Abstract
Patients undergoing cardiological procedures generally have significant cardiovascular morbidity, and therefore these patients might be at risk for major periprocedural complications. The ability to closely monitor the hemodynamic status would present a major advantage to optimize patient care in this setting. The aim of this review is to assess the available evidence for the use of near-infrared spectroscopy (NIRS) in the care of patients during cardiological procedures. A systematic literature search was conducted using electronic bibliographic databases (MEDLINE, PubMed, EMBASE) from their first available date using the following search strategy: (spectroscopy, near-infrared OR infrared spectroscopy OR NIRS OR cerebral oxygen*) AND (interventional OR electrophysiological OR catheterization OR ablation OR ICD OR defibrillator). Inclusion criteria were limited to human studies, English language and cardiac patients. All manuscripts concerning the use of NIRS in every area of catheterization and electrophysiology were included. The literature search yielded eleven observational studies and five case reports concerning the research question. No randomized trials could be retrieved. Six studies evaluated NIRS during supraventricular and ventricular arrhythmias, one during transcatheter aortic valve implantations, and four studies assessed the use of NIRS in pediatric catheterization procedures. Overall, the studies demonstrated that NIRS provides a very quick representation of cerebral oxygen saturation and that it might identify changes that could not be predicted from standard hemodynamic monitoring. However, the evidence is currently too low to conclude that NIRS can optimize patient care during cardiological procedures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
In general, patients undergoing cardiological procedures, such as cardiac catheterization or electrophysiological interventions, have significant cardiovascular morbidity, and therefore, these patients are prone to major periprocedural complications. Also patients with only minor cardiac anomalies, such as atrial septal defects, might develop adverse clinical outcomes following atrial septal device occlusion [1]. Furthermore, in some interventional procedures, ventricular arrhythmias with resultant circulatory arrest are induced intentionally. Obviously, the ability to closely monitor the hemodynamic status of these patients would present a major advantage to optimize patient care in this setting.
Near-infrared spectroscopy (NIRS) was introduced in 1977 as a technology that is capable of noninvasive monitoring of cerebral oxygenation [2]. In recent years, a growing understanding of the physiological principles of NIRS has led to the larger applicability of NIRS as an estimate of systemic venous saturation in correspondence with the adequacy of the circulatory status [3]. In many cardiac surgery centers, its use has been adopted as standard of care, and there is evidence that NIRS-guided management might lead to better perioperative outcomes [4–6].
Since patients undergoing cardiological procedures present with comparable cardiovascular morbidity as cardiac surgery patients, we hypothesize that NIRS might also prove to be a valuable tool to optimize patient care in this high-risk patient group. The present review was conducted to evaluate the available evidence for the use of NIRS in the care of patients during cardiological procedures.
This systematic review is intended to answer the following questions:
-
1.
Does NIRS allow appropriate monitoring of the hemodynamic status of the patient and does it provide additional value over standard monitoring?
-
2.
Are these results based on studies with solid methodology?
2 Methods
2.1 Search strategy
A systematic literature search was conducted using electronic bibliographic databases (MEDLINE, PubMed, EMBASE) from their first available date using the following search strategy: (spectroscopy, near-infrared OR infrared spectroscopy OR NIRS OR cerebral oxygen*) AND (interventional OR electrophysiological OR catheterization OR ablation OR ICD OR defibrillator).
Inclusion criteria were limited to human studies, English language and cardiac patients. All such manuscripts concerning the use of NIRS in every area of catheterization and electrophysiology were included. Validation studies were excluded.
The titles and abstracts of all manuscripts included were screened and irrelevant articles were excluded. Editorials and narrative reviews were also excluded. Additionally, the references of excluded articles were screened.
We performed a related articles—search from PubMed for all the articles we included.
Relevant studies were then analyzed. The assessment of the risk of bias and the classification of the level of evidence were scored by 2 investigators (FM, AM), independently of each other. On 1 May 2015, the electronic literature search strategy was last updated.
2.2 Risk of bias assessment
The risk of bias of the included studies was assessed based on the GRACE checklist (good research for comparative effectiveness) [7]. The adapted checklist focused on 10 components, 6 relating to data (D questions) and 4 relating to methods (M questions) and as such it provides guidance as a screening tool to eliminate these studies that do not meet the baseline qualifications of comparative effectiveness.
The following domains were assessed:
-
D1. Adequate treatment: Were the main purpose of the study, key research questions and target study population adequately described?
-
D2. Adequate outcomes: Were the primary outcomes adequately recorded?
-
D3. Objective outcomes: Were the primary clinical outcomes measured objectively?
-
D4. Valid outcomes: Were primary outcomes validated, adjudicated, or otherwise known to be valid?
-
D5. Similar outcomes: Was the primary outcome measured or identified in an equivalent manner between the treatment/intervention group and the comparison group?
-
D6. Covariates recorded: Were important covariates that may be known confounders available and recorded?
-
M1. New initiators: Were only new initiators of the treatment of interest included?
-
M2. Concurrent comparators: Were the comparison groups concurrent, or was the use of historical groups justified?
-
M3. Covariates accounted for: Were all important covariates taken into account in the design and/or analysis?
-
M4. Sensitivity analysis: Were any meaningful analyses conducted to test key assumptions on which primary results are based?
The risk of bias was scored as ‘high risk’ or ‘low risk’.
2.3 Level of evidence categorization
To assess the level of evidence, the SIGN (Scottish Intercollegiate Guidelines Network) grading system was used [8].
3 Results
3.1 Results of the search
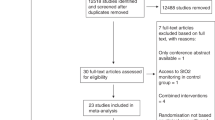
The search result of the literature survey is presented in Fig. 1.
The search yielded 255 citations. Editorials, narrative reviews, and irrelevant articles were excluded. We obtained 11 studies and 5 case reports, with a total of 299 participants, that were eligible for inclusion in our review.
3.1.1 Design of the studies
All included studies were observational studies. No randomized trials could be retrieved.
3.1.2 Settings
Six studies were performed in the setting of arrhythmia (four ventricular fibrillation [9–12], one supraventricular and ventricular arrhythmias [13], and one atrial fibrillation [14]). One study evaluated NIRS during transcatheter aortic valve implantation (TAVI) [15]. Four studies were conducted in pediatric settings (cardiac catheterization [16], valve balloon dilatation [17], balloon atrial septostomy [18], and electrophysiological study [19]).
3.1.3 Study participants
Sample size in the included studies ranged from 6 [12] to 123 [16]. The mean age of participants ranged from 1 day [18] to 82 years [15]. In all the studies the participants age was reported.
3.1.4 Type of NIRS device
In six studies [9, 11, 15–18] and four case reports [20–23], an INVOS (Covidien, Mansfield, MA, USA) device was used. In one study [10] and one case report [24], the NIRO (Hamamatsu Phototonics Corp, Tokyo, Japan) was used. Foresight (CAS Medical Systems, Branford, CT, USA) was used in one study [19], and in two studies the Equanox (Nonin Medical Inc., Minneapolis, MN, USA) device was handled [13, 14]. In one study, the measurements were made with reflectance spectroscopy based on designs of Chance and colleague [12]. None of the studies included comparison of devices.
3.1.5 Funding sources
Only five studies reported information about the funding resources [9, 10, 12, 15, 18].
3.2 Description of the studies
The articles were classified as follows:
-
(a)
Evaluation of NIRS during supraventricular and ventricular arrhythmias
-
(b)
Evaluation of NIRS during TAVI procedures
-
(c)
Evaluation of NIRS during pediatric catheterization procedures
3.2.1 Evaluation of NIRS during supraventricular and ventricular arrhythmias
Four studies [9–12] and two case reports [21, 22] were performed during implantation of an implantable cardioverter-defibrillator (ICD). During this procedure, proper functioning of the ICD is verified by induction of ventricular fibrillation (VF) and defibrillation threshold (DFT) testing. The VF induces a short-lasting normothermic circulatory arrest, providing an optimal experimental model of acute global ischemia. All studies demonstrated a significant and immediate drop in cerebral oxygen saturation (ScO2) when VF was induced [9–12, 21, 22].
Electro-encephalography (EEG) has long been the most frequently used technique for the evaluation of cerebral ischemia and is often considered the gold standard. However, after induction of VF, NIRS-measured ScO2 dropped immediately, whereas EEG changes occurred after 11–12 s [9, 22]. Compared with EEG, the sensitivity and specificity of NIRS were acceptable (60 and 84 %, respectively) [25]. However, it has to be considered that EEG might be an imperfect standard, rendering erroneous values [25]. Jugular bulb oximetry appeared to be of minor value during DFT testing, since no values were obtainable in the absence of flow [9].
In two papers, cytochrome oxidase (CytOx) was also determined [10, 24]. CytOx is the terminal enzyme in the intramitochondrial electron transfer, and therefore provides an indication of the intracellular oxygenation state. In 11 patients in which 26 episodes of VF were induced, the duration of circulatory arrest averaged 13 ± 10 s and no changes in CytOx were observed, although a minor decrease occurred in three subjects [10]. In a case report of arrhythmia during cardiac catheterization, complicated by a cardiac arrest, CytOx was shown to decrease after 1 min of arrest [24]. The CytOx values increased with the start of cardiopulmonary resuscitation and fully recovered when sinus rhythm was restored [24]. These results suggest that short episodes of circulatory arrest do not affect the intramitochondrial oxygenation status, but that the duration of the circulatory arrest is pivotal.
NIRS has also been evaluated during supraventricular arrhythmias [13], which usually have less effect on the systemic circulation compared to ventricular arrhythmias. Although some systemic perfusion might be preserved during supraventricular arrhythmias, it cannot be estimated from routine clinical monitoring parameters (such as blood pressure or pulse oximetry) if the reduced oxygen delivery meets the demand. ScO2 changes were evaluated during both rapid atrial and ventricular pacing (200/min) and were demonstrated to be primarily influenced by age and left ventricular ejection fraction [13].
In another prospective study from the same study group, cerebral oxygenation was studied during the electrical cardioversion of atrial fibrillation (AF) [14]. Previously, it has been suggested that cerebral hypoperfusion is a major contributing factor to the cognitive decline which is often observed in patients with AF [26]. The study demonstrated a significant increase of ScO2 (3 ± 2 and 4 ± 4 % from baseline for right- and left-sided ScO2, respectively) in patients after successful restoration of sinus rhythm (n = 20) compared with patients who remained in AF (n = 10), without significant differences in mean arterial pressure (MAP) or arterial oxygen saturation (SaO2). This result is in accordance with previous observations, demonstrating improved microvascular perfusion after electrical cardioversion for AF, with no clear relation to global hemodynamic parameters [27].
Overall, the studies in the setting of supraventricular and ventricular arrhythmias indicate that NIRS is an effective non-invasive tool for monitoring cerebral oxygenation, and provides a more responsive cerebral monitor to circulatory arrest than EEG and jugular bulb oximetry. Moreover, NIRS proved to identify changes in ScO2 during arrhythmias that could not be predicted from standard monitoring.
3.2.2 Evaluation of NIRS during TAVI procedures
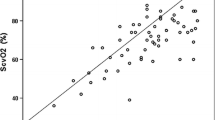
From a technical point of view, TAVI is minimally invasive, nevertheless, patients still have a significant risk for periprocedural morbidity and mortality. Mixed venous oxygen saturation (SmvO2) reflects the adequacy of systemic oxygen balance, and could benefit these high risk patients [28]. However, its obligatory need for more invasive instrumentation is a major drawback for its routine application. A case report of prolonged cardiopulmonary resuscitation during TAVI demonstrated a close relationship between ScO2 and SmvO2 [23]. The authors hypothesized that ScO2 not only reflects the cerebral, but also the systemic oxygen balance. Therefore, in a subsequent study, the equivalence and interchangeability of ScO2 and SmvO2 were investigated during the rapidly changing hemodynamic states inherent to TAVI procedures [15]. A moderate-to-close correlation between ScO2 and SmvO2 was demonstrated. However, since at all measured time points ScO2 was lower than SmvO2, the authors warn that the global oxygen balance might be underestimated, with the risk of over-treatment and unnecessary therapeutic measures.
3.2.3 Evaluation of NIRS during pediatric catheterization procedures
In recent years, many cardiac surgical procedures in children have been superseded by transcatheter interventions. These are minimally invasive compared to surgery, but nevertheless considerable risks are entailed. In a study of 123 pediatric patients undergoing cardiac transcatheter interventions, a complication rate of 33 % was reported, mainly desaturation events (20 %), arrhythmias (8 %), and cardiopulmonary resuscitation (5 %) [16].
In the above mentioned study the relationship between cerebral and renal NIRS during adverse events was evaluated [16]. It was demonstrated that NIRS values fell simultaneously with the onset of arrhythmia, and that in case of desaturation events, NIRS values dropped 10–15 s before changes in pulse oximetry. The authors concluded that both cerebral and renal NIRS monitoring provide an early warning of adverse events, however with a higher sensitivity for cerebral NIRS compared to renal NIRS.
The effect of valve balloon dilatation on cerebral perfusion and oxygenation was examined in a prospective, observational study [17]. Eleven pediatric patients were divided into two groups, based on the site of the valve stenosis and the presence or absence of intracardiac shunts. Eventually 57 balloon inflations were included. In both groups, balloon inflation led to an immediate drop in the ScO2 due to a critical reduction in cardiac output. In the group with intracardiac shunting, massive right-to-left shunting led to a much more pronounced drop in ScO2 caused by the additional decrease in arterial oxygen content. After deflation, the ScO2 restored over a period which lasted approximately two times the duration of the inflation in both groups.
One publication reported on 2 cases in which balloon dilatation of a congenital aortic valve stenosis was complicated by circulatory arrest [20]. In both cases, NIRS yielded valuable information on the efficacy of the external heart massage and the resuscitative measures.
In neonates with transposition of the great arteries (TGA), the effect of balloon atrial septostomy (BAS) (creation of an atrial septal defect) on cerebral oxygenation was assessed, and compared with the ScO2 values of neonates with TGA who did not need a BAS [18]. Twenty-one neonates with TGA were included. BAS instantaneously increased the ScO2, and the values slowly continued to increase, without a concomitant increase in SaO2. Twenty-four hours after the procedure, ScO2 was significantly higher in neonates who underwent a BAS, despite the fact that preprocedural ScO2 values had been lower in this group. The authors suggested that the clinical implication of this finding is that earlier application of BAS might reduce the duration of impaired ScO2 and therefore could contribute to a better cerebral outcome. On the other hand, BAS has been demonstrated to be a major risk factor for preoperative focal brain injury, consistent with embolism [29, 30]. Therefore, the net effect of BAS on cerebral outcome remains to be determined.
In 22 patients, 5–20 years of age, undergoing an electrophysiology study, the correlation between ScO2 and blood pressure was evaluated during induced SVT [19]. An average decrease in blood pressure of 13 mmHg was noted at the beginning of SVT, whereas ScO2 showed only a slight drop, on average 0.7 %. The authors assumed that the minimal drop might be reflective of a functional cerebral autoregulation mechanism. Despite the small cohort of patients and the minor changes in ScO2, this study showed a statistically significant positive correlation between hemodynamic changes and NIRS values, suggesting that NIRS monitoring might be used instead of more invasive hemodynamic monitoring such as invasive arterial cannulation [19].
3.2.4 Overshoot phenomenon
Of particular interest is the observation of overshoot in ScO2 when hemodynamics are restored after the circulatory arrest [9, 11, 12, 17, 20, 22, 24]. This compensatory hyperemia is presumed to be caused by endothelial release of endogeneous vasodilators in response to the sudden drop in cerebral perfusion pressure [11]. The absence of this overshoot phenomenon might identify patients who are unable to produce or release endogeneous vasodilators, and these patients are suggested to be prone to an increased risk for developing adverse cerebral events [11].
3.3 Risk of bias of included studies
The risk of bias is summarized in Table 1. In all but one study [11], the risk of bias for data collecting and reporting could be considered as low. However, none of the studies adequately accounted for important covariates or confounding variables in the design nor in the analysis.
3.4 Level of evidence of included studies
The level of evidence is presented in Table 2. Ten studies were categorized as a level of evidence 2+, while five studies had a level of evidence 3. For one study no level of evidence could be determined. No reported study had a higher level of evidence than 2+.
4 Discussion
The primary goal in the hemodynamic management of patients undergoing interventional procedures is to preserve oxygen delivery at a level sufficient to cover all metabolic needs. Nowadays, anesthesiologists can rely on a variety of monitoring tools to quantify cardiovascular performance and global oxygen delivery. Nonetheless, current standard anesthesia monitoring still has two major drawbacks.
Firstly, it provides a global assessment of the patient’s status, and as such vital organ ischemia may go unnoticed until functional organ damage becomes evident. Especially, given its vital importance, the human brain is an alarming poorly monitored organ. Yet several clinical conditions routinely encountered in the cardiac catheterization laboratory have the potential to disrupt the balance between cerebral oxygen supply and demand. In all studies of the present review, NIRS proved to respond immediately to arrhythmias and circulatory arrest, and to identify incomplete cerebral recovery, despite seemingly restored hemodynamics [14, 19, 22]. A clear relationship between the duration of reperfusion interval during DFT testing and postprocedural cognitive dysfunction has been demonstrated [31]. Intervals between induced arrhythmias should therefore be guided by ScO2 instead of relying on hemodynamic variables alone [22, 31].
The second drawback of standard anesthesia monitoring is that the majority of variables focus on oxygen supply (cardiovascular performance, hemoglobin and arterial oxygen content) but do not assess imbalances between oxygen supply and demand. Mixed venous oxygen saturation is generally accepted as an indicator of adequacy of systemic oxygen balance, but its obligatory need for more invasive instrumentation precludes its use as a standard routine monitor. NIRS assesses the venous side of the circulation, providing postextraction monitoring of how the circulatory system is functioning [32], and therefore might be a reliable surrogate of SmvO2. This has clearly been demonstrated in the study of Paarmann et al. [15]. It has been postulated in the present review and in previous papers [33] that NIRS can detect hypoperfusion despite seemingly preserved values of blood pressure and pulse oximetry. Although it is tempting to believe that implementing non-invasive cerebral monitoring might replace invasive arterial monitoring in the care of patients during cardiological procedures, the evidence is yet undefined and further study is warranted.
In evidence-based medicine, observational research is often viewed with skepticism. However, non-interventional studies may provide information that is impossible to obtain from a randomized trial or some other type of intervention study, for practical or ethically unacceptable reasons. In these situations, observational studies may be the preferred approach. Obviously, large benefits are easy to give credence to, however evidencing improved outcome with the use of some type of monitor is extremely difficult. The difficulty for obtaining evidence for improved outcome reminds one of the history of pulse oximetry. Despite its universal application and its implementation in the safety guidelines, improved clinical outcome was never evidenced for pulse oximetry [34].
In recent years, several guidelines were published as a solution for the widespread lack in familiarity in observational studies, such as the GRACE checklist which has been used in this review [7]. These principles describe key elements of good practice including defining research questions and methods a priori, reporting with sufficient detail for evaluation and replication, and evaluating the validity of the data interpretation, including sensitivity analyses and alternative explanations for findings. These guidelines promote the appreciation and quality of observational research and therefore observational and non-intervention studies might substantially contribute to evidence-based medicine and prove their value in improving decisions affecting diagnosis, treatment and delivery of medical care [35].
With regard to the current literature, it can be stated that the use of NIRS enables to measure cerebral oxygen saturation during cardiological procedures, and that NIRS might identify impaired systemic perfusion despite apparently normal hemodynamic parameters. The clear advantage of NIRS is that it is non-invasive, bedside, user-friendly, and operator-independent.
However, concerning the available literature a number of limitations must be pointed out. Firstly, a very limited number of studies on the use of NIRS during cardiological procedures have been published and virtually all publications have a low power. Secondly, there is a rather broad patient distribution and variation in the procedures. Therefore, at the moment it is impossible to perform a meta-analysis. Thirdly, children with congenital heart disease represent a very heterogeneous population with extremely complex physiology. Therefore, evidence in adults cannot be simply transposed to these pathologies. Finally, only observational studies were published so far, and not a single study has a level of evidence higher than 2+.
5 Conclusion
Thus far, both in the adult and pediatric patient population, a very limited number of studies on the use of NIRS during cardiological procedures has been published.
The current preliminary evidence, based on small studies and case reports, shows that NIRS provides a very quick representation of cerebral oxygen saturation and that it might identify changes that could not be predicted from standard hemodynamic monitoring. However, the evidence is currently too low to conclude that NIRS can optimize patient care during cardiological procedures.
References
Ermis P, Franklin W, Mulukutla V, Parekh D, Ing F. Left ventricular hemodynamic changes and clinical outcomes after transcatheter atrial septal defect closure in adults. Congenit Heart Dis. 2015;10:E48–53.
Jobsis FF. Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science. 1977;198:1264–7.
Moerman A, Vandenplas G, Bové T, Wouters P, De Hert S. Relation between mixed venous oxygen saturation and cerebral oxygen saturation measured by absolute and relative near-infrared spectroscopy during off-pump coronary artery bypass grafting. Br J Anaesth. 2013;110:258–65.
Murkin JM, Adams SJ, Novick RJ, Quantz M, Bainbridge D, Iglesias I, Cleland A, Schaefer B, Irwin B, Fox S. Monitoring brain oxygen saturation during coronary bypass surgery: a randomized, prospective study. Anesth Analg. 2007;104:51–8.
Slater JP, Guarino T, Stack J, Vinod K, Bustami RT, Brown JM 3rd, Rodriguez AL, Magovern CJ, Zaubler T, Freundlich K, Parr GV. Cerebral oxygen desaturation predicts cognitive decline and longer hospital stay after cardiac surgery. Ann Thorac Surg. 2009;87:36–44.
Goldman S, Sutter F, Ferdinand F, Trace C. Optimizing intraoperative cerebral oxygen delivery using noninvasive cerebral oximetry decreases the incidence of stroke for cardiac surgical patients. Heart Surg Forum. 2004;7:E376–81.
Dreyer N, Velentgas P, Westrich K, Dubois R. The GRACE checklist for rating the quality of observational studies of comparative effectiveness: a tale of hope and caution. J Manag Care Pharm. 2014;20:301–8.
Harbour R, Miller J, Scottish Intercollegiate Guidelines Network Grading Review Group. A new system for grading recommendations in evidence based guidelines. BMJ. 2001;323:334–6.
de Vries JW, Visser GH, Bakker PFA. Neuromonitoring in defibrillation threshold testing. A comparison between EEG, near-infrared spectroscopy and jugular bulb oximetry. J Clin Monit. 1997;13:303–7.
McNeill E, Gagnon RE, Potts JE, Yeung-Lai-Wah JA, Kerr CR, Sanatani S. Cerebral oxygenation during defibrillator threshold testing of implantable cardioverter defibrillators. Pacing Clin Electrophysiol. 2005;28:528–33.
Singer I, Edmonds H. Changes in cerebral perfusion during third-generation implantable cardioverter defibrillator testing. Am Heart J. 1994;127:1052–7.
Smith DS, Levy W, Maris M, Chance B. Reperfusion hyperoxia in brain after circulatory arrest in humans. Anesthesiology. 1990;73:12–9.
Wutzler A, Otto N, Gräser S, Boldt LH, Huemer M, Parwani A, Haverkamp W, Storm C. Acute decrease of cerebral oxygen saturation during rapid ventricular and supraventricular rhytm: a pilot study. Pacing Clin Electrophysiol. 2014;37:1159–65.
Wutzler A, Nee J, Boldt L-H, Kühnle Y, Gräser S, Schröder T, Haverkamp W, Storm C. Improvement of cerebral oxygen saturation after successful electrical cardioversion of atrial fibrillation. Europace. 2014;16:189–94.
Paarmann H, Heringlake M, Heinze H, Hanke T, Sier H, Karsten J, Schön J. Non-invasive cerebral oxygenation reflects mixed venous oxygen saturation during the varying haemodynamic conditions in patients undergoing transapical transcatheter aortic valve implantation. Interact CardioVasc Thorac Surg. 2012;14:268–72.
Tanidir IC, Ozturk E, Ozyilmaz I, Saygi M, Kiplapinar N, Haydin S, Guzeltas A, Odemis E. Near infrared spectroscopy monitoring in the pediatric cardiac catheterization laboratory. Artif Organs. 2014;38:838–44.
de Vries JW, Hoorntje TM, Sreeram N. Neurophysiological effects of pediatric balloon dilatation procedures. Pediatr Cardiol. 2000;21:461–4.
Van der Laan ME, Verhagen EA, Bos AF, Berger RMF, Kooi EMW. Effect of balloon atrial septostomy on cerebral oxygenation in neonates with transposition of the great arteries. Pediatr Res. 2011;73:62–7.
Hershenson JA, Ro PS, Miao Y, Tobias JD, Olshove V, Naguib AN. Changes in hemodynamic parameters and cerebral saturation during supraventricular tachycardia. Pediatr Cardiol. 2012;33:286–9.
de Vries JW, Haanschoten M. Resuscitation in pediatric balloon valvuloplasty: effects on cerebral perfusion and oxygenation. J Cardiothorac Vasc Anesth. 2000;14:581–3.
Jinnouchi Y, Kawahito S, Kitahata H, Tanaka K, Nozaki J, Oshita S. Anesthetic management of a patient undergoing cardioverter defibrillator implantation: usefulness of transesophageal echocardiography and near infrared spectroscopy. J Anesth. 2004;18:220–3.
de Vries JW, Hoorntje T, Bakker PFA. Cerebral oxygen saturation monitoring in an infant undergoing ICD implantation. J Cardiothorac Vasc Anesth. 1998;12:442–4.
Paarmann H, Heringlake M, Sier H, Schön J. The association of non-invasive cerebral and mixed venous oxygen saturation during cardiopulmonary resuscitation. Interact CardioVasc Thorac Surg. 2010;11:371–3.
Nagdyman N, Fleck T, Ewert P, Abdul-Khaliq H, Redlin M, Lange P. Cerebral oxygenation measured by near-infrared spectroscopy during circulatory arrest and cardiopulmonary resuscitation. Br J Anaesth. 2003;91:438–42.
Levy W, Levin S, Chance B. Near-infrared measurement of cerebral oxygenation. Anesthesiology. 1995;83:738–46.
Ettorre E, Cicerchia M, De Benedetto G, Fossati C, Guglielmi S, Manzon L, Servello A, Petrillo A, Marigliano V. A possible role of atrial fibrillation as a risk factor for dementia. Arch Gerontol Geriatr. 2009;49(Suppl 1):71–6.
Elbers P, Prins W, Plokker H, van Dongen E, van Iterson M, Ince C. Electrical cardioversion for atrial fibrillation improves microvascular flow independent of blood pressure changes. J Cardiothorac Vasc Anesth. 2012;26:799–803.
Pölönen P, Ruokonen E, Hippeläinen M, Pöyhönen M, Takala J. A prospective, randomized study of goal-oriented hemodynamic therapy in cardiac surgical patients. Anesth Analg. 2000;90:1052–9.
McQuillen PS, Hamrick SE, Perez MJ, Barkovich AJ, Glidden DV, Karl TR, Teitel D, Miller SP. Balloon atrial septostomy is associated with preoperative stroke in neonates with transposition of the great arteries. Circulation. 2006;113:280–5.
Block AJ, McQuillen PS, Chau V, Glass H, Poskitt KJ, Barkovich AJ, Esch M, Soulikias W, Azakie A, Campbell A, Miller SP. Clinically silent preoperative brain injuries do not worsen with surgery in neonates with congenital heart disease. J Thorac Cardiovasc Surg. 2010;140:550–7.
Murkin JM, Baird DL, Martzke JS, Yee R. Cognitive dysfunction after ventricular fibrillation during implantable cardiovertor/defibrillator procedures is related to duration of the reperfusion interval. Anesth Analg. 1997;84:1186–92.
Scott JP, Hoffman GM. Near-infrared spectroscopy: exposing the dark (venous) side of the circulation. Paediatr Anaesth. 2014;24:74–88.
Scheeren TWL, Schober P, Schwarte LA. Monitoring tissue oxygenation by near infrared spectroscopy (NIRS): background and current applications. J Clin Monit Comput. 2012;26:279–87.
Pedersen T, Nicholson A, Hovhannisyan K, Moller AM, Smith AF, Lewis SR. Pulse oximetry for perioperative monitoring. Cochrane Database Syst Rev. 2014;3:CD002013. doi:10.1002/14651858.CD002013.pub3.
Dreyer N. Making observational studies count. Shaping the future of comparative effectiveness research. Epidemiology. 2011;22:295–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Moerman, A., Meert, F. & De Hert, S. Cerebral near-infrared spectroscopy in the care of patients during cardiological procedures: a summary of the clinical evidence. J Clin Monit Comput 30, 901–909 (2016). https://doi.org/10.1007/s10877-015-9791-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-015-9791-7