Abstract
Non-reassuring fetal heart rate tracings reflect an imbalance between the parasympathetic and sympathetic nervous systems. In this situation, fetal asphyxia can be suspected and may be confirmed by metabolic measurements at birth like low pH or high base deficit values. The objective of this study was to determine whether fetal asphyxia during labor is related to parasympathetic nervous system activity. This is a retrospective study of a database collected in 5 centers. Two hundred and ninety-nine fetal heart rate tracings collected during labor were analyzed. Autonomic nervous system, especially the parasympathetic nervous system, was analyzed using an original index: the FSI (Fetal Stress Index). The FSI is a parasympathetic activity evaluation based on fetal heart rate variability analysis. Infants were grouped based on normal or low pH value at birth. FSI was measured during the last 30 min of labor before birth and compared between groups. The minimum value of the FSI during the last 30 min before delivery was significantly lower in the group with the lower umbilical cord arterial pH value. In this pilot study during labor, FSI was lower in the group of infants with low arterial pH at birth.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
During pregnancy and labor the fetus can be deprived of an adequate supply of oxygen. When fetal asphyxia is suspected it can be confirmed by metabolic measurements at birth like a low pH or a high base deficit in umbilical cord arterial blood [1]. Since the central nervous system and cardiovascular system are very sensitive, small changes in oxygen levels can result in severe neurosensory disorders like cerebral palsy, or even death of the newborn [2].
One serious consequence of anoxia in the fetus is metabolic acidosis which alters fetal heart rate (FHR) and fetal heart rate variability (HRV) [3] including heart rate pattern reductions in variability, decelerations, bradycardia, or tachycardia [4, 5]. Visual inspection of FHR by medical professionals during labor is the most common clinical assessment to evaluate the risk of acidosis. The American College of Obstetricians and Gynecologists (ACOG), the International Federation of Gynecology and Obstetrics (FIGO) and the Royal College of Obstetricians and Gynaecologists (RCOG) recommend a grid classification system based on FHR visual interpretation [6–8]. However, visual analysis is subject to a poor inter- and intra-observer agreement [9–11].
Several authors investigated computerized HRV analysis methods for fetal autonomic state evaluation and showed significant changes fetal HRV when fetal acidemia occurred [12–16]. As such, our first objective was to develop a non-invasive HRV based-technology for measurement of parasympathetic activity in fetuses. Based on work done with adults, this technology allows quick computation of an index that reflects parasympathetic activity variations. In brief, during a stressful situation such as pain, the index falls as parasympathetic activity decreased [17, 18]. Changes in parasympathetic activity measured with our index can predict the intensity of postoperative pain [19] and can be used in conscious patient for pain and/or stress assessment [20, 21]. Recently, this technology has been adapted to the particular context of newborn infant wellbeing monitoring. The index was significantly reduced in newborns presenting significant behavioral postoperative pain [22, 23], and was increased after a nursing care known to activate the parasympathetic activity in neonates (handling and listening to human voice) [24]. The aim of this study was to investigate the fetal parasympathetic activity by computerized HRV analysis relative to fetal acidemia. We hypothesized that fetuses with low pH values will present low parasympathetic activity evaluated by our HRV method.
2 Methods
2.1 Population
This study used a database of 299 FHR records obtained for routine medical purposes in 5 centers (Lille, Valenciennes, Saint Vincent de Paul, Robert Debré, Poissy-St-Germain, France) from November 2003 to February 2005.
For the database records, after informed consent, women in labor were connected to cardiotocograph (CTG; Philips™ series 50, Philips Medical Systems™, Böblingen, Germany) for continuous FHR recording using ultrasound probes. Inclusion criteria were singleton pregnancies between 36 and 42 weeks of gestation with cephalic presentation. The FHR recordings obtained were issued from Philips™ series 50 CTG connected to a personal computer (Toshiba Satellite Pro, Toshiba™, Japan) for data acquisition and storage. All fetal heart rate tracing were performed by ultrasound Doppler. All the records from this database showed a good signal quality. Maternal parameters including age, parity, gestational age, mode of delivery, and expulsion duration (period between the beginning of expulsive efforts and birth), were collected. Neonatal parameters including birth weight and Apgar score were also reported. Blood samples were collected from the umbilical cord artery and vein at birth in order to determine pH values, pO2, pCO2, and Base Deficit (BD blood). Data were sourced from medical chart. This study was approved by the French committee of obstetrics and gynaecology research ethics (CEROG OBS 2015-11-18).
2.2 Description of the FHR analysis method
HRV is mediated by the parasympathetic and sympathetic nervous system. High frequency FHR variations (>0.15 Hz) [25, 26] correspond to parasympathetic activity only whereas low frequency FHR variations (0.04–0.15 Hz) are related to both parasympathetic and sympathetic activity. The very low frequency variations (<0.04 Hz) are related to thermoregulatory and endocrine activities [27–30]. Our HRV based technology is already validated in adults and newborn infants [17–24] and was recently adapted for the evaluation of parasympathetic activity changes in fetuses.
Most of the published methods are based on a spectral analysis of HRV [31–33]. Our analysis consists of a filtering method followed by a continuous analysis of the filtered signal magnitude in the time domain. The following paragraph describes this technology adaptation for the calculation of fetal HRV named FSI (Fetal Stress Index).
The FSI index is based on continuous FHR analysis. FHR values are transformed into time interval in millisecond.
The time series are then re-sampled at an 8 Hz sampling frequency and isolated in a 64 s moving window. The time series is then mean centered:
and normalized:
The resulting T″i series is then high pass filtered in order to isolate oscillations above 0.15 Hz.
We then obtain a time series representative of the FHR parasympathetic variations as shown in Fig. 1.
Local maximum and minimum are detected on this filtered signal and the lower and upper envelopes are plotted in order to compute the areas between envelopes A1, A2, A3 and A4 in four 16 s sub-windows. Amin is defined as the lowest of this 4 areas.
FSI is computed from Amin as: FSI = 100 × (5.1 × Amin + 1.2)/12.8 in order to obtain a 0–100 numerical value reflecting the visual aspect of the filtered time series. Continuous computation is assumed by sliding the moving window with a 1 s moving period.
High FSI values (near 100) correspond to an important parasympathetic activity, whereas a decrease of FSI corresponds to a decrease of the parasympathetic activity.
2.3 Data analysis
The minimum, maximum and mean values of FSI (respectively FSImin, FSImax and FSImean) were computed for the last 30 min before delivery.
Kitlinski et al. [34] demonstrated a physiological linear decline of umbilical cord arterial pH with gestational age and propose gestational age-adjusted pH thresholds. For this study, we therefore decided to group infants based on low or normal umbilical cord arterial pH values using the gestational age-adjusted pH thresholds (pHGA) proposed by Kitlinski et al. [34].
2.4 Statistical analysis
All data are presented as median (1st–3rd quartile). We used non parametric Mann–Whitney tests to compare each parameter and χ2 or Fisher tests were performed for binary parameters. Probability values less than P < 0.05 were considered significant. Data were analyzed using SPSS 20.0 (IBM, Armonk, NY, USA).
3 Results
3.1 Description of the population
All maternal characteristics (birth weight, parity, gestational age, delivery mode…) were similar between the groups (Table 1). The proportion of newborns with an Apgar score ≤ 7 at 1 min was significantly higher in the group pH ≤ pHGA (P = 0.006) but no difference was observed for Apgar scores at 5 min.
3.2 FSI variations
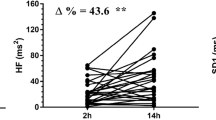
FSImin and FSImean were significantly lower in the low pH values group [P = 0.018 and P = 0.031, (Table 2)].
4 Discussion
We compared the FSI maximum, minimum, and mean values computed 30 min before delivery between groups with low and normal pH values. We found that both the minimum and mean values of the FSI were significantly lower for the low pH group. This suggests that low high frequency variations measured with FSImin and FSImean are consistent with fetal acidemia. The fetus can develop metabolic mechanisms in order to compensate oxygen deficit. During the first steps of hypoxia, chemoreceptors are activated and a bradycardia may be observed following a vagal response [35]. At the same time, the activation of α-adrenergic receptors induces a peripheral vasoconstriction that results in a redistribution of blood flow to brain, heart, and adrenals; and generated a hypertension. Then, baroreceptors are stimulated in order to decrease heart rate. Catecholamines are secreted in response to the sympathetic stimulation, heart rate is increased and glycogenolysis is activated. If the lack of oxygen increases, because of the anaerobic metabolism used in cells, a metabolic acidosis can appear. It causes an important activation of the sympathetic nervous system. The sensitivity of chemoreceptors and baroreceptors is decreased, the role of the autonomic nervous system is reduced (intensity of sympathetic and parasympathetic messages is mitigated) resulting in late heart rate decelerations and slower recuperation [36]. HRV is dramatically reduced [37, 38] and the fetus presents a high risk of sequelae. As pO2 modifications exist, fetuses engage physiological adaptation mechanisms that will have an effect on the heart rate via the autonomic nervous system. In this study, we evaluated the relative parasympathetic activity using an index between 0 and 100. Our main result is a decrease of FSI during the last 30 min of labor for fetuses born with low arterial umbilical cord pH values. In other words, the drop in FSI were more pronounced for fetuses with pH ≤ pHGA. We can assume that these data reflect the decreasing intensity of autonomic nervous system caused by a lack of oxygen.
HRV analysis methods have been used for fetal acidosis diagnosis. These methods are based on time or frequency domain analysis of fetal HRV [39]. Ayres-de-Campos et al. [40] estimated short term and long term variability (STV and LTV) in the time domain to predict neonatal outcome. They demonstrated that both STV and LTV varied with newborns with low arterial pH and low Apgar scores. Furthermore, Galazios et al. [41] found a decreased STV in the low umbilical arterial pH at birth group. When using frequency domain analysis methods there is inconsistency in the literature. Some authors found a decrease in the low frequencies [12], or a decrease in very low, low and high frequencies [31] and others did not find any modifications [13]. In several studies, an increase of low frequencies and a decrease of high frequencies were observed in case of fetal acidemia [15, 16, 32]. Our data support these results and are consistent with our hypothesis that lower FSI are found in infants with low pH at birth.
The comparisons between FHR analysis methods should be interpreted carefully because FHR signal acquisition and processing techniques vary widely. For example, Siira et al. [32] investigated fetal HRV through a spectral analysis using invasive fetal scalp electrodes whereas Chung et al. [31] performed a spectral analysis on the FHR signal issued from the Doppler ultrasound CTG. Doppler ultrasound CTG does not provide beat-to-beat FHR recordings; and FHR is usually averaged over 3 beats and sampled at 4 Hz. According to Van Laar et al. [25] FHR high frequency spectral analysis is only reliable if FHR is acquired on a beat-to-beat basis and issued from direct ECG signal obtained with a scalp electrode suggesting results using FHR that are averaged should be interpreted with caution. Other authors described time domain signal processing methods allowing the use of FHR signal issued from the Doppler ultrasound CTG [40, 41]. As our method is also based on a time domain analysis, we hypothesized that Doppler ultrasound CTG signal will be suitable for our analysis.
One limitation of our study is that we only listed one case of severe acidosis with an arterial pH at birth under 7.00 (6.91) and 12 newborns with pH values lower than the gestational age adapted threshold. However, despite this low number of severe acidosis, we showed a reduction of the FSI in the case of low pH values.
Though, this pilot study demonstrated the feasibility of computing the FSI non-invasively from FHR issued from CTG, other studies need to be performed in order to compare FSI computed from FHR issued from a CTG to FSI computed from FHR acquired on a beat-to-beat basis issued from a fetal scalp electrode. Our data showed that parasympathetic tone, illustrated by the HRV-based index FSI, is reduced during labor when a low arterial pH at birth was found. We are currently working on improving our technology sensitivity using sheep instrumented models and we will perform a prospective study in a larger population in order to detect more precisely fetuses with potential distress during delivery.
References
MacLennan A. A template for defining a causal relation between acute intrapartum events and cerebral palsy: international consensus statement. BMJ. 1999;319:1054–9.
Mwaniki MK, Atieno M, Lawn JE, Newton CR. Long-term neurodevelopmental outcomes after intrauterine and neonatal insults: a systematic review. Lancet. 2012;379:445–52.
Durosier LD, Green G, Batkin I, Seely AJ, Ross MG, Richardson BS, Frasch MG. Sampling rate of heart rate variability impacts the ability to detect acidemia in ovine fetuses near-term. Front Pediatr. 2014;2:38.
Williams KP, Galerneau F. Intrapartum fetal heart rate patterns in the prediction of neonatal acidemia. Am J Obstet Gynecol. 2003;188:820–3.
Soncini E, Paganelli S, Vezzani C, Gargano G, Giovanni Battista LS. Intrapartum fetal heart rate monitoring: evaluation of a standardized system of interpretation for prediction of metabolic acidosis at delivery and neonatal neurological morbidity. J Matern Fetal Neonatal Med. 2014;27:1465–9.
Ayres-de-Campos D, Spong CY, Chandraharan E. FIGO consensus guidelines on intrapartum fetal monitoring: cardiotocography. Int J Gynaecol Obstet. 2015;131:13–24.
American College of Obstetricians and Gynecologists. Practice bulletin no. 116: Management of intrapartum fetal heart rate tracings. Obstet Gynecol. 2010;116:1232–1240.
Royal College of Obstetricians and Gynaecologists. The use of electronic fetal monitoring. The use of cardiotocography in intrapartum fetal surveillance. Evidence-based Clinical Guideline Number 8. Clinical Effectiveness Support Unit. 2001.
Gagnon R, Campbell MK, Hunse C. A comparison between visual and computer analysis of antepartum fetal heart rate tracings. Am J Obstet Gynecol. 1993;168:842–7.
Blackwell SC, Grobman WA, Antoniewicz L, Hutchinson M, Gyamfi BC. Interobserver and intraobserver reliability of the NICHD 3-tier fetal heart rate interpretation system. Am J Obstet Gynecol. 2011;205:378–500.
Rhose S, Heinis AM, Vandenbussche F, van Drongelen J, van Dillen J. Inter- and intra-observer agreement of non-reassuring cardiotocography analysis and subsequent clinical management. Acta Obstet Gynecol Scand. 2014;93:596–602.
Li X, Tang D, Zhou S, Zhou G, Wang C, Zhuang Y, Wu G, Shen L. Redistribution of power spectrum of heart rate variability during acute umbilical artery embolism and hypoxemia in late-gestation fetal sheep. Eur J Obstet Gynecol Reprod Biol. 2004;114:137–43.
Frasch MG, Muller T, Weiss C, Schwab K, Schubert H, Schwab M. Heart rate variability analysis allows early asphyxia detection in ovine fetus. Reprod Sci. 2009;16:509–17.
Kwon JY, Park IY, Shin JC, Song J, Tafreshi R, Lim J. Specific change in spectral power of fetal heart rate variability related to fetal acidemia during labor: comparison between preterm and term fetuses. Early Hum Dev. 2012;88:203–7.
van Laar JO, Peters CH, Vullings R, Houterman S, Bergmans JW, Oei SG. Fetal autonomic response to severe acidaemia during labour. BJOG. 2010;117:429–37.
Annunziata ML, Tagliaferri S, Esposito FG, Giuliano N, Mereghini F, Di LA, Campanile M. Computerized analysis of fetal heart rate variability signal during the stages of labor. J Obstet Gynaecol Res. 2016;42:258–65.
Jeanne M, Clement C, De Jonckheere J, Logier R, Tavernier B. Variations of the analgesia nociception index during general anaesthesia for laparoscopic abdominal surgery. J Clin Monit Comput. 2012;26:289–94.
Gruenewald M, Ilies C, Herz J, Schoenherr T, Fudickar A, Hocker J, Bein B. Influence of nociceptive stimulation on analgesia nociception index (ANI) during propofol-remifentanil anaesthesia. Br J Anaesth. 2013;110:1024–30.
Boselli E, Daniela-Ionescu M, Begou G, Bouvet L, Dabouz R, Magnin C, Allaouchiche B. Prospective observational study of the non-invasive assessment of immediate postoperative pain using the analgesia/nociception index (ANI). Br J Anaesth. 2013;111:453–9.
Le Guen M, Jeanne M, Sievert K, Al MM, Chazot T, Laloe PA, Dreyfus JF, Fischler M. The Analgesia Nociception Index: a pilot study to evaluation of a new pain parameter during labor. Int. J. Obstet. Anesth. 2012;21:146–51.
Rommel D, Nandrino JL, De Jonckheere J, Swierczek M, Dodin V, Logier R. Maintenance of parasympathetic inhibition following emotional induction in patients with restrictive type anorexia nervosa. Psychiatry Res. 2015;225:651–7.
Faye PM, De Jonckheere J, Logier R, Kuissi E, Jeanne M, Rakza T, Storme L. Newborn infant pain assessment using heart rate variability analysis. Clin J Pain. 2010;26:777–82.
De Jonckheere J, Rakza T, Logier R, Jeanne M, Jounwaz R, Storme L. Heart rate variability analysis for newborn infants prolonged pain assessment. Conf Proc IEEE Eng Med Biol Soc. 2011;2011:7747–50.
Alexandre C, De Jonckheere J, Rakza T, Mur S, Carette D, Logier R, Jeanne M, Storme L. Impact of cocooning and maternal voice on the autonomic nervous system activity in the premature newborn infant. Arch Pediatr. 2013;20:963–8.
van Laar JO, Porath MM, Peters CH, Oei SG. Spectral analysis of fetal heart rate variability for fetal surveillance: review of the literature. Acta Obstet Gynecol Scand. 2008;87:300–6.
Salamalekis E, Hintipas E, Salloum I, Vasios G, Loghis C, Vitoratos N, Chrelias Ch, Creatsas G. Computerized analysis of fetal heart rate variability using the matching pursuit technique as an indicator of fetal hypoxia during labor. J Matern Fetal Neonatal Med. 2006;19(3):165–9.
Malliani A, Pagani M, Lombardi F, Cerutti S. Cardiovascular neural regulation explored in the frequency domain. Circulation. 1991;84:482–92.
Akselrod S, Gordon D, Ubel FA, Shannon DC, Berger AC, Cohen RJ. Power spectrum analysis of heart rate fluctuation: a quantitative probe of beat-to-beat cardiovascular control. Science. 1981;213:220–2.
Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J. 1996;17:354–81.
Malik M, Camm AJ. Components of heart rate variability–what they really mean and what we really measure. Am J Cardiol. 1993;72:821–2.
Chung DY, Sim YB, Park KT, Yi SH, Shin JC, Kim SP. Spectral analysis of fetal heart rate variability as a predictor of intrapartum fetal distress. Int J Gynaecol Obstet. 2001;73:109–16.
Siira SM, Ojala TH, Vahlberg TJ, Jalonen JO, Valimaki IA, Rosen KG, Ekholm EM. Marked fetal acidosis and specific changes in power spectrum analysis of fetal heart rate variability recorded during the last hour of labour. BJOG. 2005;112:418–23.
van Laar JO, Peters CH, Houterman S, Wijn PF, Kwee A, Oei SG. Normalized spectral power of fetal heart rate variability is associated with fetal scalp blood pH. Early Hum Dev. 2011;87:259–63.
Kitlinski ML, Kallen K, Marsal K, Olofsson P. Gestational age-dependent reference values for pH in umbilical cord arterial blood at term. Obstet Gynecol. 2003;102:338–45.
Hanson M, Kumar P. Chemoreceptor function in the fetus and neonate. Adv Exp Med Biol. 1994;360:99–108.
Doret M, Constans A, Gaucherand P. Physiologic basis for fetal heart rate analysis during labour. J Gynecol Obstet Biol Reprod (Paris). 2010;39:276–83.
Sheen TC, Lu MH, Lee MY, Chen SR. Nonreassuring fetal heart rate decreases heart rate variability in newborn infants. Ann Noninvasive Electrocardiol. 2014;19:273–8.
van Laar, J. Fetal autonomic cardiac response during pregnancy and labour. 2012. Thesis.
Romano M, Iuppariello L, Ponsiglione AM, Improta G, Bifulco P, Cesarelli M. Frequency and time domain analysis of foetal heart rate variability with traditional indexes: a critical survey. Comput Math Methods Med. 2016;2016:9585431.
Ayres-de-Campos D, Costa-Santos C, Bernardes J. Prediction of neonatal state by computer analysis of fetal heart rate tracings: the antepartum arm of the SisPorto multicentre validation study. Eur J Obstet Gynecol Reprod Biol. 2005;118:52–60.
Galazios G, Tripsianis G, Tsikouras P, Koutlaki N, Liberis V. Fetal distress evaluation using and analyzing the variables of antepartum computerized cardiotocography. Arch Gynecol Obstet. 2010;281:229–33.
Acknowledgements
We acknowledge all the medical staff who participated to the data collection: Monaco maternity (Valenciennes, France), Saint Vincent-de-Paul hospital (Lille, France), Jeanne de Flandre maternity (Lille, France), Poissy-Saint-Germain hospital (Poissy, France) and Robert-Debré hospital (Paris, France).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
JDJ and RL are shareholders and LB was a team member of Mdoloris Medical Systems (that commercializes ANI and NIPE monitors which are based on the presented technology). The remaining authors report no conflict of interest.
Ethics approval
The present retrospective study was approved by the French committee of obstetrics and gynaecology research ethics (CEROG OBS 2015-11-18).
Rights and permissions
About this article
Cite this article
Butruille, L., De jonckheere, J., Flocteil, M. et al. Parasympathetic tone variations according to umbilical cord pH at birth: a computerized fetal heart rate variability analysis. J Clin Monit Comput 31, 1197–1202 (2017). https://doi.org/10.1007/s10877-016-9957-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-016-9957-y