Abstract
The current study examined the link between immune functioning (CD4 count) and physical symptoms, as well as the moderating role of optimism and depressive symptoms, in a sample of 99 low income, inner city African American women with HIV. Although there was no main effect of CD4 count on physical symptoms, depressive symptoms moderated the association between CD4 count and physical symptoms. More compromised immune functioning (lower CD4 count) was associated with more physical symptoms under conditions of higher levels of depressive symptoms, but not lower levels of depressive symptoms. This finding was observed using both a self-report measure and a clinician-rating of women’s depressive symptoms. There were no main or interactive effects for optimism. Clinical implications and future research directions are presented.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Early in the HIV/AIDS epidemic women were rarely diagnosed with the disease; however, today women account for more than 25% of all new HIV/AIDS diagnoses and African American women are especially affected by the disease (Corea, 1992; Centers for Disease Control and Prevention [CDC], 2005). Sixty-four percent of the women currently living with HIV/AIDS are African American, a rate that is more than three times that of the percentage (19%) of White women living with the illness (CDC, 2005). Moreover, HIV/AIDS is the leading cause of death for African American women aged 25–34 years and the third leading cause of death for African American women aged 35–44 years (CDC, 2005), time periods representing prime childbearing and childrearing years for women. Although HIV/AIDS has been associated with compromised parenting and child functioning in African American families (e.g., Forehand et al., 2002; Jones, Foster, Zalot, Chester, & King, 2007), relatively less is known about the health-related quality of life of African American mothers who are presenting with HIV/AIDS in our public health clinics and hospital settings.
One well-established marker of quality of life in the HIV/AIDS literature is the extent to which individuals experience and report physical health symptoms (e.g., Ashton et al., 2005; Justice, Chang, Rabeneck, & Zackin, 2001; Wu, Hays, Kelly, Malitz, & Bozzette, 1997). Among individuals with HIV/AIDS, greater physical health complaints are associated with increased rates of hospitalization, lower rates of survival, and poorer coping with the illness (e.g., Ashton et al., 2005; Justice et al., 2001). Importantly, women report more physical symptoms than men, even after controlling for depression (Kroenke & Spitzer, 1998) and may place greater importance on the significance of physical symptoms when evaluating their health status and seeking medical treatment (Caces, Harford, & Aitken, 1998; Kaplan et al., 1996). In addition, racial/ethnic differences in physical symptoms may exist among women. That is, African American women may give more credence to physical health symptoms when rating their overall health than European American women (e.g., Silverman, Smola, & Musa, 2000). In turn, physical health symptoms have been shown to be more predictive of functional impairment and distress among African American than European American women (Faucett, Gordon, & Levine, 1994; McCraken, Matthews, Tang, & Cuba, 2001). Accordingly, physical health symptoms appear to be a particularly important marker of health and well-being for African American women, yet we know little about the predictors of physical health complaints among the growing number of African American mothers living with HIV/AIDS.
Although CD4 count is a primary marker of disease progression among individuals with HIV/AIDS and individuals with the illness have proven to be relatively reliable reporters of their own immune functioning (Boarts, Sledjeski, Bogart, & Delahanty, 2006), CD4 counts are an inconsistent predictor of physical health complaints in individuals with HIV/AIDS (Ashton et al., 2005; Lee, Portillo, & Miramontes, 2001; Wu et al., 1997). For example, Ashton et al. (2005) reported a significant correlation between CD4 count and physical health symptoms in their primarily low-income, ethnically diverse sample of men and women with HIV/AIDS. Although not the primary focus of the study, Ashton and colleagues reported that individuals with lower CD4 counts reported more physical health symptoms at baseline and greater change in physical health symptoms over time. Alternatively, Lee et al. (2001) reported that CD4 count was a less consistent predictor of physical health symptoms in their sample of women with HIV/AIDS. Specifically, CD4 count was not significantly related to ratings of general fatigue, a symptom associated with progression of illness and mortality among individuals with HIV/AIDS. CD4 count was, however, associated with increased daytime sleepiness.
The inconsistent role of CD4 count in predicting self-reported physical symptoms suggests that other factors may influence the level of physical symptoms experienced among African American women infected with HIV/AIDS. Of interest to clinical psychologists who work with medically ill populations is the impact of psychological variables on physical symptoms. Two potential moderators of particular relevance for African American mothers who are being treated for HIV/AIDS in our public health clinics and hospitals are optimism and depressive symptoms.
More attention has been devoted to depression in the HIV/AIDS literature relative to optimism, particularly in the study of women. Estimated lifetime rates of depression among individuals with HIV/AIDS range from 5 to 42% (Fulk, Kane, Phillips, Bopp, & Hand, 2004; Ickovics et al., 2001; Spiegel et al., 2003). Moreover, African American mothers infected with HIV/AIDS endorse higher levels of depressive symptoms relative to their non-infected, but demographically matched, counterparts (e.g., Jones, Beach, & Forehand, 2001a). In turn, depressive symptoms are associated with compromised health, including greater physical health symptoms among individuals with HIV/AIDS (e.g., Berkan et al., 2001; Breitbart et al., 1996; Jones et al., 2001b). Theoretical explanations for the link between depression and physical health suggest physiological and neurohormonal mechanisms by which depressive symptoms may directly alter health via compromises in immune functioning or, alternatively, indirectly alter health and immune functioning via increases in health-risk behavior and decreases in compliance with treatment (Cohen & Rodriquez, 1995; Cook et al., 2006; Kiecolt-Glasser, McGuire, Robles, & Glaser, 2002).
In contrast to the literature examining depression, less is known regarding protective factors in the progression of HIV/AIDS among infected African American women. Some preliminary findings provide support for the protective role of dispositional optimism among African American women with HIV/AIDS (Devine et al., 2000). The expectancy-based model of dispositional optimism relates to an individual’s positive expectations regarding the future (Carver & Scheier, 2003). Importantly, both theory and research suggest that higher levels of optimism favorably influence how individuals respond to stress and cope with hardship associated with illness (Carver et al., 1993; Lauver & Tak, 1995). Higher levels of optimism have been linked to improved functioning across a variety of variables, from coping with stress (Carver et al., 1993) to lower morbidity and mortality (see Peterson, 2000, for a review). Among HIV infected gay men/men who have sex with men, optimism has also been linked to improved functioning and resiliency (e.g., Cruess et al., 2000); however, the role of optimism among infected women, particularly African American mothers, has received less attention (e.g., Jones, O’Connell, Gound, Heller, & Forehand, 2004).
Based on the literature highlighting the role of depressive symptoms and optimism in health and illness generally and HIV/AIDS in particular, the current study examined their role as moderators of the relation between CD4 count and self-reported physical symptoms in a population of low income inner city HIV-infected African American women. Of particular interest was whether the link between CD4 counts and physical symptoms was strengthened or weakened depending on the level of depression and optimism, respectively. Specifically, it was hypothesized that optimism would buffer the link between compromised immune functioning and physical health complaints whereas it was expected that depressive symptoms would exacerbate the association. A better understanding of the moderating role of these potential psychosocial risk and protective factors could assist with the provision of psychological and medical services for the growing number of African American mothers coping with HIV/AIDS and, in turn, the well-being of their families as well.
Method
Participants
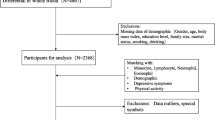
The current study represents secondary analyses of data from a larger longitudinal study examining the physical and psychosocial functioning of low-income, inner-city, African American mothers, approximately half of whom where infected with HIV/AIDS, and their non-infected children (Family Health Project Research Group, 1998). Participants for the current study were the 99 African American mothers with HIV/AIDS. Eligibility criteria included a CD4 count of less than 600, as well as no history of intravenous drug use within the past 6 months. Mothers ranged in age from 18 to 45 years, (M = 30.73, SD = 5.11), 33% had less than a high school education, and reported an average monthly income of $613.22 (SD = 397.98). Additional demographic data are included in Table 1.
Measures
Focus groups and pilot testing were conducted prior to selecting measures to ensure cultural sensitivity for the sample population. Measures that had not been previously used with similar samples were subjected to confirmatory factor analysis and items loading at .40 or higher were retained. Coefficient alphas for the modified scales were computed. Participants were given cue cards with descriptors (e.g., “not true,” “often true”), numeric anchors, and illustrated aids (e.g., shaded thermometers) to assist them in responding to the items.
Demographic Information and Medication Status
Information related to age, education, number and age(s) of children, and income was collected from all participating mothers. Information related to current use of antiretroviral medications was obtained from medical records.
Immune Functioning
T-helper cell count (CD4) was derived from the participating mothers’ medical records. The average amount of time between serum collection and assessment date (i.e., interview) was one month.
Optimism
The Life Orientation Test (LOT; Scheier & Carver, 1985) is an 8-item self-report instrument developed to measure the construct of dispositional optimism, a moderator variable being tested in the current study. The items are presented as statements to which participants respond by rating their level of agreement with each statement. The LOT has been found to have adequate internal consistency (alpha = .76) and test-retest reliability (alpha = .79) (1985). Anchors on the scale range from (0) Strongly disagree to (4) strongly agree. Four of the items are positively worded, including: “you always look on the bright side of things” and four of the items are negatively worded and require reverse scoring: “things never work out the way you want them to.” Higher scores reflect higher levels of optimism. Coefficient alpha obtained for the LOT at Assessment 1 (alpha = .76) indicated adequate internal consistency.
Depressive Symptoms
Depressive symptoms were measured using both clinician ratings and mothers’ self report. The Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960) was used to provide a clinician-rated measure of depressive symptoms. The HRSD is a widely used 17-item clinician-rated measure of depressive symptoms and is often used to provide a single ‘total’ score for depressive symptoms (Marsella, Hirschfeld, & Katz, 1987). Because 7 of the items on the HRSD are structured to assess somatic complaints that may have significant overlap with HIV-related symptoms (e.g., sleep disturbance), analyses were conducted twice, with and without the 7 somatic items. The following 7 items were controlled for in the analysis excluding somatic items: [Sleep, psychomotor retardation, somatic, gastrointestinal, genital, and ‘general’ symptoms (e.g., backache, fatigue)]. Interrater reliability for the HRSD was .77.
Self-report of depressive symptoms was measured using the depression subscale of the Brief Symptom Inventory (BSI; Derogatis & Spencer, 1982). The depression subscale is one of 9 subscales of the 53-item BSI and contains a total of 20 items to which participants rate the level that they have been bothered by each during the past 7 days. Items are rated from (0) not at all to (3) extremely and include: “trouble with your mind going blank” and “feelings of guilt.” Scores on the depression subscale range from 0 to 60, with higher scores indicating more elevated levels of depressive symptomology. Coefficient alpha for the BSI was .82.
Physical Health Symptoms
A revised version of the Physical Symptoms Inventory (PSI; Wahler, 1969) was used to provide a measure of self-reported physical symptoms, the dependent variable in the current study. The PSI is structured to assess perceived physical health concerns. Respondents provide a rating of the extent to which they have experienced or have been bothered by a range of physical symptoms. Items are rated on a 4-point Likert scale and range from (0) almost never to (4) nearly everyday.
Both directions and items on the PSI were altered to facilitate the oral administration of the measure and address issues related to cultural sensitivity. The PSI was reviewed with focus groups whose feedback prompted investigators to add four items related to women’s health (i.e., vaginal discharge) and to delete seven items, rendering a modified version containing 39 items. Scores on the modified PSI range from 0 to 139 (see Table 1). A confirmatory factor analysis was conducted on the items of this modified measure. Items loading at .40 or higher were retained in the current analyses. A coefficient alpha of .91 was obtained for the measure.
Procedures
African American mothers with HIV were approached at a public health clinic (93%), as well as private medical practices (7%), regarding their participation in this study. During regularly scheduled checkups, eligible women were approached by a member of the project team and given information regarding the study. Once eligibility was verbally confirmed, interested women were scheduled for an interview with a member of the project staff.
All interviews were conducted in a medical setting. At the start of the interview, participants reviewed and signed an approved consent form. Upon completion of the consent agreement, participants engaged in a sociological interview during which demographic information was obtained. This interview lasted approximately one hour and participants received $50 for their time.
The second interview, the psychological interview, was generally scheduled within two weeks of the initial sociological interview. This session included administration of the measures assessing the major constructs of interest in the current study, the HRSD, the BSI, and the PSI. In addition to the interview, participants’ medical records were reviewed to obtain the most recent CD4 count and current antiretroviral drug regimen.
Results
Preliminary Analyses
Lifetime history of street drugs, as well as genital ulcers and lymphadenopathy, were positively associated with physical symptoms, the outcome of interest. Participants who endorsed prior history of drug use (r = .32, p < .05), had a diagnosis of lymphadenopathy (r = .21, p < .05), or a diagnosis of genital ulcers (r = .32, p < .05) were more likely to endorse physical symptoms (see Table 1).
Bivariate associations between major study variables (CD4, optimism, and depressive symptoms) and the outcome of interest, physical symptoms, were also examined (see Table 1). The proposed independent variable, CD4 count, was not associated with physical symptoms (r = −.09, ns) in the bivariate analyses. In addition, optimism was not associated with physical symptoms (r = .17, ns). However, both self-reported (r = .60, p < .001) and clinician-rated (r = .52, p < .001) depressive symptoms were significantly associated with the physical health symptoms. Higher levels of depressive symptoms were associated with higher levels of physical symptoms.
Primary Analyses
Separate hierarchical regression analyses were conducted to examine the moderating roles of optimism and depressive symptoms. In addition, analyses for depressive symptoms were repeated for self-reported and clinician-rated depressive symptoms (controlling for vegetative items). Lifetime history of street-drug use, as well as the diagnoses of genital ulcers and lymphadenopathy, were entered into Block 1. CD4 count was entered into Block 2 and the proposed moderator variables were entered into Block 3 (optimism or depressive symptoms). In Block 4, the 2-way interactions (CD4 × optimism, CD4 × depressive symptoms) were entered. All of the variables entered into the interaction terms were first centered in order to control for multicollinearity (Baron & Kenny, 1986).
No significant main effect emerged for the impact of CD4 on physical symptoms, β = −.02, ns (see Tables 2 and 3). Individuals with more compromised immune functioning did not report more physical symptoms. Consistent with prior research with this sample, a significant main effect of depressive symptoms emerged, with higher levels of depressive symptoms, measured with either the HRSD, β = .60, p < .001, or the BSI, β = .52, p < .001, associated with elevated physical symptoms. These findings, however, must be interpreted within the context of the significant interaction obtained for CD4 count and depressive symptoms, measured both with self-report and clinician-rating.
A significant interaction between CD4 count and self-reported depressive symptoms, measured with the depression subscale of the BSI, emerged, β = −.19, p < .05 (Table 2). As per the recommendations of Aiken and West (1991), two regression lines were plotted for low (1 SD below mean) and high (1 SD above mean) values of the moderator (BSI-High and BSI-Low) at low and high values of the independent variable (CD4). The slope and intercept for each line were obtained using the web-based slope calculator for hierarchical multiple regression (Preacher, Curran, & Bauer, 2006). The slope for the value of the BSI-High line (1 SD above the mean) was significantly different from zero, t = −2.11, p < .05, indicating that CD4 count was significantly associated with physical symptoms among BSI-High women. The slope for the BSI-Low line (one SD below the mean) did not differ significantly from zero, t = −1.29, ns, indicating that CD4 was not significantly associated with physical symptoms among BSI-Low women. At higher levels of depressive symptoms, CD4 count was a representative marker of physical symptoms, but not under low levels of depressive symptoms.
Hierarchical regression analyses were repeated to examine the impact of immune functioning on physical symptoms and the moderating role of depressive symptoms, using the HRSD (see Table 3). All items on the HRSD, both vegetative and cognitive, were initially included in the analyses. A significant 2-way interaction emerged: HRSD × CD4, β = −.17, p < .05. Analyses were repeated to examine whether the relation would remain significant after controlling for somatic symptoms (vegetative items). The two-way interaction between depressive symptoms and CD4 count remained significant, β = −.18, p < .05.
The two-way interaction of depressive symptoms and CD4 count was explicated by repeating the procedure described above for testing the slopes of both high and low values of depression. High and low values of the HRSD (HRSD-High and HRSD-Low) were plotted using values of one standard deviation above and below the mean, respectively. The slope calculator revealed that the slope calculated with HRSD-High was significantly different from zero, t = 2.53, p < .05, while the slope for HRSD-Low did not differ significantly from zero, t = 1.25, ns.
The relation between CD4 count and physical symptoms emerged only at high levels of depressive symptoms. This finding is consistent with the significant interaction obtained using the BSI to measure depressive symptoms. These results suggest that after controlling for potential somatic overlap between symptoms of depression and physical symptoms of HIV/AIDS, clinician-rated depressive symptoms exacerbated the link between immune functioning and physical health symptoms, such that women with high levels of clinician-rated depressive symptoms and low CD4 counts endorsed elevated levels of physical health symptoms. This relation was not detected at low levels of clinician-rated depressive symptoms.
Hierarchical linear regression analyses were repeated to examine the impact of optimism on physical symptoms and the moderating role of optimism, using the LOT (see Table 4). Optimism did not emerge as a significant predictor of physical symptoms and did not moderate the relation between immune functioning and physical symptoms.
Discussion
This study examined optimism and depressive symptoms as moderators of the association between immune functioning (CD4 count) and physical health symptoms among low-income, African American mothers with HIV/AIDS. Findings revealed a significant main effect of depressive symptoms, but not CD4 count, on physical health symptoms. Of primary interest, there was a significant interaction of CD4 count and depressive symptoms which was replicated using both a self-report and clinician-rating of depressive symptoms. In contrast, there was no main effect for optimism and optimism did not interact with CD4 count to account for variability in physical symptoms.
Noteably, CD4 count was not a correlate of physical health symptoms among African American mothers with HIV/AIDS in the current study. To date, only a handful of studies have examined the potential link between CD4 count and self-reported physical health and findings are equivocal. Cruess et al. (2000) reported a link between lower levels of T-suppressor/cytotoxic cells and higher severity of physical health symptoms. Lee et al. (2001) found evidence for a link between CD4 count and certain physical health symptoms (e.g., increased daytime sleepiness) among a sample characterized by low income and high rates of unemployment that included a relatively large percentage of African American women (58%). These findings, though limited in breadth, support the notion that physical health symptoms may be moderated by a third variable, including those examined in the current study: optimism and depressive symptoms.
We found support for the moderating role of depressive symptoms on the association between CD4 count and physical health symptoms. The combination of lower CD4 counts and depressive symptoms was associated with more physical complaints among mothers with HIV/AIDS, relative to mothers with lower CD4 counts and lower levels of depressive symptoms, or women with higher CD4 counts, regardless of their level of depressive symptoms. Although future research must begin to examine the specific mechanisms by which depressive symptoms moderate the link between CD4 count and physical health symptoms, one possibility is that mothers with higher levels of depressive symptoms may have demonstrated characteristic alterations in immune functioning and immune response associated with depression (see Herbert & Cohen, 1993; Weisse, 1992 for reviews). These mothers may have, in turn, demonstrated a greater vulnerability to the physical impact of suppressed CD4 counts. Additionally, mothers with higher levels of depressive symptoms may have been less likely to engage in physical exercise, select healthful food choices, seek out positive social support persons, engage in pleasant activities, and/or adhere to treatment (e.g., Cohen & Rodriquez, 1995; Cook et al., 2006; Kiecolt-Glasser et al., 2002). The impact of failing to engage in health-promoting behaviors may have resulted in elevated physical health symptoms among women with greater immunological vulnerability.
Contrary to the findings for depressive symptoms, optimism did not moderate the associated between CD4 count and physical symptoms among African American mothers in the sample. One possibility for the failure to support our hypotheses regarding the moderating role of optimism is that depressive symptoms overshadowed the impact of optimism on physical symptoms such that women who were experiencing significant depressive symptomology may not have experienced the potentially protective benefits of optimism as it might relate to physical functioning. That is, although optimism has been shown to function as a protective factor related to positive health outcomes (see Peterson 2001, for a review), when the impact of optimism on physical functioning is examined among African American women with HIV/AIDS who are at higher risk for depressive symptomology, the potentially protective impact of the construct may have been overshadowed by the role of depressive symptoms. In addition, although optimism has been associated with uniformly positive outcomes for individuals with other illnesses, the findings regarding the role of optimism among individuals with HIV/AIDS has been somewhat more inconsistent. For example, while some studies have shown that optimism is associated with lower levels of distress among individuals with HIV/AIDS (e.g., Johnson & Endler 2002), other studies have linked optimism to potentially health-compromising behaviors, including elevated sexually risk taking and medication non-adherence (i.e., Holmes & Pace 2002). Third, although to our knowledge optimism has not been examined as a moderator of the link between CD4 count and physical health complaints, several studies have examined the impact of optimism on CD4 count and report rather inconsistent findings. An investigation of the relation between dispositional optimism and CD4 count over time found no relation between the two variables among gay men with HIV/AIDS (Tomakowsky, Lumley, Markowitz, & Frank, 2001). In contrast, another longitudinal investigation revealed that moderate levels of optimism predicted higher CD4 counts over time (Milam, Richardson, Marks, Kepmer, & McCutchan, 2004). Although not directly relevant to the current investigation, the inconsistent findings of these studies suggest that the link between optimism and markers of HIV/AIDS disease progression may, in turn, be moderated by yet another variable, such as environmental stress (e.g., Segerstrom, 2001). Given the lack of tangible resources, chronic environmental stressors, and the progressive nature of their disease, the impact of variables such as optimism may have operated differently, relative to populations with fewer psychological and physical health-related risk factors.
All findings discussed in the current study must be considered within the context of its limitations. First, the current findings may not be generalized beyond a community-sample of low-income, African-American mothers with HIV/AIDS. Conclusions made related to the role of psychosocial moderators in the relation between immune functioning and physical health symptoms may not apply to other groups or populations living with HIV/AIDS, including women experiencing clinical levels of depression. Second, this study examined only one marker of immune functioning, CD4 count. Future research should replicate the findings with other immune measures (e.g., viral load). Third, this study examined only one psychosocial moderator of CD4 and physical health symptoms, depressive symptoms. The examination of the other psychosocial moderators of this association is a promising research direction with this high risk group. In addition, null findings for optimism may be attributable to the psychometrics of the LOT in the current sample which was significantly lower than the other measures used in the study. Finally, cross-sectional examination of data prevents the examination of causal relationships among the study variables.
Despite the limitations, several strengths should be recognized. First, the current study contributes to understanding the immunological and psychosocial factors associated with physical health symptoms among a relatively understudied group, low-income, inner city African American mothers. In addition, these findings underscore the role of clinical psychologists in screening for and managing depressive symptoms among African American mothers living with HIV/AIDS. Third, confidence in the findings is strengthened by the consistency of findings across two measures of depressive symptoms and both before and after controlling for vegetative symptoms.
The findings of the current study suggest an important opportunity for clinical psychologists working in medical settings to intervene. The appropriate assessment and treatment of depressive symptoms, including behavioral or pharmacological interventions, provide an opportunity to modify the impact of immune functioning on physical health symptoms. These interventions will presumably result in improving both physical and mental health functioning and improved quality of life among a group disproportionately affected by HIV/AIDS.
References
Aiken, L. S., & West, S. G. (1991). Multiple regression: Testing and interpreting interactions. Thousand Oaks: Sage.
American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author.
Ashton, E., Vosvick, M., Chesney, M., Gore-Felton, C., Koopman, C., O’Shea, K., et al. (2005). Social support and maladaptive coping as predictors of the change in physical health symptoms among persons living with HIV/AIDS. AIDS Patient Care and STDs, 19, 587–598. doi:10.1089/apc.2005.19.587.
Baron, R. M., & Kenny, D. A. (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51, 1173–1182. doi:10.1037/0022-3514.51.6.1173.
Berkan, S., Cohen, M., Back, S., Fitzgerald, G., Feldman, J., Young, M., et al. (2001). Experience and covariates of depressive symptoms among a cohort of HIV infected women. Social Work in Health Care, 32, 93–111.
Boarts, J. M., Sledjeski, E. M., Bogart, L. M., & Delahanty, D. L. (2006). The differential impact of PTSD and depression on HIV disease markers and adherence to HAART in people living with HIV. AIDS and Behavior, 10, 253–261. doi:10.1007/s10461-006-9069-7.
Breitbart, W., McDonald, M., Stein, K., Calle, J., Passik, S., Rosenfield, B., et al. (1996). Correlates of depression in women with AIDS. Psychosomatics, 37, 198–199.
Caces, M. F., Harford, T. C., & Aitken, S. S. (1998). Prescription and non-prescription drug use: A longitudinal study. Substance Abuse, 10, 115–126.
Carver, C. S., & Scheier, M. F. (2003). Optimism. In S. J. Lopez & C. R. Snyder (Eds.), Positive psychological assessment: A handbook of models and measures (pp. 75–89). Washington, D.C.: American Psychological Association.
Centers for Disease Control and Prevention. (2005). HIV/AIDS surveillance report, 2005 (Vol. 17). Atlanta: US Department of Health and Human Services, CDC; 2006:1–46.
Cohen, S., & Rodriquez, M. A. (1995). Pathways linking affective disturbance and physical disorders. Health Psychology, 14, 374–380. doi:10.1037/0278-6133.14.5.374.
Cook, J. A., Grey, D., Burke-Miller, J., Cohen, M. H., Anastos, K., Gandhi, M., et al. (2006). Effects of treated and untreated depressive symptoms on highly active antiretroviral therapy use in a US multi-site cohort of HIV positive women. AIDS Care, 18, 93–100. doi:10.1080/09540120500159284.
Corea, G. (1992). The invisible epidemic: The story of women and AIDS. New York: Harper Collins.
Cruess, S., Antoni, M., Kilbourn, K., Ironson, G., Klimas, N., Fletcher, M., et al. (2000). Optimism, distress, and immunologic status in HIV-infected gay men following Hurricane Andrew. Behavioral Medicine (Washington, D.C.), 7, 160–182.
Cruess, D. G., Petitto, J. M., Leserman, J., Douglas, S. D., Gettes, S. D., Ten Have, T. R., et al. (2003). Depression and HIV infection: Impact on immune function and disease progression. CNS Spectrums, 8, 52–58.
Cunningham, W. E., Shapiro, M. F., & Hays, R. D. (1998). Constitutional symptoms and health-related quality of life in patients with symptomatic HIV disease. The American Journal of Medicine, 104, 129–136. doi:10.1016/S0002-9343(97)00349-5.
Derogatis, L. R., & Spencer, P. M. (1982). The Brief Symptom Inventory (BSI) administration, score, procedures manual–I. Baltimore: Johns Hopkins University School of Medicine, Clinical Psychometrics Research Unit.
Family Health Project Research Group. (1998). A multidisciplinary longitudinal investigation of children whose mothers are HIV infected. Clinical Psychology Review, 18, 839–856. doi:10.1016/S0272-7358(98)00018-X.
Faucett, J., Gordon, N., & Levine, J. (1994). Differences in post-operative pain severity among four ethnic groups. Journal of Pain and Symptom Management, 9, 383–389. doi:10.1016/0885-3924(94)90175-9.
Forehand, R., Jones, D. J., Kotchick, B. A., Armistead, L., Morse, E., Morse, P. S., et al. (2002). Non-infected children of HIV-infected mothers: A four year longitudinal study of child psychosocial adjustment and parenting. Behavior Therapy, 33, 579–600.
Fulk, L. J., Kane, B. E., Phillips, K. D., Bopp, C. M., & Hand, G. A. (2004). Depression in HIV infected patients allopathic, complementary, and alternative treatments. Journal of Psychosomatic Research, 57, 339–351.
Hamilton, M. (1960). A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry, 23, 56–61.
Herbert, T. B., & Cohen, S. (1993). Depression and immunity: A meta-analytic review. Psychological Bulletin, 113, 472–486.
Ickovics, J. R., Hamburger, M. E., Vlahov, D., Schoenbaum, E., Schuman, P., & Boland, R. J. (2001). Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women. Journal of the American Medical Association, 285, 1466–1474.
Jones, D. J., Beach, S. R. H., & Forehand, R. (2001a). HIV infection and depressive symptoms: An investigation of African American single-mothers. AIDS Care, 13, 343–350.
Jones, D. J., Beach, S. R. H., & Forehand, R. (2001b). Disease status in African American single mothers with HIV: The role of depressive symptoms. Health Psychology, 20, 417–423.
Jones, D. J., Foster, S. A., Zalot, A., Chester, C., & King, A. (2007). Knowledge of maternal HIV/AIDS and child adjustment: The moderating role of mother-child relationship quality. AIDS and Behavior, 11, 409–420.
Jones, D. J., O’Connell, C., Gound, M., Heller, L., & Forehand, R. (2004). Predictors of self-reported physical symptoms in low-income, inner-city African American women: The role of optimism, depressive symptoms, and chronic illness. Psychology of Women Quarterly, 28, 112–121.
Justice, A. C., Chang, C. H., Rabeneck, L., & Zackin, R. (2001). Clinical importance of provider-reported HIV symptoms compared with patient-report. Medical Care, 39, 397–408.
Kaplan, S. H., Sullivan, L. M., Spetter, D., Dukes, K. A., Khan, A., & Greenfield, S. (1996). Gender and patterns of physician-patient communication. In M. M. Falik & K. S. Collins (Eds.), Women’s health: The Commonwealth Fund survey (pp. 76–95). Baltimore, MD: Johns Hopkins University Press.
Kiecolt-Glasser, J. K., McGuire, L., Robles, T. F., & Glaser, R. (2002). Emotions, morbidity, and mortality: New perspectives from psychoneuroimmunology. Annual Review of Psychology, 53, 83–107.
Kroenke, K., & Spitzer, R. L. (1998). Gender differences in the reporting of physical and somatoform symptoms. Psychosomatic Medicine, 60, 150–155.
Lauver, D., & Tak, Y. (1995). Optimism and coping with a breast cancer symptom. Nursing Research, 44, 202–207.
Lee, K. A., Portillo, C. J., & Miramontes, H. (2001). The influence of sleep and activity patterns on fatigue in women with HIV/AIDS. Journal of the Association of Nurses in AIDS Care, 12, 19–27.
Marsella, A. J., Hirschfeld, R. M., & Katz, M. (1987). The measurement of depression. New York: Guilford Press.
McCraken, L. M., Matthews, A. K., Tang, T. S., & Cuba, S. L. (2001). A comparison of blacks and whites seeking treatment for chronic pain. Clinical Journal of Pain, 17, 249–255.
Peterson, C. (2000). The future of optimism. American Psychologist, 55, 44–55.
Preacher, K. J., Curran, P. J., & Bauer, D. J. (2006). Computational tools for probing interaction effects in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics, 31, 437–448.
Scheier, M., & Carver, C. S. (1985). Optimism, coping and health: Assessment and implications of generalized outcome expectancies. Health Psychology, 4, 219–247.
Segerstrom, S. C. (2001). Optimism, goal conflict, and stressor-related immune change. Journal of Behavioral Medicine, 24, 441–467.
Spiegel, D., Israelski, D. M., Power, R., Prentiss, D. E., Balmas, G., & Muhammad, M. (2003). Acute stress disorder, PTSD, and depression in a clinic samples of patients with HIV/AIDS. Journal of Psychosomatic Research, 55, 128.
Tomakowsky, J., Lumley, M. A., Markowitz, N., & Frank, C. (2001). Optimistic explanatory style and dispositional optimism in HIV-infected men. Journal of Psychosomatic Research, 51, 577–587.
Wahler, H. J. (1969). The Physical Symptoms Inventory: Measuring levels of somatic complaining behavior. Journal of Clinical Psychology, 24, 207–211.
Weisse, C. S. (1992). Depression and immunocompetence: A review of the literature. Psychological Bulletin, 111, 475–489.
Wu, A. W., Hays, R. D., Kelly, S., Malitz, F., & Bozzette, S. A. (1997). Applications of the medical outcomes study health-related quality of life measures in HIV/AIDS. Quality of Life Research, 6, 531–554.
Acknowledgments
This manuscript includes analyses completed as part of the doctoral dissertation of Cara O’Connell-Edwards under the mentorship of Deborah J. Jones. Funding for this project was provided by the Centers for Disease Control and Prevention (Rex Forehand, PI) and the Institute for Behavioral Research at the University of Georgia. Additional funding for manuscript analyses and preparation was provided by the Ethnicity, Culture, and Health Outcomes, the University Research Council and the Centers for AIDS Research at the University of North Carolina at Chapel Hill.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
O’Connell-Edwards, C., Jones, D.J., Forehand, R. et al. CD4 Count and Physical Symptoms Among Urban African American Mothers with HIV: An Examination of the Role of Optimism and Depressive Symptoms. J Clin Psychol Med Settings 15, 322–330 (2008). https://doi.org/10.1007/s10880-008-9133-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-008-9133-8