planning coping and social support coping increased, engagement in a health-promoting lifestyle also increased.
Implications of Results
Sample Health Characteristics
This study adds to the literature on the state of physical health among sexual minorities. It is important to highlight that while 46.4% of participants rated their health as very good or excellent, the average participant endorsed having approximately two physical health problems. At this time, it is unknown how this average compares to a heterosexual sample; however, in a general sample of adults, individuals endorsed having an average of 2.4 chronic health problems (Bayliss et al., 2012). Further research should establish if sexual minorities experience differing rates of total physical health problems compared to their heterosexual counterparts.
The high rate of overweight or obesity in this sample (44.4%) is particularly noteworthy given that these health conditions are linked to a number of serious chronic physical health problems including: type 2 diabetes (Danaei et al., 2009), cardiovascular diseases (WHO, 2009), and some cancers (Vucenik & Stains, 2012). The high rate of overweight/obesity we found is consistent with research that has shown high rates of overweight and obesity among lesbian and bisexual women (Boehmer et al., 2007; Struble et al., 2011).
Minority Stress (MS) Model
Meyer’s MS Model addresses several processes and concepts related to sexual identity; various sources of stress, coping, and social support mechanisms; and mental health (Meyer, 2007). Previous research has shown that sexual minority stress may be linked with negative mental health outcomes (Frisell, Lichtenstein, Rahman, & Langstrom, 2010; Herek & Garnets, 2007; Meyer, 2003; Szymanski, 2009).
Broadly, the results from the present study do support the hypothesized negative associations between sexual minority stress and physical health indicators (i.e., level of engagement in a health-promoting lifestyle and number of physical health problems). These results are consistent with earlier research showing that sexual minority stress is linked to physical health problems (Lick et al., 2013).
It is noteworthy, however, that coping mediation focused hypotheses in the present study were not supported. Specifically, planning (i.e., problem-focused) coping and social support coping did not mediate the relationship between sexual minority stress and level of engagement in a health-promoting lifestyle or number of physical health problems.
The finding that planning coping was not a mediator in the examined relationships is somewhat surprising given studies showing that problem-focused coping may mediate the relationship between stress and subjective well-being, which is one aspect of health (Chao, 2011; Karlsen, Dybdahl, & Vitterso, 2006). Furthermore, this finding is surprising because problem-focused coping has been shown to be a useful strategy for coping with both discrimination and physical health stressors (Duangdao & Roesch, 2008; Moskowitz, Hult, Bussolari, & Acree, 2009; Pascoe & Richman, 2009), and we therefore expected it to be a significant factor in explaining the relationship between sexual minority stress and physical health indicators.
The finding that social support coping was not a mediator in the investigated relationships in the present study is also somewhat surprising given the existing evidence that social support is a useful strategy for coping with general stress and sexual minority stress and results in positive psychological outcomes (Hequembourg & Brallier, 2009; Lehavot & Simoni, 2011; Mansini & Barrett, 2008). However, it may be that actual received social support, rather than social support coping, is positively linked to physical health outcomes. For example, individuals may indicate on the COPE that they often “try to get advice from someone about what to do.” However, this response provides very little indication about the level of support they actually receive. It may be that actual received social support mediates the relationship between sexual minority stress and physical health indicators. Whether or not this is the case can be examined in future research studies.
Limitations and Future Directions
The present study has some noteworthy limitations. The majority of the sample consisted of White (75.2%) participants, thus limiting the generalizability of study findings to other racial/ethnic populations. Despite efforts to recruit participants from diverse racial/ethnic backgrounds by specifically targeting several online groups for people of color, there was little representation of racial/ethnic minority groups in the participant sample for the present study. There was also limited representation of transgender individuals (4.8%) in participant sample. It is possible that greater representation of these minority groups could have elevated sexual minority stress scores and changed the findings in the present study. Research similar to the present study is needed but with larger and more diverse samples of sexual minorities, including sexual minorities who are also racial/ethnic minorities.
Another study limitation is the use of self-report measures, which can be unreliable and subject to participants’ biases. However, such measures are commonly used in health research despite this limitation (Bhandari & Wagner, 2006; DiMatteo, 2004). Future studies similar to the present study should ideally include objective health indicator data such as health behavior logs.
The measure of sexual minority stress (i.e., the MOGS) in the present study may be a limitation due to the complexity and subjectivity of the instruction for this measure. The instruction is to endorse an item on the MOGS if the individual had experienced the event and the event was stressful. Thus, the experience of a typically stressful event may have impacted participants without causing distress, but the present study does not capture those experiences. Future research should differentiate between experiences of sexual minority stressors and feelings of distress related to such stressors in order to better understand how these experiences impact health.
Conclusions
The results of the present study are important in part because they call attention to the fact that sexual minority stress can be negatively associated with physical health indicators (i.e., levels of engagement in a health-promoting lifestyle and number of physical health problems), and not just with psychological health indicators, as in Meyer’s (2003) MS Model. Additionally, this study suggests that planning coping and social support coping may help promote engaging in a health-promoting lifestyle among sexual minorities similar to those in this study.
The results of this study also suggest that research is needed to explore both internal and external strategies that may help reduce sexual minority stress and help to explain the relationship between sexual minority stress and physical health indicators. It would be helpful to utilize current literature that has found significant mediators between minority stress and other behavioral and health-related indicators. The current literature on such mediators can inform future research on the relationship between sexual minority stress and physical health indicators. For example, some research has shown that factors such as personality traits or relationship satisfaction are significant mediators between minority stress and other outcomes (Lewis, Milletich, Derlega, & Padilla, 2014; Livingston, Christianson, & Cochran, 2016). These factors could be potential mediators between sexual minority stress and physical health indicators.
It is important that future research includes a culturally diverse, representative sample of sexual minorities. Multiple methods of targeted participant recruitment in such research also is needed. Involving culturally diverse sexual minorities in the planning of such research may help identify recruitment methods that result in participant samples that include adequate numbers of racial/ethnic minorities.
Finally, the present study has implications for health care professionals in their efforts to promote the physical health of their sexual minority patients. Specifically, it is important that health care professionals ask sexual minority patients about their perceived level of stress and how this perceived stress impacts their health behaviors. This information will enable health care providers to make any needed recommendations for stress management interventions that may help improve the psychological and physical health of their patients.
Change history
22 December 2017
The original version of this article unfortunately contains a mistake. In page 229, first paragraph, line 5, the value 0.353 should read as 0.347. In page 230, first paragraph, line 10, the value 0.121 should read as − 0.121.
References
Arbuckle, J. L. (2008). Amos 17.0 User’s guide. Crawfordville, FL: Amos Development Corporation.
Bayliss, M., Rendas-Baum, R., White, M. K., Maruish, M., Bjorner, J., & Tunis, S. L. (2012). Health-related quality of life (HRQL) for individuals with self-reported chronic physical and/or mental health conditions: Panel survey of an adult sample in the United States. Health and Quality of Life Outcomes, 10, 154. doi:10.1186/1477-7525-10-154.
Bhandari, A., & Wagner, T. (2006). Self-reported utilization of health care services: Improving measurement and accuracy. Medical Care Research & Review, 63(2), 217–235. doi:10.1177/1077558705285298.
Blosnich, J. R., Farmer, G. W., Lee, J. G. L., Silenzio, V. M. B., & Bowen, D. J. (2014). Health inequalities among sexual minority adults: Evidence from ten U.S. states, 2010. American Journal of Preventive Medicine, 46(4), 337–349. doi:10.1016/j.amepre.2013.11.010.
Boehmer, U., Bowen, D. J., & Bauer, G. R. (2007). Overweight and obesity in sexual-minority women: Evidence from population-based data. American Journal of Public Health, 97(6), 1134–1140. doi:10.2105/AJPH.2006.088419.
Carver, C., Scheier, M., & Weintraub, J. (1989). Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology, 56(2), 267–283. doi:10.1037/0022-3514.56.2.267.
Centers for Disease Control and Prevention. (2015). Diagnoses of HIV infection in the United States and dependent areas, 2013. HIV Surveillance Report, 25. Retrieved from http://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-vol-25.pdf on 5 June 2016.
Chao, R. C. (2011). Managing stress and maintain well-being: Social support, problem-focused coping, and avoidant coping. Journal of Counseling & Development, 89(3), 338–348. doi:10.1002/j.1556-6678.2011.tb00098.x.
Conron, K. J., Mimiaga, M. J., & Landers, S. J. (2010). A population-based study of sexual orientation identity and gender differences in adult health. American Journal of Public Health, 100(10), 1953–1960. doi:10.2105/AJPH.2009.174169.
Danaei, G., Ding, E. L., Mozaffarian, D., Taylor, B., Rehm, J., Murray, C.J. L. et al. (2009). The preventable causes of death in the United States: Comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Medicine, 6(4), e1000058. doi:10.1371/journal.pmed.1000058.
DiMatteo, M. R. (2004). Variations in patients’ adherence to medical recommendations: A quantitative review of 50 years of research. Medical Care, 42(3), 200–209. doi:10.1097/01.mlr.0000114908.90348.f9.
Doty, N. D., Willoughby, B. L. B., Lindahl, K. M., & Malik, N. M. (2010). Sexuality related social support among lesbian, gay, and bisexual youth. Journal of Youth Adolescence, 39, 1134–1147. doi:10.1007/s10964-010-9566-x.
Duangdao, K. M., & Roesch, S. C. (2008). Coping with diabetes in adulthood: A meta-analysis. Journal of Behavioral Medicine, 31(4), 291–300. doi:10.1007/s10865-008-9155-6.
Farmer, G. W., Jabson, J. M., Bucholz, K. K., & Bowen, D. J. (2013). A population-based study of cardiovascular disease risk in sexual-minority women. American Journal of Public Health, 103(10), 1845–1850. doi:10.2105/AJPH.2013.301258.
Frisell, T., Lichtenstein, P., Rahman, Q., & Langstrom, N. (2010). Psychiatric morbidity associated with same-sex sexual behaviour: Influence of minority stress and familial factors. Psychological Medicine, 40(2), 315–324. doi:10.1017/S0033291709005996.
Frost, D. M., Lehavot, K., & Meyer, I. H. (2015). Minority stress and physical health among sexual minority individuals. Journal of Behavioral Medicine, 38(1), 1–8. doi:10.1007/s10865-013-9523-8.
Hequembourg, A. L., & Brallier, S. A. (2009). An exploration of sexual minority stress across the lines of gender and sexual identity. Journal of Homosexuality, 56(3), 273–298. doi:10.1080/00918360902728517.
Herek, G. M., & Garnets, L. D. (2007). Sexual orientation and mental health. Annual Review of Clinical Psychology, 3, 353–375. doi:10.1146/annurev.clinpsy.3.022806.091510.
Institute of Medicine. (2011). The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. Washington: The National Academies Press.
Karlsen, E., Dybdahl, R., & Vitterso, J. (2006). The possible benefits of difficulty: How stress can increase and decrease subjective well-being. Scandinavian Journal of Psychology, 47(5), 411–417. doi:10.1111/j.1467-9450.2006.00549.x.
Lazarus, R. S., & Folkman, S. (1984). Stress, appraisal, and coping. New York: Springer.
Lehavot, K., & Simoni, J. M. (2011). The impact of minority stress on mental health and substance use among sexual minority women. Journal of Consulting & Clinical Psychology, 79(2), 159–170. doi:10.1037/a0022839.
Lewis, R. J., Derlega, V. J., Berndt, A., Morris, L. M., & Rose, S. (2002). An empirical analysis of stressors for gay men and lesbians. Journal of Homosexuality, 42(1), 63–68. doi:10.1300/J082v42n01_04.
Lewis, R. J., Milletich, R. J., Derlega, V. J., & Padilla, M. A. (2014). Sexual minority stressors and psychological aggression in lesbian women’s intimate relationships: The mediating roles of rumination and relationship satisfaction. Psychology of Women Quarterly, 38(4), 535–550. doi:10.1177/0361684313517866.
Lick, D. J., Durso, L. E., & Johnson, K. L. (2013). Minority stress and physical health among sexual minorities. Perspectives on Psychological Science, 8(5), 521–548. doi:10.1177/1745691613497965.
Livingston, N. A., Christianson, N., & Cochran, B. N. (2016). Minority stress, psychological distress, and alcohol misuse among sexual minority young adults: A resiliency-based conditional process analysis. Addictive Behaviors, 63, 125–131. doi:10.1016/j.addbeh.2016.07.011.
Mansini, B. E., & Barrett, H. A. (2008). Social support as a predictor of psychological and physical well-being and lifestyle in lesbian, gay, and bisexual adults aged 50 and over. Journal of Gay & Lesbian Social Services, 20(1–2), 91–110. doi:10.1080/10538720802179013.
McElligott, D., Capitulo, K. L., Morris, D. L., & Click, E. R. (2010). The effect of a holistic program on health-promoting behaviors in hospital registered nurses. Journal of Holistic Nursing, 28(3), 175–183. doi:10.1177/0898010110368860.
Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. doi:10.1037/0033-2909.129.5.674.
Meyer, I. H. (2007). Prejudice and discrimination as social stressors. In I. H. Meyer & M. E. Northridge (Eds.), The health of sexual minorities: Public health perspectives on lesbian, gay, bisexual, and transgender populations (pp. 242–267). New York: Springer.
Moskowitz, J. T., Hult, J. R., Bussolari, C., & Acree, M. (2009). What works in coping with HIV? A meta-analysis with implications for coping with serious illness. Psychological Bulletin, 135(1), 121. doi:10.1037/a0014210.
National Center for Chronic Disease Prevention and Health Promotion. (2015). Chronic disease overview. Retrieved from http://www.cdc.gov/chronicdisease/overview/ on 5 June 2016.
Office of Disease Prevention and Health Promotion. (2011). Lesbian, gay, bisexual, and transgender health. Retrieved from http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=25 on 5 June 2016.
Pascoe, E. A., & Smart Richman, L. (2009). Perceived discrimination and health: A meta-analytic review. Psychological Bulletin, 135(4), 531–554. doi:10.1037/a0016059.
Preacher, K. J., & Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40(3), 879–891. doi:10.3758/BRM.40.3.879.
Shively, M. G., & DeCecco, J. P. (1977). Components of sexual identity. Journal of Homosexuality, 3(1), 41–48. doi:10.1300/J082v03n01_04.
Shrout, P. E., & Bolger, N. (2002). Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods, 7(4), 422–445. doi:10.1037//1082-989X.7.4.422.
Struble, C. B., Lindley, L. L., Montgomery, K., Hardin, J., & Burcin, M. (2011). Overweight and obesity in lesbian and bisexual college women. Journal of American College Health, 59(1), 51–56. doi:10.1080/07448481.2010.483703.
Szymanski, D. M. (2009). Examining potential moderators of the link between heterosexist events and gay and bisexual men’s psychological distress. Journal of Counseling Psychology, 56(1), 142–151. doi:10.1037/0022-0167.56.1.142.
Vucenik, I., & Stains, J. P. (2012). Obesity and cancer risk: Evidence, mechanisms, and recommendations. Annals of the New York Academy of Sciences, 1271, 37–43. doi:10.1111/j.1749-6632.2012.06750.x.
Walker, S. N., & Hill-Polerecky, D. M. (1996). Psychometric evaluation of the Health-Promoting Lifestyle Profile II. Unpublished manuscript, University of Nebraska Medical Center.
Walker, S. N., Sechrist, K. R., & Pender, N. J. (1987). The health-promoting lifestyle profile: Development and psychometric characteristics. Nursing Research, 36(2), 76–81. doi:10.1097/00006199-198703000-00002.
World Health Organization. (2009). Global health risks: Mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization
Acknowledgements
We thank the Health Psychology Research Team at the University of Florida for their assistance with this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Delphia J. Flenar, Carolyn M. Tucker, and Jaime L. Williams declared that they have no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Human and Animal Rights and Informed Consent
All procedures performed in this study involving human participants were done in accordance with the ethical standards of the University of Florida and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all study participants.
Additional information
A correction to this article is available online at https://doi.org/10.1007/s10880-017-9523-x.
Rights and permissions
About this article
Cite this article
Flenar, D.J., Tucker, C.M. & Williams, J.L. Sexual Minority Stress, Coping, and Physical Health Indicators. J Clin Psychol Med Settings 24, 223–233 (2017). https://doi.org/10.1007/s10880-017-9504-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-017-9504-0