Abstract
Purpose
A potent immunomodulatory role of Vitamin D in both innate and adaptive immunity has recently been appreciated. In allergic asthma, activation of NF-кB induces transcription of various cytokines and chemokines involved in allergic airway inflammation. The nuclear import of activated NF-кB p50/RelA subunit is dependent on importin α3 (KPNA4) and importin α4 (KPNA3). In this study, we examined the role of importin α3 in immunomodulatory effect of calcitriol in human bronchial smooth muscle cells (HBSMCs).
Methods
Cultured HBSMCs were stimulated with calcitriol in the presence and absence of cytokines, TNF-α, IL-1β, and IL-10. The mRNA transcripts of importin α3 and α4 were analyzed using qPCR while protein expression of importin α3, α4 and nuclear RelA was analyzed by immunoblotting.
Results
Calcitriol significantly decreased mRNA and protein expression of importin α3 as well as nuclear protein expression of NF-кB p65 (RelA). The decreased activation of RelA by calcitriol was confirmed by decreased release of RelA-inducible molecules, including IL-5, IL-6 and IL-8, by HBSMCs upon calcitriol treatment. Calcitriol attenuated the effect of TNF-α and IL-1β to upregulate mRNA and protein expression of importin α3. IL-10 significantly decreased the TNF-α induced expression of importin α3 and this effect was further potentiated by calcitriol.
Conclusions
These data suggest that under inflammatory conditions, calcitriol decreases the expression of importin α3 resulting in decreased nuclear import of activated RelA. This could be a novel mechanism by which calcitriol could exert its immunomodulatory effects to reduce allergic airway inflammation and thus may alleviate the symptoms in allergic asthma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Asthma is a chronic airway disease characterized by airway hyperresponsiveness (AHR), airway obstruction, airway remodeling, and infiltration of eosinophils and T-helper type 2 (Th2) cells into the airway sub-mucosa, which leads to inflammation and edema in the bronchial mucosa, and hypersecretion of mucous [1, 2]. Approximately 300 million people are affected by asthma worldwide. Its prevalence has increased significantly in developed countries and showing similar trends in developing nations recently [3].
Bronchial smooth muscle cells (BSMCs) play essential role in the pathogenesis of asthma [4]. There is narrowing of bronchial lumen due to increase in BSMC mass. BSMCs, when activated in a sensitized state, behave in an autocrine and paracrine manner by producing and responding to cytokines and other pro-inflammatory molecules [4]. Some of the main pro-inflammatory cytokines and chemokines secreted by the smooth muscle cells in asthma are TNF-α, IL-1β, IL-5, IL-6, IL-17, GM-CSF, TGF-β, IL-8, RANTES, eotaxin, and MCP-1,2,3 [5, 6]. This synthetic role of smooth muscles and the secretion of the cytokines are regulated by numerous transcriptional factors that play an important role in the pathogenesis of asthma [7]. NF-κB is one of the central transcriptional factor that co-ordinates the expression of various immune and inflammatory genes [8, 9]. There is an enhanced NF-κB activation pathway in asthmatic tissues [10]. NF-κB is activated in response to a number of stimuli, including physical and chemical stress, LPS, dsRNA, ssRNA, T and B cell mitogens and pro-inflammatory cytokines [10]. The cytokines secreted by smooth muscle cells in asthma including TNF-α, IL-1β and IL-17 are responsible for activation of NF-κB [11]. Activated NF-κB induces the rapid expression of multiple genes that play a significant role in induction of airway hyperresponsiveness, airway smooth muscle proliferation and inhibition of cell apoptosis in asthma [11–14].
Under physiological conditions, NF-κB is sequestrated in the cytoplasm in association with an inhibitory protein called IκB which controls the activation and regulation of NF-κB [15]. Upon activation, cytoplasmic NF-κB complexes, especially p50-RelA, rapidly translocate to the nucleus [16].
The transport of the molecules in and out of the cell is monitored by nuclear pore complexes (NPC). Importins are the proteins that help larger molecules to enter into the nucleus and exportin to move back to the cytoplasm. Proteins containing classical nuclear localizing sequence (NLS) are imported in the nucleus by importin α/β heterodimers [17]. Classical NLS are found in RelA (p65) and p50 subunits of NF-κB [17]. Importin α3 and importin α4 are reported to be the main importin α isoforms responsible for the nuclear translocation of NF-κB p50-RelA heterodimer on stimulation with TNF-α [17–19]. The activation of NF-κB subunits p50-RelA is detrimental in the pathogenesis of asthma and results in severe airway inflammation [18, 20]. Therefore, the inhibition of NF-κB activation or translocation would be an important focus for the development of new therapeutic modalities in asthma [20]. Thus, the drugs specifically designed to target NF-κB activation or its translocation would be clinically useful for the treatment of inflammatory diseases, including asthma [21].
Vitamin D has been known for the maintenance of calcium and phosphate homeostasis in our body. In recent years, growing body of literature suggest the role of Vitamin D in cell growth, proliferation and differentiation, and in the immune regulation of our body [22]. Calcitriol is an active metabolite of Vitamin D3, exerts its action through Vitamin D receptor (VDR), which is a member of the superfamily of high affinity steroid nuclear receptors [23, 24]. VDR is a transcription factor that interacts with its co-regulators and alters the transcription of target gene which are involved in a wide spectrum of biological responses [22].
VDR is constitutively expressed in immunologically relevant cells, including antigen presenting cells like dendritic cells and macrophages, and is induced in activated T lymphocytes indicating a central role of Vitamin D in immune regulation [25, 26]. These observations support that Vitamin D has immunosuppressive and immunomodulatory properties. However the underlying cellular and molecular mechanisms are unknown. In this study, we for the first time report the effect of calcitriol on the expression of importin α3, RelA activation and migration to the nucleus and demonstrate decreased expression and activity of importin α3 and RelA with calcitriol treatment in HBSMCs.
Materials and Methods
Cell Culture
Primary human bronchial smooth muscle cells (HBMSC) were obtained from ScienCell Research laboratories. Cells were cultured in 25 cm2 cell culture flasks in Smooth Muscle Cell Medium (SMCM) containing 10 % FBS and were maintained at 5 % CO2 at 37°C. Cells from passage 3–7 maintained their SMC phenotype and were used in all experiments. Cells were characterized for smooth muscle cell markers including smooth muscle α-actin and smooth muscle heavy chain by immunofluorescence.
Cell Stimulation
All experiments were done in three biologically independent samples. Cultured HBSMCs (70–80 % confluent cells) were growth arrested by serum starvation for 24 h by replacing the FBS containing SMCM with FBS free DMEM (Dulbecco’s modified eagle’s medium). After 24 h cells were stimulated with calcitriol (D1530 Sigma-Aldrich, St. Louis, MO) at various concentrations (0.1–100 nM) or ethanol (<0.05 %) as vehicle in fresh DMEM for 24 h. Recombinant TNF-α, IL-1β and IL-10 (PeproTech, Inc. NJ) were used at a dose of 10 ng/ml. After 24 h of stimulation, cells were harvested for RNA and protein. Each experiment was done in triplicate.
Cytokine Measurements
After appropriate stimulation with calcitriol ± TNF-α ± dexamethasone for 24 h the level of cytokines, IL-5, IL-6 and IL-8, secreted in the culture medium by HBSMCs was determined by ELISA according to the manufacturer’s instructions using ELISA Detection Ready-Set-Go kit (eBioscience, San Diego, CA)
RNA Isolation, Reverse Transcription and Real Time PCR
Total cellular RNA was extracted and mRNA expression was analyzed by Real Time PCR by methods described previously [27]. Calculation of relative gene expression was done based on the differences in the threshold cycles (Ct). The results were normalized against glyceraldehyde 3-phosphate dehydrogenase (GAPDH).
The primer sequences used are as follows:
GAPDH | Forward primer: GGGAAGGTGAAGGTCGGAGT |
Reverse primer: TTGAGGTCAATGAAGGGGTCA | |
VDR | Forward primer: CTTCAGGCGAAGCATGAAGC |
Reverse primer: CCTTCATCATGCCGATGTCC | |
CYP24A1 | Forward primer: CAAACCGTGGAAGGCCTATC |
Reverse primer: AGTCTTCCCCTTCCAGGATCA | |
CYP27B1 | Forward primer: TGGCCCAGATCCTAACACATTT |
Reverse primer: GTCCGGGTCTTGGGTCTAACT | |
Importinα3 (KPNA4) | Forward primer: TGTGAGCAAGCAGTGTGGGCA |
Reverse primer: TGGTGGTGGGTCTTTGTGGCG | |
Importin α4 (KPNA3) | Forward Primer: ATCCCCCGCCGCCTATGGAG |
Reverse Primer: CTGGGTCTGCTCGTCGGTGC |
Whole Cell and Nuclear Protein Extraction
The cell monolayer was washed with serum free medium and the whole cell protein was extracted as described previously [28]. The Nuclear protein was extracted according to the manufacture’s protocol (Active Motif, CA #40010). The cell monolayer was washed with cold PBS/phosphatase inhibitors. Cells were gently scraped with cell lifter, collected in PBS/phosphatase inhibitor and centrifuged. The pellet was gently resuspended in 150 μl 1× hypotonic buffer and 5 μl detergent was added followed by vortex for 10 s, centrifuged and supernatant was collected (cytoplasmic fraction). The pellet was resuspended in 30 μl complete lysis buffer and incubated for 30 min. After centrifugation the nuclear fraction was collected.
Transfection of the Cells
To Knockdown VDR and importin α3 genes HBSMCs were transfected with human (h)VDR-small interfering (si)RNA oligonucleotides (sc-106692) (Santa Cruz Biotechnology, CA), (h)KPNA4 siRNA (H00003840-R01) (Novus Biologicals, LLC,CO) or scrambled siRNA oligonucleotides (sc-37007) (Santa Cruz Biotechnology, CA) serving as a negative control using FuGENE-HD Transfection reagent (Roche Applied Science, Germany) according to manufacturer’s instruction. The Transfection efficiency was measured using Green Fluorescent Protein as a marker, which showed more than 85 % of the cells expressing GFP and a viability of 95 % after 30 h. The knockdown efficiency was analyzed by western blot analysis.
Luciferase Reporter Gene Assay
Human bronchial smooth muscle cells were seeded in 96-well plate at the density of 1 × 104 cells/well. After 24 h, cells were transfected with 100 ng of importin α3- responsive firefly luciferase promoter reporter (Ori-gene, Rockville, MD) or NF-κB-responsive firefly luciferase reporter and constitutively expressing Renilla construct (40:1) (SA Biosciences, Frederick, MD) using FuGENE-HD transfection reagent (Roche Applied Science, Germany). Thirty hours after transfection, cells were treated with calcitriol (100 nM) for 20 h followed by treatment with TNF-α (10 ng/ml) for an additional 4 h. Luciferase activities were assessed using Dual-Glo® Luciferase Assay System (Promega, Fitchburg, WI) following manufacturer’s protocol and the luminescence was measured with Enspire 2300 multilabel plate reader (PerkinElmer, Inc. CA).
Immunoblotting
Immunoblotting was done by methods as described previously [28]. The lysates were separated by gel electrophoresis and transferred onto nitrocellulose membranes (Bio-Rad Laboratories, Hercules, CA). The following antibodies were used in 1:500 dilutions: VDR (D-6,SC-13133) (mouse, Santa Cruz Biotechnology, CA), CYP24A1 (H00001591, Mouse, Abnova, CA), CYP27B1 (H-90,SC-67261) (rabbit, Santa Cruz Biotechnology, CA), KPNA4 (ab6039) (goat, Abcam MA), KPNA3 (ab6038) (goat, Abcam MA), NF-κB p65 (sc-372)(rabbit, Santa Cruz Biotechnology, CA), and Lamin B (sc-6216) (goat, Santa Cruz Biotechnology, CA). Protein expression in whole cell lysate was normalized against GAPDH. For nuclear extracts, results were normalized by Lamin B.
Statistical Analysis
Values of all measurements are reported as mean ± SEM. The Graph Pad Prism 4.0 biochemical statistical package (Graph Pad Software, Inc, San Diego, CA USA) software was used to analyze data and plot graphs. Statistical analysis was performed using one-way ANOVA to analyze statistically significant differences between groups. Post-hoc test included either Dunnett or Bonferroni’s test. The level of significance was calculated based on the P values (*P < 0.05, **P < 0.01, ***P < 0.001)
Results
Calcitriol Increases mRNA Transcripts and Protein Expression of VDR in HBSMCs
The unstimulated HBSMCs express VDR. Following calcitriol (0.1–100 nM) treatment, there was significant increase in both mRNA and protein expression of VDR in HBSMCs (Fig. 1a–b) Calcitriol increased mRNA transcripts and protein expression of CYP24A1 and decreased the mRNA transcripts and protein expression of CYP27B1 in HBSMCs (See Supplementary data Figure S1A–D). The effect of calcitriol (100 nM) on the mRNA expression of VDR was time-dependent with the maximum expression at 18–36 h (See Supplementary data Figure S2).
Effect of Calcitriol treatment on mRNA and protein expression of VDR (a, b), in HBSMCs: Cultured HBSMCs were serum starved for 24 h followed by treatment with different doses of calcitriol (0.1–100 nM) for 24 h. The mRNA and protein were isolated from cell lysates and subjected to qPCR and immunoblotting, respectively. Data is shown as mean ± SEM from three individual samples in each experiment; ***p < 0.001, **p < 0.01
Calcitriol Decreases mRNA Transcripts and Protein Expression of Importin α3 in HBSMCs
The unstimulated HBSMCs expressed both mRNA transcripts and protein of importin α3 . Following calcitriol (0.1–100 nM) treatment, there was significant decrease in both mRNA and protein expression of importin α3 in HBSMCs (Fig. 2a, b). However, there was no significant effect of calcitriol on the mRNA and protein expression of importin α4 (see Supplementary data Figure S4A,B). These results show that active metabolite of vitamin D decreases the expression of importin α3 with no effect on importin α4. The effect of calcitriol on the mRNA expression of importin α3 was time-dependent with a maximum decrease at 24 h (See Supplementary data Figure S3).
Effect of Calcitriol treatment on mRNA and protein expression of importin α3 (a, b) and importin α4 (c, d) in HBSMCs: Cultured HBSMCs were serum starved for 24 h followed by treatment with different doses of calcitriol (0.1–100 nM) for 24 h. The mRNA and protein were isolated from cell lysates and subjected to qPCR and immunoblotting, respectively. Data is shown as mean ± SEM from three individual samples in each experiment; ***p < 0.001, **p < 0.01
VDR Knockdown Abolishes the Reduced Expression of Importin α3 by Calcitriol in HBSMCs
To further explore the role of VDR in the regulation of importin α3, we evaluated the effect of VDR reduction in HBSMCs. VDR knockdown abolished calcitriol-induced decreased expression of importin α3. The VDR expression was reduced using hVDR -specific siRNA, with scrambled siRNA as a control. As shown in Fig. 3a, 30 h after siRNA transfection, the VDR protein expression was markedly reduced and the knockdown efficiency was nearly 90 %. The calcitriol treatment failed to reduce the expression of importin α3 in the VDR-siRNA-transfected cells, in contrast to the scrambled siRNA-treated cells (Fig. 3b). These data demonstrate that VDR knockdown abolishes calcitriol-induced inhibition of importin α3. These results are consistent with and support the data presented in Fig. 2a, b which show that calcitriol significantly decreases the expression of importin α3 in HBSMCs.
Effect of VDR siRNA on the expression of VDR (a) and the effect of calcitriol treatment on the protein expression of importin α3 (b) in VDR knockdown HBSMCs: Cultured HBSMCs were transfected with VDR siRNA or scrambled siRNA and were stimulated with calcitriol (100 nM) for 24 h. Protein was isolated from cell lysates and subjected to immunoblotting. Data is shown as mean ± SEM from three individual samples in each experiment; ***p < 0.001
TNF-α Increases the Expression of Activated RelA in the Nuclear Fraction of HBSMCs in a Dose- and Time-Dependent Manner
Pro-inflammatory cytokines, IL-1β and TNF-α, have been shown to play a prominent role in developing airway responsiveness and airway inflammation in bronchial asthma. HBSMCs were treated with different concentration of TNF-α (1–100 ng/ml) for 20 min, as the half-life of activated RelA is less than 30 min [29]. There was a basal level of RelA in the nucleus under unstimulated conditions. TNF-α (10–100 ng/ml) significantly increased the nuclear protein expression of RelA (Fig. 4a). However, the viability of the cells was significantly affected at TNF-α (100 ng/ml). Therefore, a dose of 10 ng/ml TNF-α was chosen in the following experiments.
Effect of TNF-α on the expression of activated-RelA in the nuclear fraction of HBSMCs in a dose and time dependent manner(a,b),Effect of importin α3 siRNA on the expression of importin α3 (c) & Effect of calcitriol on nuclear protein expression in importin α3 knockdown HBSMCs on stimulation with TNF-α: HBSMCs were treated with different doses of TNF-α (1–100 ng/ml) for 20 min (a) and TNF-α (10 ng/ml) at 0–60 min (b). The nuclear protein was extracted and analyzed for RelA by immunoblotting. HBSMCs were treated with calcitriol (100 nM) for 24 h followed by TNF-α (10 ng/ml) for 15 min. Cultured HBSMCs were transfected with importin α3 siRNA or scrambled siRNA and were stimulated with calcitriol (100 nM) and TNF-α (10 ng/ml) for 24 h. The nuclear protein (d) was extracted for RelA by Immunoblotting. Lamin B was used as a housekeeping gene for nuclear protein. Data is shown as mean ± SEM from three individual samples in each experiment; **p < 0.01, ***p < 0.001
Next, HBSMCs were treated with TNF-α (10 ng/ml) at different time periods (0–60 min). The nuclear protein expression of RelA in HBSMCs in response to TNF-α increased in a time-dependent manner with the maximum expression at 15 min and returned to the baseline at 30 min and beyond (Fig. 4b). Therefore, in the following nuclear experiments HBSMCs were treated with a dose of 10 ng/ml of TNF-α for 15 min.
Calcitriol Decreases Expression of Activated RelA in the Nuclear Fraction of TNF-α Stimulated HBSMCs and Importin α3 Knockdown Decreases the TNF-α Induced Activation of RelA and Abolishes the Action of Calcitriol on RelA Translocation in the Nuclear Fraction of HBSMCs
The importin α3 was knocked down using human importin α3 specific siRNA, and scrambled siRNA was used as a control. As shown in Fig. 4c, 30 h after siRNA transfection, the importin α3 protein expression was markedly reduced and knockdown efficiency was nearly 85 %.
On stimulation with TNF-α (10 ng/ml) for 15 min there was a significantly increased nuclear translocation of RelA and this effect was attenuated by calcitriol, indicating that calcitriol decreases the translocation of RelA to the nucleus (Fig. 4d). To verify the role of importin α3 to translocate RelA from cytoplasm to the nucleus,, we evaluated the effect of TNF-α to increase RelA expression in the nucleus in importin α3 siRNA-transfected HBSMCs. Importin α3 knockdown decreased the translocation of RelA to the nucleus in response to TNF-α. Since there was not complete absence of RelA translocation to the nucleus, this suggests a potential role of importin α4 [17].
In the TNF-α-treated importin α3-siRNA-transfected cells, RelA expression was significantly downregulated compared to TNF-α-treated non-transfected cells. Our results are in accordance with previous studies confirming that importin α3 plays a major role in RelA translocation to the nucleus [17, 30]. Concomitant treatment of importin α3-siRNA-transfected cells with TNF-α and calcitriol had no significant effect on RelA expression compared to TNF-α treated importin α3-siRNA transfected cells without calcitriol.
These data confirm that the action of calcitriol to reduce RelA translocation is mediated by decrease in importin α3 expression.
Calcitriol Decreases TNF-α Induced RelA and Importin α3 Transactivation
To confirm our observation on the decrease in TNF-α-induced nuclear protein expression of RelA by calcitriol, we examined the RelA transactivation by transfecting HBSMCs with NF-κB-luciferase reporter vector. TNF-α induced a 5-fold increase in relative luciferase gene expression that was significantly reduced by calcitriol. This suggests that calcitriol attenuates the TNF-α induced NF-κB transactivation (Fig. 5a). In order to validate whether the decrease in the activation of NF-κB by calcitriol is because of a decrease in the transactivation of importin α3, we examined the promoter activity of importin α3 with TNF-α ± calcitriol. There was ~50 % reduction in the activation of importin α3 with calcitriol, TNF-α induced the transactivation of importin α3 by more than 3-fold and this was significantly reduced by calcitriol (Fig. 5b). This suggests that calcitriol specifically reduced the TNF-α mediated importin α3 activation which further results in the reduction in the TNF-α induced activation of RelA (NF-κB p65).
Effect of calcitriol on TNF-α Induced RelA (a) and importin α3 (b) Transactivation: HBSMCs were seeded in 96-well plate for 24 h, followed by transfection with 100 ng NF-κB-responsive firefly luciferase reporter (a) and importin α3 luciferase reporter (b) using FuGENE-HD transfection reagent. Thirty hours after transfection, cells were treated with calcitriol (100 nM) for 20 h followed by treatment with TNF-α (10 ng/ml) for an additional 4 h. Luciferase activities were assessed using Dual-Glo® Luciferase Assay System. Data is shown as mean ± SEM from three individual samples in each experiment; **p < 0.01, ***p < 0.001
Calcitriol Decreases TNF-α- and IL-1β-Induced mRNA Transcript and Protein Expression of Importin α3 in HBSMCs
The effect of the pro-inflammatory cytokines on the expression of importin α3 was examined. HBSMCs were treated with calcitriol (100 nM) ± TNF-α (10 ng/ml)/IL-1β (10 ng/ml) for 24 h, followed by RNA and protein isolation for qPCR and immunoblotting, respectively. Following TNF-α treatment, there was ~3-fold increase in mRNA expression (Fig. 6a) and significant increase in protein expression (Fig. 6b) of importin α3. However, calcitriol treatment attenuated the TNF-α-induced increase in the expression of importin α3 (Fig. 6).
Effect of calcitriol ± TNF-α/IL-1β on mRNA transcript and protein expression of importin α3 in HBSMCs: Cultured HBSMCs were serum starved for 24 h followed by treatment with TNF-α (10 ng/ml) (a,b)/IL-1β (10 ng/ml) (c,d) ± calcitriol (100 nM) for 24 h. The mRNA and protein was isolated from whole cell lysates and subjected to qPCR and immunoblotting respectively. Data is shown as mean ± SEM from three individual samples in each experiment *p < 0.05, **p < 0.01, ***p < 0.001
After IL-1β treatment, there was ~2-fold increase in mRNA expression and significant increase in protein expression of importin α3 (Fig. 6c, d). However, calcitriol treatment attenuated the IL-1β induced increase in the expression of importin α3.
IL-10 Decreases TNF-α Induced Expression of Importin α3 and This Effect is Potentiated by Calcitriol
HBSMCs were treated with calcitriol (100 nM) ± IL-10 (10 ng/ml) ± TNFα (10 ng/ml) for 24 h, followed by RNA and protein isolation for qPCR and Western blotting. On stimulation with IL-10, there was no significant change in the mRNA and protein expression of importin α3 compared to control. This led us to conclude that IL-10 might not exert any effect on the expression of importin α3. However, IL-10 significantly attenuated the TNF-α- induced increase in the expression of importin α3 and the effect of IL-10 on the expression of importin α3 was further potentiated by addition of calcitriol (Fig. 7a, b).
Effect of IL-10 ± TNF-α ± calcitriol on mRNA transcript (a) and protein expression (b) of importin α3 in HBSMCs: Cultured HBSMCs were serum starved for 24 h followed by treatment with IL-10 (10 ng/ml) ± TNF-α (10 ng/ml) ± calcitriol (100 nM) for 24 h. mRNA and protein was isolated from whole cell lysates and subjected to qPCR (a) and immunoblotting (b), respectively. Data is shown as mean ± SEM from three individual samples in each experiment *p < 0.05, **p < 0.01,***p < 0.001
Calcitriol Decreases TNF-α Induced IL-5, IL-6 and IL-8 Secretion Which was Further Decreased by Dexamethasone Treatment
We analyzed the effect of calcitriol in the presence and absence of dexamethasone on IL-5, IL-6, and IL-8 levels secreted by TNF-α-stimulated smooth muscle cells. HBSMCs were treated with TNF-α (10 ng/ml) ± calcitriol (100 nM) ± dexamethasone (10 ng/ml) for 24 h. The protein levels of inflammatory mediators were measured by ELISA (Fig. 8a, b, c). TNF-α treatment markedly increased the production of IL-5, IL-6, and IL-8. Calcitriol significantly reduced the levels of these cytokines. However, a combination of calcitriol and dexamethasone additively decreased the secretion of the cytokines compared to calcitriol alone.
Effect of calcitriol ± Dexamethasone on TNF-α induced IL-5, IL-6 and IL-8 secretion: Cultured HBSMCs were serum starved for 24 h followed by treatment with TNF-α (10 ng/ml) ± dexamethasone ± calcitriol for 24 h. The secretion of cytokines- IL-5 (a), IL-6 (b) and IL-8 (c) secretion in the culture medium by HBSMCs were determined by ELISA. Data is shown as mean ± SEM from three individual samples in each experiment *p < 0.05, **p < 0.01, ***p < 0.001
Discussion
In this study, we for the first time, report the effect of calcitriol on the mRNA and protein expression of importin α3 and importin α4 in HBSMCs. We found that calcitriol down-regulates the mRNA and protein expression of importin α3 with no significant effect on importin α4. This decrease in importin α3 correlates with calcitriol-induced decrease in the migration of activated RelA from the cytoplasm to the nucleus.
The importin and exportin transport system present the mechanism involved in the nucleo-cytoplasmic transport [19]. Any change in the expression of the components involved in the nucleo-cytoplasmic transport machinery may play a crucial role in gene transcription and translation [19]. Currently, little is known about the regulation of importins and exportins in the airway cells. Thus, our findings on the effect of vitamin D to decrease both importin α3 and activation of NF-κB are significant.
The action of calcitriol is mediated via stimulation of vitamin D receptor [23]. There is a direct involvement of genes, CYP24A1 and CYP27B1, in the metabolism of Vitamin D and hence these are the gene of interest in vitamin D pathway [49]. CYP27B1 encodes for 1-α-hydroxylase, which converts 25-hydroxy-vitamin D [25(OH)D] into the active vitamin D metabolite 1,25(OH)2D. CYP24A1 encodes for 24-hydroxylase, the enzyme that catalyzes the inactivation of 1,25(OH)2D [49]. In this study, we found that calcitriol increased VDR and CYP24A1 expression and decreased CYP27B1 expression in HBSMCs in a dose-dependent manner. Our data is in accordance with previous studies that revealed an increased expression of VDR and CYP24A1 with vitamin D analogues in bronchial and tracheal smooth muscle cells [4, 31]. The expression of VDR and its metabolizing enzymes in airway smooth muscle cells (ASM) suggests that ASM possesses the machinery to locally metabolize vitamin D and HBSMCs functionally respond to vitamin D [49].
In asthmatics, there is an increase in the levels of various pro-inflammatory cytokines, including TNF-α, IL-1β, that activate NF-κB. Indeed, the administration of TNF-α to a normal subject can lead to the development of airway hyperresponsiveness and airway neutrophilia [4, 24, 31]. Thus, our findings in human cells could be directly relevant to in-vivo in asthmatic subjects.
There are several studies examining the therapeutic role of vitamin D in asthma. It has been postulated that the deficiency of vitamin D may lead to the development of asthma in the offspring of pregnant women since vitamin D is required for the lung growth in utero [32–34] Supplementing pregnant women with high doses of Vitamin D reduces the asthma risk by 40 % in children aged 3–5 years [35]. In a study by Brehm and colleagues [36] on 616 children with asthma of Costa Rica low levels of vitamin D were associated with more severity of asthma and allergy. A lower serum vitamin D levels was associated with a higher AHR and an increased levels of TNF-α [37]. Vitamin D deficiency is associated with decreased lung volume, decreased lung function and altered lung structure [38]. A recent study concluded that the children with severe, therapy-resistant asthma having lower Vitamin D levels had increased airway smooth muscle (ASM) mass and worse asthma control and lung function [39]. All of these reports further support the clinical importance of our findings in bronchial smooth muscle cells in regard to the anti-inflammatory and immunomodulatory effect of vitamin D.
Recent studies also demonstrate that VDR is directly involved in the regulation of NF-κB activation. In dendritic cells calcitriol targets the NF-κB pathway by inhibiting IL-12 expression [40]. In human fibroblasts and keratinocytes, calcitriol decreases the DNA binding capacity of NF-κB [41, 42]. Vitamin D is reported to significantly downregulate pro-inflammatory chemokines in pancreatic islet cells, which is associated with the up-regulation of IκBα transcription and the arrest of NF-κB RelA nuclear translocation [43]. In mouse embryonic fibroblasts VDR plays an inhibitory role in the regulation of NF-κB activation [44]. Together, these studies suggest that vitamin D has an inhibitory action on NF-κB activation. However, the underlying mechanisms are not clear. Based on our findings in this study calcitriol inhibits nuclear translocation of NF-κB by downregulating importin α3. These results were confirmed by knocking down importin α3 in HBSMCs. The decrease in NF-κB activation by calcitriol was established by a decrease in the nuclear protein expression of RelA when stimulated with TNF-α. Calcitriol suppression on TNF-α induced transcriptional activation of importin α3 and NF-κB p65 was confirmed by luciferase assay. The downstream effect of calcitriol on NF-κB was analyzed by measuring the levels of NF-κB-inducible genes, IL-5, IL-6, and IL-8,that are secreted by smooth muscle cells on stimulation with TNF-α. Calcitriol additively increased the effect of dexamethasone that is the main stay in the treatment of asthma. Our results are in accordance to previous studies that showed that calcitriol exerts anti-inflammatory activity in ASMs by modulating the expression of chemokines relevant to the pathogenesis of asthma [31]. Calcitriol may be used as a therapeutic agent in the prevention of airway remodeling manifested as increases in ASM mass, as found in asthmatic subjects [24]. This further highlights the potential significance of vitamin D in the modulation of ASM function in bronchial asthma.
A study by Theiss and colleagues [18] revealed that in colonic mucosal biopsies of moderately-to-severely inflamed Crohn’s disease patients there was an increased expression of importin α3. TNF-α is known to play a central role in the pathogenesis of inflammatory bowel disease (IBD) and its concentration is increased in serum and stool of IBD patients [18]. Our finding in HBSMCs are in accordance with this study illustrating that potent inflammatory cytokines, such as TNF-α and IL-1β, increases the expression of importin α3 to increase the import of NF-κB in the nucleus. Further, this increase in importin α3 expression is attenuated by calcitriol. Calcitriol acts through vitamin D receptor since VDR knockdown by siRNA abolished the effect of calcitriol on importin α3 downregulation. These data show that calcitriol prevents TNF-α induced increase in importin α3 and RelA through a process mediated by the VDR.
Importin α3 knock down significantly reduced the TNF-α induced expression of RelA and abolished the effect of calcitriol on RelA expression. These data confirm that importin α3 mediates the translocation of RelA and that decrease in nuclear translocation of RelA occurs through downregulation of importin α3 by calcitriol.
IL-10, an anti-inflammatory cytokine inhibits NF-κB, thereby inhibiting the transcription of various pro-inflammatory cytokines including TNF-α, IL-1 and IL-6 [45, 46]. Vitamin D status is positively correlated to IL-10- secreting T-regulatory cells [47]. IL-10 in allergic inflammation is primarily released from T-regulatory cells and these cells can decrease allergic airway inflammation and airway hyperesponsiveness [46]. Calcitriol promotes the production of IL-10 in human B-cells [48]. Our results demonstrate that calcitriol potentiated the anti-inflammatory effect of IL-10 when treated concomitantly with TNF-α. However, the mechanisms by which IL-10 in presence of TNF-α decreases the expression of importin α3 warrant further studies.
Conclusion
These results support the immunomodulatory role of vitamin D in allergic airway inflammation and thus, could be potentially beneficial in the treatment of bronchial asthma. Further studies are needed to elucidate underlying molecular mechanisms involved in the decreased expression of importin α3 on stimulation with calcitriol.
Potential Limitations
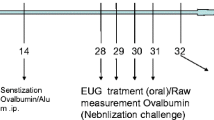
One of the potential limitations is that these studies are in-vitro, which requires confirmation under in vivo conditions in a model of asthma. Secondly, potential role of endogenous mediators, other than vitamin D, to regulate the action of importin α3, cannot be ruled out. We are developing vitamin D deficient, sufficient, and supplemented asthmatic mice to further examine such questions in airway hyperresponsiveness and allergic airway inflammation.
References
Agrawal DK, Shao Z. Pathogenesis of allergic airway inflammation. Curr Allergy Asthma Rep. 2010;10(1):39–48.
McGee HS, Stallworth AL, Agrawal T, Shao Z, Lorence L, Agrawal DK. Fms-like tyrosine kinase 3 ligand decreases t helper type 17 cells and suppressors of cytokine signaling proteins in the lung of house dust mite-sensitized and -challenged mice. Am J Respir Cell Mol Biol. 2010;43(5):520–9.
Gupta GK, Agrawal DK. Cpg oligodeoxynucleotides as tlr9 agonists: therapeutic application in allergy and asthma. BioDrugs. 2010;24(4):225–35.
Bosse Y, Maghni K, Hudson TJ. 1alpha,25-dihydroxy-vitamin d3 stimulation of bronchial smooth muscle cells induces autocrine, contractility, and remodeling processes. Physiol Genomics. 2007;29(2):161–8.
Gerthoffer WT, Singer CA. Secretory functions of smooth muscle: cytokines and growth factors. Mol Interv. 2002;2(7):447–56.
Tliba O, Panettieri Jr RA. Noncontractile functions of airway smooth muscle cells in asthma. Annu Rev Physiol. 2009;71:509–35.
Hershenson MB, Brown M, Camoretti-Mercado B, Solway J. Airway smooth muscle in asthma. Annu Rev Pathol. 2008;3:523–55.
Wertz IE, Dixit VM. Signaling to NF-kappab: regulation by ubiquitination. Cold Spring Harb Perspect Biol. 2010;2(3):a003350.
Agrawal DK, Ariyarathna K, Kelbe PW. (s)-albuterol activates pro-constrictory and pro-inflammatory pathways in human bronchial smooth muscle cells. J Allergy Clin Immunol. 2004;113(3):503–10.
Edwards MR, Bartlett NW, Clarke D, Birrell M, Belvisi M, Johnston SL. Targeting the nf-kappab pathway in asthma and chronic obstructive pulmonary disease. Pharmacol Ther. 2009;121(1):1–13.
Barnes PJ, Karin M. Nuclear factor-kappab: a pivotal transcription factor in chronic inflammatory diseases. N Engl J Med. 1997;336(15):1066–71.
Brar SS, Kennedy TP, Sturrock AB, Huecksteadt TP, Quinn MT, Murphy TM, et al. Nadph oxidase promotes nf-kappab activation and proliferation in human airway smooth muscle. Am J Physiol Lung Cell Mol Physiol. 2002;282(4):L782–95.
Pahl HL. Activators and target genes of rel/nf-kappab transcription factors. Oncogene. 1999;18(49):6853–66.
Xu SY, Xu YJ, Zhang ZX, Ni W, Chen SX. Effect of nuclear factor-kappab on signal transduction of passively sensitized human airway smooth muscle cells proliferation. Zhonghua Nei Ke Za Zhi. 2004;43(12):891–5.
Wright HL, Chikura B, Bucknall RC, Moots RJ, Edwards SW. Changes in expression of membrane tnf, nf-{kappa}b activation and neutrophil apoptosis during active and resolved inflammation. Ann Rheum Dis. 2011;70(3):537–43.
Song J, So T, Croft M. Activation of nf-kappab1 by ox40 contributes to antigen-driven t cell expansion and survival. J Immunol. 2008;180(11):7240–8.
Fagerlund R, Kinnunen L, Kohler M, Julkunen I, Melen K. Nf-{kappa}b is transported into the nucleus by importin {alpha}3 and importin {alpha}4. J Biol Chem. 2005;280(16):15942–51.
Theiss AL, Jenkins AK, Okoro NI, Klapproth JM, Merlin D, Sitaraman SV. Prohibitin inhibits tumor necrosis factor alpha-induced nuclear factor-kappa b nuclear translocation via the novel mechanism of decreasing importin alpha3 expression. Mol Biol Cell. 2009;20(20):4412–23.
Okada N, Ishigami Y, Suzuki T, Kaneko A, Yasui K, Fukutomi R, et al. Importins and exportins in cellular differentiation. J Cell Mol Med. 2008;12(5B):1863–71.
Caramori G, Oates T, Nicholson AG, Casolari P, Ito K, Barnes PJ, et al. Activation of nf-kappab transcription factor in asthma death. Histopathology. 2009;54(4):507–9.
D’Acquisto F, May MJ, Ghosh S. Inhibition of nuclear factor kappa b (nf-b): an emerging theme in anti-inflammatory therapies. Mol Interv. 2002;2(1):22–35.
Bosse Y, Lemire M, Poon AH, Daley D, He JQ, Sandford A, et al. Asthma and genes encoding components of the vitamin d pathway. Respir Res. 2009;10:98–112.
Carlberg C, Seuter S. The vitamin d receptor. Dermatol Clin. 2007;25(4):515–23. viii.
Damera G, Fogle HW, Lim P, Goncharova EA, Zhao H, Banerjee A, et al. Vitamin d inhibits growth of human airway smooth muscle cells through growth factor-induced phosphorylation of retinoblastoma protein and checkpoint kinase 1. Br J Pharmacol. 2009;158(6):1429–41.
Veldman CM, Cantorna MT, DeLuca HF. Expression of 1,25-dihydroxyvitamin d(3) receptor in the immune system. Arch Biochem Biophys. 2000;374(2):334–8.
Hewison M, Freeman L, Hughes SV, Evans KN, Bland R, Eliopoulos AG, et al. Differential regulation of vitamin d receptor and its ligand in human monocyte-derived dendritic cells. J Immunol. 2003;170(11):5382–90.
Pankajakshan D, Makinde TO, Gaurav R, Del Core M, Hatzoudis G, Pipinos I, et al. Successful transfection of genes using aav-2/9 vector in swine coronary and peripheral arteries. J Surg Res. 2011 Mar 21. [Epub ahead of print]PMID: 21529824.
Gupta GK, Dhar K, Del Core MG, Hunter 3rd WJ, Hatzoudis GI, Agrawal DK. Suppressor of cytokine signaling-3 and intimal hyperplasia in porcine coronary arteries following coronary intervention. Exp Mol Pathol. 2011;91(1):346–52.
Hohmann HP, Remy R, Scheidereit C, van Loon AP. Maintenance of nf-kappa b activity is dependent on protein synthesis and the continuous presence of external stimuli. Mol Cell Biol. 1991;11(1):259–66.
Peng X, Mehta R, Wang S, Chellappan S, Mehta RG. Prohibitin is a novel target gene of vitamin d involved in its antiproliferative action in breast cancer cells. Cancer Res. 2006;66(14):7361–9.
Banerjee A, Damera G, Bhandare R, Gu S, Lopez-Boado Y, Panettieri Jr R, et al. Vitamin d and glucocorticoids differentially modulate chemokine expression in human airway smooth muscle cells. Br J Pharmacol. 2008;155(1):84–92.
Nguyen M, Trubert CL, Rizk-Rabin M, Rehan VK, Besancon F, Cayre YE, et al. 1,25-dihydroxyvitamin d3 and fetal lung maturation: immunogold detection of vdr expression in pneumocytes type ii cells and effect on fructose 1,6 bisphosphatase. J Steroid Biochem Mol Biol. 2004;89–90(1–5):93–7.
Nguyen TM, Guillozo H, Marin L, Tordet C, Koite S, Garabedian M. Evidence for a vitamin d paracrine system regulating maturation of developing rat lung epithelium. Am J Physiol. 1996;271(3 Pt 1):L392–9.
Edelson JD, Chan S, Jassal D, Post M, Tanswell AK. Vitamin d stimulates DNA synthesis in alveolar type-ii cells. Biochim Biophys Acta. 1994;1221(2):159–66.
Litonjua AA, Weiss ST. Is vitamin d deficiency to blame for the asthma epidemic? J Allergy Clin Immunol. 2007;120(5):1031–5.
Brehm JM, Celedon JC, Soto-Quiros ME, Avila L, Hunninghake GM, Forno E, et al. Serum vitamin d levels and markers of severity of childhood asthma in costa rica. Am J Respir Crit Care Med. 2009;179(9):765–71.
Sutherland ER, Goleva E, Jackson LP, Stevens AD, Leung DY. Vitamin d levels, lung function, and steroid response in adult asthma. Am J Respir Crit Care Med. 2010;181(7):699–704.
Zosky GR, Berry LJ, Elliot JG, James AL, Gorman S, Hart PH. Vitamin d deficiency causes deficits in lung function and alters lung structure. Am J Respir Crit Care Med. 2011;183(10):1336–43.
Gupta A, Sjoukes A, Richards D, Banya W, Hawrylowicz C, Bush A, et al. Relationship between serum vitamin d, disease severity, and airway remodeling in children with asthma. Am J Respir Crit Care Med. 2011;184(12):1342–9.
D’Ambrosio D, Cippitelli M, Cocciolo MG, Mazzeo D, Di Lucia P, Lang R, et al. Inhibition of il-12 production by 1,25-dihydroxyvitamin d3. Involvement of nf-kappab downregulation in transcriptional repression of the p40 gene. J Clin Invest. 1998;101(1):252–62.
Harant H, Wolff B, Lindley IJ. 1alpha,25-dihydroxyvitamin d3 decreases DNA binding of nuclear factor-kappab in human fibroblasts. FEBS Lett. 1998;436(3):329–34.
Riis JL, Johansen C, Gesser B, Moller K, Larsen CG, Kragballe K, et al. 1alpha,25(OH)(2)D(3) regulates NF-kappab DNA binding activity in cultured normal human keratinocytes through an increase in ikappabalpha expression. Arch Dermatol Res. 2004;296(5):195–202.
Giarratana N, Penna G, Amuchastegui S, Mariani R, Daniel KC, Adorini L. A vitamin d analog down-regulates proinflammatory chemokine production by pancreatic islets inhibiting t cell recruitment and type 1 diabetes development. J Immunol. 2004;173(4):2280–7.
Sun J, Kong J, Duan Y, Szeto FL, Liao A, Madara JL, et al. Increased nf-kappab activity in fibroblasts lacking the vitamin d receptor. Am J Physiol Endocrinol Metab. 2006;291(2):E315–22.
Dhingra S, Sharma AK, Arora RC, Slezak J, Singal PK. Il-10 attenuates tnf-alpha-induced nf kappab pathway activation and cardiomyocyte apoptosis. Cardiovasc Res. 2009;82(1):59–66.
McGee HS, Agrawal DK. Naturally occurring and inducible t-regulatory cells modulating immune response in allergic asthma. Am J Respir Crit Care Med. 2009;180(3):211–25.
Smolders J, Thewissen M, Peelen E, Menheere P, Tervaert JW, Damoiseaux J, et al. Vitamin d status is positively correlated with regulatory t cell function in patients with multiple sclerosis. PLoS One. 2009;4(8):e6635.
Heine G, Niesner U, Chang HD, Steinmeyer A, Zugel U, Zuberbier T, et al. 1,25-dihydroxyvitamin D(3) promotes il-10 production in human b cells. Eur J Immunol. 2008;38(8):2210–8.
Holick CN, Stanford JL, Kwon EM, Ostrander EA, Nejentsev S, Peters U. Comprehensive association analysis of the vitamin d pathway genes, vdr, cyp27b1, and cyp24a1, in prostate cancer. Cancer Epidemiol Biomark Prev. 2007;16(10):1990–9.
Acknowledgments
This work was supported by NIH grants R01HL085680 and R01AI75315 to DKA.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 12 kb)
Figure S1
Effect of Calcitriol treatment on mRNA and protein expression of CYP24A1 (A, B) and CYP27B1 (C, D) in HBSMCs: Cultured HBSMCs were serum starved for 24 hr followed by treatment with different doses of calcitriol (0.1- 100 nM) for 24 hr. The mRNA and protein were isolated from cell lysates and subjected to qPCR and immunoblotting, respectively. Data is shown as mean ± SEM from three individual samples in each experiment; ***p<0.001. (TIFF 220 kb)
Figure S2
Effect of Calcitriol treatment on mRNA expression of VDR in HBSMCs: Cultured HBSMCs were serum starved for 24 hr followed by treatment with calcitriol (100 nM) for at times 0-36hr. The mRNA were isolated from cell lysates and subjected to qPCR. Data is shown as mean ± SEM from three individual samples; ***p<0.001 (TIFF 125 kb)
Figure S3
Effect of Calcitriol treatment on mRNA expression of importin α3 in HBSMCs: Cultured HBSMCs were serum starved for 24 hr followed by treatment with calcitriol (100 nM) for at times 0-36hr. The mRNA was isolated from cell lysates and subjected to qPCR. Data is shown as mean ± SEM from three individual samples; *p <0.05, **p<0.01, ***p <0.001. (TIFF 123 kb)
Figure S4
Effect of Calcitriol treatment on mRNA(A)and protein(B) expression of importin α4in HBSMCs: Cultured HBSMCs were serum starved for 24 hr followed by treatment with different doses of calcitriol (0.1- 100 nM) for 24 hr. The mRNA and protein were isolated from cell lysates and subjected to qPCR and immunoblotting, respectively. Data is shown as mean ± SEM from three individual samples (TIFF 122 kb)
Rights and permissions
About this article
Cite this article
Agrawal, T., Gupta, G.K. & Agrawal, D.K. Calcitriol Decreases Expression of Importin α3 and Attenuates RelA Translocation in Human Bronchial Smooth Muscle Cells. J Clin Immunol 32, 1093–1103 (2012). https://doi.org/10.1007/s10875-012-9696-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-012-9696-x