Abstract
Real-time measurement of propofol in the breath may be used for routine clinical monitoring. However, this requires unequivocal identification of the expiratory phase of the respiratory propofol signal as only expiratory propofol reflects propofol blood concentrations. Determination of CO2 breath concentrations is the current gold standard for the identification of expiratory gas but usually requires additional equipment. Human breath also contains isoprene, a volatile organic compound with low inspiratory breath concentration and an expiratory concentration plateau. We investigated whether breath isoprene could be used similarly to CO2 to identify the expiratory fraction of the propofol breath signal. We investigated real-time breath data obtained from 40 study subjects during routine anesthesia. Propofol, isoprene, and CO2 breath concentrations were determined by a combined ion molecule reaction/electron impact mass spectrometry system. The expiratory propofol signal was identified according to breath CO2 and isoprene concentrations and presented as median of intervals of 30 s duration. Bland–Altman analysis was applied to detect differences (bias) in the expiratory propofol signal extracted by the two identification methods. We investigated propofol signals in a total of 3,590 observation intervals of 30 s duration in the 40 study subjects. In 51.4 % of the intervals (1,844/3,590) both methods extracted the same results for expiratory propofol signal. Overall bias between the two data extraction methods was −0.12 ppb. The lower and the upper limits of the 95 % CI were −0.69 and 0.45 ppb. Determination of isoprene breath concentrations allows the identification of the expiratory propofol signal during real-time breath monitoring.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Propofol is a hypnotic drug that is administered intravenously. It is widely used for induction and maintenance of general anesthesia. Previous studies showed that propofol is exhaled during anesthesia in very low concentrations and that propofol breath concentrations reflect propofol blood concentrations when propofol blood concentrations are in steady-state [1–5]. Furthermore, we recently demonstrated that propofol breath concentrations change quickly after application of a propofol bolus [6]. This suggests that measurement of exhaled propofol may be used as routine monitoring and feedback to control propofol infusion in the future.
During anesthesia, propofol infusion has to be frequently modified and adjusted to different stages of the surgical procedure. Such modifications in propofol infusion lead to rapid changes in propofol blood and breath concentrations. Therefore, any measurement technique used during such non-steady-state conditions is required to quickly detect changes in propofol breath concentrations. Real-time measurement techniques with a breath-by-breath resolution fulfill this requirement. Examples of these techniques include ion molecule reaction mass spectrometry (IMR-MS), proton transfer reaction mass spectrometry (PTR-MS), or selected ion flow tube mass spectrometry (SIFT-MS) [1, 3, 7, 8].
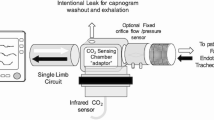
Real-time measurement techniques determine propofol concentrations in breath gas continuously. Usually a small amount of sample gas, e.g. 50 ml/min, is sampled through a T-piece connected to the patient’s endotracheal tube or laryngeal mask and analyzed regardless of the phase of the respiratory cycle. This will result in propofol measurement data from both inspiratory and expiratory gas. Yet, only propofol concentrations in expiratory gas are of interest as only these ultimately reflect blood concentrations. Therefore, the propofol measurements obtained from expiratory gas have to be clearly identified from the pool of propofol breath data obtained during continuous sampling of breathing gas. Our group used IMR-MS for propofol breath monitoring which allows determination of propofol gas concentrations within 500 ms. Hence, IMR-MS could provide around 120 propofol measurements per minute. Additionally, the propofol signal in breathing gas peaks during expiration but propofol concentrations do not decrease completely during inspiration. Therefore, the expiratory phase of the breathing cycle has to be clearly identified and only propofol measured during this time should be evaluated while propofol measurements during inspiration should be discarded.
Various techniques for the identification of the expiratory phase have been described. In anesthesia, determination of CO2 is frequently used for this purpose. Respiratory CO2 concentrations have a typical profile with very low inspiratory concentrations and an expiratory plateau. However, measurement of CO2 requires additional equipment. Though chemical ionization techniques like IMR-MS allow determination of numerous volatile organic compounds within milliseconds, they cannot determine CO2 concentrations. Thus, we previously measured CO2 with a second mass spectrometry system based on electron impact ionization (EI-MS) that was connected to the reaction chamber of the IMR-MS. Determination of CO2 concentrations in the gas sample allowed unequivocal attribution of the gas sample to the different time phases of the respiratory cycle. Another method for the identification of the expiratory phase is the determination of water vapor, a technique that was used in studies with SIFT-MS [9].
Aside from using CO2 or water vapour as a marker for expiration, the expiratory gas phase may also be identified by measuring volatile organic compounds (VOCs) that are produced systemically, e.g., isoprene or acetone. Similar to CO2, isoprene and acetone are products of body metabolism with very low inspiratory concentrations and an expiratory plateau. In contrast to CO2 they can be determined by IMR-MS thereby allowing identification of expiratory gas by the IMR-MS itself and simplifying the measurement system. Additionally these substances are not produced in the oral cavity like ammonia and ethanol and therefore they are indicative for alveolar gas. For this work we examined breath data that was collected with IMR-MS in study subjects during propofol anesthesia that included propofol and isoprene measurements. We examined whether isoprene can be used equally well for identification of expiratory propofol as CO2. We identified propofol measurements as expiratory according to both isoprene and CO2 sample gas concentrations and compared the two resulting expiratory propofol signals.
2 Materials and methods
2.1 Study design
The Institutional Review Board of the University of Munich approved this observational study. All study persons gave written informed consent prior to inclusion into the study. We present an analysis of propofol breath data from 40 study subjects undergoing general anesthesia for routine surgery. We investigated breath data during the non-steady-state conditions immediately after induction as well as during steady-state conditions intra-operatively. This work aimed to compare the marker substances CO2 and isoprene for the identification of the propofol signals during expiration.
The study subjects received total intravenous anesthesia with propofol. The observation period included the start of the anesthetic procedure when study persons were still awake and breathed spontaneously through a facial mask. After loss of consciousness, either a laryngeal mask or an endotracheal tube was inserted to secure the study person’s airway. Propofol dosage was left to the discretion of the treating anesthesiologist. Ventilation parameters were set to target an end-tidal CO2 concentration of 35–40 mmHg with a tidal volume from 6 to 10 ml/kg.
2.2 Mass spectrometry system
We used an IMR-MS system to measure propofol in breath during anesthesia (Airsense, V&F medical development, Absam, Austria). IMR-MS is a highly sensitive technology that allows detection of volatile organic compounds in gases in the parts-per-billion range (ppb) and within milliseconds. In brief, sample gas is conveyed into the reaction chamber of the IMR-MS where it interacts with positively charged mercury ions. Neutral propofol molecules in the sample gas react with the positively charged mercury ions and form product ions that can be separated by a quadrupole mass separator and quantified by a secondary electron multiplier. For propofol, this ionization process results in two different product ions, one with a mass-to-charge ratio (m/z) of 163 (propofol 163) and the other one with m/z 178 (propofol 178). Both propofol product ions were registered during our analysis. The same principle was applied to isoprene that reacts with the mercury ions to a product ion with m/z 68. However, the energy of the mercury ions used for propofol and isoprene is too low to ionize CO2, meaning CO2 cannot be quantified by IMR-MS. Therefore, the Airsense instrument contains a second mass spectrometry system based on a conventional electron impact mass spectrometer (EI-MS) that is connected to reaction chamber of the IMR-MS. This allows determination of CO2 concentration in the gas sample and identification of the different time phases of the respiratory cycle. A more detailed description of the technology was published previously [1, 10].
2.3 Breathing gas sampling and measurement setup
The IMR-MS Airsense system was connected either to the study person’s breathing mask, laryngeal mask, or endotracheal tube. We continuously sampled 50 ml/min of breathing gas. The IMR-MS of the Airsense system was set up to measure propofol 163, propofol 178, and isoprene. As the Airsense system used in our study can only measure one m/z at a time, these three compounds had to be measured consecutively in a repetitive measurement cycle. Integration time was 500 ms for propofol 163 and propofol 178, and 200 ms for isoprene. Additionally, cycle time for switching quadrupole field after each compound is 2 ms. This means that it takes 1.2 s for one cycle to be completed and that each of these three compounds was determined about every 1.2 s resulting in about 50 measurements per minute for propofol 163, propofol 178, and isoprene. In addition, the EI-MS had a measurement cycle that determined CO2 and O2 alternatingly every 200 ms. Hence, CO2 measurements were available every 400 ms or 150/min. The measurement setup is summarized in Table 1. Breath data were recorded by V&F Viewer (V&F, Absam, Austria), the proprietary data recording software of the IMR-MS.
2.4 Statistical analysis
Because residues of volatile anesthetics in the anesthesia circuit may interact with the m/z 178 signal, but not with m/z 163, we included only the propofol product ion with m/z 163 into our analyses [1].
Before extracting propofol values, the expiratory phases of the respiratory cycle were identified automatically using CO2 and isoprene measurements. For this purpose, we developed an algorithm using a flexible threshold value approach described for CO2:
First, breath data was decomposed into 30 s intervals. For each interval we then computed a threshold that served to separate inspiratory and expiratory phases. The threshold was defined as the mean value of the minimal and maximal CO2 concentration measured during the respective 30 s interval. An expiration interval was defined as the time from the last CO2 measurement before the increase of the CO2 signal above the threshold until the first CO2 measurement after the decrease of the CO2 signal below the threshold. We identified all propofol data recorded during expiration intervals of 2–7 s duration into our analysis. This was done similarly for isoprene.
From this pool of expiratory propofol data we further extracted one single propofol measurement for each expiration interval (the peak signal during that period). We then calculated the median of these peak signals obtained from all expiration intervals in a particular 30 s interval. Additionally, we applied the following two restrictions in order to extract the propofol signal more reliably: First, we excluded 30 s intervals without respiration, i.e., intervals with thresholds below 1 % (gas concentration) for CO2 or below 40 ppb for isoprene. Second, the median propofol value for a 30 s interval was only extracted if at least two expirations had been identified in the respective 30 s interval.
After extracting propofol values by CO2 and isoprene, we compared the 30 s medians of the expiratory propofol signals identified by the two methods.
In our observations, the propofol signal showed a lag time. Propofol concentrations in breath do not increase and decrease as quickly as CO2 and isoprene concentrations during ventilation. Propofol breath concentrations only decline about 50 % during inspiration instead of going back to almost zero as CO2 concentrations do. Furthermore, due to this slower reaction of the propofol measurements, high propofol concentrations can still be observed shortly after the decline of the CO2 signal. We conducted an extended CO2 analysis to assess whether this lag time influences the extracted propofol data. For this extended CO2 analysis, we additionally included the propofol data recorded up to 1 s after the end of the expiration intervals as defined by CO2 measurements in our analysis.
The Bland and Altman method was used to compare the two methods for extracting propofol values [11–14]. We obtained the differences between measurements by the two methods for each subject and calculated the mean difference (bias) and the standard deviation for constructing 95 % limits of agreement. Repeated measures for each subject were taken into account in the calculation of the standard deviation according to the approach described by Bland and Altman: the standard deviation (representing the variation for single differences on different subjects) consists of two variance components [14]. The first component corresponds to the variation within each subject while the second component corresponds to the variation among subjects representing heterogeneity. The two variance components can be obtained using the results from one-way analysis of variance. For the exact calculation we refer to Bland and Altman [14].
Statistical analysis was performed using the statistical software R 2.14 (www.r-project.org).
3 Results
We investigated breath data from 40 study persons. In these study persons we compared a total of 3,590 observation intervals of 30 s duration.
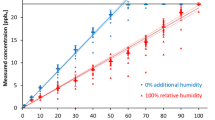
Figure 1 shows the expiratory propofol data extracted by CO2 signal versus the expiratory propofol signal extracted by the isoprene signal.
Expiratory propofol signal extracted from data recorded during continuous real-time breath monitoring using ion molecule reaction mass spectrometry. Each point shows the extracted median expiratory propofol value of a 30 s interval identified by the CO2 signal versus the propofol signal extracted by the isoprene signal (shown are 3,590 extracted propofol values from 40 study subjects). Darker areas indicate a higher amount of overlying data points
In 51.4 % of the observation intervals (1,844/3,590) both methods extracted the same results for expiratory propofol signal.
Differences between the methods for extracting expiratory propofol concentration over a 30 s interval were graphically assessed by the Bland and Altman method for repeated measurements per study subject (Figs. 2, 3). Figure 2 shows the differences in extracted propofol signal between the CO2 and isoprene extraction methods for all 40 patients (measurements from different patients are labeled with a different color). Propofol values extracted by isoprene measurements are slightly higher than propofol values extracted by CO2 measurements (bias CO2−isoprene = −0.12 ppb). There is no tendency for the difference between the two methods to increase with increasing propofol breath concentrations.
Bland-Altman plot of the expiratory propofol signal extracted from data recorded during continuous real-time breath monitoring using ion molecule reaction mass spectrometry in 40 study persons. The expiratory propofol signal was identified and extracted from the complete (inspiratory and expiratory) data using the respiratory CO2 and isoprene signal. Shown are the differences between the propofol values extracted by CO2 and isoprene versus the averaged propofol value extracted by the two methods. Each point (n = 3,590) corresponds to one propofol value extracted for a 30 s interval. Measurements from different study persons are labeled with a different color. The solid red line represents the average difference (bias) between the two data extraction methods for expiratory propofol. The dashed red lines represent the limits of the 95 % CI for the difference, i.e. the bias ± 2 SD of the difference in propofol values
Bland-Altman plot of the expiratory propofol signal extracted from data recorded during continuous real-time breath monitoring using ion molecule reaction mass spectrometry in 40 study subjects. The expiratory propofol signal was identified and extracted from the complete (inspiratory and expiratory) data using the respiratory CO2 and isoprene signal. Shown are the differences between propofol values extracted by the CO2 and isoprene signal versus the averaged propofol value extracted by the two methods. Each point (n = 40) corresponds to the averaged extracted propofol value over all 30 s intervals for one particular study person. The solid red line represents the average difference (bias) between the two extraction methods for expiratory propofol. The dashed red lines represent the limits of the 95 % CI, i.e. the bias ± 2 SD of the difference in propofol values. The CI was constructed for the difference in extracted propofol values for a 30 s interval (not for the difference in the averaged propofol values over all 30 s intervals)
The variance of the difference in extracted propofol values is 0.08. The lower and the upper limits of the 95 % CI are −0.69 and 0.45 ppb. We expect 95 % of the differences to lie between these limits.
The variance was estimated taking into account the repeated measures per study subject [14]. Looking at the single variance components suggests that there is very little variation between the subjects since the between subject variation representing heterogeneity is rather small with 0.007 compared to the within subject variation of 0.077. Further support is given by Fig. 2. Here, the between-method differences do not seem to vary across individuals more than expected simply by chance. The estimated crude variance that does not take into account the repeated measurements over the subjects is only marginally smaller with 0.0841 compared to the adjusted variance of 0.0846. We conclude from these findings that there is very little heterogeneity between study subjects and consequently, the extraction of propofol concentrations by isoprene measurements will also work on future patients.
When the extended CO2 extraction was compared with the isoprene method, the bias was 0.10 ppb. This means that propofol data extracted with the extended CO2 method were slightly higher than those extracted with the isoprene method. The lower and upper limits of the 95 % CI for the differences in extracted propofol values using the extended CO2 and isoprene extraction methods were −0.38 and 0.57 ppb.
4 Discussion
This study showed that isoprene breath concentrations can be used similarly to CO2 breath concentrations for the identification of the expiratory propofol signal during anesthesia in study subjects undergoing routine anesthesia.
Previous studies have shown the importance of the identification of expiratory gas concentrations of volatile organic compounds. Miekisch and colleagues demonstrated that alveolar concentrations of various VOCs can be up to twofold higher compared to mixed expiratory concentrations [15]. In our study, we extracted the peak expiratory signal from all propofol signals measured during each expiration rather than selecting the last propofol signal measured before the end of expiration. We selected this approach for several reasons. First, selecting the highest signal during a single expiration avoids selecting propofol signals during early-expiration, when the signal still may be low leading to the identification of an incorrectly low propofol signal. Second, until today it hasn’t been determined when the actual peak of the propofol signal is reached during expiration. Generally, it is assumed that gas exchange occurs in the alveoli. This is particularly true for O2 and CO2. However, for substances with a blood:air partition coefficient (λb:a) > 1,000, gas exchange can occur in the airway [16]. VOCs that are exchanged in the airway, e.g. acetone and ethanol, have peak concentrations more mid-expiratory than end-expiratory like CO2. Recent work suggests that propofol has a high blood:air partition coefficient and therefore may reach its expiratory peak pre-end-expiratory [17]. Finally, the extension of the CO2 extraction algorithm by one second after the end of expiration lead to a slightly higher expiratory propofol signal (bias extended CO2 - CO2 = 0.22 ppb) indicating a time lag of the propofol signal behind the CO2 and isoprene signal. It remains unclear how this time lag is caused. A potential explanation may be that propofol adheres to surfaces in the sampling line and therefore is carried more slowly into the reaction chamber of the IMR-MS. It may still be that actual propofol breath concentrations peak mid-expiratory, but this would be masked by the time lag of the propofol signal. Therefore, it seems reasonable to extract one single peak propofol value per expiration or extended expiration interval.
In our study, the bias of −0.12 and 0.10 ppb, between the isoprene method and the two CO2 methods was very small. Since mean expiratory propofol breath concentrations are commonly in the range of 6–10 ppb during the maintenance phase of anesthesia, the bias in our study would be <2 % of the actual propofol signal. We consider such bias as acceptable. The bias between the two CO2 methods was slightly larger and showed 3–4 % higher expiratory propofol values for propofol data extracted by the extended CO2 method compared to the CO2 method. We conclude from this finding that the time lag of the propofol signal actually influences extracted expiratory propofol data. Again, we consider such bias as very small and clinically acceptable. Despite this, future studies on breath propofol concentrations may analyze the data for the existence of any time lag of the propofol signal.
The actual identification of expiratory gas and measurement of expiratory propofol during continuous breath analysis can be accomplished by different methods. One approach is to separate expiratory air by an electronically controlled valve that can be triggered by a gas flow or CO2 sensor [18]. Others have manually drawn air samples with a syringe according to the signal of a CO2 sensor measuring in breath mainstream [15]. Yet, these methods do not allow measurement of the full respiratory cycle, i.e., to investigate inspiration and expiration. Another potential method is the determination of CO2 breath concentration with an additional device sampling breath separately. However, such a method would require complex time synchronization techniques between the CO2 measurements and the actual measurements of propofol. Schwoebel et al. [19] used proton transfer reaction mass spectrometry to determine water vapor concentrations as a marker for the respiratory cycle. Similar to our approach using isoprene, their approach analyzes the breath marker directly within the gas sample therefore making complex time synchronization techniques unnecessary.
Other endogenous VOCs, e.g. acetone, that have a similar inspiration-expiration concentration profile as isoprene may be used similarly for the detection of the respiratory cycle [10]. However, we did not investigate any VOCs other than propofol and isoprene in this study. The use of water vapour for the identification of respiratory cycle has been successfully used with SIFT-MS in human breath studies [9]. Water vapour could be also quantified with IMR-MS but this would need the use of Kr+ ions as primary ion source as the Hg+ ions used for determination of propofol cannot ionize water. Such a measurement setup would require switching primary ion beams between Kr+ for water and Hg+ for propofol. Switching back and forth between the two ion beams takes a total time of about 800 ms and therefore would result in a reduced time resolution of the propofol measurements. Additionally, it is not clear how the use of active humidifiers and heat moisture exchange filters routinely used during mechanical ventilation would interfere with the quantification of water vapour. Therefore, quantification of isoprene seems to be more suitable for the identification of the respiratory cycle than quantification of water vapour when IMR-MS is used for breath monitoring.
When isoprene is used for the identification of expiratory propofol one has to choose a threshold value for changes in isoprene concentrations that is able to detect the different phases of the respiratory cycle. Isoprene breath concentrations may vary according to the investigated population or breath sampling method, e.g., between studies in healthy pupils, volunteers, ventilated patients or when mixed expiratory gas is compared to end-expiratory gas. For example, previous studies reported expiratory isoprene breath concentrations of 37 ppb in 200 healthy pupils, 99 ppb in the mixed expiratory breath of 205 adult volunteers, and 224 ppb in end-expiratory breath of 62 patients during mechanical ventilation [8, 20, 21].
In the data set used for this work average expiratory isoprene concentrations ranged from 240 [187–335] ppb with a median difference between expiratory and inspiratory isoprene of 182 [124–234] ppb (median [IQR]). Therefore, the choice of a relative increase and decrease in isoprene breath concentrations of 40 ppb seems reasonable for the identification rather than selecting an absolute threshold value. For investigations in children, it might be necessary to adjust the threshold for relative changes in breath concentrations as lower isoprene concentrations were reported in children [21].
In our study, the overall advantage of measuring breath isoprene concentrations is the potential reduction in the complexity of the measurement equipment. In case of IMR-MS, determination of isoprene could allow omission of CO2 measurement with an additional EI-MS.
One limitation of our study is that isoprene measurements were only available every 1.2 s, about three times less often than CO2 measurements. Therefore, the isoprene signal may be less precise than the CO2 signal for identification of expiratory propofol. Yet, the overall bias of the isoprene extraction method compared to the CO2 method and extended CO2 method was very small with −0.12 and 0.10 ppb, rsp. Despite that low bias, isoprene could be measured more frequently in future studies by changing the measurement setup of the IMR-MS. Instead of measuring isoprene only once per each measurement of the propofol fragments 163 and 178, i.e. every 1.2 s, it could be measured more often resulting in a better resolution of the respiratory cycle. For example, one may focus on propofol fragment 163. A potential setup could then consist only of propofol 163 and isoprene measured consecutively. A reduction of the integration time for isoprene from 200 to 50 ms is also technically feasible. Hence, one cycle in such a measurement setup would only take 500 ms for propofol 163 and 50 ms for isoprene and result in isoprene measurements (when cycle times are included) <600 ms. Such a setup may result in an even smaller bias in expiratory propofol signal identified by CO2 and isoprene. However, using isoprene as a marker substance for expiratory air comes at the cost of losing time for the determination of the actual compound of interest as only one compound can be measured at a time. In the setup used in our study, about 17 % (200/1,206 ms) of measurement time in one cycle was needed for determination of isoprene. A potential future measurement setup with an integration time of 500 ms for propofol and 50 ms for isoprenen would need about 10 % of the overall measurement time for the identification of the different phases of the respiratory cycle. Yet, such a setup would still yield 109 propofol measurements per minute and thus provide very rich propofol breath data.
In summary, isoprene breath concentrations can be used for the identification of the different phases of the respiratory cycle. Future investigations involving real-time measurements of expiratory propofol may use isoprene breath concentrations for the identification of the expiratory propofol signal.
References
Hornuss C, Praun S, Villinger J, Dornauer A, Moehnle P, Dolch M, Weninger E, Chouker A, Feil C, Briegel J, Thiel M, Schelling G. Real-time monitoring of propofol in expired air in humans undergoing total intravenous anesthesia. Anesthesiology. 2007;106(4):665–74.
Perl T, Carstens E, Hirn A, Quintel M, Vautz W, Nolte J, Junger M. Determination of serum propofol concentrations by breath analysis using ion mobility spectrometry. Br J Anaesth. 2009;103(6):822–7. doi:10.1093/bja/aep312.
Takita A, Masui K, Kazama T. On-line monitoring of end-tidal propofol concentration in anesthetized patients. Anesthesiology. 2007;106(4):659–64.
Grossherr M, Hengstenberg A, Meier T, Dibbelt L, Gerlach K, Gehring H. Discontinuous monitoring of propofol concentrations in expired alveolar gas and in arterial and venous plasma during artificial ventilation. Anesthesiology. 2006;104(4):786–90.
Miekisch W, Fuchs P, Kamysek S, Neumann C, Schubert JK. Assessment of propofol concentrations in human breath and blood by means of HS-SPME-GC-MS. Clin Chim Acta. 2008;395(1–2):32–7.
Hornuss C, Wiepcke D, Praun S, Dolch ME, Apfel CC, Schelling G. Time course of expiratory propofol after bolus injection as measured by ion molecule reaction mass spectrometry. Anal Bioanal Chem. 2012;403(2):555–61. doi:10.1007/s00216-012-5856-3.
Boshier PR, Cushnir JR, Mistry V, Knaggs A, Spanel P, Smith D, Hanna GB. On-line, real time monitoring of exhaled trace gases by SIFT-MS in the perioperative setting: a feasibility study. Analyst. 2011;136(16):3233–7. doi:10.1039/c1an15356k.
Hornuss C, Zagler A, Dolch ME, Wiepcke D, Praun S, Boulesteix AL, Weis F, Apfel CC, Schelling G. Breath isoprene concentrations in persons undergoing general anesthesia and in healthy volunteers. J Breath Res. 2012;6(4):046004. doi:10.1088/1752-7155/6/4/046004.
Spanel P, Smith D. Progress in SIFT-MS: breath analysis and other applications. Mass Spectrom Rev. 2011;30(2):236–67. doi:10.1002/mas.20303.
Dolch M, Frey L, Hornuss C, Schmoelz M, Praun S, Villinger J, Schelling G. Molecular breath-gas analysis by online mass spectrometry in mechanically ventilated patients: a new software-based method of CO2-controlled alveolar gas monitoring. J Breath Res. 2009;2:10.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–10.
Bland JM, Altman DG. Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet. 1995;346(8982):1085–7.
Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8(2):135–60.
Bland JM, Altman DG. Agreement between methods of measurement with multiple observations per individual. J Biopharm Stat. 2007;17(4):571–82. doi:10.1080/10543400701329422.
Miekisch W, Kischkel S, Sawacki A, Liebau T, Mieth M, Schubert JK. Impact of sampling procedures on the results of breath analysis. J Breath Res. 2008;2(2):026007. doi:10.1088/1752-7155/2/2/026007.
Anderson JC, Hlastala MP. Breath tests and airway gas exchange. Pulm Pharmacol Ther. 2007;20(2):112–7. doi:10.1016/j.pupt.2005.12.002.
Grossherr M, Hengstenberg A, Dibbelt L, Igl BW, Noel R, Knesebeck A, Schmucker P, Gehring H. Blood gas partition coefficient and pulmonary extraction ratio for propofol in goats and pigs. Xenobiotica. 2009;39(10):782–7. doi:10.1080/00498250903056109.
King J, Kupferthaler A, Unterkofler K, Koc H, Teschl S, Teschl G, Miekisch W, Schubert J, Hinterhuber H, Amann A. Isoprene and acetone concentration profiles during exercise on an ergometer. J Breath Res. 2009;3(2):027006. doi:10.1088/1752-7155/3/2/027006.
Schwoebel H, Schubert R, Sklorz M, Kischkel S, Zimmermann R, Schubert JK, Miekisch W. Phase-resolved real-time breath analysis during exercise by means of smart processing of PTR-MS data. Anal Bioanal Chem. 2011;401(7):2079–91. doi:10.1007/s00216-011-5173-2.
Kushch I, Arendacka B, Stolc S, Mochalski P, Filipiak W, Schwarz K, Schwentner L, Schmid A, Dzien A, Lechleitner M, Witkovsky V, Miekisch W, Schubert J, Unterkofler K, Amann A. Breath isoprene–aspects of normal physiology related to age, gender and cholesterol profile as determined in a proton transfer reaction mass spectrometry study. Clin Chem Lab Med. 2008;46(7):1011–8. doi:10.1515/CCLM.2008.181.
Smith D, Spanel P, Enderby B, Lenney W, Turner C, Davies SJ. Isoprene levels in the exhaled breath of 200 healthy pupils within the age range 7-18 years studied using SIFT-MS. J Breath Res. 2010;4(1):017101. doi:10.1088/1752-7155/4/1/017101.
Acknowledgments
This work was funded by departmental funds of the Department of Anaesthesiology at the Ludwig-Maximilians-University, Munich, Germany (Klinikum der Universität München). Additionally, V&F medical development supported the study by providing an ion molecule reaction mass spectrometry system during the study period. Siegfried Praun, Ph.D. is a scientist employed by V&F medical development. Cyrill Hornuss, M.D. received an unrestricted research grant from V&F. V&F reimbursed the travel expenses of Cyrill Hornuss and Michael Dolch, M.D. for meeting presentations related to this research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hornuss, C., Dolch, M.E., Janitza, S. et al. Determination of breath isoprene allows the identification of the expiratory fraction of the propofol breath signal during real-time propofol breath monitoring. J Clin Monit Comput 27, 509–516 (2013). https://doi.org/10.1007/s10877-013-9452-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-013-9452-7